Antiplatelet Therapy and Anticoagulation before, during, and after Acute Coronary Syndrome
Abstract
:1. Acute Antithrombotic Therapy in Acute Coronary Syndrome
1.1. Choice of Antiplatelet Therapy
1.2. Pre-Treatment with P2Y12 Inhibitors
1.3. Anticoagulant Therapy in the Acute Setting (Figure 2)

1.4. Parenteral Antiplatelet Therapy
2. Long-Term Antithrombotic Therapy in Acute Coronary Syndrome
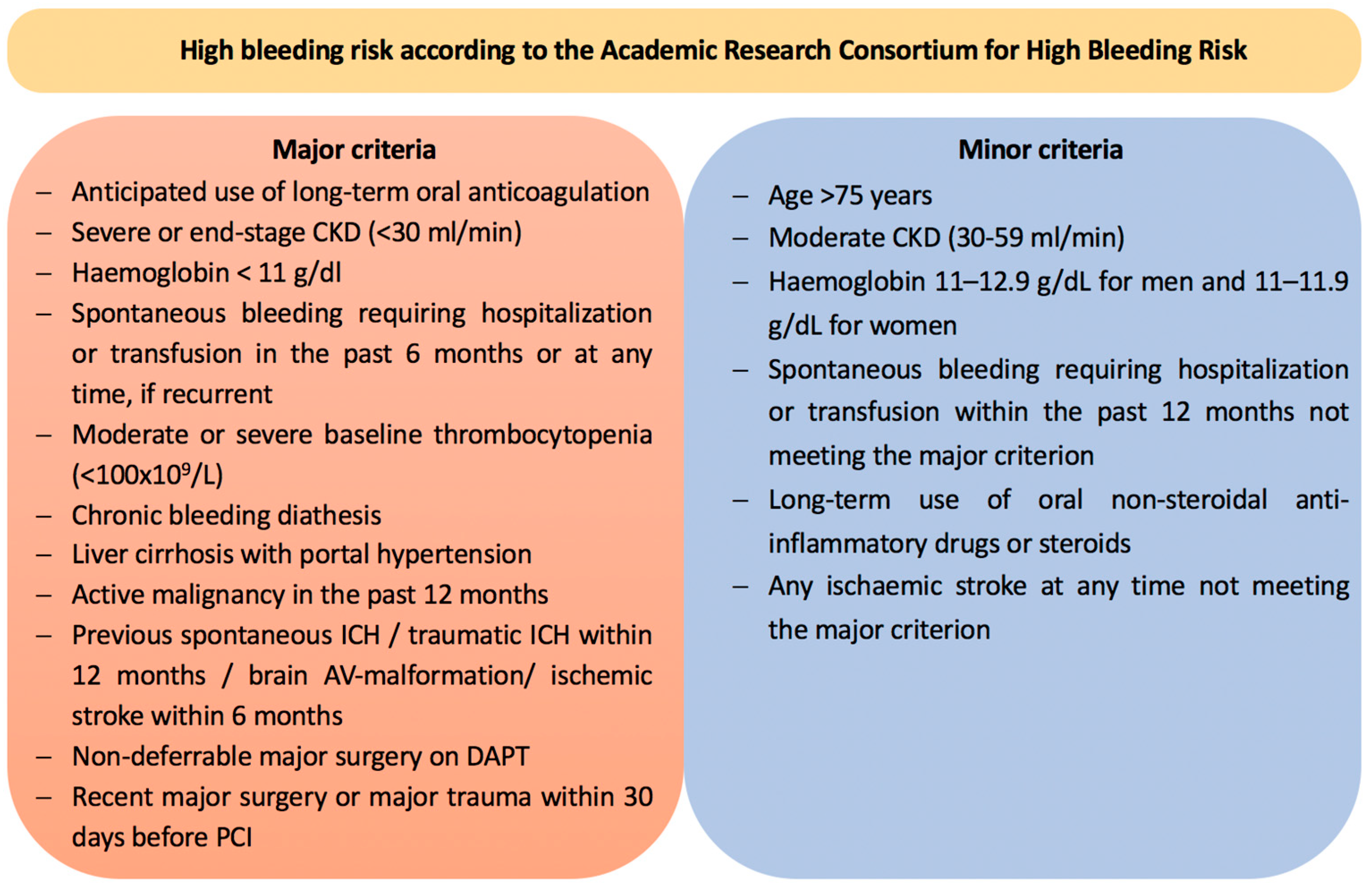
2.1. Shortening the Duration of Dual Antiplatelet Therapy
2.2. De-Escalation of Dual Antiplatelet Therapy
2.3. Prolonging Dual Antiplatelet Therapy
2.4. ACS Patients with an Indication for Long-Term Anticoagulation
3. Conclusions
Funding
Conflicts of Interest
References
- Layne, K.; Ferro, A. Antiplatelet Therapy in Acute Coronary Syndrome. Eur. Cardiol. 2017, 12, 33–37. [Google Scholar] [CrossRef]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef]
- Wallentin, L.; Becker, R.C.; Budaj, A.; Cannon, C.P.; Emanuelsson, H.; Held, C.; Horrow, J.; Husted, S.; James, S.; Katus, H.; et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N. Engl. J. Med. 2009, 361, 1045–1057. [Google Scholar] [CrossRef]
- Wiviott, S.D.; Braunwald, E.; McCabe, C.H.; Montalescot, G.; Ruzyllo, W.; Gottlieb, S.; Neumann, F.-J.; Ardissino, D.; De Servi, S.; Murphy, S.A.; et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N. Engl. J. Med. 2007, 357, 2001–2015. [Google Scholar] [CrossRef] [PubMed]
- Schüpke, S.; Neumann, F.-J.; Menichelli, M.; Mayer, K.; Bernlochner, I.; Wöhrle, J.; Richardt, G.; Liebetrau, C.; Witzenbichler, B.; Antoniucci, D.; et al. Ticagrelor or Prasugrel in Patients with Acute Coronary Syndromes. N. Engl. J. Med. 2019, 381, 1524–1534. [Google Scholar] [CrossRef] [PubMed]
- Crea, F.; Thiele, H.; Sibbing, D.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. Debate: Prasugrel rather than ticagrelor is the preferred treatment for NSTE-ACS patients who proceed to PCI and pretreatment should not be performed in patients planned for an early invasive strategy. Eur. Heart J. 2021, 42, 2973–2985. [Google Scholar] [CrossRef]
- Montalescot, G.; Bolognese, L.; Dudek, D.; Goldstein, P.; Hamm, C.; Tanguay, J.-F.; Berg JM ten Miller, D.L.; Costigan, T.M.; Goedicke, J.; Silvain, J.; et al. Pretreatment with prasugrel in non-ST-segment elevation acute coronary syndromes. N. Engl. J. Med. 2013, 369, 999–1010. [Google Scholar] [CrossRef]
- Tarantini, G.; Mojoli, M.; Varbella, F.; Caporale, R.; Rigattieri, S.; Andò, G.; Cirillo, P.; Pierini, S.; Santarelli, A.; Sganzerla, P.; et al. Timing of Oral P2Y12 Inhibitor Administration in Patients With Non-ST-Segment Elevation Acute Coronary Syndrome. J. Am. Coll. Cardiol. 2020, 76, 2450–2459. [Google Scholar] [CrossRef] [PubMed]
