Prefrontal Cortical Near-Infrared Spectroscopy for Acute Pain Assessment in Infants: A Feasibility Study
Abstract
1. Introduction
2. Patients and Methods
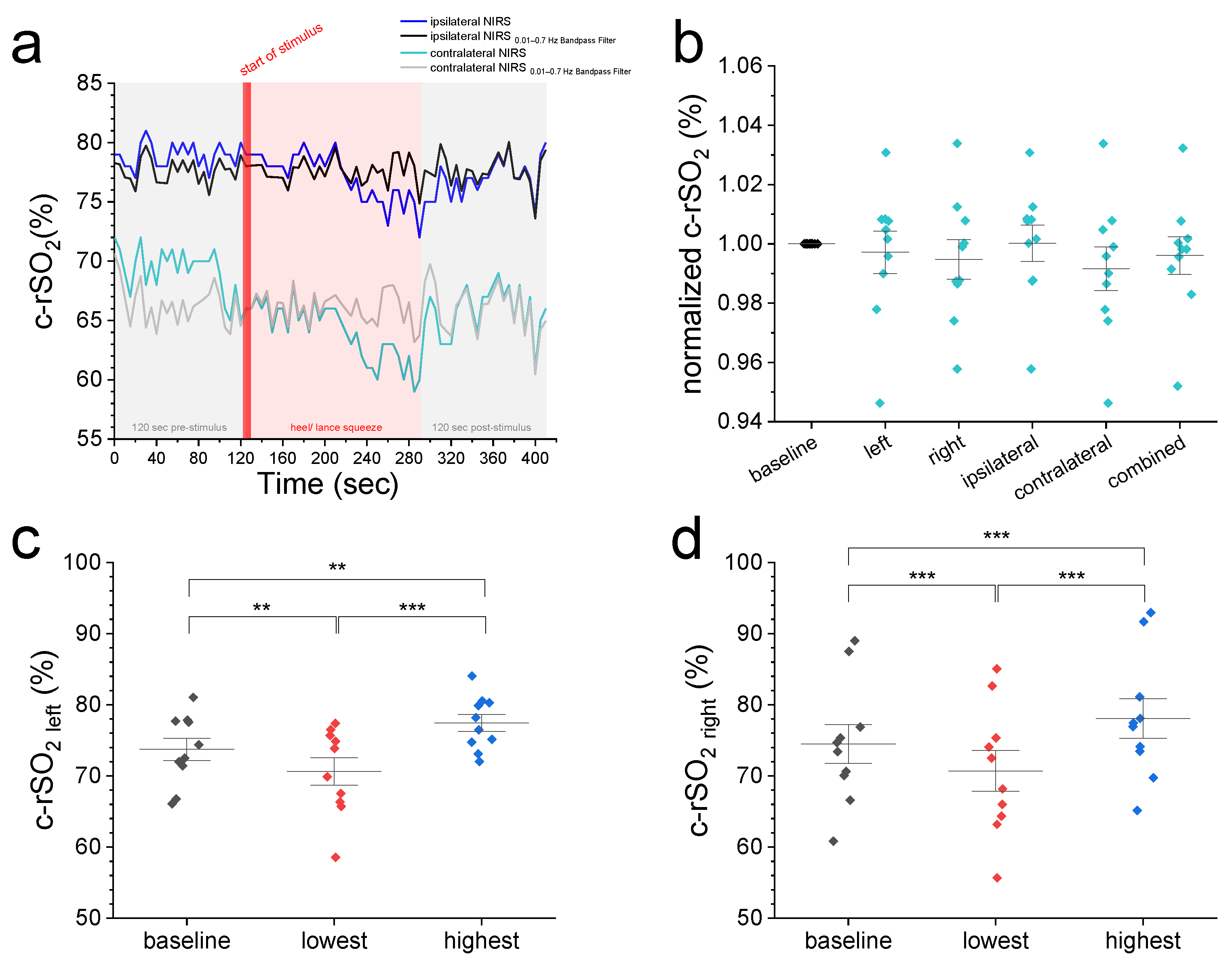
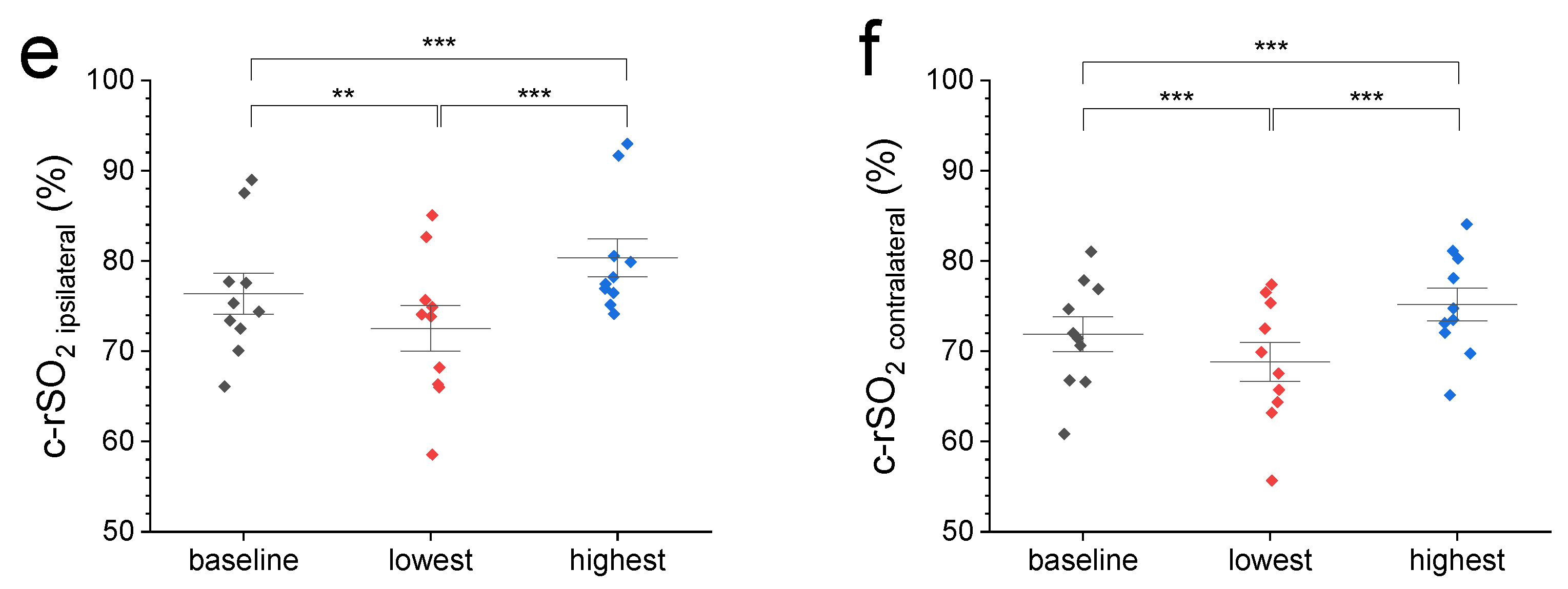
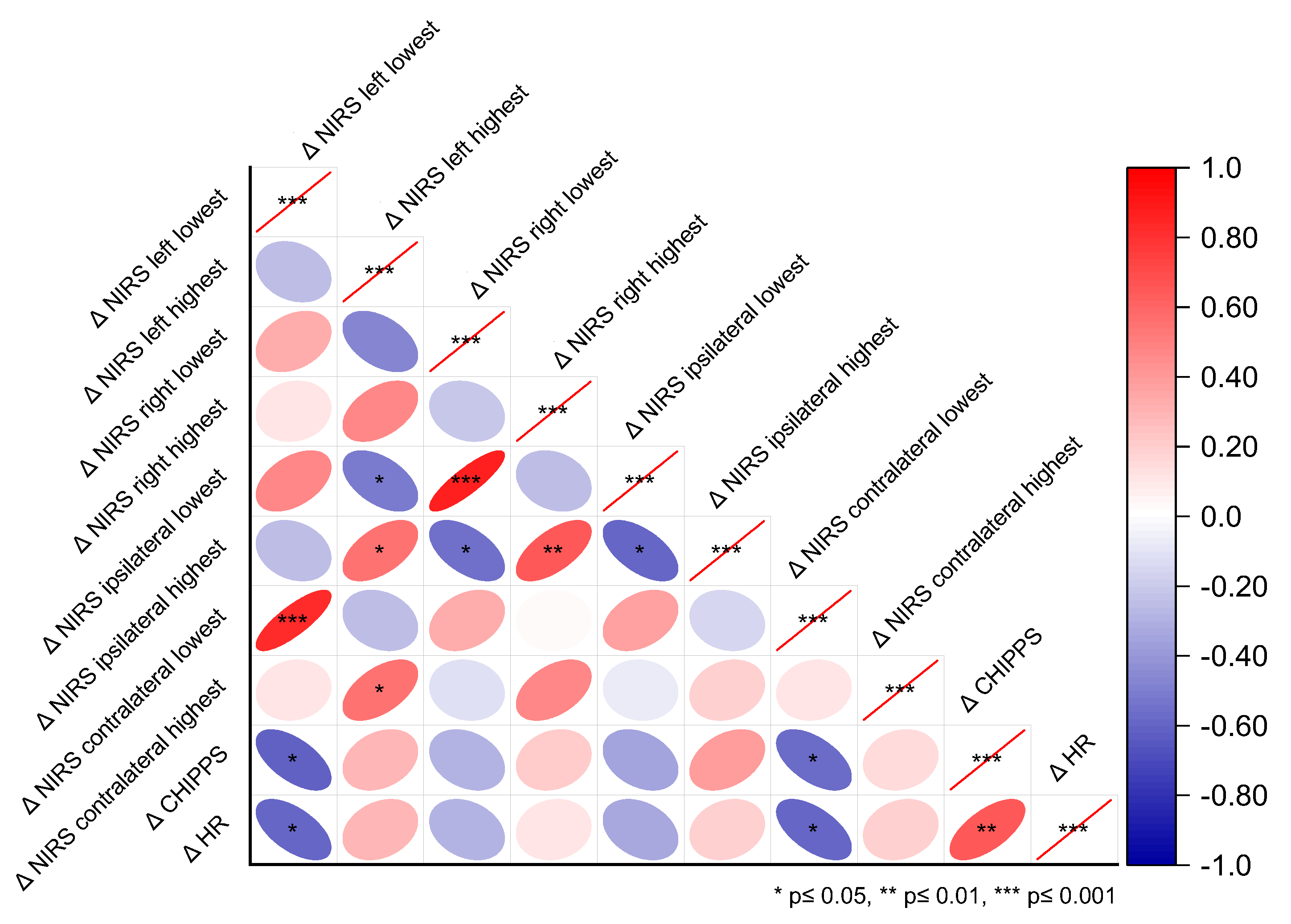
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CHIPPS | Children’s and Infant’s Postoperative Pain score |
| c-FTOE | Cerebral fractional tissue oxygen extraction |
| BOLD | Blood oxygenation level dependent fMRI |
| BGA | Blood gas analysis |
| BR | Breathing rate |
| FA | Frontal asymmetry |
| HR | Heart rate |
| NIRS | Near-infrared spectroscopy |
| HLS | Heel lance/squeeze |
| fMRI | Functional magnetic resonance imaging |
| fNIRS | Functional near-infrared spectroscopy |
| EEG | Electroencephalography |
| NIPS | Neonatal Infant Pain Scale |
| PIPP-R | Infant Pain Profile—Revised |
| ANOVA | Analysis of variance |
| ROP | Retinopathy of prematurity |
| c-rSO2 | Cerebral regional oxygenation |
| SpO2 | Peripheral oxygen saturation |
References
- Craig, K.D.; Whitfield, M.F.; Grunau, R.V.E.; Linton, J.; Hadjistavropoulos, H.D. Pain in the Preterm Neonate: Behavioural and Physiological Indices. Pain 1993, 52, 287–299. [Google Scholar] [CrossRef] [PubMed]
- Waxman, J.A.; Pillai Riddell, R.R.; Tablon, P.; Schmidt, L.A.; Pinhasov, A. Development of Cardiovascular Indices of Acute Pain Responding in Infants: A Systematic Review. Pain Res. Manag. 2016, 2016, 8458696. [Google Scholar] [CrossRef] [PubMed]
- Vinall, J.; Miller, S.P.; Bjornson, B.H.; Fitzpatrick, K.P.V.; Poskitt, K.J.; Brant, R.; Synnes, A.R.; Cepeda, I.L.; Grunau, R.E. Invasive Procedures in Preterm Children: Brain and Cognitive Development at School Age. Pediatrics 2014, 133, 412–421. [Google Scholar] [CrossRef]
- Doesburg, S.M.; Chau, C.M.; Cheung, T.P.L.; Moiseev, A.; Ribary, U.; Herdman, A.T.; Miller, S.P.; Cepeda, I.L.; Synnes, A.; Grunau, R.E. Neonatal Pain-Related Stress, Functional Cortical Activity and Visual-Perceptual Abilities in School-Age Children Born at Extremely Low Gestational Age. Pain 2013, 154, 1946–1952. [Google Scholar] [CrossRef]
- Grunau, R.E.; Whitfield, M.F.; Petrie-Thomas, J.; Synnes, A.R.; Cepeda, I.L.; Keidar, A.; Rogers, M.; MacKay, M.; Hubber-Richard, P.; Johannesen, D. Neonatal Pain, Parenting Stress and Interaction, in Relation to Cognitive and Motor Development at 8 and 18 Months in Preterm Infants. Pain 2009, 143, 138–146. [Google Scholar] [CrossRef]
- Hermann, C.; Hohmeister, J.; Demirakça, S.; Zohsel, K.; Flor, H. Long-Term Alteration of Pain Sensitivity in School-Aged Children with Early Pain Experiences. Pain 2006, 125, 278–285. [Google Scholar] [CrossRef]
