Relationship Among Global Femoral Offset, Leg Lengthening, and Tibiofemoral Rotation After Total Hip Arthroplasty
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
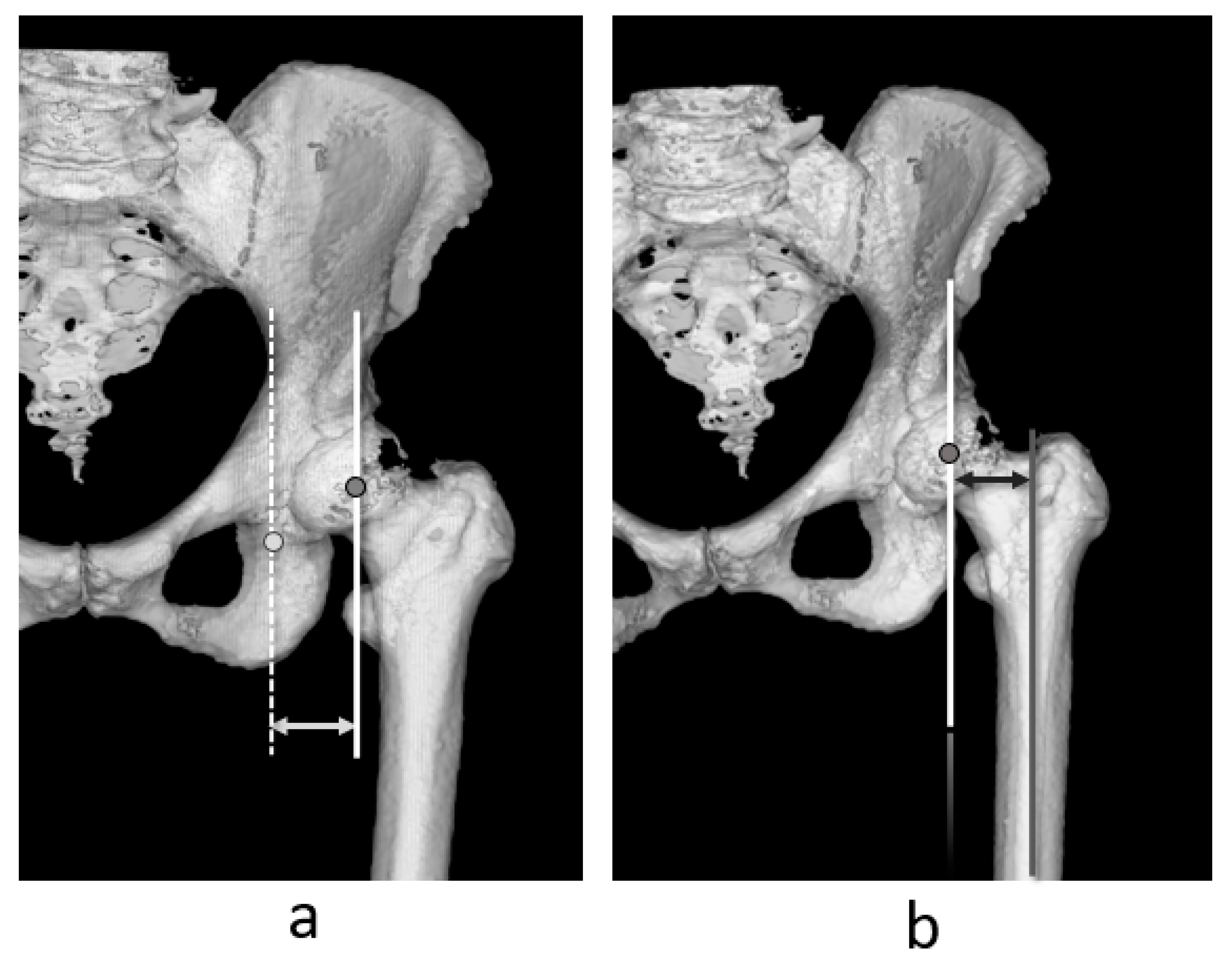
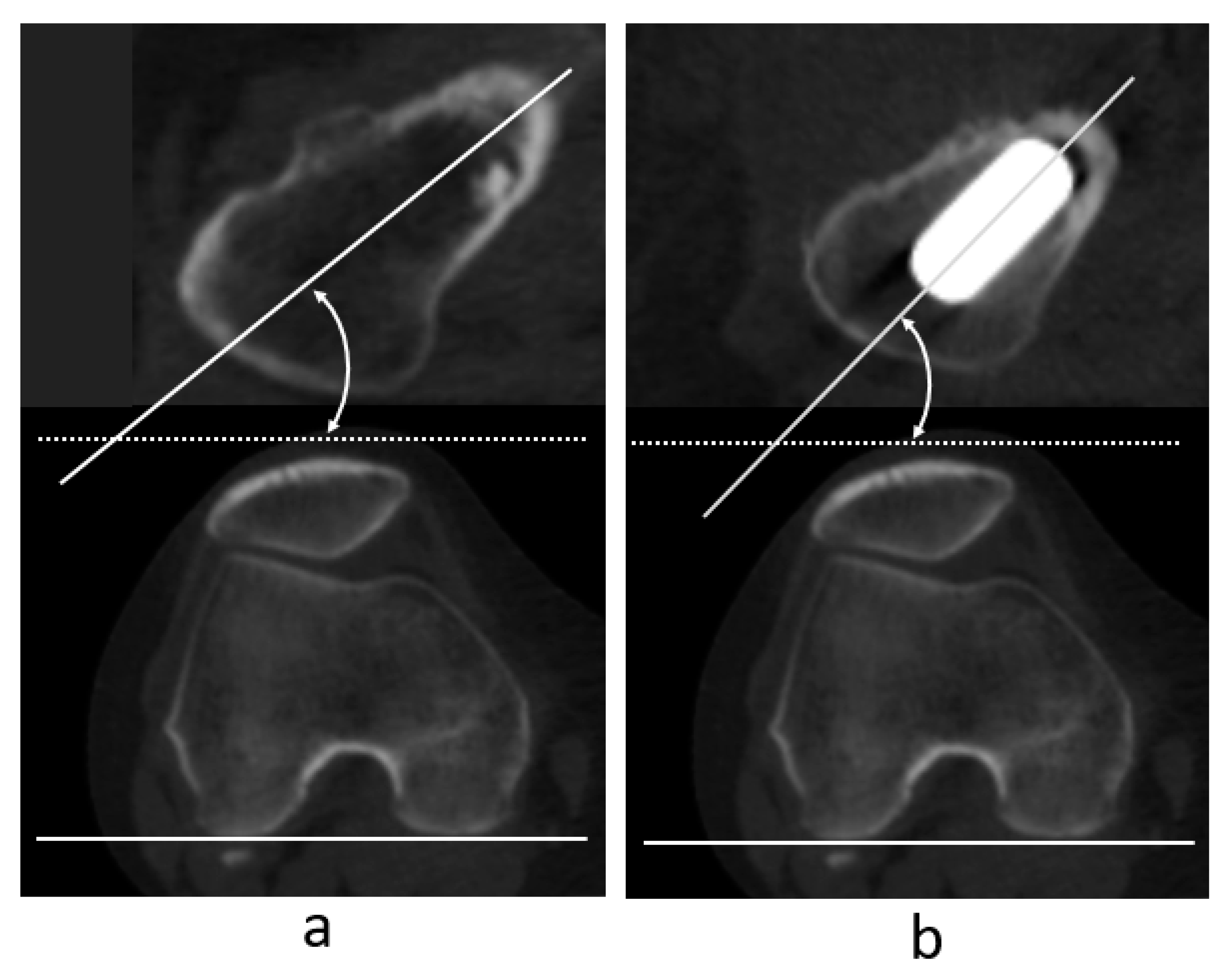
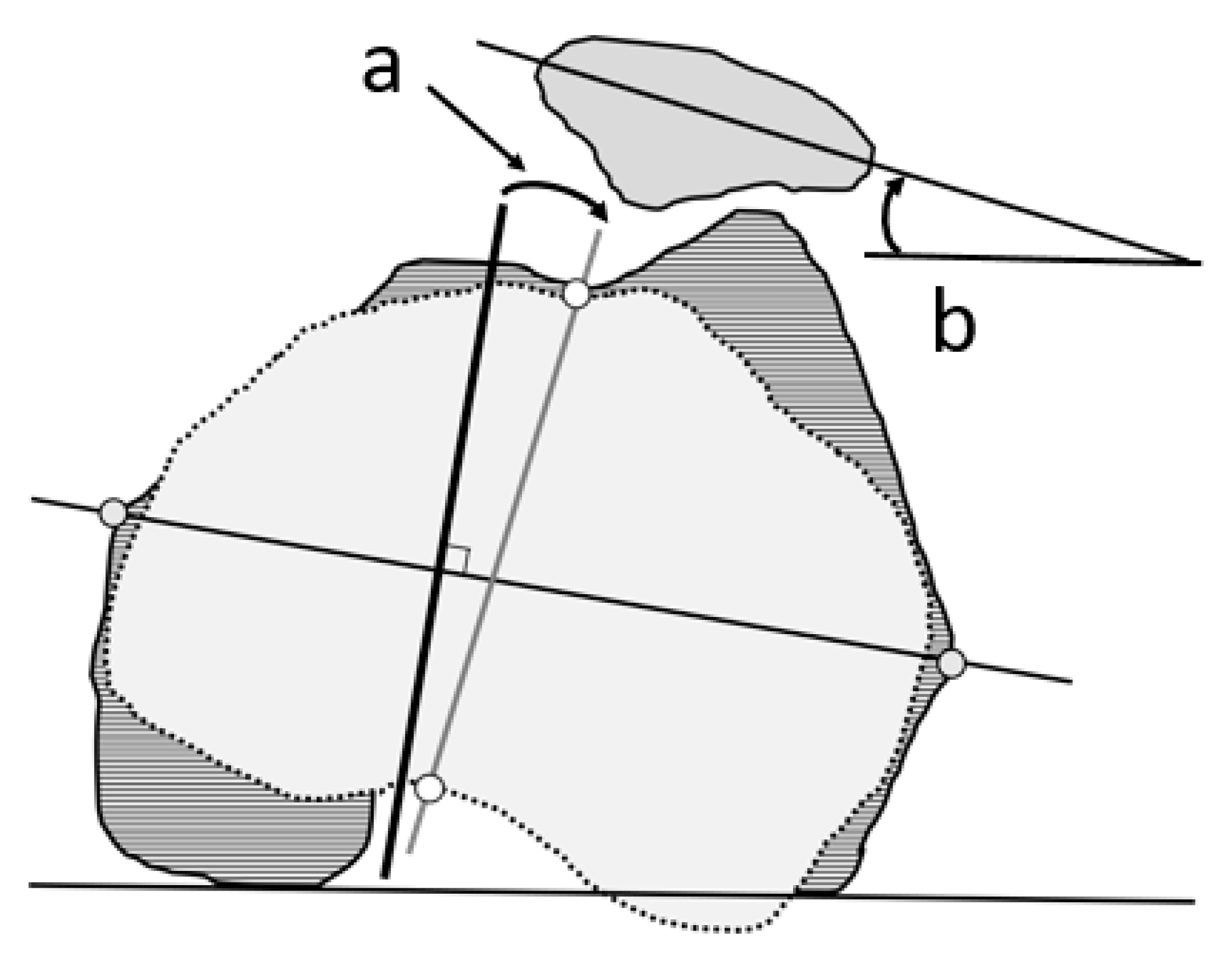
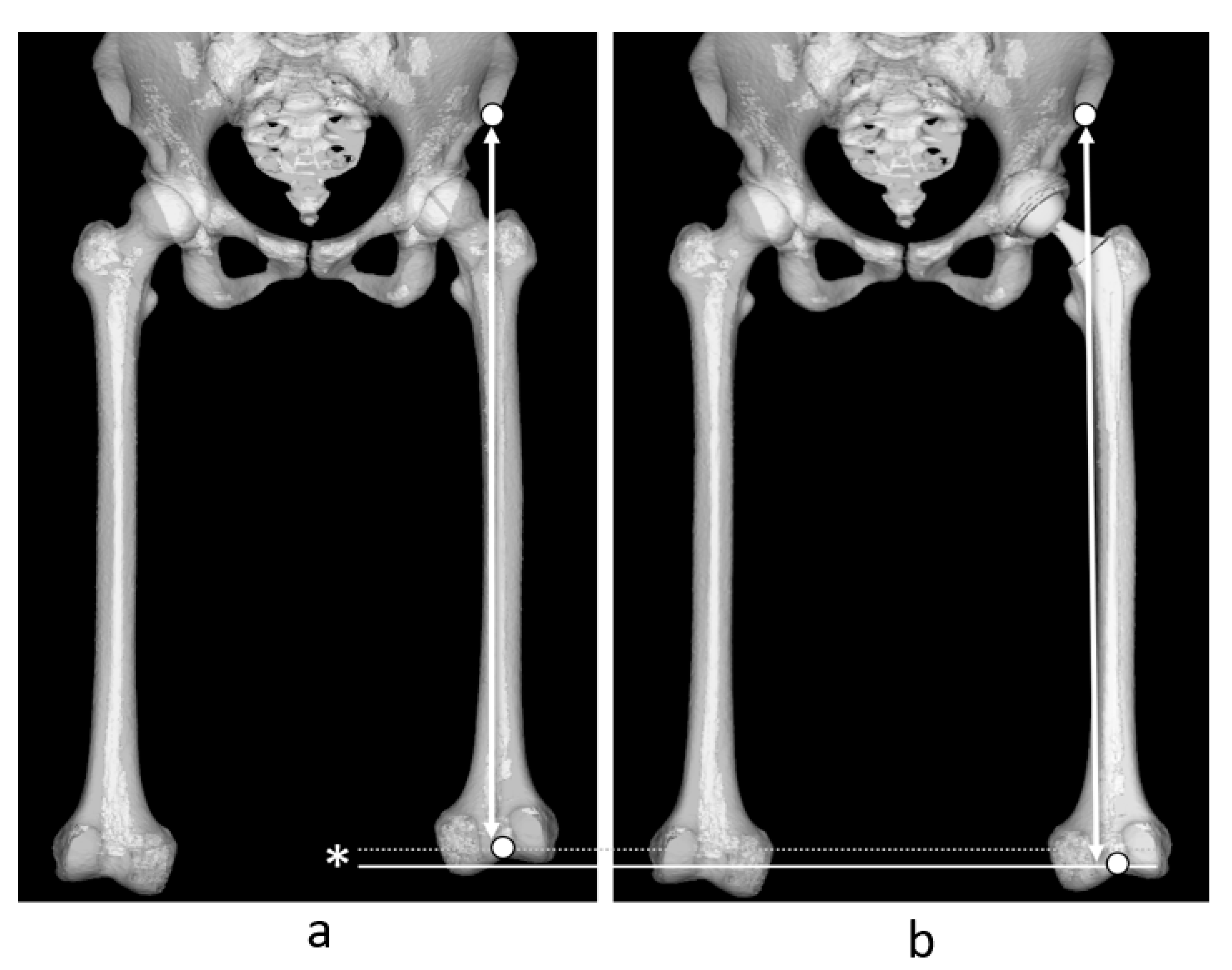
2.3. Measurement
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AO | Acetabular offset |
| AP | Anteroposterior |
| CC | Correlation coefficient |
| CT | Computed tomography |
| DDH | Developmental dysplasia of the hip |
| FNA | Femoral neck anteversion |
