Determining the Optimal Cutoff Value for the Reverse Shock Index Multiplied by the Glasgow Coma Scale for the Prediction of In-Hospital Mortality in Pediatric Trauma Patients: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
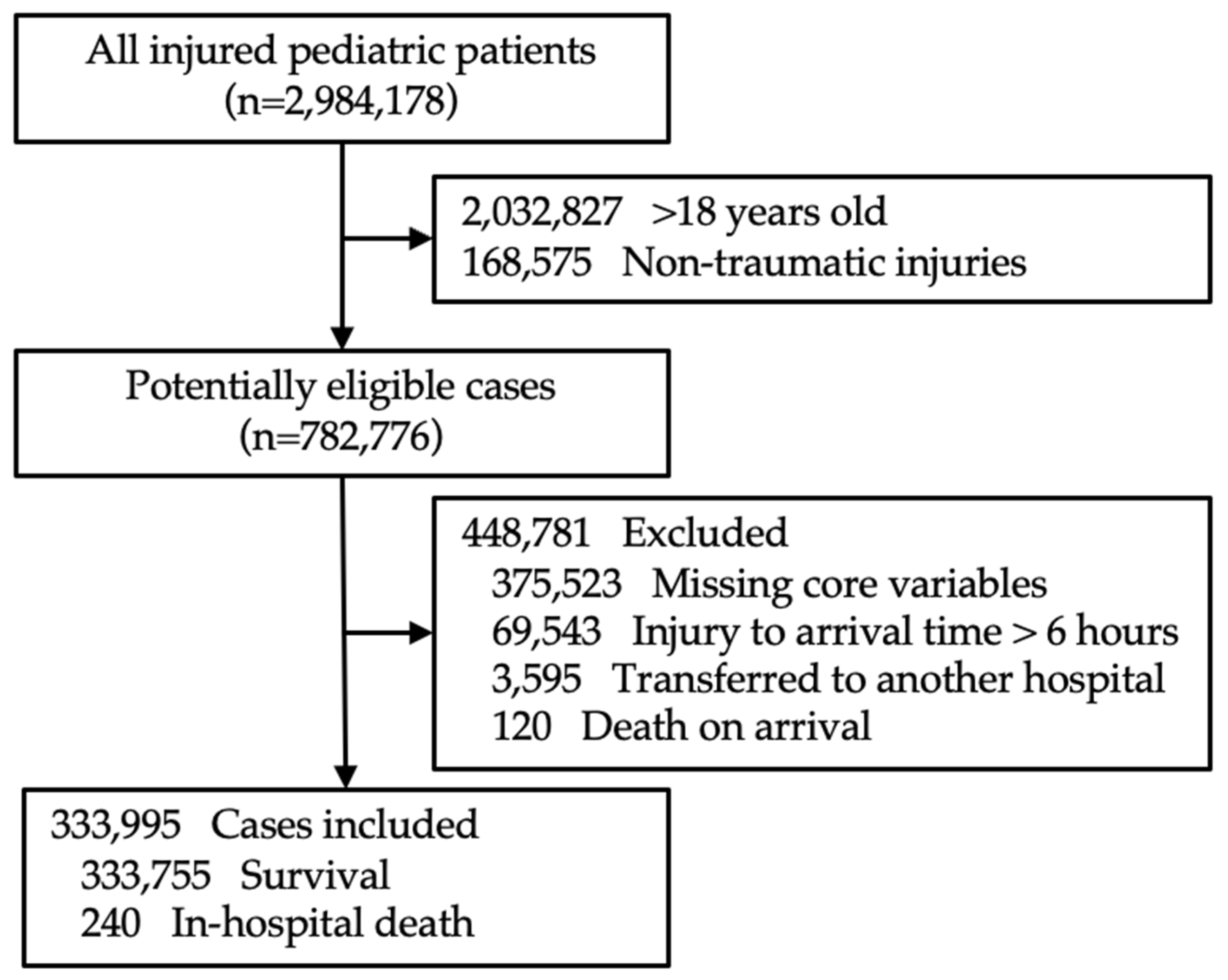
2.1. Inclusion and Exclusion Criteria
2.2. Study Data and Variables
2.3. Statistical Analysis
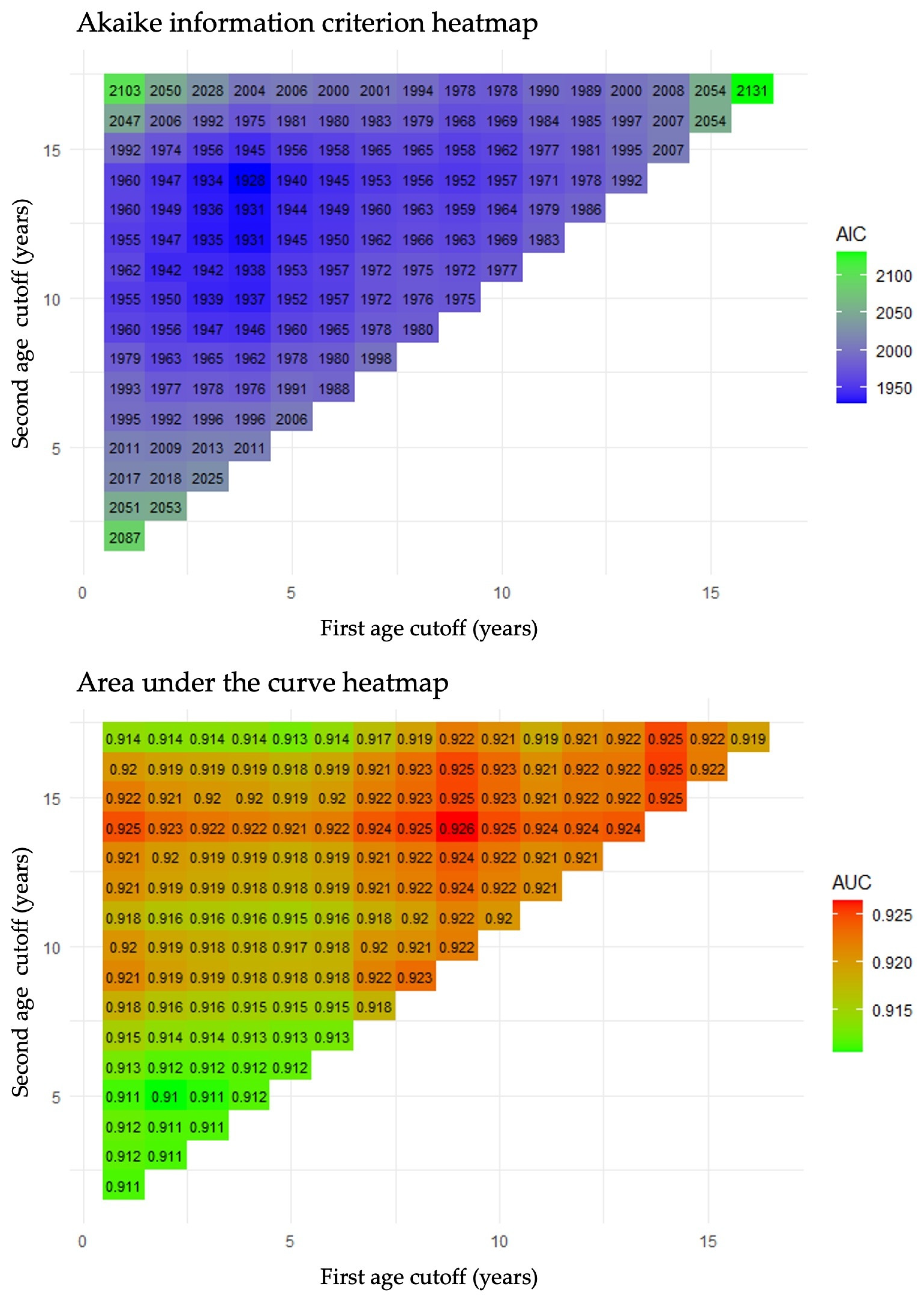
2.3.1. Establishment of Age Groups with Shared rSIG Cutoffs
2.3.2. Determination of rSIG Cutoff Values
Youden Index (YI) Method
Optimization Based on over- and Under-Triage Rates
3. Results
3.1. Characteristics of the Study Population
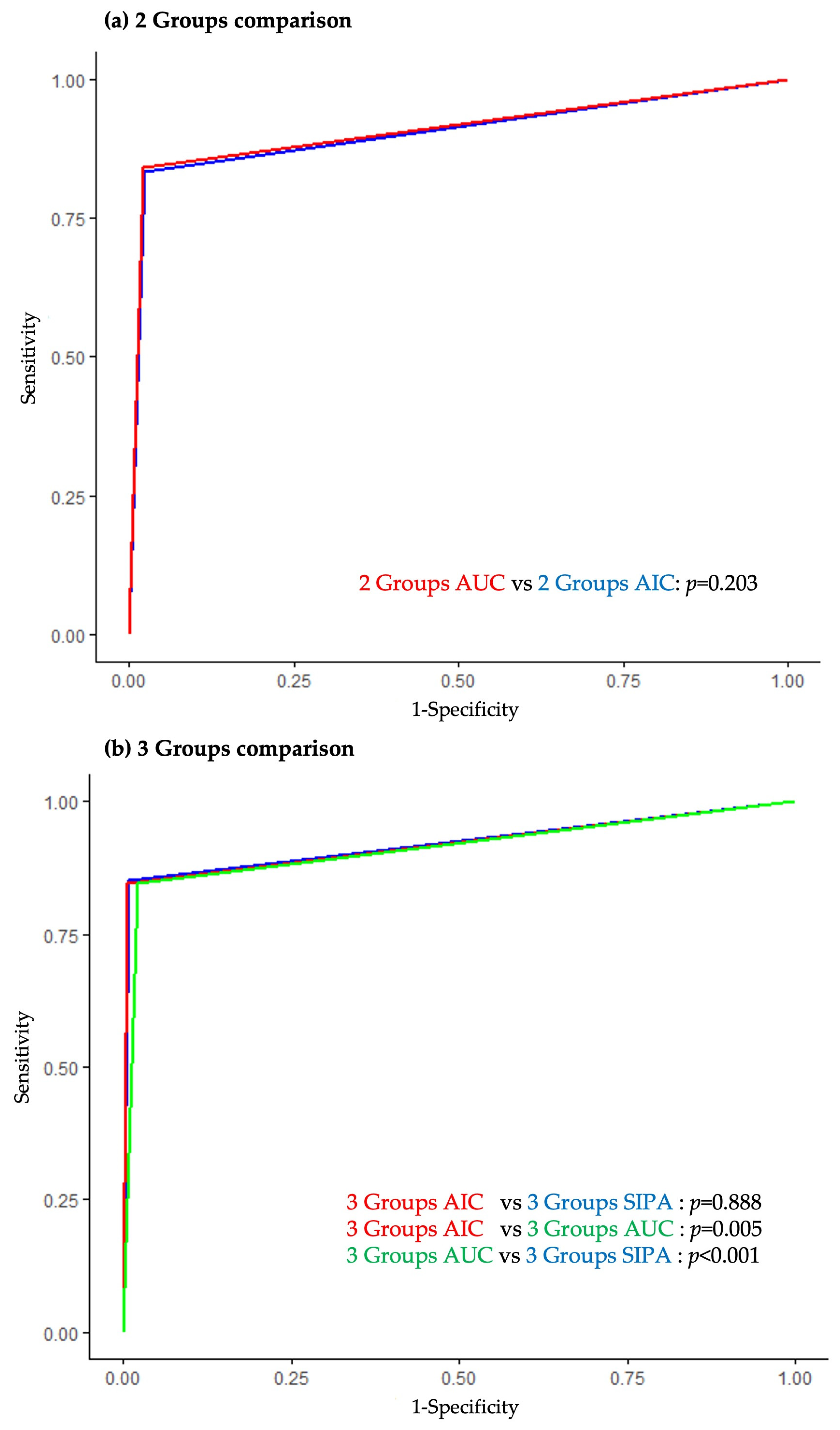
3.2. Age Groups with Shared rSIG Cutoffs
3.3. Optimal rSIG Cutoff for Maximization of AUC Using YI
3.4. Optimal rSIG Cutoff Based on Over-Triage and Under-Triage Rates
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACS | American College of Surgeons |
| rSIG | Reverse shock index multiplied by the Glasgow Coma Scale |
| SBP | Systolic blood pressure |
| HR | Heart rate |
| GCS | Glasgow Coma Scale |
| EDIIS | Emergency Department-Based Injury In-Depth Surveillance |
| KDCA | Korea Disease Control and Prevention Agency |
| EMR-ISS | Excess mortality ratio-adjusted injury severity score |
| AUC | Area under the receiver operating characteristic curve |
| AIC | Akaike information criterion |
| ROC | Receiver operating characteristic curve |
| YI | Youden index |
| DBP | Diastolic blood pressure |
| RR | Respiratory rate |
| BT | Body temperature |
| 95% CI | 95% confidence interval |
| SIPA | Pediatric age-adjusted shock index |
