Options for Fertility Treatments for Trans Women in Germany
Abstract
:1. Introduction
2. Testicular Tissue and Steroidogenesis of Trans Women
3. Testicular Tissues and Steroidogenesis in Our Cohort of Trans Women
4. Clinical Approach towards Trans Women
5. Options for Fertility Preservation for Trans Women
5.1. Fertility Preservation Options before Initiation of GCHT
5.2. Fertility Preservation Options during GCHT
5.3. Fertility Preservation on the Day of GCS
5.4. Fertility Preservation Options after GCS
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| DSD | Disorders of sexual development |
| FSH | Follicle-stimulating hormone |
| GCS | Gender confirming surgery |
| GCHT | Gender confirming hormone therapy |
| LH | Luteinizing hormone |
| LHCGR | Lutropin-choriogonadotropic hormone receptor |
| MAGE A4 | Melanoma-associated antigen 4 |
| MESA | Microsurgical epididymal sperm aspiration |
| mTESE | Microsurgical testicular sperm extraction |
| OAT-syndrome | Oligo-astheno-teratozoospermia-syndrome |
| PAS | Periodic acid-Schiff |
| SALL-4 | Sal like protein 4 |
| SCO | Sertoli cell only syndrome |
| SHBG | Sex hormone binding globuline |
| SMA | Smooth muscle actin |
| SSC | Spermatogonial stem cell |
| UTF-1 | Undifferentiated transcription factor 1 |
| VASA/DDX4 | DEAD-box helicase 4 |
| VIM | Vimentin |
| WPATH | World Professional Association of Transgender Health |
References
- Picton, H.; Wyns, C.; Anderson, R.; Goossens, E.; Jahnukainen, K.; Kliesch, S.; Mitchell, R.; Pennings, G.; Rives, N.; Tournaye, H.; et al. A European perspective on testicular tissue cryopreservation for fertility preservation in prepubertal and adolescent boys. Hum. Rep. 2015, 30, 2463–2475. [Google Scholar] [CrossRef]
- World Professional Association for Transgender Health (WPATH). Standards of care for the health of transsexual, transgender, and gender-nonconforming people, 7th version. Int. J. Transgenderism 2011, 13, 165–232. [Google Scholar]
- Geschlechtsinkrongruenz, Geschlechtsdysphorie und Trans-Gesundheit: S3-Leitlinie zur Diagnostik, Beratung und Behandlung. Available online: https://www.awmf.org/leitlinien/detail/ll/138-001.html (accessed on 21 March 2019).
- De Roo, C.; Tilleman, K.; T’Sjoen, G.; De Sutter, P. Fertility options in transgender people. Int. Rev. Psychiatry 2016, 28, 112–119. [Google Scholar] [CrossRef]
- Wierckx, K.; Stuyver, I.; Weyers, S.; Hamada, A.; Agarwal, A.; de Sutter, P.; T’Sjoen, G. Sperm Freezing in Transsexual Women. Arch. Sex. Behav. 2012, 41, 1069–1071. [Google Scholar] [CrossRef]
- Feigerlova, E.; Pascal, V.; Ganne-Devonec, M.O.; Klein, M.; Guerci, B. Fertility desires and reproductive needs of transgender people: Challenges and considerations for clinical practice. Clin. Endocrinol. 2019. [Google Scholar] [CrossRef]
- Murphy, T. Bioethics, children, and the environment. Bioethics 2018, 32, 3–9. [Google Scholar] [CrossRef]
- De Sutter, P. Gender reassignment and assisted reproduction: Present and future reproductive options for transsexual people. Hum. Reprod. 2001, 16, 612–614. [Google Scholar] [CrossRef]
