Can Biomarkers and PET Imaging Predict Abdominal Aortic Aneurysm Growth Rate?
Abstract
:1. Introduction
2. Materials and Methods
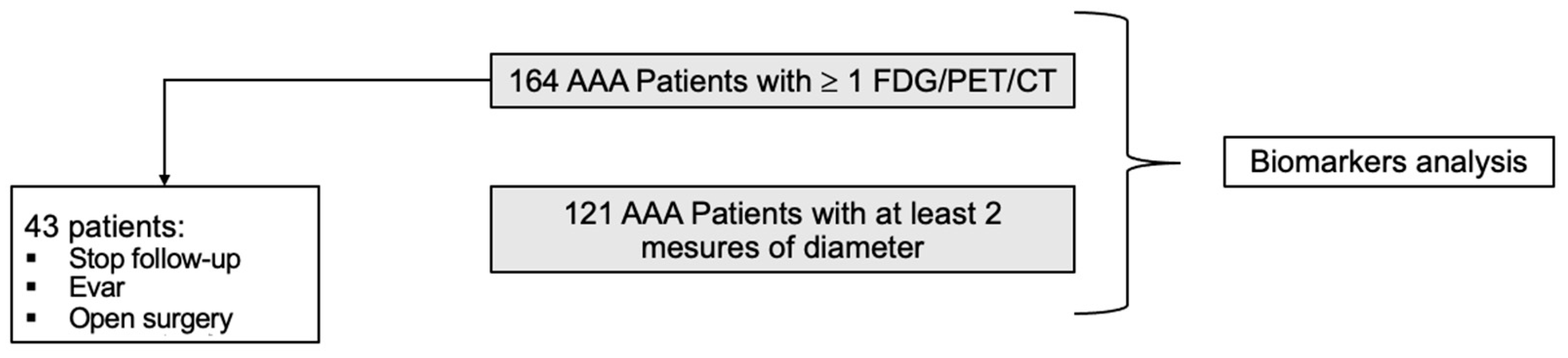
2.1. Population
2.2. Study Design
2.3. Follow-Up and AAA Diameter Progression
2.4. [18F]FDG PET/CT Image Acquisition
2.5. [18F]FDG PET/CT Quantitative Image Analysis
2.6. [18F]FDG PET/CT Visual Image Analysis
2.7. Blood Collection—Sample Analysis
2.8. Statistical Analysis
3. Results
3.1. Patient Characteristics at Inclusion
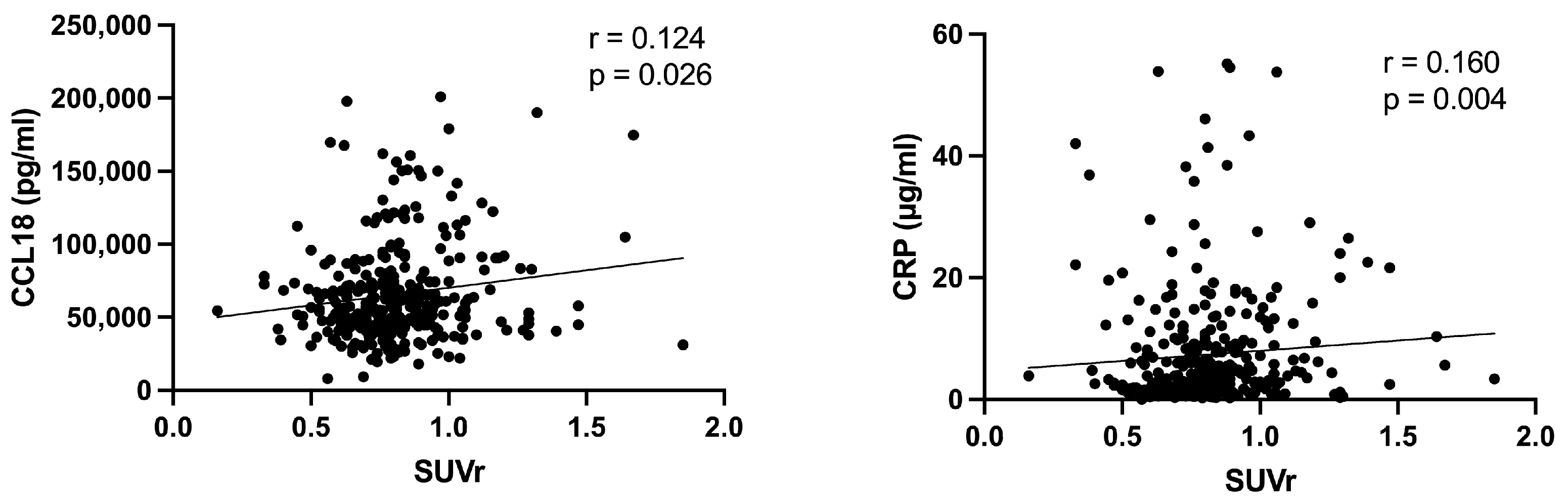
3.2. Correlation between Biomarkers and PET Results
3.3. Clinical Characteristics and Biomarkers Associated with AAA Diameter Progression
3.4. Clinical Characteristics and Biomarkers Associated with Mortality
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sakalihasan, N.; Michel, J.-B.; Katsargyris, A.; Kuivaniemi, H.; Defraigne, J.-O.; Nchimi, A.; Powell, J.T.; Yoshimura, K.; Hultgren, R. Abdominal Aortic Aneurysms. Nat. Rev. Dis. Primer 2018, 4, 34. [Google Scholar] [CrossRef] [PubMed]
- Wanhainen, A.; Van Herzeele, I.; Bastos Goncalves, F.; Bellmunt Montoya, S.; Berard, X.; Boyle, J.R.; D’Oria, M.; Prendes, C.F.; Karkos, C.D.; Kazimierczak, A.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2024 Clinical Practice Guidelines on the Management of Abdominal Aorto-Iliac Artery Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2024, 67, 192–331. [Google Scholar] [CrossRef]
- Truijers, M.; Kurvers, H.A.J.M.; Bredie, S.J.H.; Oyen, W.J.G.; Blankensteijn, J.D. In Vivo Imaging of Abdominal Aortic Aneurysms: Increased FDG Uptake Suggests Inflammation in the Aneurysm Wall. J. Endovasc. Ther. Off. J. Int. Soc. Endovasc. Spec. 2008, 15, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Treska, V.; Kocova, J.; Boudova, L.; Neprasova, P.; Topolcan, O.; Pecen, L.; Tonar, Z. Inflammation in the Wall of Abdominal Aortic Aneurysm and Its Role in the Symptomatology of Aneurysm. Cytokines Cell. Mol. Ther. 2002, 7, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Barwick, T.D.; Lyons, O.T.A.; Mikhaeel, N.G.; Waltham, M.; O’Doherty, M.J. 18F-FDG PET-CT Uptake Is a Feature of Both Normal Diameter and Aneurysmal Aortic Wall and Is Not Related to Aneurysm Size. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 2310–2318. [Google Scholar] [CrossRef] [PubMed]
