Long COVID Clinical Severity Types Based on Symptoms and Functional Disability: A Longitudinal Evaluation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Participants
- They had a diagnosis of LC. They were not required to have had a positive polymerase chain reaction (PCR) test or antibody test for SARS-CoV-2, as per NICE definition [2]. These tests were not widely available to the general population of the UK at the start of the pandemic.
- They were receiving management for the condition from a LOCOMOTION study participating LC service.
- They had LC symptoms which could not be explained through alternative medical diagnosis.
- They were registered on the ELAROS digital PROMs platform [22] and were required to complete PROMs every three months after being registered.
2.3. C19-YRS Instrument
2.4. Statistical Analysis
2.5. Role of the Funding Source
3. Results
3.1. Patients
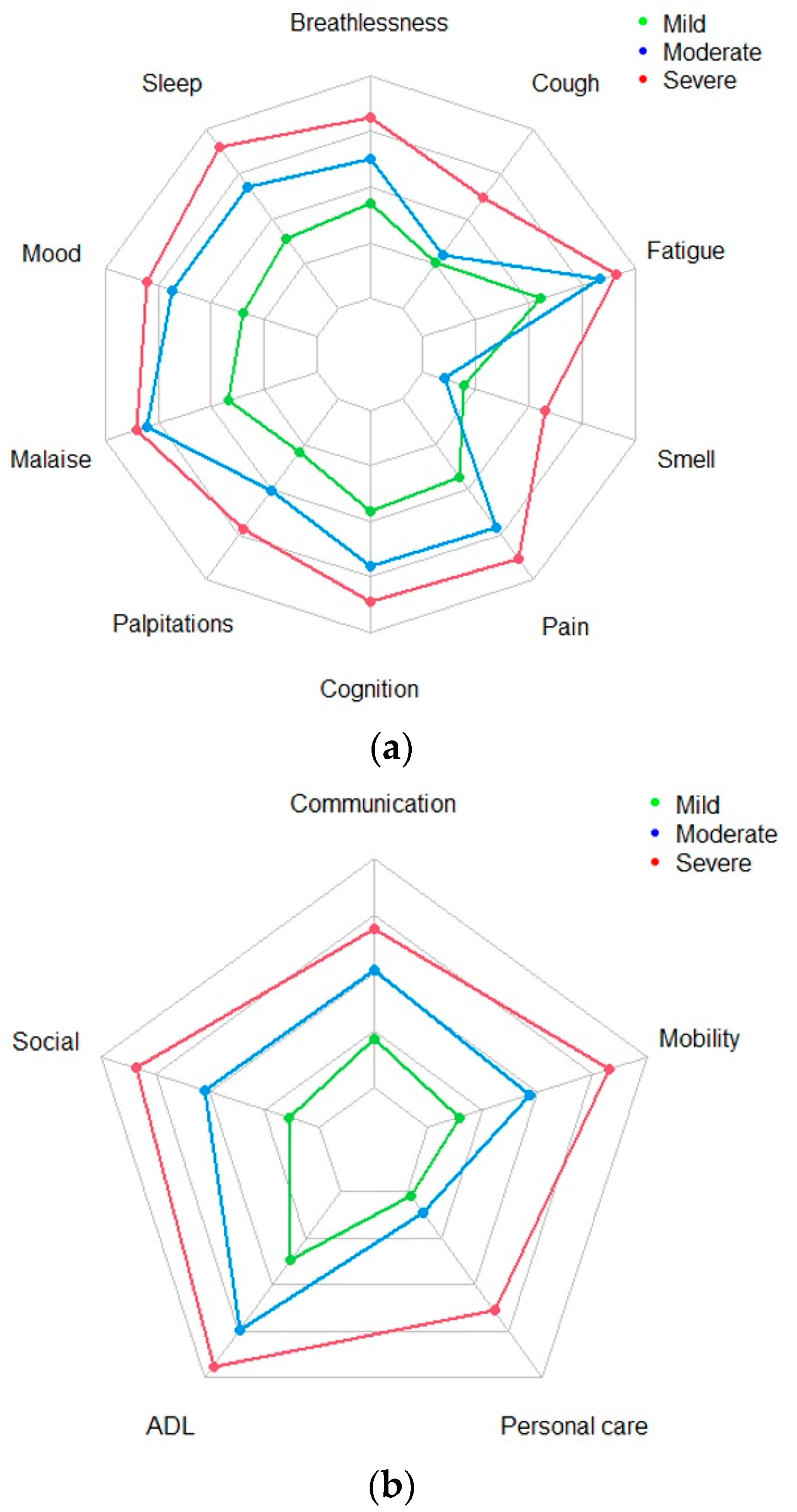
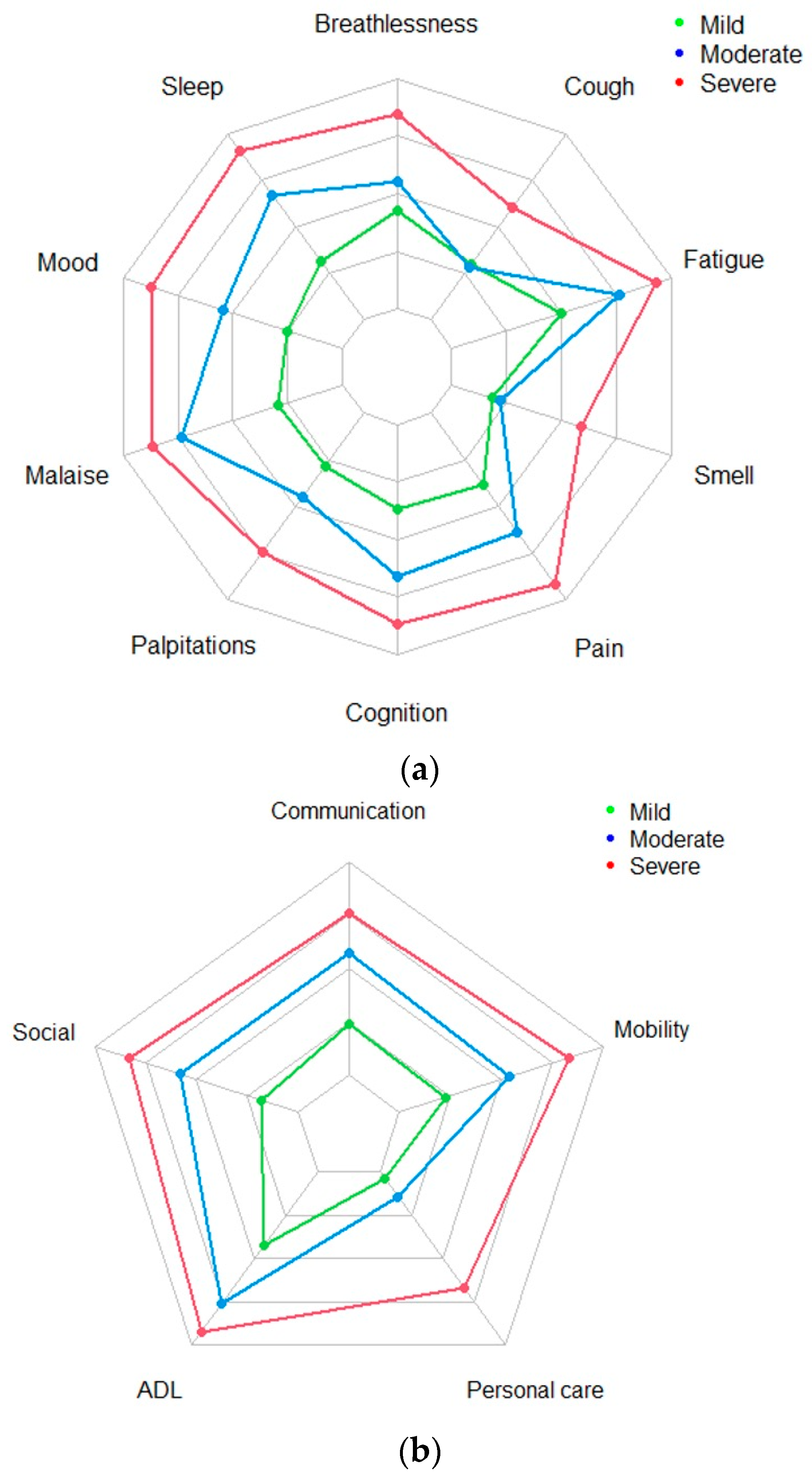
3.2. Cluster Analysis
3.3. Polychoric Factor Analysis (PFA)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Callard, F.; Perego, E. How and why patients made Long COVID. Soc. Sci. Med. 2021, 268, 113426. [Google Scholar] [CrossRef] [PubMed]
- NICE. COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19; NICE: Ra’anana, Israel, 2022. [Google Scholar]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V.; Condition WHOCCDWGoP-C. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef] [PubMed]
- ONS. Prevalence of Ongoing Symptoms following Coronavirus (COVID-19) Infection in the UK: 2 February 2023. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/2february2023 (accessed on 4 March 2023).