- Slater, R.; Fabrizi, L.; Worley, A.; Meek, J.; Boyd, S.; Fitzgerald, M. Premature Infants Display Increased Noxious-Evoked Neuronal Activity in the Brain Compared to Healthy Age-Matched Term-Born Infants. Neuroimage 2010, 52, 583–589. [Google Scholar] [CrossRef]
- Maitre, N.L.; Key, A.P.; Chorna, O.D.; Slaughter, J.C.; Matusz, P.J.; Wallace, M.T.; Murray, M.M. The Dual Nature of Early-Life Experience on Somatosensory Processing in the Human Infant Brain. Curr. Biol. 2017, 27, 1048–1054. [Google Scholar] [CrossRef]
- Valeri, B.O.; Ranger, M.; Chau, C.M.Y.; Cepeda, I.L.; Synnes, A.; Linhares, M.B.M.; Grunau, R.E. Neonatal Invasive Procedures Predict Pain Intensity at School Age in Children Born Very Preterm. Clin. J. Pain 2016, 32, 1086–1093. [Google Scholar] [CrossRef]
- Walker, S.M.; Melbourne, A.; O’Reilly, H.; Beckmann, J.; Eaton-Rosen, Z.; Ourselin, S.; Marlow, N. Somatosensory Function and Pain in Extremely Preterm Young Adults from the UK EPICure Cohort: Sex-Dependent Differences and Impact of Neonatal Surgery. Br. J. Anaesth. 2018, 121, 623–635. [Google Scholar] [CrossRef]
- Benoit, B.; Martin-Misener, R.; Newman, A.; Latimer, M.; Campbell-Yeo, M. Neurophysiological Assessment of Acute Pain in Infants: A Scoping Review of Research Methods. Acta Paediatr. 2017, 106, 1053–1066. [Google Scholar] [CrossRef]
- Coghill, R.C.; McHaffie, J.G.; Yen, Y.-F. Neural Correlates of Interindividual Differences in the Subjective Experience of Pain. Proc. Natl. Acad. Sci. USA 2003, 100, 8538–8542. [Google Scholar] [CrossRef] [PubMed]
- Schnitzler, A.; Ploner, M. Neurophysiology and Functional Neuroanatomy of Pain Perception. J. Clin. Neurophysiol. 2000, 17, 592–603. [Google Scholar] [CrossRef] [PubMed]
- Gursul, D.; Hartley, C.; Slater, R. Nociception and the Neonatal Brain. Semin. Fetal Neonatal Med. 2019, 24, 101016. [Google Scholar] [CrossRef] [PubMed]
- Hartley, C.; Duff, E.P.; Green, G.; Mellado, G.S.; Worley, A.; Rogers, R.; Slater, R. Nociceptive Brain Activity as a Measure of Analgesic Efficacy in Infants. Sci. Transl. Med. 2017, 9, eaah6122. [Google Scholar] [CrossRef]
- Roche-Labarbe, N.; Wallois, F.; Ponchel, E.; Kongolo, G.; Grebe, R. Coupled Oxygenation Oscillation Measured by NIRS and Intermittent Cerebral Activation on EEG in Premature Infants. Neuroimage 2007, 36, 718–727. [Google Scholar] [CrossRef]
- Bartocci, M.; Bergqvist, L.L.; Lagercrantz, H.; Anand, K.J.S. Pain Activates Cortical Areas in the Preterm Newborn Brain. Pain 2006, 122, 109–117. [Google Scholar] [CrossRef]