- Palombo, D.; Morbelli, S.; Spinella, G.; Pane, B.; Marini, C.; Rousas, N.; Massollo, M.; Cittadini, G.; Camellino, D.; Sambuceti, G. A Positron Emission Tomography/Computed Tomography (PET/CT) Evaluation of Asymptomatic Abdominal Aortic Aneurysms: Another Point of View. Ann. Vasc. Surg. 2012, 26, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Tegler, G.; Ericson, K.; Sörensen, J.; Björck, M.; Wanhainen, A. Inflammation in the Walls of Asymptomatic Abdominal Aortic Aneurysms Is Not Associated with Increased Metabolic Activity Detectable by 18-Fluorodeoxglucose Positron-Emission Tomography. J. Vasc. Surg. 2012, 56, 802–807. [Google Scholar] [CrossRef]
- Xu, X.Y.; Borghi, A.; Nchimi, A.; Leung, J.; Gomez, P.; Cheng, Z.; Defraigne, J.O.; Sakalihasan, N. High Levels of 18F-FDG Uptake in Aortic Aneurysm Wall Are Associated with High Wall Stress. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2010, 39, 295–301. [Google Scholar] [CrossRef]
- Courtois, A.; Nusgens, B.V.; Hustinx, R.; Namur, G.; Gomez, P.; Somja, J.; Defraigne, J.-O.; Delvenne, P.; Michel, J.-B.; Colige, A.C.; et al. 18F-FDG Uptake Assessed by PET/CT in Abdominal Aortic Aneurysms Is Associated with Cellular and Molecular Alterations Prefacing Wall Deterioration and Rupture. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2013, 54, 1740–1747. [Google Scholar] [CrossRef]
- Courtois, A.; Nusgens, B.; Garbacki, N.; Hustinx, R.; Gomez, P.; Defraigne, J.-O.; Colige, A.C.; Sakalihasan, N. Circulating microRNAs Signature Correlates with Positive [18F]Fluorodeoxyglucose-Positron Emission Tomography in Patients with Abdominal Aortic Aneurysm. J. Vasc. Surg. 2018, 67, 585–595.e3. [Google Scholar] [CrossRef]
- Stepien, K.L.; Bajdak-Rusinek, K.; Fus-Kujawa, A.; Kuczmik, W.; Gawron, K. Role of Extracellular Matrix and Inflammation in Abdominal Aortic Aneurysm. Int. J. Mol. Sci. 2022, 23, 11078. [Google Scholar] [CrossRef] [PubMed]
- Memon, A.A.; Zarrouk, M.; Ågren-Witteschus, S.; Sundquist, J.; Gottsäter, A.; Sundquist, K. Identification of Novel Diagnostic and Prognostic Biomarkers for Abdominal Aortic Aneurysm. Eur. J. Prev. Cardiol. 2020, 27, 132–142. [Google Scholar] [CrossRef]
- Urbonavicius, S.; Urbonaviciene, G.; Honoré, B.; Henneberg, E.W.; Vorum, H.; Lindholt, J.S. Potential Circulating Biomarkers for Abdominal Aortic Aneurysm Expansion and Rupture—A Systematic Review. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2008, 36, 273–280, discussion 281–282. [Google Scholar] [CrossRef] [PubMed]