References
- Peden, M.; Oyegbite, K.; Ozanne-Smith, J.; Hyder, A.A.; Branche, C.; Rahman, A.K.M.F.; Rivara, F.; Bartolomeos, K. (Eds.) World Report on Child Injury Prevention; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Pressley, J.C.; Barlow, B.; Durkin, M.; Jacko, S.A.; Dominguez, D.R.; Johnson, L. A national program for injury prevention in children and adolescents: The injury free coalition for kids. J. Urban Health 2005, 82, 389–402. [Google Scholar] [CrossRef] [PubMed]
- Mannix, C.; Neuman, M.; Mannix, R. Trends in Pediatric Nonfatal and Fatal Injuries. Pediatrics 2023, 152, e2023063411. [Google Scholar] [CrossRef] [PubMed]
- Smida, T.; Bonasso, P.; Bardes, J.; Price, B.S.; Seifarth, F.; Gurien, L.; Maxson, R.; Letton, R. Reverse shock index multiplied by the motor component of the Glasgow Coma Scale predicts mortality and need for intervention in pediatric trauma patients. J. Trauma Acute Care Surg. 2024, 97, 393–399. [Google Scholar] [CrossRef] [PubMed]
- van der Sluijs, R.; van Rein, E.A.; Wijnand, J.G.; Leenen, L.P.; van Heijl, M. Accuracy of pediatric trauma field triage: A systematic review. JAMA Surg. 2018, 153, 671–676. [Google Scholar] [CrossRef]
- Newgard, C.D.; Fischer, P.E.; Gestring, M.; Michaels, H.N.; Jurkovich, G.J.; Lerner, E.B.; Fallat, M.E.; Delbridge, T.R.; Brown, J.B.; Bulger, E.M. National guideline for the field triage of injured patients: Recommendations of the National Expert Panel on Field Triage, 2021. J. Trauma Acute Care Surg. 2022, 93, e49–e60. [Google Scholar] [CrossRef]
