Analysis of Risk Factors for Augmented Vertebral Refracture After Percutaneous Kyphoplasty in Osteoporotic Vertebral Compression Fractures
Abstract
:1. Introduction
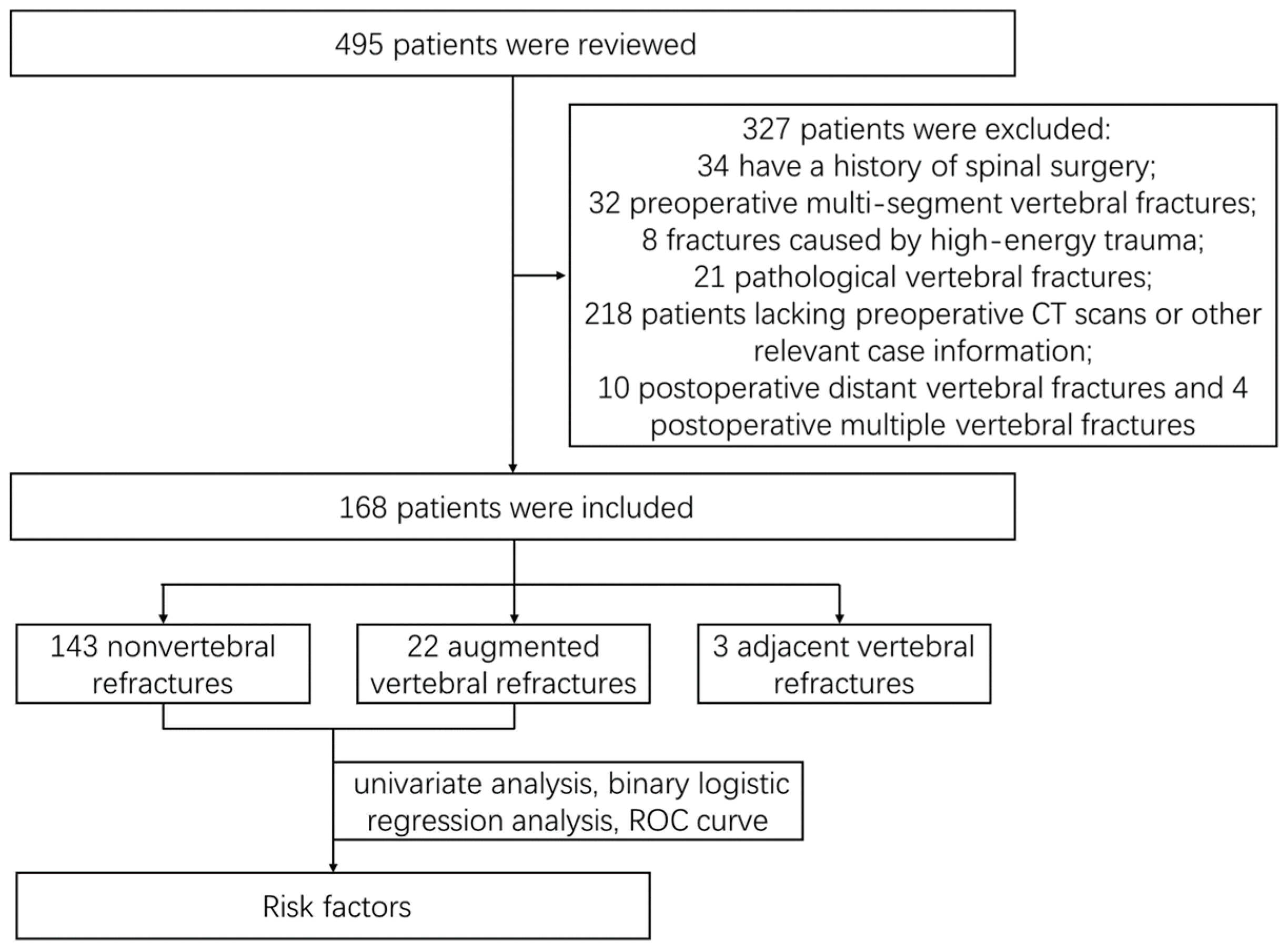
2. Materials and Methods
2.1. General Data
2.2. Treatment Method
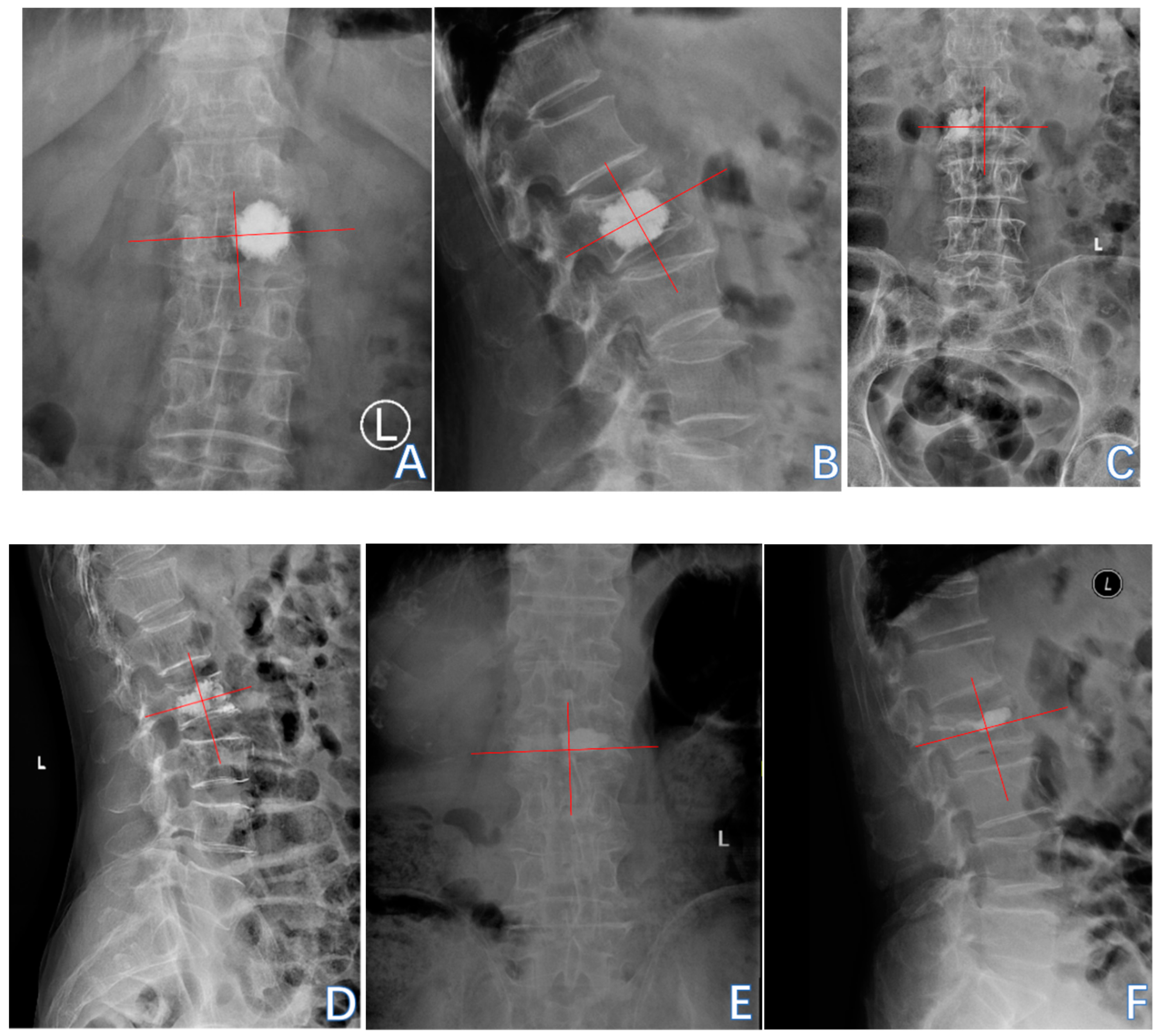
2.3. Evaluation Index
2.4. Statistical Analysis
3. Results
3.1. General Situation
3.2. Augmented Vertebral Refractures
3.2.1. Univariate Analysis
3.2.2. Binary Logistic Regression Analysis
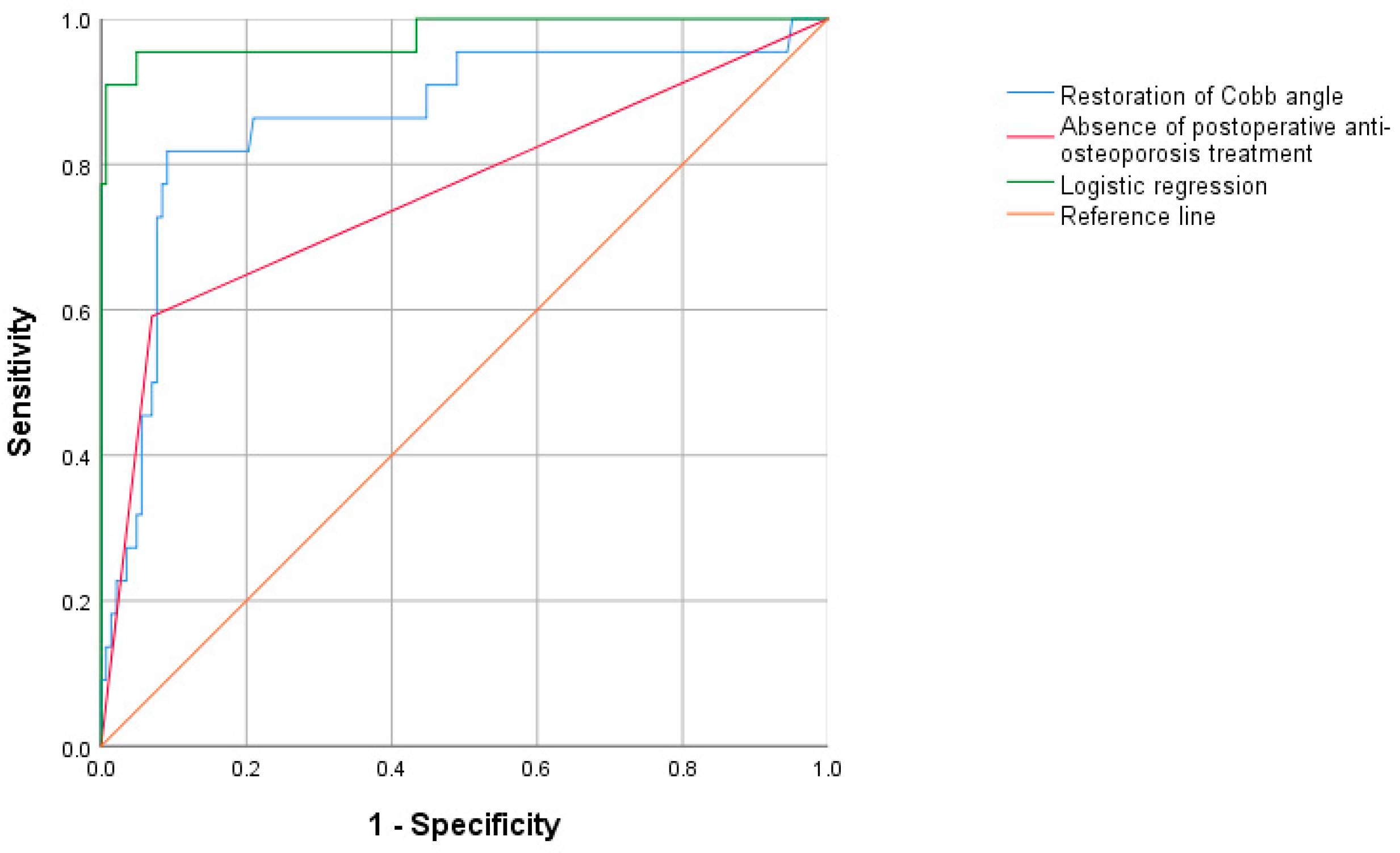
3.2.3. Receiver Operating Characteristic (ROC) Curve
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Looker, A.C.; Sarafrazi Isfahani, N.; Fan, B.; Shepherd, J.A. Trends in osteoporosis and low bone mass in older US adults, 2005–2006 through 2013–2014. Osteoporos. Int. 2017, 28, 1979–1988. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Zhai, T. Coffee Drinking and the Odds of Osteopenia and Osteoporosis in Middle-Aged and Older Americans: A Cross-Sectional Study in NHANES 2005–2014. Calcif. Tissue Int. 2024, 114, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Felsenberg, D.; Silman, A.J.; Lunt, M.; Armbrecht, G.; Ismail, A.A.; Finn, J.D.; Cockerill, W.C.; Banzer, D.; Benevolenskaya, L.I.; Bhalla, A.; et al. Incidence of vertebral fracture in europe: Results from the European Prospective Osteoporosis Study (EPOS). J. Bone Miner. Res. 2002, 17, 716–724. [Google Scholar] [CrossRef] [PubMed]
- Gregson, C.L.; Armstrong, D.J.; Bowden, J.; Cooper, C.; Edwards, J.; Gittoes, N.J.L.; Harvey, N.; Kanis, J.; Leyland, S.; Low, R.; et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch. Osteoporos. 2022, 17, 58. [Google Scholar] [CrossRef] [PubMed]
- Pongchaiyakul, C.; Charoensri, S.; Leerapun, T.; Wongsiri, S.; Songpatanasilp, T.; Taechakraichana, N. Prevalence of asymptomatic radiographic vertebral fracture in postmenopausal Thai women. Arch. Osteoporos. 2020, 15, 78. [Google Scholar] [CrossRef]
- Wang, L.; Yu, W.; Yin, X.; Cui, L.; Tang, S.; Jiang, N.; Cui, L.; Zhao, N.; Lin, Q.; Chen, L.; et al. Prevalence of Osteoporosis and Fracture in China: The China Osteoporosis Prevalence Study. JAMA Netw. Open 2021, 4, e2121106. [Google Scholar] [CrossRef]
- Zheng, X.Q.; Xu, L.; Huang, J.; Zhang, C.G.; Yuan, W.Q.; Sun, C.G.; Zhang, Z.S.; Wei, C.; Wang, J.X.; Cummings, S.R.; et al. Incidence and cost of vertebral fracture in urban China: A 5-year population-based cohort study. Int. J. Surg. 2023, 109, 1910–1918. [Google Scholar] [CrossRef]
