Bariatric Surgery Outcomes in Patients with Severe Obesity Compared to Patients with Non-Severe Obesity at A New Institution in The United Arab Emirates
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Aims
2.3. Definitions
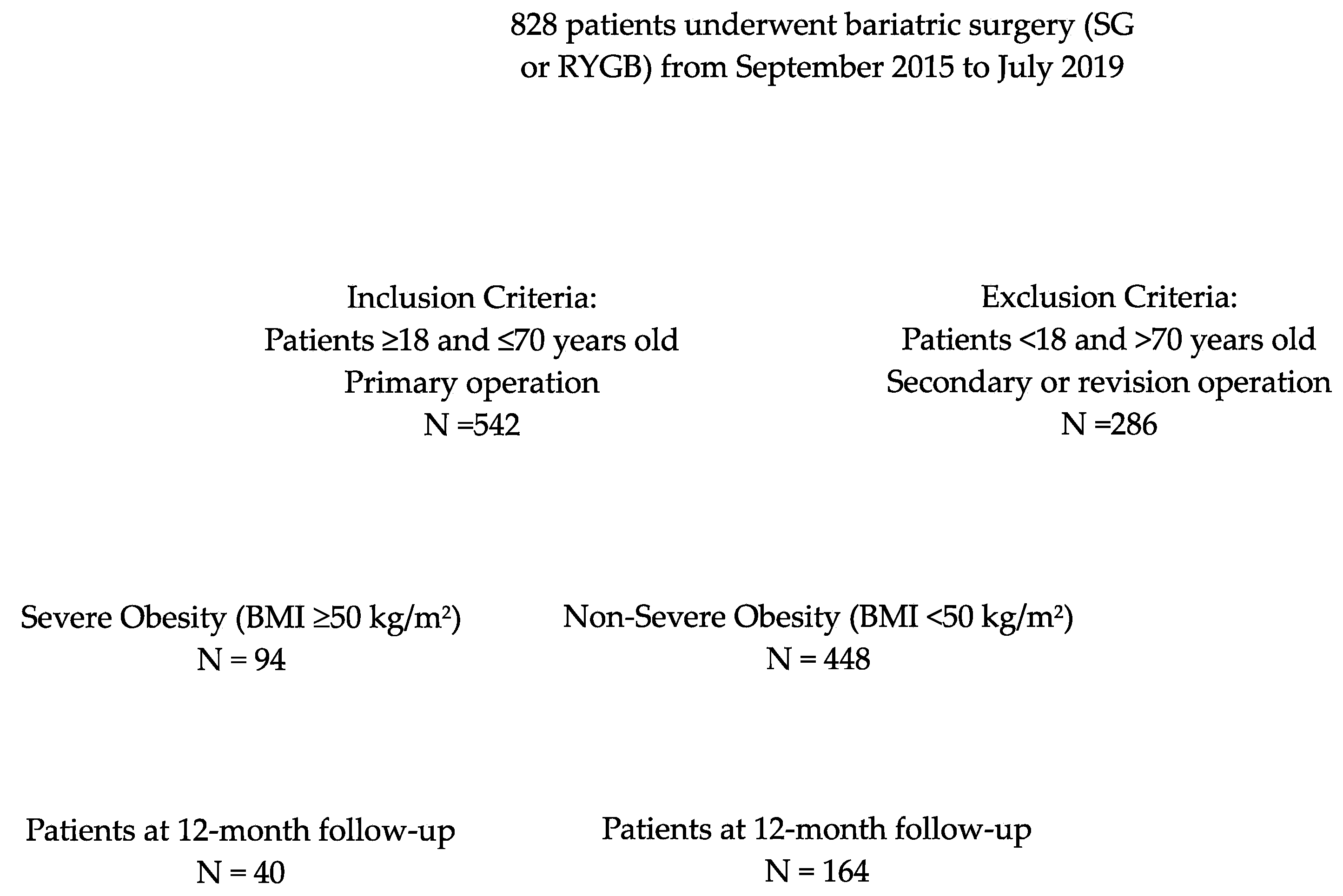
2.4. Inclusion/Exclusion Criteria for Study Participation
2.5. Preoperative Evaluation
2.6. Surgical Approach
2.7. Institutional Surgical Techniques and Bariatric Procedures
2.8. Postoperative Care
2.9. Data Collection and Surgical Outcomes
2.10. Statistical Analyses
3. Results
3.1. Demographic Characteristics
3.2. Operative Details
3.3. Postoperative Complications
3.4. Postoperative Outcomes
3.5. Follow-up Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 2 July 2022).
- Sulaiman, N.; Elbadawi, S.; Hussein, A.; Abusnana, S.; Madani, A.; Mairghani, M.; Alawadi, F.; Sulaiman, A.; Zimmet, P.; Huse, O.; et al. Prevalence of overweight and obesity in United Arab Emirates Expatriates: The UAE National Diabetes and Lifestyle Study. Diabetol. Metab. Syndr. 2017, 9, 88. [Google Scholar] [CrossRef]
- Nawar, R.; Ibrahim, E.; Abusnana, S.; Al Awadi, F.; Al Hammadi, F.H.; Farghaly, M.; Fiad, T.M.; Aly, H.; Mohamed, Y.A.; Ben Serghin, Z. Understanding the Gaps in Obesity Management in the UAE: Perceptions, Barriers, and Attitudes. Dubai Diabetes Endocrinol. J. 2021, 27, 37–49. [Google Scholar] [CrossRef]
- Radwan, H.; Ballout, R.A.; Hasan, H.; Lessan, N.; Karavetian, M.; Rizk, R. The Epidemiology and Economic Burden of Obesity and Related Cardiometabolic Disorders in the United Arab Emirates: A Systematic Review and Qualitative Synthesis. J. Obes. 2018, 2018, 2185942. [Google Scholar] [CrossRef] [PubMed]
- Abusnana, S.; Fargaly, M.; Alfardan, S.H.; Al Hammadi, F.H.; Bashier, A.; Kaddaha, G.; McGowan, B.; Nawar, R.; Sadiya, A. Clinical Practice Recommendations for the Management of Obesity in the United Arab Emirates. Obes. Facts 2018, 11, 413–428. [Google Scholar] [CrossRef]
- AlAbdulKader, A.M.; Tuwairqi, K.; Rao, G. Obesity and Cardiovascular Risk in the Arab Gulf States. Curr. Cardiovasc. Risk Rep. 2020, 14, 7. [Google Scholar] [CrossRef]
- Rozjabek, H.; Fastenau, J.; LaPrade, A.; Sternbach, N. Adult Obesity and Health-Related Quality of Life, Patient Activation, Work Productivity, and Weight Loss Behaviors in the United States. Diabetes Metab. Syndr. Obesity Targets Ther. 2020, 13, 2049–2055. [Google Scholar] [CrossRef]