- Chen, C.; Haupert, S.R.; Zimmermann, L.; Shi, X.; Fritsche, L.G.; Mukherjee, B. Global Prevalence of Post-Coronavirus Disease 2019 (COVID-19) Condition or Long COVID: A Meta-Analysis and Systematic Review. J. Infect. Dis. 2022, 226, 1593–1607. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef] [PubMed]
- Sivan, M.; Preston, N.; Parkin, A.; Makower, S.; Gee, J.; Ross, D.; Tarrant, R.; Davison, J.; Halpin, S.; O’Connor, R.J.; et al. The modified COVID-19 Yorkshire Rehabilitation Scale (C19-YRSm) patient-reported outcome measure for Long Covid or Post-COVID-19 syndrome. J. Med. Virol. 2022, 94, 4253–4264. [Google Scholar] [CrossRef] [PubMed]
- NHSEngland. National Guidance for Post-COVID Syndrome Assessment Clinics; NHSEngland: London, UK, 2021. [Google Scholar]
- Ayuso Garcia, B.; Besteiro Balado, Y.; Perez Lopez, A.; Romay Lema, E.; Marchan-Lopez, A.; Rodriguez Alvarez, A.; Garcia Pais, M.J.; Corredoira Sanchez, J.; Rabunal Rey, R. Assessment of Post-COVID Symptoms Using the C19-YRS Tool in a Cohort of Patients from the First Pandemic Wave in Northwestern Spain. Telemed. J. E-Health 2023, 29, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Gozdziewicz, L.; Tobis, S.; Chojnicki, M.; Wieczorowska-Tobis, K.; Neumann-Podczaska, A. The Value of the COVID-19 Yorkshire Rehabilitation Scale in the Assessment of Post-COVID among Residents of Long-Term Care Facilities. Healthcare 2024, 12, 333. [Google Scholar] [CrossRef]
- Kustura, L.; Bobek, D.; Poljicanin, A.; Pavelin, S.; Buljubasic Soda, M.; Soda, J.; Aksentijevic, J.; Duka Glavor, K.; Narancic Knez, N.; Viali, V.; et al. Psychometric properties and observational data for COVID-19 Yorkshire Rehabilitation Scale (C19-YRSm) for post-COVID-19 syndrome. QJM Int. J. Med. 2024, 117, 38–47. [Google Scholar] [CrossRef]
- Tamadoni, N.; Bakhtiari, A.; Nikbakht, H.A. Psychometric properties of the COVID-19 Yorkshire Rehabilitation Scale: Post-COVID-19 syndrome in Iranian elderly population. BMC Infect. Dis. 2024, 24, 77. [Google Scholar] [CrossRef]
- Gorst, S.L.; Seylanova, N.; Harman, N.; O’Hara, M.; Terwee, C.B.; Williamson, P.R.; Needham, D.M.; Munblit, D.; Nicholson, T.; Group, P.-C.S. A Core Outcome Measurement Set (COMS) for Research and Clinical Practice in Post COVID-19 Condition (Long COVID) in Adults: An International Delphi Consensus Study. Lancet Respir Med. 2023, in press.