- Yao, R.; Yin, P.; Zhang, Y.; Li, D.; Zhang, X.N.; Tao, L.; Zhou, J.; Su, Q. Is there a risk of further displacement of the fractured fragment into the spinal canal in osteoporotic vertebral burst fractures after unilateral PKP? A prospective study. Spine J. 2024, 24, 1077–1086. [Google Scholar] [CrossRef]
- Gao, W.; Chen, Y.; Wang, X.; Liu, G.; Cui, K.; Guo, J.; Zheng, J.; Hao, Y. Establishment and Verification of a Predictive Nomogram for New Vertebral Compression Fracture Occurring after Bone Cement Injection in Middle-Aged and Elderly Patients with Vertebral Compression Fracture. Orthop. Surg. 2023, 15, 961–972. [Google Scholar] [CrossRef] [PubMed]
- Praveen, A.D.; Aspelund, T.; Ferguson, S.J.; Sigurðsson, S.; Guðnason, V.; Pálsson, H.; Matchar, D.; Helgason, B. Refracture and mortality risk in the elderly with osteoporotic fractures: The AGES-Reykjavik study. Osteoporos. Int. 2024, 35, 1231–1241. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Li, J.; Wu, S.; Yuan, L.; Qu, L.; Wang, Y.; Yang, H.; Yang, S.; Sun, C.; Zou, J. The clinical effect of different vertebral body height restoration rates after percutaneous kyphoplasty for osteoporotic vertebral compression fractures. BMC Musculoskelet. Disord. 2024, 25, 711. [Google Scholar] [CrossRef] [PubMed]
- Dai, C.; Liang, G.; Zhang, Y.; Dong, Y.; Zhou, X. Risk factors of vertebral re-fracture after PVP or PKP for osteoporotic vertebral compression fractures, especially in Eastern Asia: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 161. [Google Scholar] [CrossRef] [PubMed]
- Sahinturk, F.; Sonmez, E.; Ayhan, S.; Gulsen, S.; Yilmaz, C. The Influence of Percutaneous Vertebral Augmentation Techniques on Recompression in Patients with Osteoporotic Vertebral Compression Fractures. Percutaneous Vertebroplasty versus Balloon Kyphoplasty. World Neurosurg. 2023, 176, e447–e455. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.; Graffy, P.M.; Ziemlewicz, T.J.; Lee, S.J.; Summers, R.M.; Pickhardt, P.J. Opportunistic Osteoporosis Screening at Routine Abdominal and Thoracic CT: Normative L1 Trabecular Attenuation Values in More than 20 000 Adults. Radiology 2019, 291, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Aynaszyan, S.; Devia, L.G.; Parry, M.W.; Badve, S.; DelSole, E.M. Patterns of Misdiagnosis and Discordance in Detecting Osteoporosis: A Comparison of Dual-energy X-ray Absorptiometry and Lumbar Computed Tomography Hounsfield Units. Clin. Spine Surg. 2023, 36, E369–E374. [Google Scholar] [CrossRef] [PubMed]