- Reppucci, M.L.; Acker, S.N.; Cooper, E.; Meier, M.; Stevens, J.; Phillips, R.; Moulton, S.L.; Bensard, D.D. Improved identification of severely injured pediatric trauma patients using reverse shock index multiplied by Glasgow Coma Scale. J. Trauma Acute Care Surg. 2022, 92, 69–73. [Google Scholar] [CrossRef]
- Reppucci, M.L.; Stevens, J.; Cooper, E.; Nolan, M.M.; Jujare, S.; Acker, S.N.; Moulton, S.L.; Bensard, D.D. Use of reverse shock index times Glasgow coma scale (rSIG) to determine need for transfer of pediatric trauma patients to higher levels of care. J. Pediatr. Surg. 2023, 58, 320–324. [Google Scholar] [CrossRef]
- American College of Surgeon. Resources for Optimal Care of the Injured Patient; American College of Surgeons: Chicago, IL, USA, 2014. [Google Scholar]
- Lupton, J.R.; Davis-O’Reilly, C.; Jungbauer, R.M.; Newgard, C.D.; Fallat, M.E.; Brown, J.B.; Mann, N.C.; Jurkovich, G.J.; Bulger, E.; Gestring, M.L.; et al. Under-Triage and Over-Triage Using the Field Triage Guidelines for Injured Patients: A Systematic Review. Prehosp. Emerg. Care 2023, 27, 38–45. [Google Scholar] [CrossRef]
- Kimura, A.; Tanaka, N. Reverse shock index multiplied by Glasgow Coma Scale score (rSIG) is a simple measure with high discriminant ability for mortality risk in trauma patients: An analysis of the Japan Trauma Data Bank. Crit. Care 2018, 22, 87. [Google Scholar] [CrossRef]
- Lammers, D.T.; Marenco, C.W.; Do, W.S.; Conner, J.R.; Horton, J.D.; Martin, M.J.; Escobar, M.A.; Bingham, J.R.; Eckert, M.J. Pediatric adjusted reverse shock index multiplied by Glasgow Coma Scale as a prospective predictor for mortality in pediatric trauma. J. Trauma Acute Care Surg. 2021, 90, 21–26. [Google Scholar] [CrossRef]
