Measuring Cardiorespiratory Fitness without Exercise Testing: The Development and Validation of a New Tool for Spanish Adults
Abstract
1. Introduction
2. Materials and Method
2.1. Study Populations
2.2. Measurement of Indirect Maximum Oxygen Volume (VO2max) by Exercise-Test
2.3. Assessment of Leisure-Time Physical Activity
2.4. Anthropometry
2.5. Cardiovascular Risk Factors
2.6. Statistical Analysis
3. Results
3.1. Study Population
3.2. Prediction Function of VO2max
3.3. Concurrent Validity of the Function
3.4. Concordance Analysis
3.5. Construct Validity
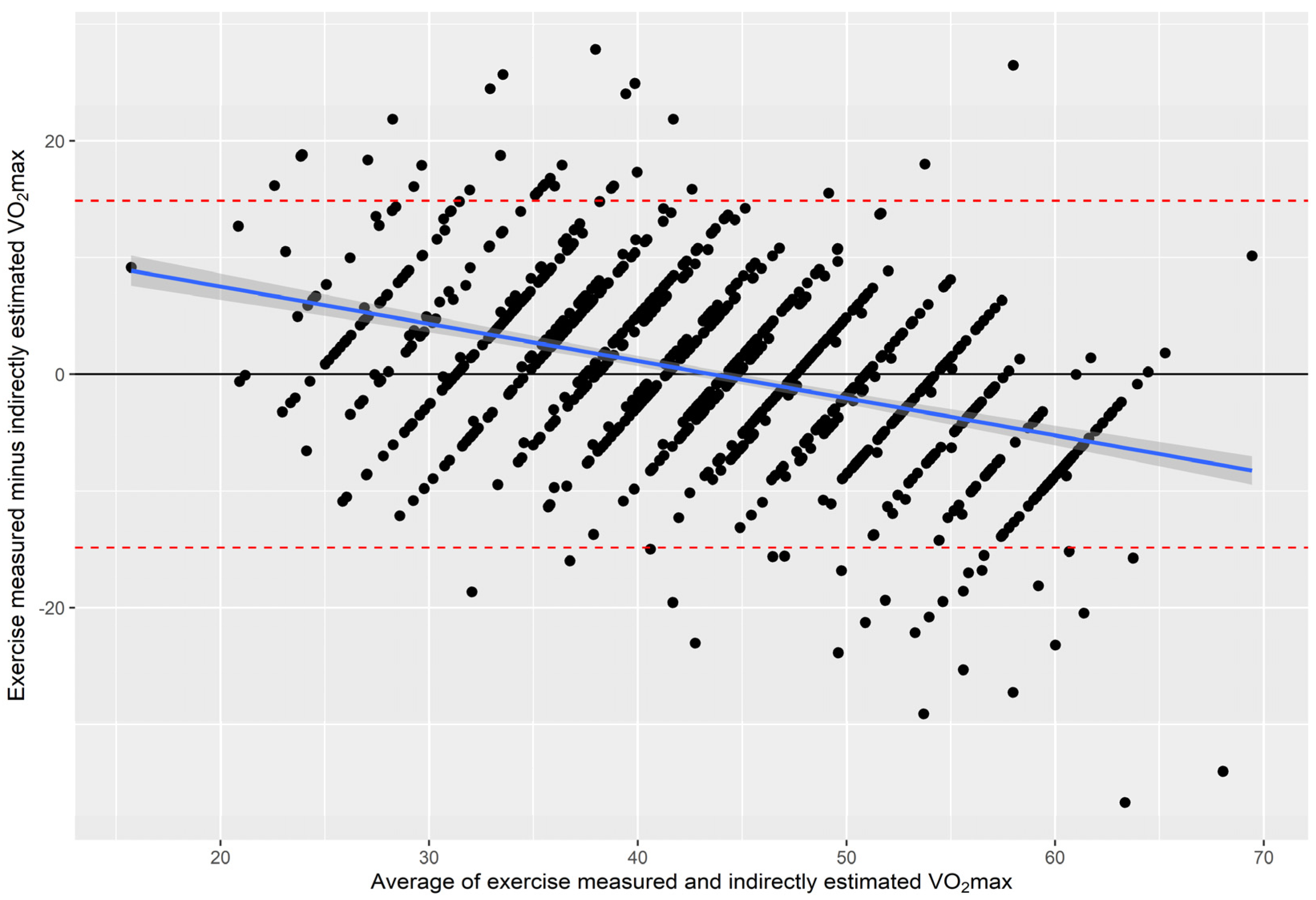
3.6. Agreement between Measured and Estimated VO2max
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Després, J.P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J.; et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement from the American Heart Association. Circulation 2016, 134, e653–e699. [Google Scholar] [CrossRef] [PubMed]
- Harber, M.P.; Kaminsky, L.A.; Arena, R.; Blair, S.N.; Franklin, B.A.; Myers, J.; Ross, R. Impact of Cardiorespiratory Fitness on All-Cause and Disease-Specific Mortality: Advances Since 2009. Prog. Cardiovasc. Dis. 2017, 60, 11–20. [Google Scholar] [CrossRef]
- Kokkinos, P.; Faselis, C.; Samuel, I.B.H.; Pittaras, A.; Doumas, M.; Murphy, R.; Heimall, M.S.; Sui, X.; Zhang, J.; Myers, J. Cardiorespiratory Fitness and Mortality Risk Across the Spectra of Age, Race, and Sex. J. Am. Coll. Cardiol. 2022, 80, 598–609. [Google Scholar] [CrossRef] [PubMed]
- Han, M.; Qie, R.; Shi, X.; Yang, Y.; Lu, J.; Hu, F.; Zhang, M.; Zhang, Z.; Hu, D.; Zhao, Y. Cardiorespiratory Fitness and Mortality from All Causes, Cardiovascular Disease and Cancer: Dose-Response Meta-Analysis of Cohort Studies. Br. J. Sports Med. 2022, 56, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Laukkanen, J.A.; Isiozor, N.M.; Kunutsor, S.K. Objectively Assessed Cardiorespiratory Fitness and All-Cause Mortality Risk: An Updated Meta-Analysis of 37 Cohort Studies Involving 2,258,029 Participants. Mayo Clin. Proc. 2022, 97, 1054–1073. [Google Scholar] [CrossRef]