- Nahata, L.; Tishelman, A.C.; Caltabellotta, N.M.; Quinn, G.P. Low fertility. preservation utilization among transgender youth. J. Adolesc. Health 2017, 61, 40–44. [Google Scholar] [CrossRef]
- Chen, D.; Simons, L.; Johnson, E.K.; Lockart, B.A.; Finlay, C. Fertility preservation for. transgender adolescents. J. Adolesc. Health 2017, 61, 120–123. [Google Scholar] [CrossRef]
- Cartaya, J.; Lopez, X. Gender dysphoria in youth: A review of recent literatur. Curr. Opin. Endocrinol. Diabetes Obes. 2018, 44–48. [Google Scholar] [CrossRef]
- Millar, A.; Kim, B.H.K.; Livne-Segev, D.; Fung, R.; Jarvi, K.; Millar, A.C. Attitudes, knowledge and beliefs regarding fertility preservation among people of. transgendered experience: Preliminary results. Can. J. Diabetes 2015, 39, 536. [Google Scholar] [CrossRef]
- Jones, C.A.; Reiter, L.; Greenblatt, E. Fertility preservation in transgender. patients. Int. J. Transgend. 2016, 17, 76–82. [Google Scholar] [CrossRef]
- Riggs, D.; Bartholomaeus, C. Fertility preservation decision making amongst Australian transgender and non-binary adults. Reprod. Health 2018, 15. [Google Scholar] [CrossRef] [PubMed]
- De Sutter, P.; Kira, K.; Verschoor, A.; Hotimsky, A. The desire to have children. and the preservation of fertility in transsexual women: A survey. Int. J. Transgend. 2002, 6, 97–103. [Google Scholar]
- Auer, M.K.; Fuss, J.; Nieder, T.O.; Briken, P.; Biedermann, S.V.; Biedermann, G.K.; Beckmann, M.W.; Hildebrand, T. Desire to Have Children Among Transgender People in Germany: A Cross-Sectional Multi-Center Study. J. Sex. Med. 2018, 15, 757–767. [Google Scholar] [CrossRef]
- Wierckx, K.; Van Caenegem, E.; Pennings, G.; Elaut, E.; Dedecker, D.; Van de Peer, F.; Weyers, S.; De Sutter, P.; T’Sjoen, G. Reproductive wish in transsexual men. Hum. Reprod. 2012, 27, 483–487. [Google Scholar] [CrossRef]
- Light, A.; Obedin-Maliver, J.; Sevelius, J.; Kerns, J. Transgender Men Who Experienced Pregnancy After Female-to-Male Gender Transitioning. Obstet. Gynecol. 2014, 124, 1120–1127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldman, R.; Kaser, D.; Missmer, S.; Farland-Scout, L.; Ashby, R.; Ginsburg, E. Fertility treatment for the transgender community: A public opinion study. J. Assist. Reprod. Genet. 2017, 34, 1457–1467. [Google Scholar] [CrossRef]
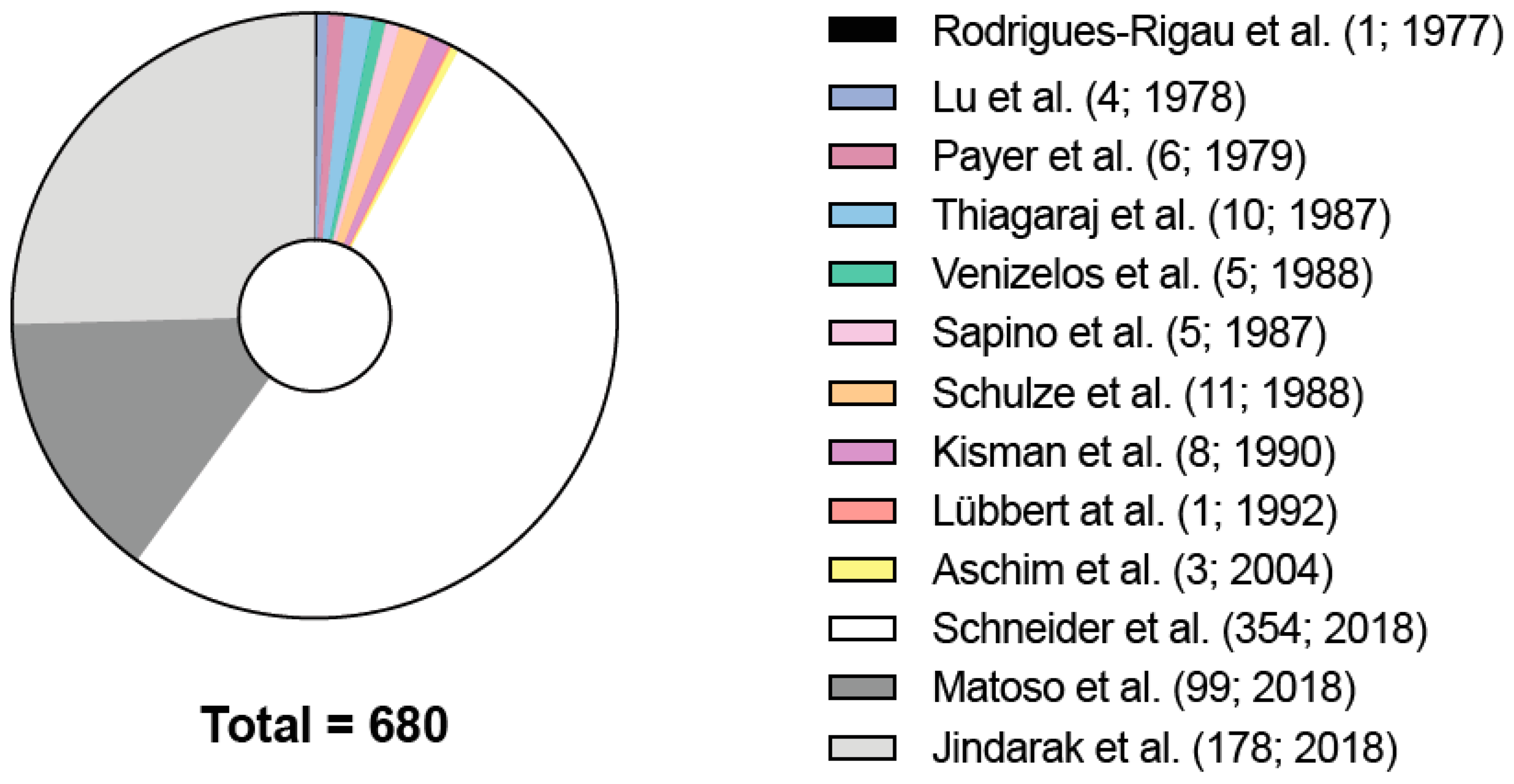
- Schneider, F.; Neuhaus, N.; Wistuba, J.; Zitzmann, M.; Hess, J.; Mahler, D.; von Ahlen, H.; Schlatt, S.; Kliesch, S. Testicular functions and clinical characterization of patients with gender dysphoria (GD) undergoing sex reassignment surgery (SRS). J. Sex. Med. 2015, 12, 2190–2200. [Google Scholar] [CrossRef]
- Matoso, A.; Khandakar, B.; Yuan, S.; Wu, T.; Wang, L.; Lombardo, K.; Mangray, S.; Mannan, A.; Yakirevich, E. Spectrum of findings in orchiectomy specimens of persone undergoing gender confirmation surgery. Hum. Pathol. 2018, 76, 91–99. [Google Scholar] [CrossRef]