- Black, D.M.; Cummings, S.R.; Karpf, D.B.; Cauley, J.A.; Thompson, D.E.; Nevitt, M.C.; Bauer, D.C.; Genant, H.K.; Haskell, W.L.; Marcus, R.; et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 1996, 348, 1535–1541. [Google Scholar] [CrossRef]
- Klazen, C.A.; Venmans, A.; de Vries, J.; van Rooij, W.J.; Jansen, F.H.; Blonk, M.C.; Lohle, P.N.; Juttmann, J.R.; Buskens, E.; van Everdingen, K.J.; et al. Percutaneous vertebroplasty is not a risk factor for new osteoporotic compression fractures: Results from VERTOS II. Am. J. Neuroradiol. 2010, 31, 1447–1450. [Google Scholar] [CrossRef]
- He, D.; Lou, C.; Yu, W.; Zhu, K.; Wu, Z.; Liu, F.; Chen, M.; Zheng, L.; Chen, Z.; Fan, S. Cement Distribution Patterns Are Associated with Recompression in Cemented Vertebrae After Percutaneous Vertebroplasty: A Retrospective Study. World Neurosurg. 2018, 120, e1–e7. [Google Scholar] [CrossRef]
- Viswanathan, V.K.; Shetty, A.P.; Rai, N.; Sindhiya, N.; Subramanian, S.; Rajasekaran, S. What is the role of CT-based Hounsfield unit assessment in the evaluation of bone mineral density in patients undergoing 1- or 2-level lumbar spinal fusion for degenerative spinal pathologies? A prospective study. Spine J. 2023, 23, 1427–1434. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Du, J.; Gao, L.; Hao, D.; Hui, H.; He, B.; Yan, L. Risk factors for bone cement displacement after percutaneous vertebral augmentation for osteoporotic vertebral compression fractures. Front. Surg. 2022, 9, 947212. [Google Scholar] [CrossRef]
- Wu, Y.; Zhu, S.; Li, Y.; Zhang, C.; Xia, W.; Zhu, Z.; Wang, K. Risk Factors for Bone Cement Displacement After Percutaneous Kyphoplasty in Osteoporotic Vertebral Fractures: A Retrospective Analysis. Med. Sci. Monit. 2024, 30, e945884. [Google Scholar] [CrossRef]
- Jeon, I.; Kim, S.W.; Yu, D. Paraspinal muscle fatty degeneration as a predictor of progressive vertebral collapse in osteoporotic vertebral compression fractures. Spine J. 2022, 22, 313–320. [Google Scholar] [CrossRef]