- Slater, R.; Cantarella, A.; Gallella, S.; Worley, A.; Boyd, S.; Meek, J.; Fitzgerald, M. Cortical Pain Responses in Human Infants. J. Neurosci. 2006, 26, 3662–3666. [Google Scholar] [CrossRef]
- Bembich, S.; Brovedani, P.; Cont, G.; Travan, L.; Grassi, V.; Demarini, S. Pain Activates a Defined Area of the Somatosensory and Motor Cortex in Newborn Infants. Acta Paediatr. 2015, 104, e530–e533. [Google Scholar] [CrossRef]
- Verriotis, M.; Fabrizi, L.; Lee, A.; Cooper, R.J.; Fitzgerald, M.; Meek, J. Mapping Cortical Responses to Somatosensory Stimuli in Human Infants with Simultaneous Near-Infrared Spectroscopy and Event-Related Potential Recording. eNeuro 2016, 3, ENEURO.0026-16.2016. [Google Scholar] [CrossRef]
- Beken, S.; Hirfanoğlu, İ.M.; Gücüyener, K.; Ergenekon, E.; Turan, Ö.; Ünal, S.; Altuntaş, N.; Kazancı, E.; Kulalı, F.; Türkyılmaz, C.; et al. Cerebral Hemodynamic Changes and Pain Perception During Venipuncture. J. Child Neurol. 2014, 29, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Sava, S.; Lebel, A.A.; Leslie, D.S.; Drosos, A.; Berde, C.; Becerra, L.; Borsook, D. Challenges of Functional Imaging Research of Pain in Children. Mol. Pain 2009, 5, 1744–8069. [Google Scholar] [CrossRef]
- Goksan, S.; Baxter, L.; Moultrie, F.; Duff, E.; Hathway, G.; Hartley, C.; Tracey, I.; Slater, R. The Influence of the Descending Pain Modulatory System on Infant Pain-Related Brain Activity. Elife 2018, 7, e37125. [Google Scholar] [CrossRef]
- Goksan, S.; Hartley, C.; Emery, F.; Cockrill, N.; Poorun, R.; Moultrie, F.; Rogers, R.; Campbell, J.; Sanders, M.; Adams, E.; et al. FMRI Reveals Neural Activity Overlap between Adult and Infant Pain. Elife 2015, 4, e06356. [Google Scholar] [CrossRef] [PubMed]
- Apkarian, A.V.; Bushnell, M.C.; Treede, R.; Zubieta, J. Human Brain Mechanisms of Pain Perception and Regulation in Health and Disease. Eur. J. Pain 2005, 9, 463. [Google Scholar] [CrossRef]
- Aasted, C.M.; Yücel, M.A.; Steele, S.C.; Peng, K.; Boas, D.A.; Becerra, L.; Borsook, D. Frontal Lobe Hemodynamic Responses to Painful Stimulation: A Potential Brain Marker of Nociception. PLoS ONE 2016, 11, e0165226. [Google Scholar] [CrossRef]
- Lee, C.-H.; Sugiyama, T.; Kataoka, A.; Kudo, A.; Fujino, F.; Chen, Y.-W.; Mitsuyama, Y.; Nomura, S.; Yoshioka, T. Analysis for Distinctive Activation Patterns of Pain and Itchy in the Human Brain Cortex Measured Using Near Infrared Spectroscopy (NIRS). PLoS ONE 2013, 8, e75360. [Google Scholar] [CrossRef]
- Sakuma, S.; Inamoto, K.; Higuchi, N.; Ariji, Y.; Nakayama, M.; Izumi, M. Experimental Pain in the Gingiva and Its Impact on Prefrontal Cortical Hemodynamics: A Functional near-Infrared Spectroscopy Study. Neurosci. Lett. 2014, 575, 74–79. [Google Scholar] [CrossRef]