- Bradshaw, D.I.; George, J.D.; Hyde, A.; LaMonte, M.J.; Vehrs, P.R.; Hager, R.L.; Yanowitz, F.G. An Accurate VO2max Nonexercise Regression Model for 18-65-Year-Old Adults. Res. Q. Exerc. Sport 2005, 76, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Jurca, R.; Jackson, A.S.; LaMonte, M.J.; Morrow, J.R.; Blair, S.N.; Wareham, N.J.; Haskell, W.L.; Van Mechelen, W.; Church, T.S.; Jakicic, J.M.; et al. Assessing Cardiorespiratory Fitness without Performing Exercise Testing. Am. J. Prev. Med. 2005, 29, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chen, S.; Lavie, C.J.; Zhang, J.; Sui, X. An Overview of Non-Exercise Estimated Cardiorespiratory Fitness: Estimation Equations, Cross-Validation and Application. J. Sci. Sport Exerc. 2019, 1, 38–53. [Google Scholar] [CrossRef]
- Peterman, J.E.; Harber, M.P.; Imboden, M.T.; Whaley, M.H.; Fleenor, B.S.; Myers, J.; Arena, R.; Finch, W.H.; Kaminsky, L.A. Accuracy of Nonexercise Prediction Equations for Assessing Longitudinal Changes to Cardiorespiratory Fitness in Apparently Healthy Adults: Ball St Cohort. J. Am. Heart Assoc. 2020, 9, e015117. [Google Scholar] [CrossRef]
- Marrugat, J.; Elosua, R.; Covas, M.I.; Molina, L.; Rubiés-Prat, J. Amount and Intensity of Physical Activity, Physical Fitness, and Serum Lipids in Men. The MARATHOM Investigators. Am. J. Epidemiol. 1996, 143, 562–569. [Google Scholar] [CrossRef]
- Elosua, R.; Garcia, M.; Aguilar, A.; Molina, L.; Covas, M.I.; Marrugat, J. Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish Women. Med. Sci. Sports Exerc. 2000, 32, 1431–1437. [Google Scholar] [CrossRef]
- Bruce, R.A. Exercise Testing of Patients with Coronary Heart Disease. Principles and Normal Standards for Evaluation. Ann. Clin. Res. 1971, 3, 323–332. [Google Scholar] [PubMed]
- Bruce, R.; Kusumi, F.; Hosmer, D. Fundamentals of Clinical Cardiology and Recognition. Fundam. Clin. Cardiol. 1974, 88, 372–379. [Google Scholar]
- Elosua, R.; Marrugat, J.; Molina, L.; Pons, S.; Pujol, E. Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish Men. Am. J. Epidemiol. 1994, 139, 1197–1209. [Google Scholar] [CrossRef]
- Molina, L.; Sarmiento, M.; Peñafiel, J.; Donaire, D.; Garcia-Aymerich, J.; Gomez, M.; Ble, M.; Ruiz, S.; Frances, A.; Schröder, H.; et al. Validation of the Regicor Short Physical Activity Questionnaire for the Adult Population. PLoS ONE 2017, 12, e0168148. [Google Scholar] [CrossRef]
- Lin, L.I. A Concordance Correlation Coefficient to Evaluate Reproducibility. Biometrics 1989, 45, 255–268. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G.; Bland, J.M. Measurement in Medicine: The Analysis of Method Comparison Studies. J. R. Stat. Soc. 1983, 32, 307. [Google Scholar] [CrossRef]