- Chen, T.H.; Wu, M.Y.; Do Shin, S.; Jamaluddin, S.F.; Son, D.N.; Hong, K.J.; Jen-Tang, S.; Tanaka, H.; Hsiao, C.H.; Hsieh, S.L.; et al. Discriminant ability of the shock index, modified shock index, and reverse shock index multiplied by the Glasgow coma scale on mortality in adult trauma patients: A PATOS retrospective cohort study. Int. J. Surg. 2023, 109, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.T.; Bae, B.K.; Cho, Y.M.; Park, S.C.; Jeon, C.H.; Huh, U.; Lee, D.S.; Ko, S.H.; Ryu, D.M.; Wang, I.J. Reverse shock index multiplied by Glasgow coma scale as a predictor of massive transfusion in trauma. Am. J. Emerg. Med. 2021, 46, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Chedid, I.; Bachir, R.; Rizk, J.; El Sayed, M.; Sawaya, R.D. Which Trauma Severity Scores Are Useful in Predicting Pediatric Mortality? Pediatr. Emerg. Care 2023, 39, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Hanna, S.; Montmayeur, J.; Vergnaud, E.; Orliaguet, G. Prognosis and assessment of the predictive value of severity scores in paediatric abdominal trauma: A French national cohort study. Eur. J. Anaesthesiol. 2024, 41, 632–640. [Google Scholar] [CrossRef]
- Kim, S.Y.; Hong, K.J.; Shin, S.D.; Ro, Y.S.; Ahn, K.O.; Kim, Y.J.; Lee, E.J. Validation of the Shock Index, Modified Shock Index, and Age Shock Index for Predicting Mortality of Geriatric Trauma Patients in Emergency Departments. J. Korean Med. Sci. 2016, 31, 2026–2032. [Google Scholar] [CrossRef]