- Yücel, M.A.; Aasted, C.M.; Petkov, M.P.; Borsook, D.; Boas, D.A.; Becerra, L. Specificity of Hemodynamic Brain Responses to Painful Stimuli: A Functional near-Infrared Spectroscopy Study. Sci. Rep. 2015, 5, 9469. [Google Scholar] [CrossRef]
- Becerra, L.; Aasted, C.M.; Boas, D.A.; George, E.; Yücel, M.A.; Kussman, B.D.; Kelsey, P.; Borsook, D. Brain Measures of Nociception Using Near-Infrared Spectroscopy in Patients Undergoing Routine Screening Colonoscopy. Pain 2016, 157, 840–848. [Google Scholar] [CrossRef]
- Büttner, W.; Finke, W. Analysis of Behavioural and Physiological Parameters for the Assessment of Postoperative Analgesic Demand in Newborns, Infants and Young Children: A Comprehensive Report on Seven Consecutive Studies. Pediatr. Anesth. 2000, 10, 303–318. [Google Scholar] [CrossRef]
- Kumar, S.; Priyadarshi, M.; Singh, P.; Pallapothu, B.; Chaurasia, S.; Basu, S. Correlation of Clinical Pain Scores with Cerebral Oxygenation in Preterm Neonates during Acute Painful Procedures: A Prospective Observational Study. J. Perinatol. 2023, 43, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zhang, J.; Chen, X.; Yang, Y.; Qiu, J.; Lu, K.; Cheng, R. Effectiveness of Gentle Human Touch for Pain Control During Examination for Retinopathy of Pre-Maturity: A Randomized Controlled Trial. Front. Pediatr. 2020, 8, 608378. [Google Scholar] [CrossRef] [PubMed]
- Ozawa, M.; Kanda, K.; Hirata, M.; Kusakawa, I.; Suzuki, C. Influence of Repeated Painful Procedures on Prefrontal Cortical Pain Responses in Newborns. Acta Paediatr. 2011, 100, 198–203. [Google Scholar] [CrossRef]
- Tanida, M.; Katsuyama, M.; Sakatani, K. Relation between Mental Stress-Induced Prefrontal Cortex Activity and Skin Conditions: A near-Infrared Spectroscopy Study. Brain Res. 2007, 1184, 210–216. [Google Scholar] [CrossRef]
- Pellicer, A.; de Boode, W.; Dempsey, E.; Greisen, G.; Mintzer, J.; Naulaers, G.; Pichler, G.; Roehr, C.C.; Roll, C.; Schwarz, C.; et al. Cerebral Near-Infrared Spectroscopy Guided Neonatal Intensive Care Management for the Preterm Infant. Pediatr. Res. 2024. [Google Scholar] [CrossRef]
- Kooi, E.M.W.; Mintzer, J.P.; Rhee, C.J.; Ergenekon, E.; Schwarz, C.E.; Pichler, G.; de Boode, W.P.; Alarcón, A.; Alderliesten, T.; Austin, T.; et al. Neonatal Somatic Oxygenation and Perfusion Assessment Using Near-Infrared Spectroscopy. Pediatr. Res. 2024, 96, 1180–1194. [Google Scholar] [CrossRef]
- Levy, P.T.; Pellicer, A.; Schwarz, C.E.; Neunhoeffer, F.; Schuhmann, M.U.; Breindahl, M.; Fumagelli, M.; Mintzer, J.; de Boode, W.; Alarcon, A.; et al. Near-Infrared Spectroscopy for Perioperative Assessment and Neonatal Interventions. Pediatr. Res. 2024, 96, 922–932. [Google Scholar] [CrossRef]