- Nes, B.M.; Janszky, I.; Vatten, L.J.; Nilsen, T.I.L.; Aspenes, S.T.; Wisløff, U. Estimating V·O2peak from a Nonexercise Prediction Model: The HUNT Study, Norway. Med. Sci. Sports Exerc. 2011, 43, 2024–2030. [Google Scholar] [CrossRef]
- Laukkanen, J.A.; Kurl, S.; Salonen, R.; Rauramaa, R.; Salonen, J.T. The Predictive Value of Cardiorespiratory Fitness for Cardiovascular Events in Men with Various Risk Profiles: A Prospective Population-Based Cohort Study. Eur. Heart J. 2004, 25, 1428–1437. [Google Scholar] [CrossRef]
- O’Donovan, G.; Bakrania, K.; Ghouri, N.; Yates, T.; Gray, L.J.; Hamer, M.; Stamatakis, E.; Khunti, K.; Davies, M.; Sattar, N.; et al. Nonexercise Equations to Estimate Fitness in White European and South Asian Men. Med. Sci. Sports Exerc. 2016, 48, 854–859. [Google Scholar] [CrossRef]
- Zeiher, J.; Ombrellaro, K.J.; Perumal, N.; Keil, T.; Mensink, G.B.M.; Finger, J.D. Correlates and Determinants of Cardiorespiratory Fitness in Adults: A Systematic Review. Sport Med. Open 2019, 5, 39. [Google Scholar] [CrossRef] [PubMed]
- Peterman, J.E.; Whaley, M.H.; Harber, M.P.; Fleenor, B.S.; Imboden, M.T.; Myers, J.; Arena, R.; Kaminsky, L.A. Comparison of Non-Exercise Cardiorespiratory Fitness Prediction Equations in Apparently Healthy Adults. Eur. J. Prev. Cardiol. 2021, 28, 142–148. [Google Scholar] [CrossRef]
- Peterman, J.E.; Harber, M.P.; Imboden, M.T.; Whaley, M.H.; Fleenor, B.S.; Myers, J.; Arena, R.; Kaminsky, L.A. Accuracy of Exercise-Based Equations for Estimating Cardiorespiratory Fitness. Med. Sci. Sports Exerc. 2021, 53, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Evans, H.J.L.; Ferrar, K.E.; Smith, A.E.; Parfitt, G.; Eston, R.G. A Systematic Review of Methods to Predict Maximal Oxygen Uptake from Submaximal, Open Circuit Spirometry in Healthy Adults. J. Sci. Med. Sport 2015, 18, 183–188. [Google Scholar] [CrossRef]
- Jang, W.Y.; Kang, D.O.; Park, Y.; Lee, J.; Kim, W.; Choi, J.Y.; Roh, S.Y.; Jang, Y.; Park, S.H.; Kim, W.S.; et al. Validation of FRIEND and ACSM Equations for Cardiorespiratory Fitness: Comparison to Direct Measurement in CAD Patients. J. Clin. Med. 2020, 9, 1889. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.; Myers, J. Cardiorespiratory Fitness and Its Place in Medicine. Rev. Cardiovasc. Med. 2023, 24, 14. [Google Scholar] [CrossRef]