- Sangiorgi, G.; Biondi-Zoccai, G.; Pizzuto, A.; Martelli, E. Commentary: Biochemical Markers for Diagnosis and Follow-up of Aortic Diseases: An Endless Search for the Holy Grail. J. Endovasc. Ther. Off. J. Int. Soc. Endovasc. Spec. 2019, 26, 836–842. [Google Scholar] [CrossRef] [PubMed]
- Golledge, J.; Tsao, P.S.; Dalman, R.L.; Norman, P.E. Circulating Markers of Abdominal Aortic Aneurysm Presence and Progression. Circulation 2008, 118, 2382–2392. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, A.T.; Haskal, Z.J.; Hertzer, N.R.; Bakal, C.W.; Creager, M.A.; Halperin, J.L.; Hiratzka, L.F.; Murphy, W.R.C.; Olin, J.W.; Puschett, J.B.; et al. ACC/AHA 2005 Practice Guidelines for the Management of Patients With Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic): A Collaborative Report from the American Association for Vascular Surgery/Society for Vascular Surgery,* Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients with Peripheral Arterial Disease): Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 2006, 113, e463–e654. [Google Scholar] [CrossRef] [PubMed]
- Limet, R.; Sakalihassan, N.; Albert, A. Determination of the Expansion Rate and Incidence of Rupture of Abdominal Aortic Aneurysms. J. Vasc. Surg. 1991, 14, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Paquet, N.; Albert, A.; Foidart, J.; Hustinx, R. Within-Patient Variability of (18)F-FDG: Standardized Uptake Values in Normal Tissues. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2004, 45, 784–788. [Google Scholar]
- Hadi, T.; Boytard, L.; Silvestro, M.; Alebrahim, D.; Jacob, S.; Feinstein, J.; Barone, K.; Spiro, W.; Hutchison, S.; Simon, R.; et al. Macrophage-Derived Netrin-1 Promotes Abdominal Aortic Aneurysm Formation by Activating MMP3 in Vascular Smooth Muscle Cells. Nat. Commun. 2018, 9, 5022. [Google Scholar] [CrossRef]
- Carrell, T.W.G.; Burnand, K.G.; Wells, G.M.A.; Clements, J.M.; Smith, A. Stromelysin-1 (Matrix Metalloproteinase-3) and Tissue Inhibitor of Metalloproteinase-3 Are Overexpressed in the Wall of Abdominal Aortic Aneurysms. Circulation 2002, 105, 477–482. [Google Scholar] [CrossRef]
- Wang, Y.; Shen, G.; Wang, H.; Yao, Y.; Sun, Q.; Jing, B.; Liu, G.; Wu, J.; Yuan, C.; Liu, S.; et al. Association of High Sensitivity C-Reactive Protein and Abdominal Aortic Aneurysm: A Meta-Analysis and Systematic Review. Curr. Med. Res. Opin. 2017, 33, 2145–2152. [Google Scholar] [CrossRef] [PubMed]