- Jindarak, S.; Nilprapha, K.; Atikankul, T.; Angspatt, A.; Pungrasmi, P.; Iamphongsai, S.; Promniyom, P.; Suwajo, P.; Selvaggi, G.; Tiewtranon, P. Spermatogenesis Abnormalities following Hormonal Therapy in Transwomen. BioMed Res. Int. 2018. [Google Scholar] [CrossRef]
- Byne, W.; Bradley, S.J.; Coleman, E.; Eyler, A.E.; Green, R.; Menvielle, E.J.; Meyer-Bahlburg, H.F.; Pleak, R.R.; Tompkins, D.A. American Psychiatric Association Task Force on Treatment of Gender Identity Disorder. Report of the American psychiatric association task force on treatment of gender identity disorder. Arch. Sex. Behav. 2012, 41, 759–796. [Google Scholar] [CrossRef]
- T’Sjoen, G.; van Caenegem, E.; Wierckx, K. Transgenderism and reproduction. Curr. Opin. Endocrinol. Diabetes Obes. 2012, 20, 575–579. [Google Scholar] [CrossRef] [PubMed]
- Mitu, K. Transgender Reproductive Choice and Fertlity Preservation. AMA J. Ethics 2016, 18, 1119–1125. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, B.; Boguszweski, K.; Cheney, D.; Taylor, J. Trends in Fertility Preservation for Transgender Adolescents and Young Adults at an Acedemic Referral Center. J. Adolesc. Health 2018, 62, 37–140. [Google Scholar] [CrossRef]
- Brik, T.; Vrouenraets, L.; Schagen, S.; Meissner, A.; de Vries, M.; Hannema, S. Use of Fertility Preservation Among a Cohort of Transgirls in the Netherlands. J. Adolesc. Health 2019. [Google Scholar] [CrossRef]
- Strang, J.F.; Jarin, J.; Call, D.; Clark, B.; Wallace, G.L.; Anthony, L.G.; Kenworthy, L.; Gomez-Lobo, V. Transgender Youth Fertility Attitudes Questionnaire: Measure Development in Nonautistic and Autistic Transgender Youth and Their Parents. J. Adolesc. Health 2018, 62, 128–135. [Google Scholar] [CrossRef]
- Arcelus, J.; Bouman, W.P.; van den Noortgate, W.; Claes, L.; Witcomb, G. Fernandez-Aranda Systematic review and meta-analysis of prevalence studies in transsexualism. Eur. Psychiatry 2015, 30, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Mattawanon, N.; Spencer, J.B.; Schirmer, D.A.; Trangpricha, V. Fertility preservation options in transgender people: A review. Rev. Endocr. Metab. Disord. 2018, 19, 231–242. [Google Scholar] [CrossRef] [PubMed]
- James-Abra, S.; Tarasoff, L.A.; Epstein, R.; Anderson, S.; Marvel, S.; Steele, L.S.; Ross, L.E. Trans people’s experiences with assisted reproduction services: A qualitative study. Hum. Rep. 2015, 30, 1365–1374. [Google Scholar] [CrossRef] [PubMed]
- Kosenko, K.; Rintamaki, L.; Raney, S.; Maness, K. Transgender Patient Perceptions of Stigma in Health Care Contexts. Med. Care 2013, 51, 819–822. [Google Scholar] [CrossRef]
- Payne, J.G.; Erbenius, T. Conceptions of transgender parenthood fertility care and family planning in Sweden: From reproductive rights to concrete practices. Anthropol. Med. 2018, 25, 329–343. [Google Scholar] [CrossRef]