- Qi, J.; Hu, Y.; Yang, Z.; Dong, Y.; Zhang, X.; Hou, G.; Lv, Y.; Guo, Y.; Zhou, F.; Liu, B.; et al. Incidence, Risk Factors, and Outcomes of Symptomatic Bone Cement Displacement following Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fracture: A Single Center Study. J. Clin. Med. 2022, 11, 7530. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Tang, J.; Liu, H.; Gu, Z.; Zhang, Y.; Yu, S. A novel and convenient method to evaluate bone cement distribution following percutaneous vertebral augmentation. Sci. Rep. 2020, 10, 16320. [Google Scholar] [CrossRef] [PubMed]
- Xinyu, G.; Na, Z.; Haihong, Z.; Dingjun, H. Vertebral refracture after percutaneous vertebroplasty for osteoporotic vertebral compression fractures with and without brace wearing: A retrospective study of 300 patients. Front. Surg. 2023, 9, 1056729. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.P.; Bei, M.J.; Yan, C.Q.; Chang, J.Z. Analysis of the effect of percutaneous vertebroplasty in the treatment of thoracolumbar Kümmell’s disease with or without bone cement leakage. BMC Musculoskelet. Disord. 2021, 22, 10. [Google Scholar] [CrossRef]
- Han, X.; Meng, C. Correlation between anterior vertebral height recovery rate and new-onset adjacent vertebral body fracture after percutaneous vertebroplasty. Orthop. J. China 2019, 27, 885–889. [Google Scholar]
- Zhu, S.; Su, Q.; Zhang, Y.; Sun, Z.; Yin, P.; Hai, Y. Risk factors of cemented vertebral refracture after percutaneous vertebral augmentation: A systematic review and meta-analysis. Neuroradiology 2020, 62, 1353–1360. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Wang, G.; Hui, W.; Liu, B.; Liu, Z.; Sun, J. Percutaneous kyphoplasty for osteoporotic vertebral compression fractures improves spino-pelvic alignment and global sagittal balance maximally in the thoracolumbar region. PLoS ONE 2020, 15, e0228341. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Du, J.; Zhang, Y.; Gong, Y.; Zhang, B.; Qu, Z.; Hao, D.; He, B.; Yan, L. Predictive Factors for Bone Cement Displacement following Percutaneous Vertebral Augmentation in Kümmell’s Disease. J. Clin. Med. 2022, 11, 7479. [Google Scholar] [CrossRef]
- Li, J.; Xie, Y.; Sun, S.; Xue, C.; Xu, W.; Xu, C.; Xi, Z. Regional differences in bone mineral density biomechanically induce a higher risk of adjacent vertebral fracture after percutaneous vertebroplasty: A case-comparative study. Int. J. Surg. 2023, 109, 352–363. [Google Scholar] [CrossRef]