- Dos Santos, T.D.; Souza, J.A.; Cardoso, D.M.; Berni, V.B.; Pasqualoto, A.S.; de Albuquerque, I.M. Predictors of Post-COVID-19 Functional Status Scale in Hospitalized Patients Recovering From SARS-CoV-2 Infection. Am. J. Phys. Med. Rehabil. 2024, 103, 143–148. [Google Scholar] [CrossRef]
- Hughes, S.E.; Haroon, S.; Subramanian, A.; McMullan, C.; Aiyegbusi, O.L.; Turner, G.M.; Jackson, L.; Davies, E.H.; Frost, C.; McNamara, G.; et al. Development and validation of the symptom burden questionnaire for long covid (SBQ-LC): Rasch analysis. BMJ 2022, 377, e070230. [Google Scholar] [CrossRef]
- Evans, R.A.; McAuley, H.; Harrison, E.M.; Shikotra, A.; Singapuri, A.; Sereno, M. Physical, cognitive and mental health impacts of COVID-19 after hospitalisation: A UK multicentre prospective cohort study. Lancet Respir. Med. 2021, 9, 1275–1287. [Google Scholar] [CrossRef] [PubMed]
- Sivan, M.; Parkin, A.; Makower, S.; Greenwood, D.C. Post-COVID syndrome symptoms, functional disability, and clinical severity phenotypes in hospitalized and nonhospitalized individuals: A cross-sectional evaluation from a community COVID rehabilitation service. J. Med. Virol. 2022, 94, 1419–1427. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Shi, L.; Jiang, Z.; Zeng, N.; Mei, H.; Lu, Y.; Yang, J.; Jin, F.; Ni, S.; Wu, S.; et al. The phenotype and prediction of long-term physical, mental and cognitive COVID-19 sequelae 20 months after recovery, a community-based cohort study in China. Mol. Psychiatry 2023, 28, 1793–1801. [Google Scholar] [CrossRef]
- Fischer, A.; Badier, N.; Zhang, L.; Elbeji, A.; Wilmes, P.; Oustric, P.; Benoy, C.; Ollert, M.; Fagherazzi, G. Long COVID Classification: Findings from a Clustering Analysis in the Predi-COVID Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 16018. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-de-Las-Penas, C.; Martin-Guerrero, J.D.; Florencio, L.L.; Navarro-Pardo, E.; Rodriguez-Jimenez, J.; Torres-Macho, J.; Pellicer-Valero, O.J. Clustering analysis reveals different profiles associating long-term post-COVID symptoms, COVID-19 symptoms at hospital admission and previous medical co-morbidities in previously hospitalized COVID-19 survivors. Infection 2023, 51, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Sivan, M.; Greenhalgh, T.; Darbyshire, J.L.; Mir, G.; O’Connor, R.J.; Dawes, H.; Greenwood, D.; O’Connor, D.; Horton, M.; Petrou, S. LOng COvid Multidisciplinary consortium Optimising Treatments and servIces acrOss the NHS (LOCOMOTION): Protocol for a mixed-methods study in the UK. BMJ Open 2022, 12, e063505. [Google Scholar] [CrossRef] [PubMed]
- Sivan, M.; Rocha Lawrence, R.; O’Brien, P. Digital Patient Reported Outcome Measures Platform for Post-COVID-19 Condition and Other Long-Term Conditions: User-Centered Development and Technical Description. JMIR Hum. Factors 2023, 10, e48632. [Google Scholar] [CrossRef]
- WHO. World Health Organization International Classification of Functioning, Disability and Health; WHO: Geneva, Switzerland, 2001. [Google Scholar]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Gloeckl, R.; Leitl, D.; Schneeberger, T.; Jarosch, I.; Koczulla, A.R. Rehabilitative interventions in patients with persistent post COVID-19 symptoms-a review of recent advances and future perspectives. In European Archives of Psychiatry and Clinical Neuroscience; Springer: Berlin/Heidelberg, Germany, 2023. [Google Scholar] [CrossRef]
- Faghy, M.A.; Duncan, R.; Hume, E.; Gough, L.; Roscoe, C.; Laddu, D.; Arena, R.; Asthon, R.E.M.; Dalton, C. Developing effective strategies to optimize physical activity and cardiorespiratory fitness in the long Covid population—The need for caution and objective assessment. In Progress in Cardiovascular Diseases; Elsevier: Amsterdam, The Netherlands, 2024. [Google Scholar] [CrossRef]
- Owen, R.; Ashton, R.E.M.; Ferraro, F.V.; Skipper, L.; Bewick, T.; Leighton, P.; Phillips, B.E.; Faghy, M.A. Forming a consensus opinion to inform long COVID support mechanisms and interventions: A modified Delphi approach. EClinicalMedicine 2023, 62, 102145. [Google Scholar] [CrossRef] [PubMed]
- National Health Service England. Your Covid Recovery. Available online: https://www.nhs.uk/conditions/covid-19/long-term-effects-of-covid-19-long-covid/ (accessed on 21 March 2024).
