Systemic Capillary Leak Syndrome (Clarkson Syndrome) in Cancer Patients: A Systematic Review
Abstract
1. Introduction
2. Methods
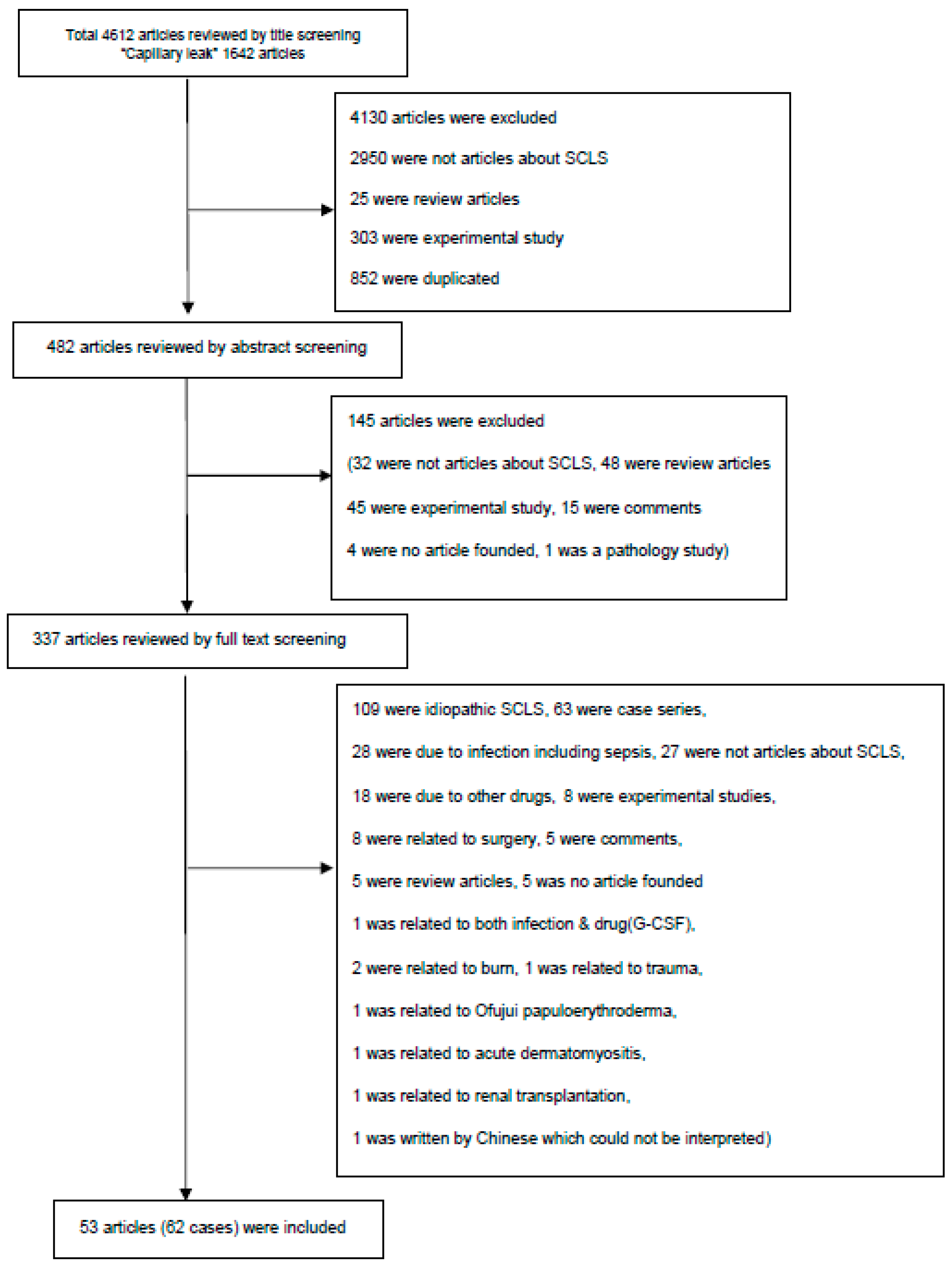
2.1. Literature Search and Study Selection
2.2. Data Extraction
2.3. Analyses of Case Reports
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Conflicts of Interest
References
- Clarkson, B.; Thompson, D.; Horwith, M.; Luckey, E.H. Cyclical edema and shock due to increased capillary permeability. Am. J. Med. 1960, 29, 193–216. [Google Scholar] [CrossRef]
- Druey, K.M.; Greipp, P.R. Narrative review: The systemic capillary leak syndrome. Ann. Intern. Med. 2010, 153, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Druey, M.; Parikh, S.M. Idiopathic systemic capillary leak syndrome (Clarkson disease). J. Allergy Clin. Immunol. 2017, 140, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Duron, L.; Delestre, F.; Amour, Z.; Arnaud, L. Idiopathic and secondary capillary leak syndromes: A systematic review of the literature. Rev. Med. Interne. 2015, 36, 386–394. [Google Scholar] [CrossRef] [PubMed]
- Eo, T.S.; Chun, K.J.; Hong, S.J.; Kim, J.Y.; Lee, I.R.; Lee, K.H.; Eisenhut, M.; Kronbichler, A.; Shin, J.I. Clinical presentation, management, and prognostic factors of idiopathic systemic capillary leak syndrome: A systematic review. J. Allergy Clin. Immunol. Pract. 2018, 6, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Pineton De Chambrun, M.; Gousseff, M.; Mauhin, W.; Lega, J.C.; Lambert, M.; Rivière, S.; Dossier, A.; Ruivard, M.; Lhote, F.; Blaison, G.; et al. Intravenous immunoglobulins improve survival in monoclonal gammopathy-associated systemic capillary-leak syndrome. Am. J. Med. 2017, 130. [Google Scholar] [CrossRef] [PubMed]
- Banerji, A.; Weller, P.F.; Sheikh, J. Cytokine-associated angioedema syndromes including episodic angioedema with eosinophilia (Gleich’s syndrome). Immunol. Allergy Clin. N. Am. 2006, 26, 769–781. [Google Scholar] [CrossRef] [PubMed]
- Bonadies, N.; Baud, P.; Peter, H.J.; Buergi, U.; Mueller, B.U. A case report of Clarkson’s disease: If you don’t know it, you’ll miss it. Eur. J. Intern. Med. 2006, 17, 363–365. [Google Scholar] [CrossRef] [PubMed]