- Groeneveld, M.E.; Meekel, J.P.; Rubinstein, S.M.; Merkestein, L.R.; Tangelder, G.J.; Wisselink, W.; Truijers, M.; Yeung, K.K. Systematic Review of Circulating, Biomechanical, and Genetic Markers for the Prediction of Abdominal Aortic Aneurysm Growth and Rupture. J. Am. Heart Assoc. 2018, 7, e007791. [Google Scholar] [CrossRef] [PubMed]
- Courtois, A.; Nusgens, B.V.; Hustinx, R.; Namur, G.; Gomez, P.; Kuivaniemi, H.; Defraigne, J.-O.; Colige, A.C.; Sakalihasan, N. Gene Expression Study in Positron Emission Tomography-Positive Abdominal Aortic Aneurysms Identifies CCL18 as a Potential Biomarker for Rupture Risk. Mol. Med. Camb. Mass 2015, 20, 697–706. [Google Scholar] [CrossRef] [PubMed]
- Mao, D.; Lee, J.K.; VanVickle, S.J.; Thompson, R.W. Expression of Collagenase-3 (MMP-13) in Human Abdominal Aortic Aneurysms and Vascular Smooth Muscle Cells in Culture. Biochem. Biophys. Res. Commun. 1999, 261, 904–910. [Google Scholar] [CrossRef] [PubMed]
- Makrygiannis, G.; Mourmoura, E.; Spanos, K.; Roussas, N.; Kuivaniemi, H.; Sakalihasan, N.; Tsezou, A.; Giannoukas, A. Risk Factor Assessment in a Greek Cohort of Patients with Large Abdominal Aortic Aneurysms. Angiology 2019, 70, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Golledge, J.; Muller, J.; Shephard, N.; Clancy, P.; Smallwood, L.; Moran, C.; Dear, A.E.; Palmer, L.J.; Norman, P.E. Association between Osteopontin and Human Abdominal Aortic Aneurysm. Arterioscler. Thromb. Vasc. Biol. 2007, 27, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Filis, K.; Martinakis, V.; Galyfos, G.; Sigala, F.; Theodorou, D.; Andreadou, I.; Zografos, G. Osteopontin and Osteoprotegerin as Potential Biomarkers in Abdominal Aortic Aneurysm before and after Treatment. Int. Sch. Res. Not. 2014, 2014, 461239. [Google Scholar] [CrossRef] [PubMed]
- Koole, D.; Hurks, R.; Schoneveld, A.; Vink, A.; Golledge, J.; Moran, C.S.; de Kleijn, D.P.; van Herwaarden, J.A.; de Vries, J.-P.; Laman, J.D.; et al. Osteoprotegerin Is Associated with Aneurysm Diameter and Proteolysis in Abdominal Aortic Aneurysm Disease. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 1497–1504. [Google Scholar] [CrossRef] [PubMed]
- Hellenthal, F.A.M.V.I.; Buurman, W.A.; Wodzig, W.K.W.H.; Schurink, G.W.H. Biomarkers of Abdominal Aortic Aneurysm Progression. Part 2: Inflammation. Nat. Rev. Cardiol. 2009, 6, 543–552. [Google Scholar] [CrossRef]