- WHO. Support for Rehabilitation: Self-Management after COVID-19-Related Illness; WHO, Ed.; WHO Regional Office for Europe: Copenhagen, Denmark, 2021. [Google Scholar]
- Galland-Decker, C.; Marques-Vidal, P.; Vollenweider, P. Prevalence and factors associated with fatigue in the Lausanne middle-aged population: A population-based, cross-sectional survey. BMJ Open 2019, 9, e027070. [Google Scholar] [CrossRef] [PubMed]
- Ruscio, A.M.; Hallion, L.S.; Lim, C.C.W.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Alonso, J.; Andrade, L.H.; Borges, G.; Bromet, E.J.; Bunting, B.; et al. Cross-sectional Comparison of the Epidemiology of DSM-5 Generalized Anxiety Disorder across the Globe. JAMA Psychiatry 2017, 74, 465–475. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, K.K.; Brown, D.A.; McDuff, K.; St Clair-Sullivan, N.; Solomon, P.; Chan Carusone, S.; McCorkell, L.; Wei, H.; Goulding, S.; O’Hara, M.; et al. Conceptualising the episodic nature of disability among adults living with Long COVID: A qualitative study. BMJ Glob. Health 2023, 8, e011276. [Google Scholar] [CrossRef]
- Stelson, E.A.; Dash, D.; McCorkell, L.; Wilson, C.; Assaf, G.; Re’em, Y.; Wei, H. Return-to-work with long COVID: An Episodic Disability and Total Worker Health(R) analysis. Soc. Sci. Med. 2023, 338, 116336. [Google Scholar] [CrossRef]

| All (n = 759) | Mild (n = 96) | Moderate (n = 422) | Severe (n = 241) | |
|---|---|---|---|---|
| Female | 527 (69.4%) | 69 (71.9%) | 291 (69.0%) | 167 (69.3%) |
| Mean age (SD) in years | 46.8 (12.7) | 46.2 (11.9) | 46.6 (12.7) | 47.3 (13.0) |
| Mean weight (kg) (SD) (n = 127) | 82.4 (23.0) | 79.5 (16.9) | 82.0 (22.1) | 86.4 (36.1) |
| Mean BMI (kg/m2) (SD) (n = 127) | 28.0 (8.37) | 26.2 (3.95) | 28.1 (6.51) | 28.8 (10.00) |
| Ethnicity | ||||
| White (n = 565) | 74.4% | 9.0% | 60.4% | 30.6% |
| Black, African, Black British or Caribbean (n = 20) | 2.6% | 15.0% | 50.0% | 35.0% |
| Asian (any Asian background) (n = 45) | 5.9% | 17.8% | 53.3% | 28.9% |
| Mixed or multiple ethnic groups (n = 14) | 1.8% | 41.3% | 50.0% | 35.7% |
| Other ethnicity (n = 11) | 1.5% | 27.3% | 54.5% | 18.2% |
| Not recorded (n = 104) | 13.7% | |||
| Smoking status | ||||
| Never smoked (n = 405) | 53.4% | 12.8% | 55.8% | 31.4% |
| Current regular smoker (n = 29) | 3.8% | 13.8% | 65.5% | 20.7% |
| Current occasional smoker (n = 28) | 3.7% | 7.1% | 75.0% | 17.9% |
| Ex-smoker (n = 185) | 24.4% | 5.4% | 61.6% | 33.0% |
| Not recorded (n = 112) | 14.8% | |||
| Change in employment status | ||||
| No change (n = 177) | 23.3% | 6.8% | 62.1% | 31.1% |
| Lost job (n = 29) | 3.8% | 10.3% | 51.7% | 37.9% |
| On reduced working hours (n = 107) | 14.1% | 12.1% | 60.7% | 27.1% |
| On sick leave (n = 146) | 19.2% | 8.9% | 58.2% | 32.9% |
| Had to retire or change job (n = 35) | 4.6% | 5.7% | 62.9% | 31.4% |
| Changes made to role or working arrangements (n = 167) | 22.0% | 15.0% | 47.3% | 37.7% |
| Not recorded (n = 98) | 12.9% | |||
| Other details | ||||
| Positive COVID-19 test | 30.8% | |||
| Mean days admitted to hospital (n = 78) (SD) | 12.9 (20.3) | 10.2 (10.9) | 12.3 (20.5) | 15.0 (22.3) |