- Cicardi, M.; Gardinali, M.; Bisiani, G.; Rosti, A.; Allavena, P.; Agostoni, A. The systemic capillary leak syndrome: Appearance of interleukin-2-receptor-positive cells during attacks. Ann. Intern. Med. 1990, 113, 475–477. [Google Scholar] [CrossRef] [PubMed]
- Dowden, A.M.; Rullo, O.J.; Aziz, N.; Fasano, M.B.; Chatila, T.; Ballas, Z.K. Idiopathic systemic capillary leak syndrome: Novel therapy for acute attacks. J. Allergy Clin. Immunol. 2009, 124, 1111–1113. [Google Scholar] [CrossRef] [PubMed]
- Cicardi, M.; Berti, E.; Caputo, V.; Radice, F.; Gardinali, M.; Agostoni, A. Idiopathic capillary leak syndrome: Evidence of CD8-positive lymphocytes surrounding damaged endothelial cells. J. Allergy Clin. Immunol. 1997, 99, 417–419. [Google Scholar] [CrossRef]
- Johansson, B.R.; Lofdahl, C.G. Ultrastructure of the microvessels in skeletal muscle in a case of systemic capillary leak syndrome. Acta. Med. Scand. 1979, 206, 413–416. [Google Scholar] [CrossRef] [PubMed]
- Assaly, R.; Olson, D.; Hammersley, J.; Fan, P.S.; Liu, J.; Shapiro, J.I.; Kahaleh, M.B. Initial evidence of endothelial cell apoptosis as a mechanism of systemic capillary leak syndrome. Chest 2001, 120, 1301–1308. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Chan, E.; Yin, Y.; Ghosh, C.C.; Wisch, L.; Nelson, C.; Young, M.; Parikh, S.M.; Druey, K.M. Inflammatory markers of the systemic capillary leak syndrome (Clarkson disease). J. Clin. Cell Immunol. 2014, 5, 1000213. [Google Scholar] [PubMed]
- Hsu, P.; Xie, Z.; Frith, K.; Wong, M.; Kakakios, A.; Stone, K.D.; Druey, K.M. Idiopathic systemic capillary leak syndrome in children. Pediatrics 2015, 135, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Ghosh, C.C.; Patel, R.; Iwaki, S.; Gaskins, D.; Nelson, C.; Jones, N.; Greipp, P.R.; Parikh, S.M.; Druey, K.M. Vascular endothelial hyperpermeability induces the clinical symptoms of Clarkson disease (the systemic capillary leak syndrome). Blood 2012, 119, 4321–4332. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, D.C.; Bhatt, R.S.; Parikh, S.M.; Patel, P.; Seery, V.; McDermott, D.F.; Atkins, M.B.; Sukhatme, V.P. Angiopoietin 2 is a potential mediator of high-dose interleukin 2-induced vascular leak. Clin. Cancer Res. 2007, 13, 2115–2120. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.C.; Lai, A.; Kompala, T.; Ten, R. Mimicker of hereditary angioedema: Idiopathic systemic capillary leak syndrome successfully treated with intravenous immunoglobulin. Ann. Allergy Asthma Immunol. 2017, 118, 631–632. [Google Scholar] [CrossRef] [PubMed]