- Park, J.S.; Choi, S.J.; Kim, M.J.; Choi, S.Y.; Kim, H.Y.; Park, Y.S.; Chung, S.P.; Lee, J.H. Cutoff of the reverse shock index multiplied by the Glasgow coma scale for predicting in-hospital mortality in adult patients with trauma: A retrospective cohort study. BMC Emerg. Med. 2024, 24, 55. [Google Scholar] [CrossRef]
- Kim, J.; Shin, S.D.; Im, T.H.; Kug Jong, L.; Ko, S.B.; Park, J.O.; Ahn, K.O.; Song, K.J. Development and validation of the Excess Mortality Ratio-adjusted Injury Severity Score Using the International Classification of Diseases 10th Edition. Acad. Emerg. Med. 2009, 16, 454–464. [Google Scholar] [CrossRef]
- Lammers, D.T.; Marenco, C.W.; Morte, K.R.; Conner, J.R.; Horton, J.D.; Barlow, M.; Martin, M.J.; Bingham, J.R.; Eckert, M.J.; Escobar, M.A. Addition of neurological status to pediatric adjusted shock index to predict early mortality in trauma: A pediatric Trauma Quality Improvement Program analysis. J. Trauma Acute Care Surg. 2021, 91, 584–589. [Google Scholar] [CrossRef]
- Peng, J.; Xiang, H. Trauma undertriage and overtriage rates: Are we using the wrong formulas? Am. J. Emerg. Med. 2016, 34, 2191–2192. [Google Scholar] [CrossRef]
- Acker, S.N.; Ross, J.T.; Partrick, D.A.; Tong, S.; Bensard, D.D. Pediatric specific shock index accurately identifies severely injured children. J. Pediatr. Surg. 2015, 50, 331–334. [Google Scholar] [CrossRef]
- Trust, M.D.; Schellenberg, M.; Biswas, S.; Inaba, K.; Cheng, V.; Warriner, Z.; Love, B.E.; Demetriades, D. Prehospital Vital Signs Accurately Predict Initial Emergency Department Vital Signs. Prehosp. Disaster Med. 2020, 35, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Levin, H.S.; Aldrich, E.F.; Saydjari, C.; Eisenberg, H.M.; Foulkes, M.A.; Bellefleur, M.; Luerssen, T.G.; Jane, J.A.; Marmarou, A.; Marshall, L.F.; et al. Severe Head Injury in Children: Experience of the Traumatic Coma Data Bank. Neurosurgery 1992, 31, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Sarnaik, A.; Ferguson, N.M.; O’Meara, A.M.I.; Agrawal, S.; Deep, A.; Buttram, S.; Bell, M.J.; Wisniewski, S.R.; Luther, J.F.; Hartman, A.L.; et al. Age and Mortality in Pediatric Severe Traumatic Brain Injury: Results from an International Study. Neurocritical Care 2018, 28, 302–313. [Google Scholar] [CrossRef] [PubMed]
- McKiernan, C.A.; Lieberman, S.A. Circulatory Shock in Children: An Overview. Pediatr. Rev. 2005, 26, 451–460. [Google Scholar] [CrossRef]
- Caruana, M.; Hackenbruch, S.N.; Grech, V.; Farrugia, R. Inconsistency in the Application of Glasgow Coma Scale in Pediatric Patients. Med. Princ. Pract. 2024, 33, 41–46. [Google Scholar] [CrossRef]
- DiBrito, S.R.; Cerullo, M.; Goldstein, S.D.; Ziegfeld, S.; Stewart, D.; Nasr, I.W. Reliability of Glasgow Coma Score in pediatric trauma patients. J. Pediatr. Surg. 2018, 53, 1789–1794. [Google Scholar] [CrossRef]
- National Clinical Guideline Centre (UK). Head Injury: Triage, Assessment, Investigation and Early Management of Head Injury in Children, Young People and Adults; National Institute for Health and Care Excellence (UK): London, UK, 2014; (NICE Clinical Guidelines, No. 176.) 5, Pre-Hospital Assessment, Advice and Referral to Hospital. Available online: https://www.ncbi.nlm.nih.gov/books/NBK332983/ (accessed on 20 April 2025).