- Bellemain-Appaix, A.; O’Connor, S.A.; Silvain, J.; Cucherat, M.; Beygui, F.; Barthélémy, O.; Collet, J.-P.; Jacq, L.; Bernasconi, F.; Montalescot, G.; et al. Association of clopidogrel pretreatment with mortality, cardiovascular events, and major bleeding among patients undergoing percutaneous coronary intervention: A systematic review and meta-analysis. JAMA 2012, 308, 2507–2516. [Google Scholar] [CrossRef]
- Montalescot, G.; Hof, A.W.; van’t Lapostolle, F.; Silvain, J.; Lassen, J.F.; Bolognese, L.; Cantor, W.J.; Cequier, Á.; Chettibi, M.; Goodman, S.G.; et al. Prehospital Ticagrelor in ST-Segment Elevation Myocardial Infarction. N. Engl. J. Med. 2014, 371, 1016–1027. [Google Scholar] [CrossRef]
- Mehran, R.; Baber, U.; Sharma, S.K.; Cohen, D.J.; Angiolillo, D.J.; Briguori, C.; Cha, J.Y.; Collier, T.; Dangas, G.; Dudek, D.; et al. Ticagrelor with or without Aspirin in High-Risk Patients after PCI. N. Engl. J. Med. 2019, 381, 2032–2042. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.-K.; Hong, S.-J.; Cho, Y.-H.; Yun, K.H.; Kim, Y.H.; Suh, Y.; Cho, J.Y.; Her, A.-Y.; Cho, S.; Jeon, D.W.; et al. Effect of Ticagrelor Monotherapy vs Ticagrelor With Aspirin on Major Bleeding and Cardiovascular Events in Patients With Acute Coronary Syndrome: The TICO Randomized Clinical Trial. JAMA 2020, 323, 2407–2416. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, H.; Domei, T.; Morimoto, T.; Natsuaki, M.; Shiomi, H.; Toyota, T.; Ohya, M.; Suwa, S.; Takagi, K.; Nanasato, M.; et al. Effect of 1-Month Dual Antiplatelet Therapy Followed by Clopidogrel vs 12-Month Dual Antiplatelet Therapy on Cardiovascular and Bleeding Events in Patients Receiving PCI: The STOPDAPT-2 Randomized Clinical Trial. JAMA 2019, 321, 2414–2427. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, H.; Morimoto, T.; Natsuaki, M.; Yamamoto, K.; Obayashi, Y.; Ogita, M.; Suwa, S.; Isawa, T.; Domei, T.; Yamaji, K.; et al. Comparison of Clopidogrel Monotherapy After 1 to 2 Months of Dual Antiplatelet Therapy With 12 Months of Dual Antiplatelet Therapy in Patients With Acute Coronary Syndrome: The STOPDAPT-2 ACS Randomized Clinical Trial. JAMA Cardiol. 2022, 7, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Valgimigli, M.; Frigoli, E.; Heg, D.; Tijssen, J.; Jüni, P.; Vranckx, P.; Ozaki, Y.; Morice, M.-C.; Chevalier, B.; Onuma, Y.; et al. Dual Antiplatelet Therapy after PCI in Patients at High Bleeding Risk. N. Engl. J. Med. 2021, 385, 1643–1655. [Google Scholar] [CrossRef] [PubMed]
- Sibbing, D.; Aradi, D.; Jacobshagen, C.; Gross, L.; Trenk, D.; Geisler, T.; Orban, M.; Hadamitzky, M.; Merkely, B.; Kiss, R.G.; et al. Guided de-escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL-ACS): A randomised, open-label, multicentre trial. Lancet 2017, 390, 1747–1757. [Google Scholar] [CrossRef] [PubMed]