- Walker, M.D.; Shane, E. Postmenopausal Osteoporosis. N. Engl. J. Med. 2023, 389, 1979–1991. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Lin, Y.; Kong, M.; Chen, J.; Gao, W.; Fan, J.; Wang, J.; Chen, Z. A nomogram for predicting the risk of new vertebral compression fracture after percutaneous kyphoplasty. Eur. J. Med. Res. 2023, 28, 280. [Google Scholar] [CrossRef] [PubMed]
- Svejme, O.; Ahlborg, H.G.; Nilsson, J.; Karlsson, M.K. Low BMD is an independent predictor of fracture and early menopause of mortality in post-menopausal women—A 34-year prospective study. Maturitas 2013, 74, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.X.; Guo, D.Q.; Zhang, S.C.; Liang, D.; Yuan, K.; Mo, G.Y.; Li, D.X.; Guo, H.Z.; Tang, Y.; Luo, P.J. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP). Int. Orthop. 2018, 42, 2131–2139. [Google Scholar] [CrossRef]
- Long, Y.; Yi, W.; Yang, D. Advances in Vertebral Augmentation Systems for Osteoporotic Vertebral Compression Fractures. Pain Res. Manag. 2020, 2020, 3947368. [Google Scholar] [CrossRef] [PubMed]
- Korovessis, P.; Vardakastanis, K.; Repantis, T.; Vitsas, V. Balloon kyphoplasty versus KIVA vertebral augmentation--comparison of 2 techniques for osteoporotic vertebral body fractures: A prospective randomized study. Spine 2013, 38, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Otten, L.A.; Bornemnn, R.; Jansen, T.R.; Kabir, K.; Pennekamp, P.H.; Wirtz, D.C.; Stuwe, B.; Pflugmacher, R. Comparison of balloon kyphoplasty with the new Kiva® VCF system for the treatment of vertebral compression fractures. Pain Physician 2013, 16, E505–E512. [Google Scholar] [CrossRef]
- Hu, X.; Zhang, Z.; Yang, Y.; Zhang, G.; Cao, S.; Yu, B.; Zhang, Y. Enhanced bone cement distribution in percutaneous vertebroplasty using a curved guide wire: A propensity score matching analysis. BMC Musculoskelet. Disord. 2024, 25, 835. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Wan, Y.; Ma, L.; Dong, L.; Yuan, W. Percutaneous Curved Vertebroplasty Decrease the Risk of Cemented Vertebra Refracture Compared with Bilateral Percutaneous Kyphoplasty in the Treatment of Osteoporotic Vertebral Compression Fractures. Clin. Interv. Aging 2024, 19, 289–301. [Google Scholar] [CrossRef]