- Mailey, E.L.; White, S.M.; Wójcicki, T.R.; Szabo, A.N.; Kramer, A.F.; McAuley, E. Construct Validation of a Non-Exercise Measure of Cardiorespiratory Fitness in Older Adults. BMC Public Health 2010, 10, 59. [Google Scholar] [CrossRef]
- Pollock, M.L.; Foster, C.; Schmidt, D.; Hellman, C.; Linnerud, A.C.; Ward, A. Comparative analysis of physiologic responses to three different maximal graded exercise test protocols in healthy women. Am. Heart J. 1982, 103, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Storer, T.W.; Davis, J.A.; Caiozzo, V.J. Accurate Prediction of VO2max in Cycle Ergometry. Med. Sci. Sports Exerc. 1990, 22, 704–712. [Google Scholar] [CrossRef]
- Bruce, R.A.; Kusumi, F.; Hosmer, D. Maximal Oxygen Intake and Nomographic Assessment of Functional Aerobic Impairment in Cardiovascular Disease. Am. Heart J. 1973, 85, 546–562. [Google Scholar] [CrossRef] [PubMed]
| Men n = 569 | Women n = 478 | |
|---|---|---|
| Age (years) | 40.1 (9.0) | 39.6 (11.0) |
| Baseline Heart Rate (bpm) | 69.5 (13.4) | 74.6 (13.2) |
| Body mass index (kg/m2) | 24.7 (3.05) | 24.0 (3.59) |
| Moderate-vigorous Physical Activity (METs/min/d) | 192 [41.1; 398] * | 208 [89.6; 414] * |
| VO2max (mL/kg/min) | 48.0 (10.7) | 38.3 (10.3) |
| eVO2max (mL/kg/min) | 48.0 (6.83) | 38.3 (7.70) |
| Glucose (mg/dL) | 86.7 (15.0) | 94.5 (10.1) |
| Total cholesterol (mg/dL) | 208 (38.9) | 200 (37.7) |
| C-HDL (mg/dL) | 49.1 (12.5) | 59.6 (13.6) |
| C-LDL (mg/dL) | 138 (37.1) | 127 (34.6) |
| Triglycerides (mg/dL) | 88.0 (64.0; 120) | 63.0 (51.0; 83.0) |
| β Coefficient | 95% CI | p Value | |
|---|---|---|---|
| Validation sample | |||
| Intercept | 103.815 | ||
| Sex (1 = men; 2 = women) | −10.400 | −11.360; −9.440 | <0.001 |
| Age (years) | −0.261 | −0.311; −0.211 | <0.001 |
| Resting heart rate (bpm) | −0.163 | −0.199; −0.127 | <0.001 |
| BMI (kg/m2) | −1.056 | −1.211; −0.902 | <0.001 |
| MVPA (METs/min/d) | 0.010 | 0.008; 0.012 | <0.001 |
| Model performance by sex and age groups | R2 | SEE | %SEE |
| All (n = 1047) | 0.57 | 7.59 | 17.4 |
| Men (n = 569) | 0.55 | 7.18 | 15.0 |
| Women (n = 478) | 0.41 | 7.91 | 20.6 |
| 17–31 y (n = 223) | 0.47 | 7.11 | 14.8 |
| 32–49 y (n = 616) | 0.53 | 7.62 | 17.1 |
| ≥50 y (n = 202) | 0.50 | 7.87 | 22.2 |
| Cross-validation by the leave-one-out method | R2 | SEE | %SEE |
| All (n = 1047) | 0.56 | 7.65 | 17.6 |