- Claassens, D.M.F.; Vos, G.J.A.; Bergmeijer, T.O.; Hermanides, R.S.; Hof, A.W.J.; van’t der Harst, P.; van der Barbato, E.; Morisco, C.; Tjon Joe Gin, R.M.; Asselbergs, F.W.; et al. A Genotype-Guided Strategy for Oral P2Y12 Inhibitors in Primary PCI. N. Engl. J. Med. 2019, 381, 1621–1631. [Google Scholar] [CrossRef] [PubMed]
- Cuisset, T.; Deharo, P.; Quilici, J.; Johnson, T.W.; Deffarges, S.; Bassez, C.; Bonnet, G.; Fourcade, L.; Mouret, J.P.; Lambert, M.; et al. Benefit of switching dual antiplatelet therapy after acute coronary syndrome: The TOPIC (timing of platelet inhibition after acute coronary syndrome) randomized study. Eur. Heart J. 2017, 38, 3070–3078. [Google Scholar] [CrossRef]
- Kim, C.J.; Park, M.-W.; Kim, M.C.; Choo, E.-H.; Hwang, B.-H.; Lee, K.Y.; Choi, Y.S.; Kim, H.-Y.; Yoo, K.-D.; Jeon, D.-S.; et al. Unguided de-escalation from ticagrelor to clopidogrel in stabilised patients with acute myocardial infarction undergoing percutaneous coronary intervention (TALOS-AMI): An investigator-initiated, open-label, multicentre, non-inferiority, randomised trial. Lancet 2021, 398, 1305–1316. [Google Scholar] [CrossRef]
- Gibson, C.M.; Mehran, R.; Bode, C.; Halperin, J.; Verheugt, F.W.; Wildgoose, P.; Birmingham, M.; Ianus, J.; Burton, P.; Eickels M van Korjian, S.; et al. Prevention of Bleeding in Patients with Atrial Fibrillation Undergoing PCI. N. Engl. J. Med. 2016, 375, 2423–2434. [Google Scholar] [CrossRef]
- Cannon, C.P.; Lip, G.Y.H.; Oldgren, J. Dual Antithrombotic Therapy with Dabigatran after PCI in Atrial Fibrillation. N. Engl. J. Med. 2018, 378, 485–486. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.D.; Heizer, G.; Aronson, R.; Vora, A.N.; Massaro, T.; Mehran, R.; Goodman, S.G.; Windecker, S.; Darius, H.; Li, J.; et al. Antithrombotic Therapy after Acute Coronary Syndrome or PCI in Atrial Fibrillation. N. Engl. J. Med. 2019, 380, 1509–1524. [Google Scholar] [CrossRef] [PubMed]
- Vranckx, P.; Valgimigli, M.; Eckardt, L.; Tijssen, J.; Lewalter, T.; Gargiulo, G.; Batushkin, V.; Campo, G.; Lysak, Z.; Vakaliuk, I.; et al. Edoxaban-based versus vitamin K antagonist-based antithrombotic regimen after successful coronary stenting in patients with atrial fibrillation (ENTRUST-AF PCI): A randomised, open-label, phase 3b trial. Lancet 2019, 394, 1335–13343. [Google Scholar] [CrossRef] [PubMed]
- Koul, S.; Smith, J.G.; Götberg, M.; Omerovic, E.; Alfredsson, J.; Venetsanos, D.; Persson, J.; Jensen, J.; Lagerqvist, B.; Redfors, B.; et al. No Benefit of Ticagrelor Pretreatment Compared With Treatment During Percutaneous Coronary Intervention in Patients With ST-Segment-Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Circ. Cardiovasc. Interv. 2018, 11, e005528. [Google Scholar] [CrossRef] [PubMed]