- Busutil, R.; Espallardo, O.; Torres, A.; Martínez-Galdeano, L.; Zozaya, N.; Hidalgo-Vega, Á. The impact of obesity on health-related quality of life in Spain. Health Qual. Life Outcomes 2017, 15, 197. [Google Scholar] [CrossRef] [PubMed]
- Wadden, T.A.; Tronieri, J.S.; Butryn, M.L. Lifestyle modification approaches for the treatment of obesity in adults. Am. Psychol. 2020, 75, 235–251. [Google Scholar] [CrossRef] [PubMed]
- Courcoulas, A.P.; Gallagher, J.W.; Neiberg, R.H.; Eagleton, E.B.; DeLany, J.P.; Lang, W.; Punchai, S.; Gourash, W.; Jakicic, J.M. Bariatric Surgery vs. Lifestyle Intervention for Diabetes Treatment: 5-Year Outcomes from a Randomized Trial. J. Clin. Endocrinol. Metab. 2020, 105, 866–876. [Google Scholar] [CrossRef]
- Coimbra, S.; Reis, F.; Ferreira, C.; Nunes, S.; Viana, S.; Catarino, A.; Rocha-Pereira, P.; Belo, L.; Monteiro, L.; Catarino, C.; et al. Weight loss achieved by bariatric surgery modifies high-density lipoprotein subfractions and low-density lipoprotein oxidation towards atheroprotection. Clin. Biochem. 2019, 63, 46–53. [Google Scholar] [CrossRef]
- Ozsoy, Z.; Demir, E. Which Bariatric Procedure Is the Most Popular in the World? A Bibliometric Comparison. Obes. Surg. 2018, 28, 2339–2352. [Google Scholar] [CrossRef] [PubMed]
- Angrisani, L.; Santonicola, A.; Iovino, P.; Vitiello, A.; Higa, K.; Himpens, J.; Buchwald, H.; Scopinaro, N. IFSO Worldwide Survey 2016: Primary, Endoluminal, and Revisional Procedures. Obes. Surg. 2018, 28, 3783–3794. [Google Scholar] [CrossRef]
- Hung, K.-C.; Kao, C.-L.; Sun, C.-K.; Lin, H.-J. Perioperative complications and Intensive Care Unit utilization in super-superobese patients undergoing laparoscopic bariatric surgery. Tzu Chi Med. J. 2019, 31, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Pierpont, Y.N.; Dinh, T.P.; Salas, R.E.; Johnson, E.L.; Wright, T.G.; Robson, M.C.; Payne, W.G. Obesity and Surgical Wound Healing: A Current Review. ISRN Obes. 2014, 2014, 638936. [Google Scholar] [CrossRef]
- Kakarla, V.R.; Nandipati, K.; Lalla, M.; Castro, A.; Merola, S. Are laparoscopic bariatric procedures safe in superobese (BMI ≥ 50 kg/m2) patients? An NSQIP data analysis. Surg. Obes. Relat. Dis. 2011, 7, 452–458. [Google Scholar] [CrossRef]