- Marra, A.M.; Gigante, A.; Rosato, E. Intravenous immunoglobulin in systemic capillary leak syndrome: A case report and review of literature. Expert Rev. Clin. Immunol. 2014, 10, 349–352. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.I.; Lee, J.S. Beneficial effect of intravenous immunoglobulins on systemic capillary leak syndrome in patients with monoclonal gammopathy. Crit. Care Med. 2009, 37, 795. [Google Scholar] [CrossRef] [PubMed]
| Variables | Observed Number of Patients (%) among Total Number of Patients (n = 62) |
|---|---|
| Age (years) | |
| <10 | 5 (8.1%) |
| 10–19 | 8 (12.9%) |
| 20–29 | 1 (1.6%) |
| 30–39 | 8 (12.9%) |
| 40–49 | 11 (17.7%) |
| 50–59 | 12 (19.4%) |
| >60 | 17 (27.4%) |
| Sex | |
| Male | 40 (64.5%) |
| Female | 22 (35.5%) |
| Diagnosis of cancer | |
| Hematologic malignancy | 38 (61.3%) |
| Hodgkin lymphoma | 4 (6.5%) |
| Non-Hodgkin lymphoma | 14 (22.7%) |
| Multiple myeloma | 8 (12.9%) |
| Hemophagocytic lymphohistiocytosis | 3 (4.8%) |
| Acute lymphoblastic leukemia | 2 (3.2%) |
| Acute myeloid leukemia | 1 (1.6%) |
| Chronic myelocytic leukemia | 2 (3.2%) |
| Plasma cell leukemia | 1 (1.6%) |
| Malignant lymphoma of tonsil | 1 (1.6%) |
| Malignant lymphoma of cervical cord | 1 (1.6%) |
| Fanconi anemia | 1 (1.6%) |
| Non-hematologic malignancy | 24 (38.7%) |
| Renal cell carcinoma | 4 (6.5%) |
| Colorectal cancer | 4 (6.5%) |
| Pancreatic cancer | 3 (4.8%) |
| Hepatic carcinoma | 2 (3.2%) |
| Non-small cell lung cancer | 2 (3.2%) |
| Breast cancer | 2 (3.2%) |
| Pituitary adenoma | 1 (1.6%) |
| Primitive neuroectodermal tumor | 1 (1.6%) |
| Distal common bile duct cancer | 1 (1.6%) |
| Nasopharyngeal cancer | 1 (1.6%) |
| Ovarian cystic teratoma | 1 (1.6%) |
| Sarcoma | 1 (1.6%) |
| Myxofibroma of maxilla | 1 (1.6%) |
| Variables | Total Number of Patients (n = 62) Observed Number of Patients (%) |
|---|---|
| Cancer * | 27 (43.6%) |
| BMT-related GVHD | 3 (4.8%) |
| Anti-cancer agents | 32 (51.6%) |
| G-CSF | 9 (14.6%) |
| Interleukin-2 | 7 (11.4%) |