- Rohla, M.; Ye, S.X.; Shibutani, H.; Bruno, J.; Otsuka, T.; Häner, J.D.; Bär, S.; Temperli, F.; Kavaliauskaite, R.; Lanz, J.; et al. Pretreatment With P2Y12 Inhibitors in ST-Segment Elevation Myocardial Infarction: Insights From the Bern-PCI Registry. JACC Cardiovasc. Interv. 2024, 17, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Idorsia Pharmaceuticals Ltd. Multi-Center, Double-Blind, Randomized, Placebo-Controlled, Parallel-Group Study to Evaluate the Efficacy and Safety of Self-Administered Subcutaneous Selatogrel for Prevention of All-Cause Death and Treatment of Acute Myocardial Infarction in Subjects with a Recent History of Acute Myocardial Infarction; Idorsia Pharmaceuticals Ltd.: Allschwil, Switzerland, 2016. [Google Scholar]
- Albuquerque, F.; Gomes, D.A.; Ferreira, J.; de Araújo Gonçalves, P.; Lopes, P.M.; Presume, J.; Teles, R.C.; de Sousa Almeida, M. Upstream anticoagulation in patients with ST-segment elevation myocardial infarction: A systematic review and meta-analysis. Clin. Res. Cardiol. 2023, 112, 1322–1330. [Google Scholar] [CrossRef] [PubMed]
- Montalescot, G.; Zeymer, U.; Silvain, J.; Boulanger, B.; Cohen, M.; Goldstein, P.; Ecollan, P.; Combes, X.; Huber, K.; Pollack, C.; et al. Intravenous enoxaparin or unfractionated heparin in primary percutaneous coronary intervention for ST-elevation myocardial infarction: The international randomised open-label ATOLL trial. Lancet 2011, 378, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liang, Z.; Qin, L.; Wang, M.; Wang, X.; Zhang, H.; Liu, Y.; Li, Y.; Jia, Z.; Liu, L.; et al. Bivalirudin plus a high-dose infusion versus heparin monotherapy in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: A randomised trial. Lancet 2022, 400, 1847–1857. [Google Scholar] [CrossRef] [PubMed]
- Oldgren, J.; Wallentin, L.; Afzal, R.; Bassand, J.-P.; Budaj, A.; Chrolavicius, S.; Fox, K.A.A.; Granger, C.B.; Mehta, S.R.; Pais, P.; et al. Effects of fondaparinux in patients with ST-segment elevation acute myocardial infarction not receiving reperfusion treatment. Eur. Heart J. 2008, 29, 315–323. [Google Scholar] [CrossRef]
- Fifth Organization to Assess Strategies in Acute Ischemic Syndromes Investigators; Yusuf, S.; Mehta, S.R.; Chrolavicius, S.; Afzal, R.; Pogue, J.; Granger, C.B.; Budaj, A.; Peters, R.J.G.; Bassand, J.-P.; et al. Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N. Engl. J. Med. 2006, 354, 1464–1476. [Google Scholar]
- Boersma, E.; Harrington, R.A.; Moliterno, D.J.; White, H.; Théroux, P.; Van de Werf, F.; Torbal A de Armstrong, P.W.; Wallentin, L.C.; Wilcox, R.G.; Simes, J.; et al. Platelet glycoprotein IIb/IIIa inhibitors in acute coronary syndromes: A meta-analysis of all major randomised clinical trials. Lancet 2002, 359, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Storey, R.F.; Sanderson, H.M.; White, A.E.; May, J.A.; Cameron, K.E.; Heptinstall, S. The central role of the P(2T) receptor in amplification of human platelet activation, aggregation, secretion and procoagulant activity. Br. J. Haematol. 2000, 110, 925–934. [Google Scholar] [CrossRef]