| Men (n = 569) | 0.54 | 7.23 | 15.1 |
| Women (n = 478) | 0.40 | 7.97 | 20.8 |
| 17–31 y (n = 223) | 0.45 | 7.20 | 15.0 |
| 32–49 y (n = 616) | 0.52 | 7.67 | 17.2 |
| ≥50 y (n = 202) | 0.49 | 7.93 | 22.2 |
| All (n = 1047) | Men (n = 569) | Women (n = 478) | 17 to 31 Years (n = 223) | 32 to 49 Years (n = 616) | ≥50 Years (n = 202) | |
|---|---|---|---|---|---|---|
| Mean, VO2max, mL/kg/min (SD) | ||||||
| 43.56 (11.6) | 47.99 (10.66) | 38.29 (10.30) | 47.95 (9.71) | 44.63 (11.07) | 35.68 (11.33) |
| 43.59 (8.7) | 48.03 (6.83) | 38.32 (7.70) | 48.78 (7.11) | 44.06 (7.91) | 36.67 (8.08) |
| Difference of means, (95% CI) 1 | −0.03 (−0.49; 0.43) | −0.03 (−0.63; 0.56) | −0.03 (−0.75; 0.68) | −0.83 (−1.77; 0.11) | 0.58 (−0.03; 1.18) | −0.99 (−2.06; 0.08) |
| Pearson correlation coefficient | 0.75 | 0.74 | 0.64 | 0.68 | 0.73 | 0.71 |
| Lin’s CCC | 0.72 | 0.67 | 0.62 | 0.65 | 0.69 | 0.67 |
| Correct classification 2, (%) | 64.3 | 66.6 | 61.5 | 62.7 | 61.9 | 73.1 |
| Gross misclassification 2 (%) | 2.7 | 2.6 | 2.7 | 1.3 | 3.6 | 1.4 |
| Measured CRF | |||
|---|---|---|---|
| Low | Medium | High | |
| Predicted CRF | |||
| All (n = 1047) | |||
| Low (mean = 33.8 ± 4.8 VO2/kg/min) | 69.9 | 25.4 | 4.8 |
| Medium (mean = 43.8 ± 2.2 VO2/kg/min) | 24.6 | 49.9 | 25.3 |
| High (mean = 52.9 ± 4.0 VO2/kg/min) | 3.2 | 23.3 | 73.5 |
| Men (n = 569) | |||
| Low (mean = 36.4 ± 3.5 VO2/kg/min) | 43.7 | 46.0 | 10.3 |
| Medium (mean = 44.2 ± 2.2 VO2/kg/min) | 7.3 | 54.8 | 37.9 |
| High (mean = 53.1 ± 3.9 VO2/kg/min) | 0.8 | 13.9 | 85.3 |
| Women (n = 478) | |||
| Low (mean = 33.1 ± 4.8 VO2/kg/min) | 84.3 | 14.0 | 1.7 |
| Medium (mean = 43.4 ± 2.2 VO2/kg/min) | 42.0 | 44.9 | 13.1 |
| High (mean = 51.8 ± 4.3 VO2/kg/min) | 12.3 | 57.5 | 30.1 |
| 17–31 y (n = 223) | |||
| Low (mean = 36.9 ± 2.4 VO2/kg/min) | 35.7 | 57.1 | 7.1 |
| Medium (mean = 43.7 ± 2.3 VO2/kg/min) | 7.3 | 52.2 | 40.6 |
| High (mean = 54.1 ± 4.7 VO2/kg/min) | 1.0 | 18.2 | 80.8 |
| 31–50 y (n = 688) | |||
| Low (mean = 34.8 ± 4.3 VO2/kg/min) | 63.8 | 28.7 | 7.4 |
| Medium (mean = 44.0 ± 2.2 VO2/kg/min) | 31.4 | 48.6 | 20.0 |
| High (mean = 52.4 ± 3.4 VO2/kg/min) | 3.7 | 23.4 | 72.9 |
| >50 y (n = 190) | |||
| Low (mean = 31.9 ± 5.0 VO2/kg/min) | 84.9 | 14.4 | 0.7 |
| Medium (mean = 43.2 ± 2.1 VO2/kg/min) | 29.8 | 51.1 | 19.1 |
| High (mean = 51.1 ± 3.2 VO2/kg/min) | 9.0 | 45.5 | 45.5 |