| Variable | Survival Group (n = 333,755) | In-Hospital Death Group (n = 240) | p-Value |
|---|---|---|---|
| Age, years | 7 (3, 13) | 15 (6, 17) | <0.001 |
| Male, n (%) | 224,200 (67.2) | 175 (72.9) | 0.058 |
| Injury mechanism, n (%) | <0.001 | ||
| Traffic accident | 47,275 (14.2) | 145 (60.4) | |
| Fall | 130,166 (39.0) | 87 (36.3) | |
| Blunt injury | 123,011 (36.9) | 6 (2.5) | |
| Penetrating injury | 33,064 (9.9) | 2 (0.8) | |
| Other a | 239 (0.1) | 0 (0.0) | |
| Time from injury to arrival (min) | 60 (30, 94) | 41 (26, 94) | <0.001 |
| Arrived by ambulance, n (%) | 46,142 (13.8) | 165 (68.8) | <0.001 |
| SBP (mmHg) | 110 (100, 125) | 110 (84, 130) | 0.043 |
| DBP (mmHg, n= 333,155) | 68 (60, 78) | 70 (55, 84) | 0.346 |
| HR (beats/min) | 98 (85, 112) | 110 (84, 134) | <0.001 |
| RR (breaths/min, n = 333,142) | 20 (20, 24) | 20 (18, 26) | 0.059 |
| BT (°C, n = 333,583) | 36.6 (36.4, 36.8) | 36.2 (36.0, 36.6) | <0.001 |
| GCS | 15 (15, 15) | 4 (3, 8) | <0.001 |
| rSIG | 17.31 (14.10, 21.15) | 4.67 (2.78, 8.62) | <0.001 |
| EMR-ISS | 9.0 (4.0, 9.0) | 50 (25, 66) | <0.001 |
| Group 1 | Group 2 | Group 3 | Overall | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Age Range (years) | Cutoff | AUC (95% CI) | Age Range (years) | Cutoff | AUC (95% CI) | Age Range (years) | Cutoff | AUC (95% CI) | AUC (95% CI) |
| 2 Groups AUC | 0–14 | 9.643 | 0.872 (0.833–0.912) | 15–18 | 13.507 | 0.946 (0.920–0.971) | - | - | - | 0.910 (0.887–0.933) |
| 2 Groups AIC | 0–10 | 9.643 | 0.847 (0.797–0.896) | 11–18 | 13.507 | 0.945 (0.923–0.968) | - | - | - | 0.905 (0.881–0.928) |
| 3 Groups AUC | 0–9 | 9.643 | 0.850 (0.799–0.901) | 10–14 | 12.092 | 0.931 (0.876–0.985) | 15–18 | 13.507 | 0.946 (0.92–0.971) | 0.912 (0.889–0.934) |
| 3 Groups AIC | 0–4 | 7.558 | 0.850 (0.781–0.918) | 5–14 | 10.142 | 0.946 (0.92–0.971) | 15–18 | 13.507 | 0.946 (0.92–0.971) | 0.920 (0.897–0.943) |
| 3 Groups SIPA | 0–6 | 7.558 | 0.850 (0.793–0.908) | 7–12 | 12.089 | 0.949 (0.926–0.972) | 13–18 | 13.507 | 0.911 (0.846–0.977) | 0.920 (0.897–0.943) |
| Group 1 | Group 2 | Group 3 | Overall | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Age Range (years) | Cut Off | Over-Triage Rate Under-Triage Rate | Age Range (years) | Cut Off | Over-Triage Rate Under-Triage Rate | Age Range (years) | Cut Off | Over-Triage Rate Under-Triage Rate | Over-Triage Rate Under-Triage Rate |
| 2 Groups AUC | 0–14 | 14.8 | 35.87 15.18 | 15–18 | 20.9 | 35.64 5.47 | - | - | - | 35.82 10.00 |
| 2 Groups AIC | 0–10 | 13.3 | 28.04 20.25 | 11–18 | 19.3 | 28.07 5.59 | - | - | - | 30.78 10.42 |
| 3 Groups AUC | 0–9 | 13.3 | 29.57 18.92 | 10–14 | 18.4 | 30.62 2.63 | 15–18 | 20.9 | 35.64 5.47 | 30.94 9.17 |