- Harrington, R.A.; Stone, G.W.; McNulty, S.; White, H.D.; Lincoff, A.M.; Gibson, C.M.; Pollack, C.V.; Montalescot, G.; Mahaffey, K.W.; Kleiman, N.S.; et al. Platelet inhibition with cangrelor in patients undergoing PCI. N. Engl. J. Med. 2009, 361, 2318–2329. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Lincoff, A.M.; Gibson, C.M.; Stone, G.W.; McNulty, S.; Montalescot, G.; Kleiman, N.S.; Goodman, S.G.; White, H.D.; Mahaffey, K.W.; et al. Intravenous platelet blockade with cangrelor during PCI. N. Engl. J. Med. 2009, 361, 2330–2341. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, D.L.; Stone, G.W.; Mahaffey, K.W.; Gibson, C.M.; Steg, P.G.; Hamm, C.W.; Price, M.J.; Leonardi, S.; Gallup, D.; Bramucci, E.; et al. Effect of platelet inhibition with cangrelor during PCI on ischemic events. N. Engl. J. Med. 2013, 368, 1303–1313. [Google Scholar] [CrossRef] [PubMed]
- Sardar, P.; Nairooz, R.; Chatterjee, S.; Mushiyev, S.; Pekler, G.; Visco, F. Cangrelor for patients undergoing percutaneous coronary intervention: Evidence from a meta-analysis of randomized trials. J. Thromb. Thrombolysis 2014, 38, 1–10. [Google Scholar] [CrossRef]
- Vogel, B.; Baber, U.; Cohen, D.J.; Sartori, S.; Sharma, S.K.; Angiolillo, D.J.; Farhan, S.; Goel, R.; Zhang, Z.; Briguori, C.; et al. Sex Differences Among Patients With High Risk Receiving Ticagrelor With or Without Aspirin After Percutaneous Coronary Intervention: A Subgroup Analysis of the TWILIGHT Randomized Clinical Trial. JAMA Cardiol. 2021, 6, 1032–1041. [Google Scholar] [CrossRef]
- Baber, U.; Dangas, G.; Angiolillo, D.J.; Cohen, D.J.; Sharma, S.K.; Nicolas, J.; Briguori, C.; Cha, J.Y.; Collier, T.; Dudek, D.; et al. Ticagrelor alone vs. ticagrelor plus aspirin following percutaneous coronary intervention in patients with non-ST-segment elevation acute coronary syndromes: TWILIGHT-ACS. Eur. Heart J. 2020, 41, 3533–3545. [Google Scholar] [CrossRef]
- Dangas, G.; Baber, U.; Sharma, S.; Giustino, G.; Mehta, S.; Cohen, D.J.; Angiolillo, D.J.; Sartori, S.; Chandiramani, R.; Briguori, C.; et al. Ticagrelor With or Without Aspirin After Complex PCI. J. Am. Coll. Cardiol. 2020, 75, 2414–2424. [Google Scholar] [CrossRef]
- Escaned, J.; Cao, D.; Baber, U.; Nicolas, J.; Sartori, S.; Zhang, Z.; Dangas, G.; Angiolillo, D.J.; Briguori, C.; Cohen, D.J.; et al. Ticagrelor monotherapy in patients at high bleeding risk undergoing percutaneous coronary intervention: TWILIGHT-HBR. Eur. Heart J. 2021, 42, 4624–4634. [Google Scholar] [CrossRef]