| FO | Femoral offset |
| FPP | Functional pelvic plane |
| FV | Femoral version |
| GFO | Global femoral offset |
| HOA | Hip osteoarthritis |
| OA | Osteoarthritis |
| mHHS | m-Harris Hip Score |
| PTA | Patellar tilt angle |
| RCP | Retrocondylar plane |
| TFRA | Tibiofemoral rotation angle |
| THA | Total hip anthroplasty |
References
- Mahmood, S.S.; Mukka, S.S.; Crnalic, S.; Wretenberg, P.; Sayed-Noor, A.S. Association between changes in global femoral offset after total hip arthroplasty and function, quality of life, and abductor muscle strength. A prospective cohort study of 222 patients. Acta. Orthop. 2016, 87, 36–41. [Google Scholar] [CrossRef]
- Cassidy, K.A.; Noticewala, M.S.; Macaulay, W.; Lee, J.H.; Geller, J.A. Effect of femoral offset on pain and function after total hip arthroplasty. J. Arthroplast. 2022, 27, 1863–1869. [Google Scholar] [CrossRef]
- Esbjörnsson, A.C.; Kiernan, S.; Mattsson, L.; Flivik, G. Geometrical restoration during total hip arthroplasty is related to change in gait pattern—A study based on computed tomography and three-dimensional gait analysis. BMC Musculoskelet. Disord. 2021, 22, 369. [Google Scholar] [CrossRef]
- Bonnin, M.P.; Archbold, P.H.; Basiglini, L.; Selmi, T.A.; Beverland, D.E. Should the acetabular cup be medialised in total hip arthroplasty. Hip Int. 2011, 21, 428–435. [Google Scholar] [CrossRef]
- Weber, M.; Woerner, M.L.; Springorum, H.-R.; Hapfelmeier, A.; Grifka, J.; Renkawitz, T. Plain radiographs fail to reflect femoral offset in total hip arthroplasty. J. Arthroplast. 2014, 29, 1661–1665. [Google Scholar] [CrossRef]
- Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). 2023 Annual Report. Available online: https://aoanjrr.sahmri.com/documents/10180/1579982/AOA_NJRR_AR23.pdf/c3bcc (accessed on 3 April 2023).