- Kurihara, K.; Kawaguchi, H.; Obata, T.; Ito, H.; Sakatani, K.; Okada, E. The Influence of Frontal Sinus in Brain Activation Measurements by Near-Infrared Spectroscopy Analyzed by Realistic Head Models. Biomed. Opt. Express 2012, 3, 2121. [Google Scholar] [CrossRef]
- Gregory, A.J.; Hatem, M.A.; Yee, K.; Grocott, H.P. Optimal Placement of Cerebral Oximeter Monitors to Avoid the Frontal Sinus as Determined by Computed Tomography. J. Cardiothorac. Vasc. Anesth. 2016, 30, 127–133. [Google Scholar] [CrossRef]
- Devi, R.; Priyadarshi, M.; Singh, P.; Chaurasia, S.; Basu, S. Neonatal Pain Response to Various Heel Prick Devices: A Randomized Controlled Trial. Indian Pediatr. 2023, 60, 893–898. [Google Scholar] [CrossRef]
- Hwang, M.-J.; Seol, G.H. Cerebral Oxygenation and Pain of Heel Blood Sampling Using Manual and Automatic Lancets in Premature Infants. J. Perinat. Neonatal Nurs. 2015, 29, 356–362. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, L.; Lei, X.; Dong, W.; Zhang, L. Pain-Related Changes in CrSO2 among Premature Infants Undergoing PICC Insertion. J. Matern.-Fetal Neonatal Med. 2023, 36, 2241976. [Google Scholar] [CrossRef]
- Kara, N.; Arman, D.; Seymen, Z.; Gül, A.; Cömert, S. Effects of Fentanyl and Sucrose on Pain in Retinopathy Examinations with Pain Scale, near-Infrared Spectroscopy, and Ultrasonography: A Randomized Trial. World J. Pediatr. 2023, 19, 873–882. [Google Scholar] [CrossRef]
- Ranger, M.; Albert, A.; MacLean, K.; Holsti, L. Cerebral Hemodynamic Response to a Therapeutic Bed for Procedural Pain Management in Preterm Infants in the NICU: A Randomized Controlled Trial. Pain Rep. 2021, 6, e890. [Google Scholar] [CrossRef]
- Gélinas, C.; Choinière, M.; Ranger, M.; Denault, A.; Deschamps, A.; Johnston, C. Toward a New Approach for the Detection of Pain in Adult Patients Undergoing Cardiac Surgery: Near-Infrared Spectroscopy—A Pilot Study. Heart Lung 2010, 39, 485–493. [Google Scholar] [CrossRef]
- Gélinas, C.; Boitor, M.; Ranger, M.; Johnston, C.C.; de Marchie, M.; Cervero, F.; Choinière, M. Is near Infrared Spectroscopy Valid for the Detection of Procedural Pain in Postoperative Cardiac Surgery Intensive Care Unit Adults? J. Near Infrared Spectrosc. 2017, 25, 391–399. [Google Scholar] [CrossRef]
- Mukaihara, K.; Hasegawa-Moriyama, M.; Kanmura, Y. Contralateral Cerebral Hemoglobin Oxygen Saturation Changes in Patients Undergoing Thoracotomy with General Anesthesia with or without Paravertebral Block: A Randomized Controlled Trial. J. Anesth. 2017, 31, 829–836. [Google Scholar] [CrossRef]