- Angiolillo, D.J.; Baber, U.; Sartori, S.; Briguori, C.; Dangas, G.; Cohen, D.J.; Mehta, S.R.; Gibson, C.M.; Chandiramani, R.; Huber, K.; et al. Ticagrelor With or Without Aspirin in High-Risk Patients With Diabetes Mellitus Undergoing Percutaneous Coronary Intervention. J. Am. Coll. Cardiol. 2020, 75, 2403–2413. [Google Scholar] [CrossRef] [PubMed]
- Vranckx, P.; Valgimigli, M.; Jüni, P.; Hamm, C.; Steg, P.G.; Heg, D.; van Es, G.A.; McFadden, E.P.; Onuma, Y.; van Meijeren, C.; et al. Ticagrelor plus aspirin for 1 month, followed by ticagrelor monotherapy for 23 months vs aspirin plus clopidogrel or ticagrelor for 12 months, followed by aspirin monotherapy for 12 months after implantation of a drug-eluting stent: A multicentre, open-label, randomised superiority trial. Lancet 2018, 392, 940–949. [Google Scholar] [PubMed]
- Mega, J.L.; Close, S.L.; Wiviott, S.D.; Shen, L.; Hockett, R.D.; Brandt, J.T.; Walker, J.R.; Antman, E.M.; Macias, W.; Braunwald, E.; et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N. Engl. J. Med. 2009, 360, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Bonaca, M.P.; Bhatt, D.L.; Cohen, M.; Steg, P.G.; Storey, R.F.; Jensen, E.C.; Magnani, G.; Bansilal, S.; Fish, M.P.; Im, K.; et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N. Engl. J. Med. 2015, 372, 1791–1800. [Google Scholar] [CrossRef] [PubMed]
- Mauri, L.; Kereiakes, D.J.; Yeh, R.W.; Driscoll-Shempp, P.; Cutlip, D.E.; Steg, P.G.; Normand, S.-L.T.; Braunwald, E.; Wiviott, S.D.; Cohen, D.J.; et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N. Engl. J. Med. 2014, 371, 2155–2166. [Google Scholar] [CrossRef] [PubMed]
- Gargiulo, G.; Goette, A.; Tijssen, J.; Eckardt, L.; Lewalter, T.; Vranckx, P.; Valgimigli, M. Safety and efficacy outcomes of double vs. triple antithrombotic therapy in patients with atrial fibrillation following percutaneous coronary intervention: A systematic review and meta-analysis of non-vitamin K antagonist oral anticoagulant-based randomized clinical trials. Eur. Heart J. 2019, 40, 3757–3767. [Google Scholar] [PubMed]
- Yasuda, S.; Kaikita, K.; Akao, M.; Ako, J.; Matoba, T.; Nakamura, M.; Miyauchi, K.; Hagiwara, N.; Kimura, K.; Hirayama, A.; et al. Antithrombotic Therapy for Atrial Fibrillation with Stable Coronary Disease. N. Engl. J. Med. 2019, 381, 1103–1113. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Kim, W.; Hwang, S.H.; Kang, W.Y.; Cho, S.C.; Kim, W.; Jeong, M.H.; Other Korean Working Group in Myocardial Infarction Registry Investigators. The CHA2DS2VASc score can be used to stratify the prognosis of acute myocardial infarction patients irrespective of presence of atrial fibrillation. J. Cardiol. 2015, 65, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Podolecki, T.; Lenarczyk, R.; Kowalczyk, J.; Swierad, M.; Swiatkowski, A.; Jedrzejczyk, E.; Chodor, P.; Zielinska, T.; Kalarus, Z. Stroke and death prediction with CHA2DS2-vasc score after myocardial infarction in patients without atrial fibrillation. J. Cardiovasc. Med. 2015, 16, 497–502. [Google Scholar] [CrossRef]