- Romero-Velez, G.; Pechman, D.M.; Flores, F.M.; Moran-Atkin, E.; Choi, J.; Camacho, D.R. Bariatric surgery in the super-super morbidly obese: Outcome analysis of patients with BMI > 70 using the ACS-NSQIP database. Surg. Obes. Relat. Dis. Off. J. Am. Soc. Bariatr. Surg. 2020, 16, 894–899. [Google Scholar] [CrossRef] [PubMed]
- Dapri, G.; Cadière, G.B.; Himpens, J. Superobese and super-superobese patients: 2-step laparoscopic duodenal switch. Surg. Obes. Relat. Dis. Off. J. Am. Soc. Bariatr. Surg. Off. J. Am. Soc. Bariatr. Surg. 2011, 7, 703–708. [Google Scholar] [CrossRef]
- Daigle, C.R.; Andalib, A.; Corcelles, R.; Cetin, D.; Schauer, P.R.; Brethauer, S.A. Bariatric and metabolic outcomes in the super-obese elderly. Surg. Obes. Relat. Dis. Off. J. Am. Soc. Bariatr. Surg. 2016, 12, 132–137. [Google Scholar] [CrossRef]
- Mukherjee, S.; Devalia, K.; Rahman, M.G.; Mannur, K.R. Sleeve gastrectomy as a bridge to a second bariatric procedure in superobese patients—A single institution experience. Surg. Obes. Relat. Dis. Off. J. Am. Soc. Bariatr. Surg. 2012, 8, 140–144. [Google Scholar] [CrossRef]
- Torchia, F.; Mancuso, V.; Civitelli, S.; Di Maro, A.; Cariello, P.; Rosano, P.T.; Sionne, G.C.; Lorenzo, M.; Cascardo, A.J. LapBand System® in Super-Superobese Patients (>60 kg/m2): 4-Year Results. Obes. Surg. 2009, 19, 1211–1215. [Google Scholar] [CrossRef]
- Brethauer, S.A.; Kim, J.; el Chaar, M.; Papasavas, P.; Eisenberg, D.; Rogers, A.; Ballem, N.; Kligman, M.; Kothari, S. Standardized outcomes reporting in metabolic and bariatric surgery. Surg. Obes. Relat. Dis. 2015, 11, 489–506. [Google Scholar] [CrossRef] [PubMed]
- Abdelaal, M.; le Roux, C.W.; Docherty, N.G. Morbidity and mortality associated with obesity. Ann. Transl. Med. 2017, 5, 161. [Google Scholar] [CrossRef] [PubMed]
- AlBlooshi, A.; Shaban, S.; AlTunaiji, M.; Fares, N.; AlShehhi, L.; AlShehhi, H.; AlMazrouei, A.; Souid, A. Increasing obesity rates in school children in United Arab Emirates. Obes. Sci. Pr. 2016, 2, 196–202. [Google Scholar] [CrossRef] [PubMed]
- UAE. Bariatric Surgery Market- Growth Trends and Forecasts (2023–2028). Mordor Intelligence. Available online: https://www.mordorintelligence.com/industry-reports/uae-bariatric-surgery-market (accessed on 31 January 2024).