- Wiech, K.; Ploner, M.; Tracey, I. Neurocognitive Aspects of Pain Perception. Trends Cogn. Sci. 2008, 12, 306–313. [Google Scholar] [CrossRef]
- Dedovic, K.; Duchesne, A.; Andrews, J.; Engert, V.; Pruessner, J.C. The Brain and the Stress Axis: The Neural Correlates of Cortisol Regulation in Response to Stress. Neuroimage 2009, 47, 864–871. [Google Scholar] [CrossRef]
- Ozdemir, H.; Bilgen, H.; Gokulu, G.; Memisoglu, A.; Ozek, E. Does Repeated Painful Stimuli Change Cerebral Near-Infrared Spectroscopy Response in Healthy, Term, Large for Gestational Age Newborns? Clin. J. Pain 2020, 36, 110–116. [Google Scholar] [CrossRef]
- Buratto, E.; Horton, S.; Konstantinov, I.E. So near, yet so Far: Is Isolated Cerebral near-Infrared Spectroscopy in Neonates Nearly as Useful as It Is Noninvasive? J. Thorac. Cardiovasc. Surg. 2017, 154, 1054–1055. [Google Scholar] [CrossRef]
- Fernandez, M.; Blass, E.M.; Hernandez-Reif, M.; Field, T.; Diego, M.; Sanders, C. Sucrose Attenuates a Negative Electroencephalographic Response to an Aversive Stimulus for Newborns. J. Dev. Behav. Pediatr. 2003, 24, 261–266. [Google Scholar] [CrossRef]
- Saito, Y.; Fukuhara, R.; Aoyama, S.; Toshima, T. Frontal Brain Activation in Premature Infants’ Response to Auditory Stimuli in Neonatal Intensive Care Unit. Early Hum. Dev. 2009, 85, 471–474. [Google Scholar] [CrossRef]
- Missana, M.; Grigutsch, M.; Grossmann, T. Developmental and Individual Differences in the Neural Processing of Dynamic Expressions of Pain and Anger. PLoS ONE 2014, 9, e93728. [Google Scholar] [CrossRef][Green Version]
- Mamie, C.; Rebsamen, M.C.; Morris, M.A.; Morabia, A. First Evidence of a Polygenic Susceptibility to Pain in a Pediatric Cohort. Anesth. Analg. 2013, 116, 170–177. [Google Scholar] [CrossRef]
- Upadhyay, J.; Kumar, S.; Singh, P.; Basu, S. Cortical Hemodynamic Activity and Pain Perception during Insertion of Feeding Tubes in Preterm Neonates: A Randomized Controlled Cross-over Trial. J. Perinatol. 2022, 42, 121–125. [Google Scholar] [CrossRef]
- Bell, J.T.; Loomis, A.K.; Butcher, L.M.; Gao, F.; Zhang, B.; Hyde, C.L.; Sun, J.; Wu, H.; Ward, K.; Harris, J.; et al. Differential Methylation of the TRPA1 Promoter in Pain Sensitivity. Nat. Commun. 2014, 5, 2978. [Google Scholar] [CrossRef]
- Matic, M.; van den Bosch, G.E.; de Wildt, S.N.; Tibboel, D.; van Schaik, R.H.N. Genetic Variants Associated with Thermal Pain Sensitivity in a Paediatric Population. Pain 2016, 157, 2476–2482. [Google Scholar] [CrossRef]
- Johnston, C.C.; Stevens, B.J. Experience in a Neonatal Intensive Care Unit Affects Pain Response. Pediatrics 1996, 98, 925–930. [Google Scholar]