| Denileukin diftitox | 2 (3.2%) |
| Gemcitabine | 2 (3.2%) |
| MINE regimen | 2 (3.2%) |
| Gemcitabine + paclitaxel | 1 (1.6%) |
| Doxorubicin | 1 (1.6%) |
| Bortezomib | 1 (1.6%) |
| Clofarabine | 1 (1.6%) |
| Cyclosporin A | 1 (1.6%) |
| Trastuzumab | 1 (1.6%) |
| Busulfan + etoposide + nimustine | 1 (1.6%) |
| Pemetrexed | 1 (1.6%) |
| Oxaliplatin | 1 (1.6%) |
| Oxaliplatin + capecitabine | 1 (1.6%) |
| Clinical Presentation | Observed Number of Patients (%) among Total Number of Patients (n = 62) |
|---|---|
| General condition | |
| Edema | 42 (67.7%) |
| Weight gain | 13 (21.0%) |
| Malaise | 5 (8.1%) |
| General weakness | 3 (4.8%) |
| Skin rash | 4 (6.4%) |
| Hot flushing | 1 (1.6%) |
| Sweating | 1 (1.6%) |
| Gum hypertrophy | 1 (1.6%) |
| Weight loss | 1 (1.6%) |
| Disturbance of consciousness | 1 (1.6%) |
| Inflammation-related | |
| Fever | 11 (17.7%) |
| Lymph node enlargement | 3 (4.8%) |
| Otalgia | 1 (1.6%) |
| Pulmonary | |
| Dyspnea | 17 (27.4%) |
| Pleural effusion | 18 (29.0%) |
| Pulmonary edema | 7 (11.3%) |
| Tachypnea | 5 (8.1%) |
| Hypoxemia | 4 (6.4%) |
| Pulmonary hypertension | 1 (1.6%) |
| Cardiovascular | |
| Hypotension | 20 (32.2%) |
| Hypertension | 3 (4.8%) |
| Pericardial effusion | 6 (9.7%) |
| Tachycardia | 5 (8.1%) |
| Bradycardia | 1 (1.6%) |
| Chest pain | 1 (1.6%) |
| Syncope | 1 (1.6%) |
| Decreased exercise tolerance | 1 (1.6%) |
| Pericarditis | 1 (1.6%) |
| Gastrointestinal | |
| Ascites | 14 (22.7%) |
| Nausea | 3 (4.8%) |
| Vomiting | 4 (6.4%) |
| Abdominal distention | 3 (4.8%) |
| Diarrhea | 2 (3.2%) |
| Hepatosplenomegaly | 1 (1.6%) |
| Renal | |
| Oliguria | 14 (22.7%) |
| Proteinuria | 1 (1.6%) |
| Neurologic | |
| Dizziness | 1 (1.6%) |
| Back discomfort | 1 (1.6%) |
| Tremor | 1 (1.6%) |
| Paresthesia | 1 (1.6%) |
| Laboratory Findings | Total Number of Patients (n = 62) Observed/Measured Number of Patients (%) |
|---|---|
| WBC count | |
| Leukocytosis (>15,000/μL) | 11/27 (40.1%) |
| Leukopenia (<4000/μL) | 9/27 (33.3%) |
| Normal (4000–15,000/μL) | 7/27 (25.9%) |
| No information | 35/62 (56.4%) |
| Hemoglobin | |
| Anemia (<12.0 g/dL) | 12/25 (48.0%) |
| Polycythemia (>15.0 g/dL) | 6/25 (24.0%) |
| Normal (12.0–15.0 g/dL) | 7/25 (28.0%) |