- Khosla, S.; Arrighi, H.M.; Melton, L.J.; Atkinson, E.J.; O’Fallon, W.M.; Dunstan, C.; Riggs, B.L. Correlates of Osteoprotegerin Levels in Women and Men. Osteoporos. Int. J. Establ. Result Coop. Eur. Found. Osteoporos. Natl. Osteoporos. Found. USA 2002, 13, 394–399. [Google Scholar] [CrossRef]
- Hofbauer, L.C.; Khosla, S.; Dunstan, C.R.; Lacey, D.L.; Spelsberg, T.C.; Riggs, B.L. Estrogen Stimulates Gene Expression and Protein Production of Osteoprotegerin in Human Osteoblastic Cells. Endocrinology 1999, 140, 4367–4370. [Google Scholar] [CrossRef] [PubMed]
- Mofidi, R.; Goldie, V.J.; Kelman, J.; Dawson, A.R.W.; Murie, J.A.; Chalmers, R.T.A. Influence of Sex on Expansion Rate of Abdominal Aortic Aneurysms. Br. J. Surg. 2007, 94, 310–314. [Google Scholar] [CrossRef] [PubMed]
- Villard, C.; Eriksson, P.; Swedenborg, J.; Hultgren, R. Differences in Elastin and Elastolytic Enzymes between Men and Women with Abdominal Aortic Aneurysm. Aorta Stamford Conn 2014, 2, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Thompson, S.G.; Brown, L.C.; Sweeting, M.J.; Bown, M.J.; Kim, L.G.; Glover, M.J.; Buxton, M.J.; Powell, J.T. Systematic Review and Meta-Analysis of the Growth and Rupture Rates of Small Abdominal Aortic Aneurysms: Implications for Surveillance Intervals and Their Cost-Effectiveness. Health Technol. Assess. Winch. Engl. 2013, 17, 1–118. [Google Scholar] [CrossRef] [PubMed]
- Forbes, T.L.; Lawlor, D.K.; DeRose, G.; Harris, K.A. Gender Differences in Relative Dilatation of Abdominal Aortic Aneurysms. Ann. Vasc. Surg. 2006, 20, 564–568. [Google Scholar] [CrossRef]
- Villard, C.; Wågsäter, D.; Swedenborg, J.; Eriksson, P.; Hultgren, R. Biomarkers for Abdominal Aortic Aneurysms from a Sex Perspective. Gend. Med. 2012, 9, 259–266.e2. [Google Scholar] [CrossRef]

| Variable | Without Rapid Growth (n = 85) | With Rapid Growth (n = 36) | p-Value *** |
|---|---|---|---|
| Age (years) | 70.5 ± 7.3 | 71.1 ± 10.0 | 0.73 |
| Sex (Male) | 80 (94.1) | 28 (77.8) | 0.013 |
| Smokers (Current) | 31 (36.5) | 18 (50) | 0.32 |
| Diabetes | 15 (17.6) | 3 (8.3) | 0.20 |
| Hypertension | 50 (58.8) | 27 (75.0) | 0.094 |
| Chronic obstructive pulmonary disease | 28 (32.9) | 10 (27.8) | 0.58 |
| Renal insufficiency | 13 (15.3) | 4 (11.1) | 0.55 |
| Stroke | 15 (17.6) | 4 (11.1) | 0.37 |
| Hyperlipidemia | 60 (70.6) | 17 (47.2) | 0.016 |
| Acute myocardial infarction | 25 (29.4) | 8 (22.2) | 0.42 |