- Taddio, A. Conditioning and Hyperalgesia in Newborns Exposed to Repeated Heel Lances. JAMA 2002, 288, 857. [Google Scholar] [CrossRef] [PubMed]
- Hohmeister, J.; Demirakça, S.; Zohsel, K.; Flor, H.; Hermann, C. Responses to Pain in School-aged Children with Experience in a Neonatal Intensive Care Unit: Cognitive Aspects and Maternal Influences. Eur. J. Pain 2009, 13, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Hohmeister, J.; Kroll, A.; Wollgarten-Hadamek, I.; Zohsel, K.; Demirakça, S.; Flor, H.; Hermann, C. Cerebral Processing of Pain in School-Aged Children with Neonatal Nociceptive Input: An Exploratory FMRI Study. Pain 2010, 150, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Verriotis, M.; Jones, L.; Whitehead, K.; Laudiano-Dray, M.; Panayotidis, I.; Patel, H.; Meek, J.; Fabrizi, L.; Fitzgerald, M. The Distribution of Pain Activity across the Human Neonatal Brain Is Sex Dependent. Neuroimage 2018, 178, 69–77. [Google Scholar] [CrossRef]
- Guinsburg, R.; Peres, C.d.A.; de Almeida, M.F.B.; de Xavier Balda, R.C.; Berenguel, R.C.; Tonelotto, J.; Kopelman, B.I. Differences in Pain Expression between Male and Female Newborn Infants. Pain 2000, 85, 127–133. [Google Scholar] [CrossRef]
- Fuller, B.F. Infant Gender Differences Regarding Acute Established Pain. Clin. Nurs. Res. 2002, 11, 190–203. [Google Scholar] [CrossRef]
| Heel Lance/Squeeze Event | p | |||||
|---|---|---|---|---|---|---|
| T1 Before | T2 During | T3 After | T1 vs. T2 | T1 vs. T3 | T2 vs. T3 | |
| CHIPPS | 0 (0–2) | 6 (4–8) | 1 (0–5) | 0.003 | 0.94 | 0.07 |
| HR (1/min) | 148 ± 6 | 167 ± 5 | 151 ± 8 | 0.023 | 0.91 | 0.053 |
| BR (1/min) | 33 (29–36) | 30 (28–47) | 41 (34–42) | 1 | 0.45 | 0.61 |
| SpO2 (%) | 100 (99–100) | 100 (99–100) | 100 (100–100) | 1 | 1 | 0.74 |
| NIRS | ||||||
| c-rSO2 combined * (%) | 74 ± 2 | 74 ± 2 | 74 ± 2 | 0.83 | 0.97 | 0.70 |
| c-rSO2 left (%) | 74 ± 2 | 74 ± 2 | 74 ± 2 | 0.83 | 0.58 | 0.27 |
| c-rSO2 right (%) | 75 ± 3 | 75 ± 3 | 75 ± 3 | 0.93 | 0.71 | 0.18 |
| normalized c-rSO2 combined * | 1 | 1 ± 0.002 | 0.99 ± 0.002 | 0.90 | 0.89 | 0.66 |
| normalized c-rSO2 left | 1 | 1 ± 0.003 | 0.99 ± 0.002 | 0.87 | 0.52 | 0.26 |
| normalized c-rSO2 right | 1 | 1 ± 0.002 | 1 ± 0.003 | 0.35 | 0.99 | 0.99 |
| adjusted to stimulus | ||||||
| c-rSO2 ipsilateral (%) | 76 ± 2 | 77 ± 2 | 76 ± 2 | 0.44 | 0.99 | 0.36 |
| c-rSO2 contralateral (%) | 72 ± 2 | 72 ± 2 | 72 ± 2 | 0.97 | 0.96 | 1 |
| normalized c-rSO2 ipsilateral | 1 | 1 ± 0.003 | 0.99 ± 0.002 | 0.48 | 0.96 | 0.34 |
| normalized c-rSO2 contralateral | 1 | 0.99 ± 0.002 | 0.99 ± 0.003 | 0.99 | 0.89 | 0.99 |