- Ramezani, A.; Raeini, A.G.; Sharafi, A.; Sheikhvatan, M.; Mortazavi, J.; Shafiei, S.H. Simultaneous versus staged bilateral total hip arthroplasty: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 392. [Google Scholar] [CrossRef]
- Sloan, M.; Premkumar, A.; Sheth, N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J. Bone Jt. Surg. Am. 2018, 100, 1455–1460. [Google Scholar] [CrossRef]
- Hirano, Y.; Imai, N.; Nozaki, A.; Horigome, Y.; Suzuki, H.; Kawashima, H. The association of postoperative global femoral offset with total hip arthroplasty outcomes. Sci. Rep. 2023, 13, 1621. [Google Scholar] [CrossRef]
- Kawakami, T.; Imagama, T.; Matsuki, Y.; Okazaki, T.; Kaneoka, T.; Sakai, T. Forgotten joint score is worse when the affected leg perceived longer than shorter after total hip arthroplasty. BMC Musculoskelet. Disord. 2023, 24, 440. [Google Scholar] [CrossRef]
- Worlicek, M.; Messmer, B.; Grifka, J.; Renkawitz, T.; Weber, M. Restoration of leg length and offset correlates with trochanteric pain syndrome in total hip arthroplasty. Sci. Rep. 2020, 10, 7107. [Google Scholar] [CrossRef]
- Imai, N.; Hirano, Y.; Endo, Y.; Horigome, Y.; Suzuki, H.; Kawashima, H. The sum of the leg length discrepancy and the difference in global femoral offset is equal to that of the contralateral intact side and improves postoperative outcomes after total hip arthroplasty: A three-dimensional analysis. J. Clin. Med. 2024, 13, 1698. [Google Scholar] [CrossRef]
- Yu, D.-G.; Zhang, J.-W.; Xu, C.; Xu, J.-W.; Li, H.-W.; Zhu, Z.-A.; Liu, F.-X.; Mao, Y.-Q. Changes in alignment of ipsilateral knee on computed tomography after total hip arthroplasty for developmental dysplasia of the hip. Orthop. Surg. 2019, 11, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Tokuhara, Y.; Kadoya, Y.; Kim, M.; Shoundou, M.; Kanno, T.; Masuda, T. Anterior knee pain after total hip arthroplasty in developmental dysplasia. J. Arthroplast. 2011, 26, 955–960. [Google Scholar] [CrossRef]
- Imai, N.; Miyasaka, D.; Ito, T.; Suzuki, H.; Minato, I.; Endo, N. The anteroposterior axis of the tibia is approximately perpendicular to the anterior pelvic plane in the standing position in healthy Japanese subjects. J. Orthop. Surg. Res. 2017, 12, 136. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Imai, N.; Miyasaki, S.; Suzuki, H.; Tsuchiya, K.; Ito, T.; Minato, I.; Endo, N. The anteroposterior axis of the tibia is adjusted to approximately a right angle to the anterior pelvic plane in the standing position in patients with hip dysplasia similar to normal subjects: A cross-sectional study. J. Orthop. Surg. Res. 2018, 13, 105. [Google Scholar] [CrossRef] [PubMed]