- Middle East and Africa Bariatric Surgery Market 2019–2028. Triton Market Research. Available online: https://www.tritonmarketresearch.com/reports/middle-east-and-africa-bariatric-surgery-market (accessed on 31 January 2024).
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018 Key Findings Data from the National Health and Nutrition Examination Survey. 2017. Available online: https://www.cdc.gov/nchs/products/index.htm (accessed on 28 February 2024).
- Ward, Z.J.; Bleich, S.N.; Cradock, A.L.; Barrett, J.L.; Giles, C.M.; Flax, C.; Long, M.W.; Gortmaker, S.L. Projected U.S. state-level prevalence of adult obesity and severe obesity. N. Engl. J. Med. 2019, 381, 2440–2450. [Google Scholar] [CrossRef] [PubMed]
| N = 542 | SO (n = 94) | NSO (n = 448) | p-Value |
|---|---|---|---|
| Age, yr, mean ± SD | 33.8 ± 13.4 | 37.0 ± 11.5 | 0.02 |
| BMI, kg/m2, mean ± SD | 56.5 ± 6.2 | 41.8 ± 4.1 | <0.00001 |
| Female, n (%) | 52 (55.3) | 282 (62.9) | 0.17 |
| ASA, median (Range) | 2.7 (2–3) | 2.6 (2–3) | 0.10 |
| Comorbidities, n (%) | |||
| Obstructive sleep apnea | 44 (46.8) | 138 (30.8) | 0.003 |
| Hyperlipidemia | 33 (35.1) | 217 (48.4) | 0.02 |
| Hypertension | 32 (34.0) | 154 (34.4) | 0.95 |
| Diabetes mellitus | 28 (29.8) | 133 (29.7) | 0.98 |
| GERD | 21 (22.3) | 116 (25.9) | 0.47 |
| Chronic kidney disease | 5 (5.3) | 22 (4.9) | 0.87 |
| Coronary artery disease | 2 (2.1) | 20 (4.5) | 0.30 |
| End stage renal disease | 1 (1.1) | 3 (0.7) | 0.68 |
| COPD | 0 (0) | 8 (1.8) | 0.19 |
| Current smoker, n (%) | 15 (15.9) | 66 (14.7) | 0.76 |
| Type of bariatric surgery, n (%) | |||
| RYGB | 37 (39.4) | 199 (44.4) | 0.37 |
| Sleeve gastrectomy | 57 (60.6) | 249 (55.6) | 0.37 |
| N = 542 | SO (n = 94) | NSO (n = 448) | p-Value |
|---|---|---|---|
| Laparoscopic surgical approach, n (%) | 93 (98.9) | 442 (98.6) | 0.83 |
| Conversion rate, n (%) | 0 (0) | 1 (0.2) | 0.65 |
| Complications, n (%) | 6 (6.4) | 26 (5.8) | 0.83 |
| Operative time, min (mean ± SD) | |||
| RYGB | 159 ± 32 | 161 ± 58 | 0.80 |
| SG | 90 ± 20 | 92 ± 32 | 0.70 |
| Blood loss <125 mL (mean ± SD) | 94 (100) | 448 (100) | --- |
| N = 542 | SO (n = 94) | NSO (n = 448) | p-Value |
|---|---|---|---|
| Early minor complications, n (%) | 5 (5.3) | 24 (5.3) | 0.99 |
| Nausea, vomiting | 4 (4.3) | 15 (3.3) | 0.67 |
| Trocar/surgical site infection | 1 (1.0) | 3 (0.6) | 0.68 |
| Pneumonia | 0 (0) | 0 (0) | - |
| UTI | 0 (0) | 1 (0.2) | 0.65 |
| Dumping syndrome | 0 (0) | 2 (0.4) | 0.52 |
| Other | 0 (0) | 3 (0.6) | 0.42 |
| Early major complications, n (%) | 5 (5.3) | 16 (3.5) | 0.42 |
| VTE | 0 (0) | 0 (0) | - |
| Anastomotic leakage | 1 (1.0) | 2 (0.4) | 0.47 |
| GI bleeding | 1 (1.0) | 7 (1.5) | 0.72 |
| Postoperative transfusion | 0 (0) | 0 (0) | - |
| Small bowel obstruction | 1 (1.0) | 1 (0.2) | 0.22 |
| Bowel perforation | 0 (0) | 0 (0) | - |