- Zhang, G.; Li, J.; Zhang, L.; Song, J.; Shao, J.; Lv, C.; Bai, T.; Du, Y.; Xi, Y. Biomechanical Effect of Different Posterior Fixation Techniques on Stability and Adjacent Segment Degeneration in Treating Thoracolumbar Burst Fracture with Osteoporosis: A Finite Element Analysis. Spine 2024, 49, E229–E238. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.; Zhou, Q.; Jin, X.; Zhang, J. Cement-augmented pedicle screw for thoracolumbar degenerative diseases with osteoporosis: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2023, 18, 631. [Google Scholar] [CrossRef]




| Nonvertebral Refracture Group (n = 143) | Augmented Vertebral Refracture Group (n = 22) | χ2/t Value/z Value | p Value | |
|---|---|---|---|---|
| Age (years) | 73.000 (65.500, 80.000) | 78.500 (67.500, 81.75) | −1.831 | 0.067 * |
| Gender | 0.343 | 0.558 | ||
| Male [n (%)] | 31 (21.7%) | 6 (27.3%) | ||
| Female [n (%)] | 112 (78.3%) | 16 (72.7%) | ||
| BMI (kg/cm2) | 24.358 ± 3.469 | 24.024 ± 3.709 | 0.400 | 0.489 |
| Underlying diseases | ||||
| Hypertension [n (%)] | 65 (45.5%) | 10 (45.5%) | <0.001 | 1.000 |
| Diabetes [n (%)] | 30 (21.0%) | 5 (22.7%) | 0.035 | 0.852 |
| Cardiovascular and cerebrovascular diseases [n (%)] | 32 (22.4%) | 8 (36.4%) | 2.031 | 0.154 |
| History of fracture at other sites [n (%)] | 22 (15.4%) | 3 (13.6%) | <0.001 | 1.000 |
| Hu at upper lumbar levels | 83.000 (68.000, 100.000) | 66.000 (61.250, 80.250) | −3.110 | 0.002 * |
| Primary fractured vertebral segment | 7.259 | 0.027 | ||
| Thoracic segment [n (%)] | 14 (9.8%) | 1 (4.5%) | ||
| Thoracolumbar junction (T11-L2) [n (%)] | 109 (76.2%) | 21 (95.5%) | ||
| Lumbar segment [n (%)] | 20 (14.0%) | 0 | ||
| Preoperative IVC | 91 (63.6%) | 22 (100.0%) | 10.057 | 0.002 |
| Preoperative vertebral height (cm) | 1.559 ± 0.410 | 1.514 ± 0.380 | 0.489 | 0.502 |
| Collapse of vertebral body (%) | 24.301 (14.643, 34.963) | 34.379 (16.520, 44.591) | −1.544 | 0.123 * |
| Preoperative vertebral anterior margin height (cm) | 1.811 ± 0.478 | 1.748 ± 0.470 | 0.573 | 0.518 |
| Postoperative vertebral anterior margin height (cm) | 1.996 ± 0.465 | 2.233 ± 0.461 | −2.229 | 0.578 |
| Recovery rate of vertebral anterior margin height (%) | 5.904 (1.099, 15.621) | 17.068 (9.541, 33.189) | −3.554 | <0.001 * |
| Preoperative Cobb angle (°) | 14.000 (8.800, 19.000) | 14.650 (10.550, 21.775) | −0.988 | 0.323 * |
| Postoperative Cobb angle (°) | 12.700 (7.900, 18.400) | 7.500 (4.325, 13.150) | −2.495 | 0.013 * |