- Hirano, Y.; Imai, N.; Suzuki, H.; Endo, N. Differences in tibio-femoral rotation and patellar tilt angle between normal and the patients with acetabular dysplasia in female. Arch. Niigata Soc. Orthop. Surg. 2020, 35, 87–92. (In Japanese) [Google Scholar]
- Cho, E.; Hisatome, T.; Oda, S.; Fujimaki, H.; Nakanishi, K. Accuracy of acetabular cup placement during anterolateral supine total hip arthroplasty using intraoperative fluoroscopy: A retrospective study. J. Orthop. Surg. Res. 2022, 17, 523. [Google Scholar] [CrossRef]
- Stolarczyk, A.; Stolarczyk, M.; Stępiński, P.; Dorocińska, M.K.; Świercz, M.; Szymczak, J.; Żarnovsky, K.; Żuchniewicz, A.; Maciąg, B.M. The direct anterior approach to primary total hip replacement: Radiological analysis in comparison to other approaches. J. Clin. Med. 2021, 10, 2246. [Google Scholar] [CrossRef]
- Ohta, Y.; Sugama, R.; Minoda, Y.; Mizokawa, S.; Takahashi, S.; Ikebuchi, M.; Nakatsuchi, T.; Nakamura, H. Is the anterolateral or posterolateral approach more effective for early postoperative recovery after minimally invasive total hip arthroplasty? J. Clin. Med. 2022, 12, 139. [Google Scholar] [CrossRef]
- Murray, D.W. The definition and measurement of acetabular orientation. J. Bone Jt. Surg. Br. 1993, 75, 228–232. [Google Scholar] [CrossRef]
- Sugano, N.; Nishii, T.; Miki, H.; Yoshikawa, H.; Sato, Y.; Tamura, S. Mid-term results of cementless total hip replacement using a ceramic-on-ceramic bearing with and without computer navigation. J. Bone Jt. Surg. Br. 2007, 89, 455–460. [Google Scholar] [CrossRef]
- Suda, K.; Ito, T.; Miyasaka, D.; Imai, N.; Minato, I.; Endo, N. Cup implantation accuracy using the HipCOMPASS mechanical intraoperative support device. Springerplus 2016, 5, 784. [Google Scholar] [CrossRef] [PubMed]
- Imai, N.; Takubo, R.; Suzuki, H.; Shimada, H.; Miyasaka, D.; Tsuchiya, K.; Endo, N. Accuracy of acetabular cup placement using CT-based navigation in total hip arthroplasty: Comparison between obese and non-obese patients. J. Orthop. Sci. 2019, 24, 482–487. [Google Scholar] [CrossRef] [PubMed]
- Matsubayashi, S.; Isobe, Y.; Chiba, K.; Tsujimoto, R.; Osaki, M.; Imamura, T.; Tsurumoto, T. Measurement of femoral axial offset. J. Orthop. Res. 2021, 39, 1383–1389. [Google Scholar] [CrossRef]
- Dorr, L.D.; Malik, A.; Dastane, M.; Wan, Z. Combined anteversion technique for total hip arthroplasty. Clin. Orthop. Relat. Res. 2009, 467, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Widmer, K.H.; Zurfluh, B. Compliant positioning of total hip components for optimal range of motion. J. Orthop. Res. 2004, 22, 815–821. [Google Scholar] [CrossRef]
- Nozaki, A.; Imai, N.; Funayama, K.; Horigome, Y.; Suzuki, H.; Minato, I.; Kobayashi, K.; Kawashima, H. Accuracy of ZedView, the software for three-dimensional measurement and preoperative planning: A basic study. Medicina 2023, 59, 1030. [Google Scholar] [CrossRef]