| Mean symptom severity score at Assessment 1 (SD) | 17.5 (5.71) | 7.4 (1.84) | 15.8 (2.95) | 24.0 (2.33) |
| Mean functional disability score at Assessment 1 (SD) | 7.0 (3.81) | 2.4 (1.81) | 6.0 (3.04) | 10.2 (3.02) |
| Mean overall health score at Assessment 1 (SD) | 4.7 (1.89) | 6.4 (1.72) | 4.9 (1.75) | 3.74(1.67) |
| Mean duration of symptoms (days) (SD) | 408.8 (260.7) | 390.0 (233.6) | 381.9 (243.0) | 467.4 (292.9) |
| Mean interval between Assessments 1 and 2 (days) (SD) | 16.2 (17.6) | 17.8 (16.9) | 16.6 (17.3) | 14.8 (18.4) |
| Median interval between Assessments 1 and 2 (days) (range, min to max) | 12.5 (0 to 97) | 15.8 (0 to 84) | 13.8 (0 to 97) | 9.7 (0 to 94) |
| A1 Functional Disability Cluster | |||
|---|---|---|---|
| A1 Symptom Severity Cluster | Mild | Moderate | Severe |
| Mild | 0.22 | 0.10 | 0.00 |
| Moderate | 0.06 | 0.20 | 0.11 |
| Severe | 0.02 | 0.11 | 0.16 |
| A2 Functional Disability Cluster | |||
|---|---|---|---|
| A2 Symptom Severity Cluster | Mild | Moderate | Severe |
| Mild | 0.20 | 0.02 | 0.00 |
| Moderate | 0.19 | 0.22 | 0.04 |
| Severe | 0.03 | 0.12 | 0.17 |
| A2 Symptom Severity Cluster | |||
|---|---|---|---|
| A1 Symptom Severity Cluster | Mild | Medium | Severe |
| Mild | 0.14 | 0.14 | 0.05 |
| Moderate | 0.05 | 0.18 | 0.10 |
| Severe | 0.04 | 0.14 | 0.16 |
| A2 Functional Disability Cluster | |||
|---|---|---|---|
| A1 Functional Disability Cluster | Mild | Moderate | Severe |
| Mild | 0.17 | 0.09 | 0.04 |
| Moderate | 0.18 | 0.18 | 0.06 |
| Severe | 0.07 | 0.09 | 0.12 |
| A2 Overall Health Cluster | |||
|---|---|---|---|
| A1 Overall Health Cluster | Mild | Moderate | Severe |
| Mild | 0.04 | 0.05 | 0.01 |
| Moderate | 0.06 | 0.54 | 0.11 |
| Severe | 0.01 | 0.10 | 0.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sivan, M.; Smith, A.B.; Osborne, T.; Goodwin, M.; Lawrence, R.R.; Baley, S.; Williams, P.; Lee, C.; Davies, H.; Balasundaram, K.; et al. Long COVID Clinical Severity Types Based on Symptoms and Functional Disability: A Longitudinal Evaluation. J. Clin. Med. 2024, 13, 1908. https://doi.org/10.3390/jcm13071908
Sivan M, Smith AB, Osborne T, Goodwin M, Lawrence RR, Baley S, Williams P, Lee C, Davies H, Balasundaram K, et al. Long COVID Clinical Severity Types Based on Symptoms and Functional Disability: A Longitudinal Evaluation. Journal of Clinical Medicine. 2024; 13(7):1908. https://doi.org/10.3390/jcm13071908
Chicago/Turabian StyleSivan, Manoj, Adam B. Smith, Thomas Osborne, Madeline Goodwin, Román Rocha Lawrence, Sareeta Baley, Paul Williams, Cassie Lee, Helen Davies, Kumaran Balasundaram, and et al. 2024. "Long COVID Clinical Severity Types Based on Symptoms and Functional Disability: A Longitudinal Evaluation" Journal of Clinical Medicine 13, no. 7: 1908. https://doi.org/10.3390/jcm13071908
APA StyleSivan, M., Smith, A. B., Osborne, T., Goodwin, M., Lawrence, R. R., Baley, S., Williams, P., Lee, C., Davies, H., Balasundaram, K., & Greenwood, D. C., on behalf of the LOCOMOTION Consortium. (2024). Long COVID Clinical Severity Types Based on Symptoms and Functional Disability: A Longitudinal Evaluation. Journal of Clinical Medicine, 13(7), 1908. https://doi.org/10.3390/jcm13071908