| Restoration of Cobb angle (%) | 4.368 (1.917, 12.050) | 43.316 (36.996, 56.754) | −5.474 | <0.001 * |
| Volume of cement (mL) | 2.500 (2.250, 3.000) | 2.500 (2.500, 2.500) | −1.077 | 0.281 * |
| Sagittal position of cement filling | 4.852 | 0.088 | ||
| 1/3 of vertebral body [n (%)] | 11 (7.7%) | 2 (9.1%) | ||
| 2/3 of vertebral body [n (%)] | 45 (31.5%) | 12 (54.5%) | ||
| Whole vertebral body [n (%)] | 87 (60.8%) | 8 (36.4%) | ||
| Contact between bone cement and endplate | 18.474 | <0.001 | ||
| Non-cement–endplate contact [n (%)] | 8 (5.6%) | 3 (13.6%) | ||
| Contact with upper vertebral endplates [n (%)] | 25 (17.5%) | 11 (50.0%) | ||
| Contact with lower vertebral endplates [n (%)] | 40 (28.0%) | 6 (27.3%) | ||
| Contact with upper and lower vertebral endplates [n (%)] | 70 (49.0%) | 2 (9.1%) | ||
| Distance between bone cement and vertebral endplates (cm) | 0.160 (0, 0.430) | 0.380 (0.203, 0.598) | −3.123 | 0.002 * |
| Bone–cement distribution score | 7.000 (5.000, 8.000) | 5.000 (4.250, 6.000) | −3.761 | <0.001 * |
| Bone cement leakage | 12.696 | 0.013 | ||
| No leakage [n (%)] | 99 (69.2%) | 11 (50.0%) | ||
| Anterior leakage [n (%)] | 17 (11.9%) | 4 (18.2%) | ||
| Posterior leakage [n (%)] | 6 (4.2%) | 4 (18.2%) | ||
| Lateral leakage [n (%)] | 6 (4.2%) | 3 (13.6%) | ||
| Disc leakage [n (%)] | 15 (10.5%) | 0 | ||
| Postoperative anti-osteoporosis treatment | 133 (93.0%) | 9 (40.9%) | 43.139 | <0.001 |
| B Value | Standard Error | Wald Value | p Value | OR | 95% CI | |
|---|---|---|---|---|---|---|
| Hu at upper lumbar levels | −0.036 | 0.024 | 2.269 | 0.132 | 0.965 | 0.920~1.011 |
| Thoracolumbar junction | 16.777 | >2.000 | <0.001 | 0.995 | >1.000 | - |
| Preoperative IVC | 21.605 | >2.000 | <0.001 | 0.996 | >1.000 | - |
| Recovery rate of vertebral anterior margin height | 0.026 | 0.100 | 0.070 | 0.791 | 1.027 | 0.844~1.249 |
| Postoperative Cobb angle | −0.187 | 0.218 | 0.741 | 0.389 | 0.829 | 0.541~1.271 |
| Restoration of Cobb angle | 0.068 | 0.018 | 14.467 | <0.001 | 1.070 | 1.034~1.109 |
| Contact between bone cement and endplate | ||||||
| Non-cement–endplate contact * | 1.057 | 0.787 | ||||
| Contact with upper vertebral endplates | 2.541 | 12.172 | 0.044 | 0.835 | 12.696 | - |
| Contact with lower vertebral endplates | 5.361 | 12.478 | 0.185 | 0.667 | 212.964 | - |
| Contact with upper and lower vertebral endplates | 6.088 | 12.771 | 0.227 | 0.634 | 440.691 | - |