- Ariumi, A.; Sato, T.; Kobayashi, K.; Koga, Y.; Omori, G.; Minato, I.; Endo, N. Three-dimensional lower extremity alignment in the weight-bearing standing position in healthy elderly subjects. J. Orthop. Sci. 2010, 15, 64–70. [Google Scholar] [CrossRef]
- Sato, T.; Koga, Y.; Omori, G. Three-dimensional lower extremity alignment assessment system: Application to evaluation of component position after total knee arthroplasty. J. Arthroplasty 2004, 19, 620–628. [Google Scholar] [CrossRef]
- Kubota, S.; Inaba, Y.; Kobayashi, N.; Choe, H.; Tezuka, T.; Saito, T. Comparison of improved range of motion between cam-type femoroacetabular impingement and borderline developmental dysplasia of the hip -evaluation by virtual osteochondroplasty using computer simulation. BMC Musculoskelet. Disord. 2017, 18, 417. [Google Scholar] [CrossRef]
- Lecerf, G.; Fessy, M.H.; Philippot, R.; Massin, P.; Giraud, F.; Flecher, X.; Girard, J.; Mertl, P.; Marchetti, E.; Stindel, E. Femoral offset: Anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop. Traumatol. Surg. Res. 2009, 95, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Imai, N.; Suzuki, H.; Nozaki, A.; Miyasaka, D.; Tsuchiya, K.; Ito, T.; Minato, I.; Endo, N. Evaluation of anatomical pelvic parameters between normal, healthy men and women using three-dimensional computed tomography: A cross-sectional study of sex-specific and age-specific differences. J. Orthop. Surg. Res. 2019, 14, 126. [Google Scholar] [CrossRef] [PubMed]
- Sugano, N.; Noble, P.C.; Kamaric, E. A comparison of alternative methods of measuring femoral anteversion. J. Comput. Assist. Tomogr. 1998, 22, 610–614. [Google Scholar] [CrossRef]
- Akagi, M.; Mori, S.; Nishimura, S.; Asano, T.; Hamanishi, C. Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin. Orthop. Relat. Res. 2005, 436, 172–176. [Google Scholar] [CrossRef]
- Kobayashi, D.; Choe, H.; Kobayashi, N.; Watanabe, S.; Inaba, Y. Effects of changes in whole-body alignment on ipsilateral knee pain after total hip arthroplasty. J. Orthop. Sci. 2023, 28, 398–402. [Google Scholar] [CrossRef]
- Iseki, T.; Iseki, T.; Tachibana, T. Total hip arthroplasty concomitant with patellofemoral arthroplasty and medial patellofemoral ligament reconstruction for a patient with patellar dislocation combined with hip dysplasia: A case report of a successful outcome at 5-year follow-up. Case Rep. Orthop. 2021, 2021, 9970975. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.S.; Park, J.-W.; Kim, T.W.; Kang, K.S.; Lee, Y.-K.; Koo, K.-H.; Chang, C.B. Effect of total hip arthroplasty on ipsilateral lower limb alignment and knee joint space width: Minimum 5-year follow-up. J. Korean Med. Sci. 2023, 38, e148. [Google Scholar] [CrossRef]