| Tertiles of VO2max Non-Exercise eCRF (mL/kg/min) | ||||
|---|---|---|---|---|
| Low (n = 329) | Medium (n = 312) | High (n = 294) | p Linear Trend | |
| VO2max (mL/kg/min) * | 33.7 (20.3–39.8) | 43.8 (39.9–47.3) | 52.7 (47.4–66.2) | <0.001 |
| Total cholesterol (mg/dL) | 208 (204; 212) | 207 (203; 211) | 198 (194; 202) | 0.003 |
| LDL-Cholesterol (mg/dL) | 136 (132; 140) | 135 (131; 138) | 126 (122; 1309 | 0.003 |
| HDL-Cholesterol (mg/dL) | 50.7 (49.2; 52.2) | 53.6 (52.2; 55.1) | 59.0 (57.4; 60.6) | <0.001 |
| Total cholesterol:HDL-cholesterol ratio | 4.5 (4.3; 4.6) | 4.1 (4.0; 4.3) | 3.4 (3.3; 3.6) | <0.001 |
| Triglycerides:HDL-cholesterol ratio | 2.5 (2.3; 2.7) | 2.0 (1.8; 2.2) | 1.1 (0.9; 1.3) | <0.001 |
| Triglycerides (mg/dL) | 107 (101; 113) | 91.8 (86.4; 97.2) | 64.2 (58.3; 70.1) | <0.001 |
| Fasting blood glucose (mg/dL) | 90.7 (89.2; 92.2) | 89.1 (90.2; 93.4) | 91.8 (90.3; 93.4) | 0.355 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schröder, H.; Subirana, I.; Elosua, R.; Camps-Vilaró, A.; Tizón-Marcos, H.; Fitó, M.; Gómez, S.F.; Dégano, I.R.; Marrugat, J. Measuring Cardiorespiratory Fitness without Exercise Testing: The Development and Validation of a New Tool for Spanish Adults. J. Clin. Med. 2024, 13, 2210. https://doi.org/10.3390/jcm13082210
Schröder H, Subirana I, Elosua R, Camps-Vilaró A, Tizón-Marcos H, Fitó M, Gómez SF, Dégano IR, Marrugat J. Measuring Cardiorespiratory Fitness without Exercise Testing: The Development and Validation of a New Tool for Spanish Adults. Journal of Clinical Medicine. 2024; 13(8):2210. https://doi.org/10.3390/jcm13082210
Chicago/Turabian StyleSchröder, Helmut, Isaac Subirana, Roberto Elosua, Anna Camps-Vilaró, Helena Tizón-Marcos, Montserrat Fitó, Santiago F. Gómez, Irene R. Dégano, and Jaume Marrugat. 2024. "Measuring Cardiorespiratory Fitness without Exercise Testing: The Development and Validation of a New Tool for Spanish Adults" Journal of Clinical Medicine 13, no. 8: 2210. https://doi.org/10.3390/jcm13082210
APA StyleSchröder, H., Subirana, I., Elosua, R., Camps-Vilaró, A., Tizón-Marcos, H., Fitó, M., Gómez, S. F., Dégano, I. R., & Marrugat, J. (2024). Measuring Cardiorespiratory Fitness without Exercise Testing: The Development and Validation of a New Tool for Spanish Adults. Journal of Clinical Medicine, 13(8), 2210. https://doi.org/10.3390/jcm13082210