- Sonaglioni, A.; Lonati, C.; Rigamonti, E.; Viganò, M.; Nicolosi, G.L.; Proietti, M.; Lombardo, M.; Harari, S. CHA2DS2-VASc score stratifies mortality risk in heart failure patients aged 75 years and older with and without atrial fibrillation. Aging Clin. Exp. Res. 2022, 34, 1707–1720. [Google Scholar] [CrossRef]


| Study | Year | Study Population | Study Design | Follow-Up | Primary-Endpoint | Results | |
|---|---|---|---|---|---|---|---|
| PRE-TREATMENT IN ACS | |||||||
| ACCOAST [7] | 2013 | 4033 pts | Pre-treatment with prasugrel vs. placebo (NSTE-ACS) | 30 days | death from CV causes, MI, stroke, urgent revascularization or GP IIb/IIIa bailout | HR 1.02; 95% CI, 0.84 to 1.25; p = 0.81 | |
| DUBIUS [8] | 2020 | 1499 pts | Pre-treatment with ticagrelor vs. no pre-treatment (NSTE-ACS) | 30 days | death due to vascular causes, non-fatal MI or non-fatal stroke | ARR: –0.46; 95% CI: –2.87 to 1.89 | |
| ATLANTIC [10] | 2014 | 1862 pts | Pre-treatment with ticagrelor vs. in-hospital treatment with ticagrelor (STEMI) | 30 days | 70% or greater resolution of ST-elevation / no TIMI flow grade 3 in the IRA | ST-elevation: OR 0.93; 95% CI, 0.69 to 1.25; p = 0.63 TIMI flow: 0.97; 95% CI, 0.75 to 1.25; p = 0.82 | |
| SHORTENING OF DAPT | |||||||
| TWILIGHT [11] | 2019 | 7119 pts | 3 vs. 12 mo ticagrelor-based DAPT | 15 mo | BARC type 2,3, or 5 | HR 0.99; 95% CI, 0.78 to 1.25; Pnon-inferiority < 0.001 | |
| TICO [12] | 2020 | 3056 pts | 3 vs. 12 mo ticagrelor-based DAPT | 12 mo | TIMI major bleeding, all-cause death, MI, ST, stroke, or TVR | HR 0.66; 95% CI, 0.48 to 0.92; p = 0.01 | |
| STOPDAPT-2 [13] | 2019 | 3045 pts | 1 vs. 12 mo clopidogrel-based DAPT | 12 mo | CV death, MI, ST, stroke, or TIMI major or minor bleeding | HR 0.26, 95% CI, 0.11 to 0.64, p = 0.004 | |
| STOPDAPT2-ACS [14] | 2022 | 4169 pts | 1 vs. 12 mo clopidogrel-based DAPT | 12 mo | CV death, MI, ST, stroke, or TIMI major or minor bleeding | HR 1.14; 95% CI, 0.80 to 1.6; Pnon-inferiority = 0.06 | |
| MASTER-DAPT [15] | 2021 | 4434 pts | 1 vs. ≥ 3 mo clopidogrel-based DAPT | 11 mo | all-cause death, MI, stroke, or BARC type 3, or 5 | −0.23 percentage points; 95% CI, −1.80 to 1.33; Pnon-inferiority < 0.001 | |
| DE-ESCALATION OF DAPT | |||||||
| TROPICAL-ACS [16] | 2017 | 2610 pts | de-escalation to clopidogrel-based DAPT at day 7–14 after discharge vs. standard DAPT | 12 mo | CV death, MI, stroke, BARC type ≥ 2 | HR 0.81; 95% CI, 0.62 to 1.06; Pnon-inferiority = 0.0004 | |
| POPULAR GENETICS [17] | 2019 | 2499 pts | de-escalation to clopidogrel-based DAPT at day 1 to 3 after PCI vs. standard DAPT | 12 mo | all-cause death, MI, ST, stroke, or PLATO major bleeding | 95% CI, 2.0 to 0.7; Pnon-inferiority < 0.001 | |