| Distance between bone cement and vertebral endplates | 1.166 | 1.154 | 1.020 | 0.312 | 3.209 | 0.334~30.841 |
| Bone–cement distribution score | −0.311 | 0.697 | 0.199 | 0.655 | 0.733 | 0.187~2.870 |
| Bone cement leakage | ||||||
| No leakage * | 2.319 | 0.677 | ||||
| Anterior leakage | 5.190 | 4.306 | 1.453 | 0.228 | 179.557 | 0.039~830,739.907 |
| Posterior leakage | 1.435 | 3.784 | 0.144 | 0.704 | 4.200 | 0.003~6986.566 |
| Lateral leakage | 5.791 | 3.824 | 2.293 | 0.130 | >1.000 | 0.182~588,576.042 |
| Disc leakage | −14.362 | >2.000 | <0.001 | 0.999 | <1.000 | - |
| Postoperative anti-osteoporosis treatment | −3.878 | 1.277 | 9.221 | 0.002 | 0.021 | 0.002~0.253 |
| AUC | p Value | 95% CI | Optimal Cutoff Value | Sensitivity | Specificity | Youden’s Index | |
|---|---|---|---|---|---|---|---|
| Restoration of Cobb angle | 0.863 | <0.001 | 0.768~0.958 | 36.432 | 0.818 | 0.909 | 0.727 |
| Absence of postoperative anti-osteoporosis treatment | 0.760 | <0.001 | 0.631~0.890 | - | 0.591 | 0.930 | 0.521 |
| Logistic regression | 0.977 | <0.001 | 0.939~1.000 | 0.955 | 0.951 | 0.906 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Y.; Zhu, S.; Li, Y.; Zhang, C.; Xia, W.; Zhu, Z.; Wang, K. Analysis of Risk Factors for Augmented Vertebral Refracture After Percutaneous Kyphoplasty in Osteoporotic Vertebral Compression Fractures. J. Clin. Med. 2025, 14, 329. https://doi.org/10.3390/jcm14020329
Wu Y, Zhu S, Li Y, Zhang C, Xia W, Zhu Z, Wang K. Analysis of Risk Factors for Augmented Vertebral Refracture After Percutaneous Kyphoplasty in Osteoporotic Vertebral Compression Fractures. Journal of Clinical Medicine. 2025; 14(2):329. https://doi.org/10.3390/jcm14020329
Chicago/Turabian StyleWu, Yonghao, Shuaiqi Zhu, Yuqiao Li, Chenfei Zhang, Weiwei Xia, Zhenqi Zhu, and Kaifeng Wang. 2025. "Analysis of Risk Factors for Augmented Vertebral Refracture After Percutaneous Kyphoplasty in Osteoporotic Vertebral Compression Fractures" Journal of Clinical Medicine 14, no. 2: 329. https://doi.org/10.3390/jcm14020329
APA StyleWu, Y., Zhu, S., Li, Y., Zhang, C., Xia, W., Zhu, Z., & Wang, K. (2025). Analysis of Risk Factors for Augmented Vertebral Refracture After Percutaneous Kyphoplasty in Osteoporotic Vertebral Compression Fractures. Journal of Clinical Medicine, 14(2), 329. https://doi.org/10.3390/jcm14020329