- Tone, S.; Hasegawa, M.; Naito, Y.; Wakabayashi, H.; Sudo, A. Comparison between two- and three-dimensional methods for offset measurements after total hip arthroplasty. Sci. Rep. 2022, 12, 12644. [Google Scholar] [CrossRef]


| Sex (Female/Male) | 28/83 |
|---|---|
| Age (years) * | 56.6 ± 10.4 (36–78) |
| Surgical side (right/left) | 69/42 |
| Primary disease | Developmental dysplasia of the hip: 96 Osteonecrosis of the femoral head: 14 Primary hip osteoarthritis: 2 |
| Acetabular component | PlasmaFit®, B. Braun: 38 Trident®, Stryker: 73 |
| Femoral component | BiCONTACT D stem®, B. Braun: 14 BiCONTACT E stem®, B. Braun: 24 Accolade II®, Stryker: 66 Exeter cemented stem®, Stryker: 7 |
| Before Surgery | After Surgery | Difference: Δ | |
|---|---|---|---|
| GFO (mm) * | 66.7 ± 7.1 (51.8–87.1) | 64.2 ± 7.0 (45.6–82.6) | −2.5 ± 6.7 (−22.0–9.9) |
| Leg lengthening (mm) * | 10.0 ± 6.3 (−0.2–30.0) | ||
| FV (°) | 23.4 ± 13.5 (−15.7–55.2) | 26.9 ± 10.9 (−3.8–57.3) | 3.5 ± 12.4(−31.6–53.6) |
| TFRA (°) | 6.5 ± 7.4 (−11.3–26.2) | 5.5 ± 7.0 (−15.8–20.7) | 0.9 ± 4.6 (−9.6–11.3) |
| PTA (°) | 12.8 ± 5.8 (−1.5–29.9) | 15.5 ± 7.0 (−9.0–37.3) | 2.7 ± 3.6 (−6.1–12.3) |
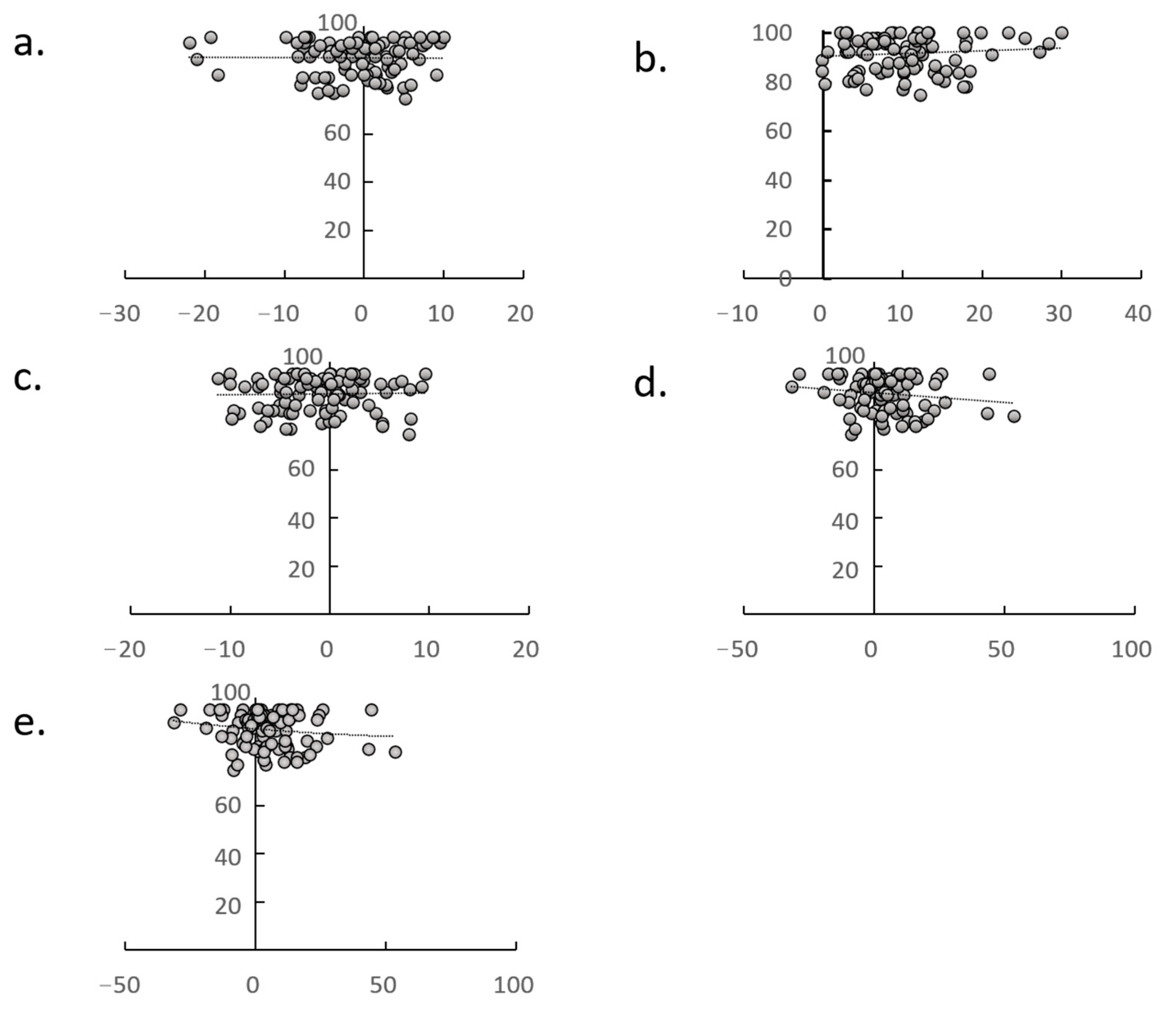
| Formula | Correlation Coefficient | p-Value | |
|---|---|---|---|
| * | y = 0.3355x − 0.8332 | r = 0.317 | 0.008 |
| ** | y = 0.4868x − 0.3424 | r = 0.566 | <0.001 |
| ☨ | y = −0.2712x | r = 0.289 | 0.018 |
| ☨☨ | y = −0.7824x | r = 0.342 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Imai, N.; Hirano, Y.; Homma, D.; Komuta, Y.; Horigome, Y.; Kawashima, H. Relationship Among Global Femoral Offset, Leg Lengthening, and Tibiofemoral Rotation After Total Hip Arthroplasty. J. Clin. Med. 2025, 14, 2893. https://doi.org/10.3390/jcm14092893
Imai N, Hirano Y, Homma D, Komuta Y, Horigome Y, Kawashima H. Relationship Among Global Femoral Offset, Leg Lengthening, and Tibiofemoral Rotation After Total Hip Arthroplasty. Journal of Clinical Medicine. 2025; 14(9):2893. https://doi.org/10.3390/jcm14092893
Chicago/Turabian StyleImai, Norio, Yuki Hirano, Daisuke Homma, Yuki Komuta, Yoji Horigome, and Hiroyuki Kawashima. 2025. "Relationship Among Global Femoral Offset, Leg Lengthening, and Tibiofemoral Rotation After Total Hip Arthroplasty" Journal of Clinical Medicine 14, no. 9: 2893. https://doi.org/10.3390/jcm14092893
APA StyleImai, N., Hirano, Y., Homma, D., Komuta, Y., Horigome, Y., & Kawashima, H. (2025). Relationship Among Global Femoral Offset, Leg Lengthening, and Tibiofemoral Rotation After Total Hip Arthroplasty. Journal of Clinical Medicine, 14(9), 2893. https://doi.org/10.3390/jcm14092893