| No information | 37/62(60.0%) |
| Hematocrit | |
| Hemoconcentration (Hct > 41%) | 7/11 (63.6%) |
| Decreased hematocrit (Hct < 30%) | 2/11 (18.2%) |
| Normal (Hct 30–41%) | 2/11 (18.2%) |
| No information | 51/62 (82.3%) |
| Platelet count | |
| Thrombocytopenia (<150,000/μL) | 14/19 (73.7%) |
| Normal (150,000–450,000/μL) | 5/19 (26.3%) |
| No information | 43/62 (69.4%) |
| Albumin | |
| Very low (<2.5 g/dL) | 16/32 (50.0%) |
| Low (2.5–3.5 g/dL) | 15/32 (46.9%) |
| Normal (>3.5 g/dL) | 1/32 (3.1%) |
| No information | 30/62 (48.4%) |
| Treatment | Observed Number of Patients (%) among Total Number of Patients (n = 62) |
|---|---|
| Steroids | 37 (59.7%) |
| Methylprednisolone | 14 (22.7%) |
| Prednisolone | 12 (19.4%) |
| Cortisone | 4 (6.4%) |
| Hydrocortisone | 3 (4.8%) |
| Dexamethasone | 2 (3.2%) |
| Methylprednisolone → prednisolone | 1 (1.6%) |
| Other steroids | 1 (1.6%) |
| Volume replacement | 21 (33.8%) |
| Fluid resuscitation | 4 (6.4%) |
| Crystalloid/colloid | 2 (3.2%) |
| Transfusion * | 1 (1.6%) |
| Albumin | 11 (17.7%) |
| Hydroxyethyl starch | 1 (1.6%) |
| Fluid resuscitation + albumin | 1 (1.6%) |
| Fluid resuscitation + transfusion + albumin + hydroxyethyl starch | 1 (1.6%) |
| Diuretics | 15 (24.2%) |
| Furosemide | 6 (9.6%) |
| Other diuretics | 9 (14.6%) |
| Inotropes | 6 (9.6%) |
| Dopamine | 1 (1.6%) |
| Norepinephrine | 1 (1.6%) |
| Other vasopressors | 4 (6.4%) |
| Methylxanthines | 8 (12.8%) |
| Theophylline | 6 (9.6%) |
| Aminophylline | 2 (3.2%) |
| β2 agonists | 3 (4.8%) |
| Terbutaline | 2 (3.2%) |
| Terbutaline + tulobuterol | 1 (1.6%) |
| Intravenous immunoglobulins | 2 (3.2%) |
| Chemotherapeutic or immunosuppressive agents † | 7 (11.3%) |
| Cyclosporine A | 2 (3.2%) |
| Cyclophosphamide | 1 (1.6%) |
| Melphalan | 1 (1.6%) |
| Chloraminophene | 1 (1.6%) |
| Bevacizumab | 1 (1.6%) |
| Cyclosporine A + cyclophosphamide + melphalan | 1 (1.6%) |
| Other agents | 6 (9.6%) |
| Antibiotics (cefepime + vancomycin) | 1 (1.6%) |
| Antihistamine | 1 (1.6%) |
| Leukotriene antagonist (Montelukast®) | 1 (1.6%) |
| Serine protease inhibitor (Ulinastatin®) | 1 (1.6%) |
| Radiosone | 1 (1.6%) |
| Naftazone | 1 (1.6%) |
| Procedure | 5 (8.0%) |
| SLEDD | 1 (1.6%) |
| CRRT | 1 (1.6%) |