| Reference | Cohort | Procedure/Setting | NIRS-Device | Frontal Optodes (n) | Referent Behavioral Pain Measures | Cortical NIRS Outcome |
|---|---|---|---|---|---|---|
| This study | 10 t | HLS after hernia repair | INVOS 5100C | 2 (ipsi- vs. contralateral, left vs. right, and combined) | CHIPPS |
|
| Sun et al. [41] | 82 p | During ROP screening # | EGOS-600A | 1 (central) | PIPP-R |
|
| Ozawa et al. [32] | 80 p&t | During hand venipuncture ## | NIRO-200 | 2 (left vs. right) | PIPP |
|
| Devi et al. [42] | 180 p | Automatic vs. manual vs. needle HLS | INVOS 5100C | 1 (forehead, n.s.) | PIPP-R |
|
| Kumar et al. [57] | 64 p | During HLS and venipuncture | INVOS 5100C | 1 (contralateral) | NIPS, PIPP-R |
|
| Hwang et al. [51] | 24 p | Manual vs. automatic HLS | INVOS 5100 | 1 (central) | PIPP |
|
| Upadhyay et al. [43] | 50 p | OG vs. NG tube insertion | INVOS 5100C | 1 (forehead, n.s.) | PIPP-R |
|
| Ozdemir et al. [44] | 119 t | HLS in LGA newborns vs. controls | Equanox 7600 | 2 (ipsi- vs. contralateral) | NIPS |
|
| Zhang et al. [45] | 48 p | Pain during PICC | EGOS-600A | 1 (central) | PIPP |
|
| Kara et al. [46] | 42 p | During ROP screening ### | INVOS 5100 | 1 (forehead, n.s.) | PIPP |
|
| Ranger et al. [47] | 29 p | Calmer vs. facilitated tucking at HLS | Portalite Mini | 1 (left) | BIIP |
|
| Gélinas et al. [48] | 40 a | Painful procedures #### | INVOS-4100 | 2 (left vs. right) | Self-report |
|
| Gélinas et al. [49] | 125 a | Non-painful vs. painful procedures #### | INVOS 5100 | 2 (left vs. right) | Self-report |
|
| Mukaihara et al. [50] | 34 a | GA vs. GA and PVB at thoracotomy | NIRO-200 | 2 (ipsi- vs. contralateral) | n.a. |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nissen, M.; Tröbs, R.-B. Prefrontal Cortical Near-Infrared Spectroscopy for Acute Pain Assessment in Infants: A Feasibility Study. J. Clin. Med. 2025, 14, 2525. https://doi.org/10.3390/jcm14072525
Nissen M, Tröbs R-B. Prefrontal Cortical Near-Infrared Spectroscopy for Acute Pain Assessment in Infants: A Feasibility Study. Journal of Clinical Medicine. 2025; 14(7):2525. https://doi.org/10.3390/jcm14072525
Chicago/Turabian StyleNissen, Matthias, and Ralf-Bodo Tröbs. 2025. "Prefrontal Cortical Near-Infrared Spectroscopy for Acute Pain Assessment in Infants: A Feasibility Study" Journal of Clinical Medicine 14, no. 7: 2525. https://doi.org/10.3390/jcm14072525
APA StyleNissen, M., & Tröbs, R.-B. (2025). Prefrontal Cortical Near-Infrared Spectroscopy for Acute Pain Assessment in Infants: A Feasibility Study. Journal of Clinical Medicine, 14(7), 2525. https://doi.org/10.3390/jcm14072525