| 3 Groups AIC | 0–4 | 12.2 | 29.83 22.73 | 5–14 | 16.7 | 33.99 10.29 | 15–18 | 20.9 | 35.64 5.47 | 33.78 10.00 |
| 3 Groups SIPA | 0–6 | 12.6 | 29.96 22.95 | 7–12 | 16.1 | 23.60 9.68 | 13–18 | 19.3 | 23.65 6.08 | 29.62 10.83 |
| Group 1 | Group 2 | Group 3 | Overall | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Age Range (years) | Cutoff | Over-Triage Rate Under-Triage Rate | Age Range (years) | Cutoff | Over-Triage Rate Under-Triage Rate | Age Range (years) | Cutoff | Over-Triage Rate Under-Triage Rate | Over-Triage Rate Under-Triage Rate |
| 2 Groups AUC | 0–14 | 9.643 | 2.3323.21 | 15–18 | 13.507 | 1.529.38 | - | - | - | 2.1815.83 |
| 2 Groups AIC | 0–10 | 9.643 | 2.8327.85 | 11–18 | 13.507 | 1.619.32 | - | - | - | 2.4115.42 |
| 3 Groups AUC | 0–9 | 9.643 | 3.0027.03 | 10–14 | 12.092 | 0.7013.16 | 15–18 | 13.507 | 1.529.38 | 2.2715.42 |
| 3 Groups AIC | 0–4 | 7.558 | 0.5231.82 | 5–14 | 10.142 | 0.3317.65 | 15–18 | 13.507 | 1.529.38 | 0.6215.83 |
| 3 Groups SIPA | 0–6 | 7.558 | 0.4131.15 | 7–12 | 12.089 | 1.5919.35 | 13–18 | 13.507 | 1.438.78 | 0.9915.83 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, S.J.; Kim, M.J.; Kim, H.Y.; Park, S.Y.; Park, Y.S.; Kim, M.K.; Lee, J.H.; Yoon, S.H. Determining the Optimal Cutoff Value for the Reverse Shock Index Multiplied by the Glasgow Coma Scale for the Prediction of In-Hospital Mortality in Pediatric Trauma Patients: A Retrospective Cohort Study. J. Clin. Med. 2025, 14, 2994. https://doi.org/10.3390/jcm14092994
Choi SJ, Kim MJ, Kim HY, Park SY, Park YS, Kim MK, Lee JH, Yoon SH. Determining the Optimal Cutoff Value for the Reverse Shock Index Multiplied by the Glasgow Coma Scale for the Prediction of In-Hospital Mortality in Pediatric Trauma Patients: A Retrospective Cohort Study. Journal of Clinical Medicine. 2025; 14(9):2994. https://doi.org/10.3390/jcm14092994
Chicago/Turabian StyleChoi, Sol Ji, Min Joung Kim, Ha Yan Kim, Shin Young Park, Yoo Seok Park, Moon Kyu Kim, Ji Hwan Lee, and Seo Hee Yoon. 2025. "Determining the Optimal Cutoff Value for the Reverse Shock Index Multiplied by the Glasgow Coma Scale for the Prediction of In-Hospital Mortality in Pediatric Trauma Patients: A Retrospective Cohort Study" Journal of Clinical Medicine 14, no. 9: 2994. https://doi.org/10.3390/jcm14092994
APA StyleChoi, S. J., Kim, M. J., Kim, H. Y., Park, S. Y., Park, Y. S., Kim, M. K., Lee, J. H., & Yoon, S. H. (2025). Determining the Optimal Cutoff Value for the Reverse Shock Index Multiplied by the Glasgow Coma Scale for the Prediction of In-Hospital Mortality in Pediatric Trauma Patients: A Retrospective Cohort Study. Journal of Clinical Medicine, 14(9), 2994. https://doi.org/10.3390/jcm14092994