| Surgical site infection | 0 (0) | 2 (0.4) | 0.36 |
| Myocardial infarction | 0 (0) | 0 (0) | - |
| Respiratory failure | 1 (1.0) | 1 (0.2) | 0.22 |
| Sepsis | 0 (0) | 2 (0.4) | 0.52 |
| Cerebrovascular accident | 1 (1.0) | 1 (0.2) | 0.22 |
| Endoscopy needed within 30 days | 3 (3.1) | 21 (4.6) | 0.52 |
| Placement of percutaneous drain | 1 (1.0) | 1 (0.2) | 0.22 |
| N = 542 | SO (n = 94) | NSO (n = 448) | p-Value |
|---|---|---|---|
| Length of stay, days (mean ± SD) | 3.1 ± 3.9 | 2.7 ± 1.3 | 0.06 |
| ED visits within 30 days, n (%) | 18 (19.1) | 112 (25) | 0.27 |
| Readmission within 30 days, n (%) | 5 (5.3) | 15 (3.3) | 0.36 |
| Reoperations within 30 days, n (%) | 3 (3.2) | 12 (2.7) | 0.78 |
| Mortality, n (%) | 0 (0) | 0 (0) | --- |
| N = 542 | SO (n = 94) | NSO (n = 448) | p-Value |
|---|---|---|---|
| Duration of follow-up, months, mean ± SD | 13.5 ± 11.0 | 10.9 ± 9.2 | 0.02 |
| Patients at 12-month follow-up, N, % | 40 (42.5) | 164 (36.6) | 0.02 |
| BMI at 12 months postop, kg/m2, mean ± SD | 40.8 ± 8.1 | 29.4 ± 4.2 | <0.00001 |
| % TBWL, mean ± SD | 28.1 ± 10.2 | 29.0 ± 7.7 | 0.58 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
DeCicco, J.P.; Barajas-Gamboa, J.S.; Dang, J.T.; Diaz Del Gobbo, G.; Raza, J.; Abril, C.; Guerron, A.D.; Pantoja, J.P.; Hegazin, S.B.; Corcelles, R.; et al. Bariatric Surgery Outcomes in Patients with Severe Obesity Compared to Patients with Non-Severe Obesity at A New Institution in The United Arab Emirates. J. Clin. Med. 2024, 13, 1907. https://doi.org/10.3390/jcm13071907
DeCicco JP, Barajas-Gamboa JS, Dang JT, Diaz Del Gobbo G, Raza J, Abril C, Guerron AD, Pantoja JP, Hegazin SB, Corcelles R, et al. Bariatric Surgery Outcomes in Patients with Severe Obesity Compared to Patients with Non-Severe Obesity at A New Institution in The United Arab Emirates. Journal of Clinical Medicine. 2024; 13(7):1907. https://doi.org/10.3390/jcm13071907
Chicago/Turabian StyleDeCicco, Jamie P., Juan S. Barajas-Gamboa, Jerry T. Dang, Gabriel Diaz Del Gobbo, Javed Raza, Carlos Abril, Alfredo D. Guerron, Juan Pablo Pantoja, Safa Botros Hegazin, Ricard Corcelles, and et al. 2024. "Bariatric Surgery Outcomes in Patients with Severe Obesity Compared to Patients with Non-Severe Obesity at A New Institution in The United Arab Emirates" Journal of Clinical Medicine 13, no. 7: 1907. https://doi.org/10.3390/jcm13071907
APA StyleDeCicco, J. P., Barajas-Gamboa, J. S., Dang, J. T., Diaz Del Gobbo, G., Raza, J., Abril, C., Guerron, A. D., Pantoja, J. P., Hegazin, S. B., Corcelles, R., Rodriguez, J., & Kroh, M. (2024). Bariatric Surgery Outcomes in Patients with Severe Obesity Compared to Patients with Non-Severe Obesity at A New Institution in The United Arab Emirates. Journal of Clinical Medicine, 13(7), 1907. https://doi.org/10.3390/jcm13071907