| TOPIC [18] | 2017 | 646 pts | de-escalation 30 days after PCI to clopidogrel-based DAPT vs. standard DAPT | 12 mo | CV death, TVR, stroke, BARC type ≥ 2 | HR 0.48; 95% CI 0.34–0.68; p < 0.01 | |
| TALOS-AMI [19] | 2021 | 2697 pts | de-escalation 30 days after PCI to clopidogrel-based DAPT vs. standard DAPT | 12 mo | CV death, MI, stroke, BARC type 2,3, or 5 | HR 0.55; 95% CI, 0.40 to 0.76; Pnon-inferiority < 0.001 | |
| TRIPLE- AND DUAL ANTITHROMBOTIC THERAPY | |||||||
| PIONEER AF-PCI [20] | 2016 | 2124 pts | DAT with rivaroxaban (gr 1) vs. TAT with low-dose rivaroxaban (gr 2) vs. TAT with VKA (gr 3) | 36 mo | TIMI major bleeding or minor bleeding or bleeding requiring medical attention | gr 1 vs. gr 3: HR 0.59; 95% CI, 0.47 to 0.76; p < 0.001 gr 2 vs. gr 3: HR 0.63; 95% CI, 0.50 to 0.80; p < 0.001 | |
| RE-DUAL-PCI [21] | 2018 | 2725 pts | DAT with dabigatran vs. TAT with VKA | 14 mo | ISTH major or clinically relevant non major bleeding | 110 mg: HR 0.52; 95% CI, 0.42 to 0.63; Psuperiority < 0.001 150 mg: HR 0.72; 95% CI, 0.58 to 0.88; Pnon-inferiority < 0.001 | |
| AUGUSTUS [22] | 2019 | 4614 pts | DAT with apixaban vs. DAT with VKA TAT with apixaban vs. TAT with VKA | 6 mo | ISTH major or clinically relevant non-major bleeding | Apixaban vs. VKA: HR, 0.69; 95% CI, 0.58 to 0.81; p < 0.001 DAT vs. TAT: HR 1.89; 95% CI, 1.59 to 2.24; p < 0.001 | |
| ENTRUST AF-PCI [23] | 2019 | 1506 pts | DAT with edoxaban vs. TAT with VKA | 12 mo | Major or clinically relevant non-major bleeding (CRNM) | HR 0.83; 95% CI 0.65–1.05; Pnon-inferiority = 0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaufmann, C.C.; Muthspiel, M.; Lunzer, L.; Pogran, E.; Zweiker, D.; Burger, A.L.; Wojta, J.; Huber, K. Antiplatelet Therapy and Anticoagulation before, during, and after Acute Coronary Syndrome. J. Clin. Med. 2024, 13, 2313. https://doi.org/10.3390/jcm13082313
Kaufmann CC, Muthspiel M, Lunzer L, Pogran E, Zweiker D, Burger AL, Wojta J, Huber K. Antiplatelet Therapy and Anticoagulation before, during, and after Acute Coronary Syndrome. Journal of Clinical Medicine. 2024; 13(8):2313. https://doi.org/10.3390/jcm13082313
Chicago/Turabian StyleKaufmann, Christoph C., Marie Muthspiel, Laura Lunzer, Edita Pogran, David Zweiker, Achim Leo Burger, Johann Wojta, and Kurt Huber. 2024. "Antiplatelet Therapy and Anticoagulation before, during, and after Acute Coronary Syndrome" Journal of Clinical Medicine 13, no. 8: 2313. https://doi.org/10.3390/jcm13082313
APA StyleKaufmann, C. C., Muthspiel, M., Lunzer, L., Pogran, E., Zweiker, D., Burger, A. L., Wojta, J., & Huber, K. (2024). Antiplatelet Therapy and Anticoagulation before, during, and after Acute Coronary Syndrome. Journal of Clinical Medicine, 13(8), 2313. https://doi.org/10.3390/jcm13082313