| Peripheral arterial disease | 22 (25.9) | 12 (33.3) | 0.41 |
| Angina pectoris | 12 (14.1) | 3 (8.3) | 0.38 |
| Aspirin | 48 (56.5) | 21(58.3) | 0.85 |
| Statin | 55 (65.5) | 20 (55.6) | 0.31 |
| Betablockers Biomarkers of Inflammation CRP (µg/mL) CCL18 (ng/mL) Biomarkers of AAA MMP3 (ng/mL) MMP9 (ng/mL) MMP13 (pg/mL) OPN (ng/mL) OPG (pg/mL) | 22 (26.2) 5.59 ± 7.39 63.2 ± 34.6 3.72 ± 1.75 696 ± 388 246 ± 256 88.5 ± 35.8 3066 ± 1293 | 15 (41.7) 12.5 ± 17.1 69.7 ± 35.2 3.52 ± 1.63 1039 ± 636 247 ± 224 98.0 ± 22.4 3481 ± 1418 | 0.095 0.010 0.22 0.89 0.0006 0.40 0.018 0.043 |
| Diameter PET1 | 46.5 ± 8.34 | 52.3 ± 10.8 | 0.0037 |
| SUVr * | 0.77 ± 0.24 | 0.80 ± 0.23 | 0.56 |
| PET+ Median Growth Rate (mm/year) ** | 9 (10.6%) 4.4 (2.1–6.3) | 7 (19.4%) 20.0 (14.4–33.2) | 0.19 0.0003 |
| OR | 95%CI OR | p-Value | |
|---|---|---|---|
| Model 1 * | |||
| Sex (Female) | 5.62 | 1.48–21.4 | 0.011 |
| Hyperlipidemia | 0.28 | 0.11–0.72 | 0.0080 |
| Betablockers | 3.11 | 1.13–8.58 | 0.029 |
| Diameter PET at entry ≥ 55 mm | 3.16 | 1.05–13.5 | 0.035 |
| Model 2 ** | |||
| CRP (μg/mL) | 4.11 | 1.46–11.6 | 0.0074 |
| Diameter PET at entry ≥ 55 mm | 1.51 | 1.03–2.20 | 0.035 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bruls, S.; Musumeci, L.; Courtois, A.; Hustinx, R.; Sakalihasan, S.; Namur, G.; Defraigne, J.-O.; Sakalihasan, N. Can Biomarkers and PET Imaging Predict Abdominal Aortic Aneurysm Growth Rate? J. Clin. Med. 2024, 13, 2448. https://doi.org/10.3390/jcm13082448
Bruls S, Musumeci L, Courtois A, Hustinx R, Sakalihasan S, Namur G, Defraigne J-O, Sakalihasan N. Can Biomarkers and PET Imaging Predict Abdominal Aortic Aneurysm Growth Rate? Journal of Clinical Medicine. 2024; 13(8):2448. https://doi.org/10.3390/jcm13082448
Chicago/Turabian StyleBruls, Samuel, Lucia Musumeci, Audrey Courtois, Roland Hustinx, Sarah Sakalihasan, Gauthier Namur, Jean-Olivier Defraigne, and Natzi Sakalihasan. 2024. "Can Biomarkers and PET Imaging Predict Abdominal Aortic Aneurysm Growth Rate?" Journal of Clinical Medicine 13, no. 8: 2448. https://doi.org/10.3390/jcm13082448
APA StyleBruls, S., Musumeci, L., Courtois, A., Hustinx, R., Sakalihasan, S., Namur, G., Defraigne, J. -O., & Sakalihasan, N. (2024). Can Biomarkers and PET Imaging Predict Abdominal Aortic Aneurysm Growth Rate? Journal of Clinical Medicine, 13(8), 2448. https://doi.org/10.3390/jcm13082448