| Pericardial/thoracic/ascites drainage | 2 (3.2%) |
| Plasma exchange | 1 (1.6%) |
| Variables | Univariate Cox Proportional Hazard Model | ||
|---|---|---|---|
| Hazard Ratio | 95% CI | p Value | |
| Age | 1.005 | 0.978 to 1.032 | 0.739 |
| Sex | 1.293 | 0.415 to 4.024 | 0.657 |
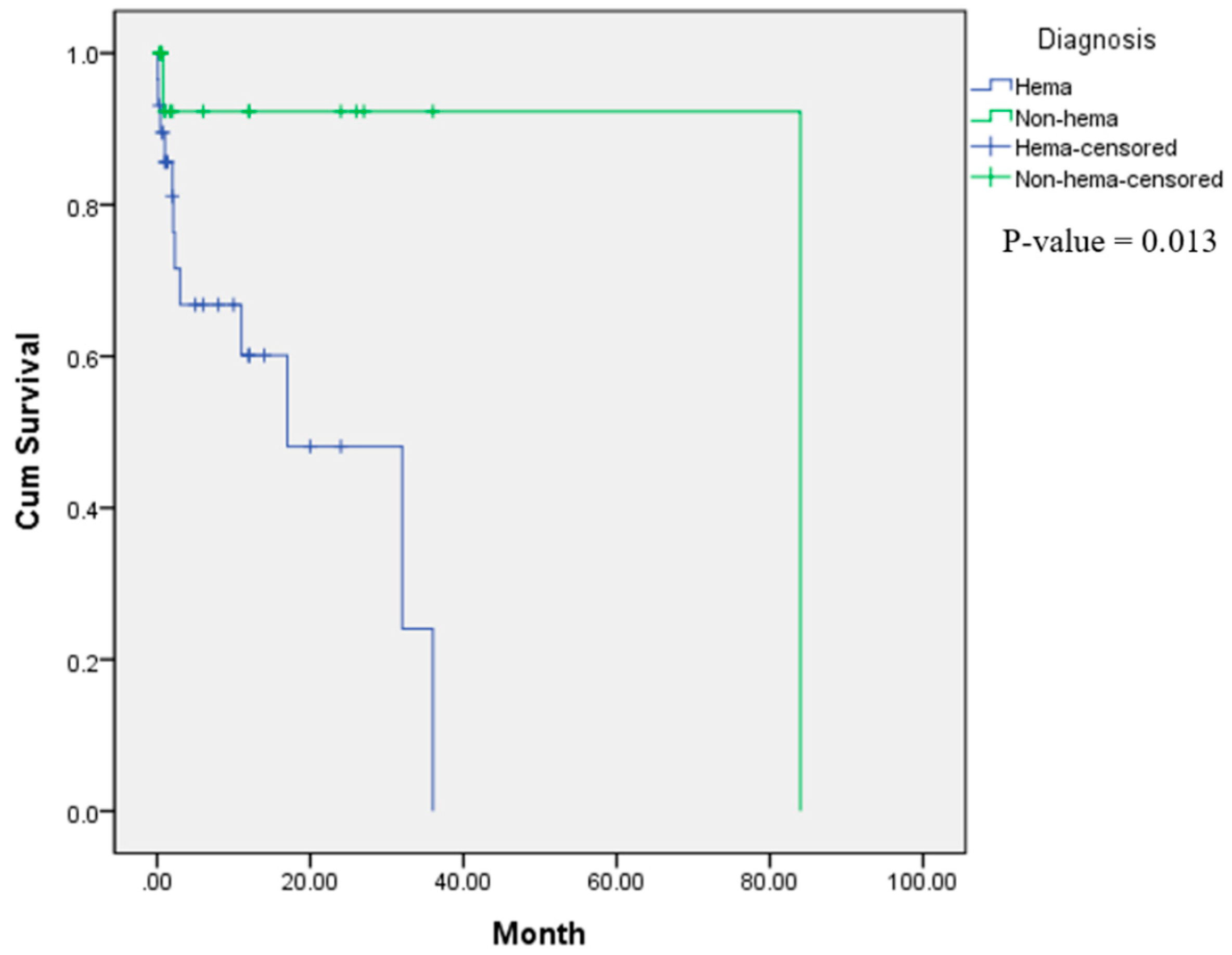
| Hematologic | 8.820 | 1.126 to 69.063 | 0.038 |
| Cancer-induced | 0.498 | 0.161 to 1.543 | 0.227 |
| Drug-induced | 2.455 | 0.794 to 7.591 | 0.119 |
| SBP | 1.012 | 0.945 to 1.085 | 0.728 |
| DBP | 1.371 | 0.452 to 4.16 | 0.578 |
| Hypotension | 1.235 | 0.36 to 4.244 | 0.737 |
| Alb | 1.379 | 0.417 to 4.558 | 0.598 |
| Alb < 2.5 g/dL | 3.878 | 0.402 to 37.423 | 0.241 |
| Alb < 3.0 g/dL | 1.687 | 0.17 to 16.773 | 0.655 |
| WBC | 1.000 | 1 to 1 | 0.352 |
| WBC > 15,000/μL | 0.022 | 0 to 2908.101 | 0.526 |
| Hemoglobin | 1.059 | 0.863 to 1.301 | 0.582 |
| Platelet | 1.000 | 1 to 1 | 0.600 |
| Steroid | 0.561 | 0.169 to 1.858 | 0.344 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, J.I.; Lee, K.H.; Lee, I.R.; Oh, J.H.; Kim, D.W.; Shin, J.W.; Eo, T.S.; Kronbichler, A.; Eisenhut, M.; Van der Vliet, H.J. Systemic Capillary Leak Syndrome (Clarkson Syndrome) in Cancer Patients: A Systematic Review. J. Clin. Med. 2018, 7, 418. https://doi.org/10.3390/jcm7110418
Shin JI, Lee KH, Lee IR, Oh JH, Kim DW, Shin JW, Eo TS, Kronbichler A, Eisenhut M, Van der Vliet HJ. Systemic Capillary Leak Syndrome (Clarkson Syndrome) in Cancer Patients: A Systematic Review. Journal of Clinical Medicine. 2018; 7(11):418. https://doi.org/10.3390/jcm7110418
Chicago/Turabian StyleShin, Jae Il, Keum Hwa Lee, I. Re Lee, Ji Hyun Oh, Dong Wook Kim, Jae Won Shin, Tae Seong Eo, Andreas Kronbichler, Michael Eisenhut, and Hans J. Van der Vliet. 2018. "Systemic Capillary Leak Syndrome (Clarkson Syndrome) in Cancer Patients: A Systematic Review" Journal of Clinical Medicine 7, no. 11: 418. https://doi.org/10.3390/jcm7110418
APA StyleShin, J. I., Lee, K. H., Lee, I. R., Oh, J. H., Kim, D. W., Shin, J. W., Eo, T. S., Kronbichler, A., Eisenhut, M., & Van der Vliet, H. J. (2018). Systemic Capillary Leak Syndrome (Clarkson Syndrome) in Cancer Patients: A Systematic Review. Journal of Clinical Medicine, 7(11), 418. https://doi.org/10.3390/jcm7110418