- Tornello, S.; Bos, H. Parenting Intentions Among Transgender Individuals. LGBT Health 2017, 4, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Weinbauer, G.F.; Luetjens, C.M.; Simoni, M.; Nieschlag, E. Physiology of testicular function. In Andrology—Male Reproductive Health and Dysfunction; Nieschlag, E., Behre, H.M., Nieschlag, S., Eds.; Springer-Verlag: Berlin/Heidelberg, Germany, 2010; pp. 11–60. [Google Scholar]
- Schneider, F.; Kliesch, S.; Schlatt, S.; Neuhaus, N. Andrologoy of Male-to-Female transsexuals: Influence of cross-sex hormone therapy on testicular function. Andrology 2017, 5, 873–880. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Rigau, L.J.; Tcholakian, R.K.; Smith, K.D.; Steinberger, E. In vitro steroid metabolic studies in human testes. II: Metabolism of cholesterol, pregnenolone, progesterone, androstenedione and testosterone by testes of an estrogen-treated man. Steroids 1977, 30, 729–739. [Google Scholar] [CrossRef]
- Lu, C.C.; Steinberger, A. Effects of estrogen on human seminiferous tubules: Light and electron microscopic analysis. Am. J. Anat. 1978, 153, 1–13. [Google Scholar] [CrossRef]
- Payer, A.F.; Meyer, W.J.; Walker, P.A. The ultrastructural response of human Leydig cells to exogenous estrogens. Andrologia 1979, 11, 423–436. [Google Scholar] [CrossRef] [PubMed]
- Thiagaraj, D.; Gunasegaram, R.; Loganath, A.; Peh, K.L.; Kottegoda, S.R.; Ratnam, S.S. Histopathology of the testes from male transsexuals on oestrogen therapy. Ann. Acad. Med. Singapore 1987, 16, 347–348. [Google Scholar] [PubMed]
- Venizelos, I.D.; Paradinas, F.J. Testicular atrophy after oestrogen therapy. Histopathology 1988, 12, 451–454. [Google Scholar] [CrossRef]
- Sapino, A.; Pagani, A.; Godano, A.; Bussolati, G. Effects of estrogens on the testis of transsexuals: A pathological and immunocytochemical study. Virchows. Arch. Pathol. Anat. Histopathol. 1987, 411, 409–414. [Google Scholar] [CrossRef]
- Schulze, C. Response of the human testis to long-term estrogen treatment: Morphology of Sertoli cells, Leydig cells and spermatogonial stem cells. Cell Tissue Res. 1988, 251, 31–43. [Google Scholar] [CrossRef]
- Kisman, O.K.; de Voogt, H.J.; Baak, J.A. Reversibility of the effect of LHRH agonists and other antiandrogenic hormones on the testis: A histomorphometric study. Eur. Urol. 1990, 18, 299–301. [Google Scholar] [CrossRef]
- Lubbert, H.; Leo-Rossberg, I.; Hammerstein, J. Effects of ethinyl estradiol on semen quality and various hormonal parameters in a eugonadal male. Fertil. Steril. 1992, 58, 603–608. [Google Scholar] [CrossRef]
- Aschim, E.L.; Saether, T.; Wiger, R.; Grotmol, T.; Haugen, T.B. Differential distribution of splice variants of estrogen receptor beta in human testicular cells suggests specific functions in spermatogenesis. J. Steroid. Biochem. Mol. Biol. 2004, 92, 97–106. [Google Scholar] [CrossRef]
- Bergmann, M.; Kliesch, S. Testicular biopsy and histology. In Andrology: Male Reproductive Health and Dysfunction; Nieschlag, E., Behre, H.M., Nieschlag, S., Eds.; Springer-Verlag: Berlin/Heidelberg, Germany, 2010; pp. 155–167. [Google Scholar]
- Schneider, F.; Redman, K.; Wistuba, J.; Schlatt, S.; Kliesch, S.; Neuhaus, N. Comparison of enzymatic digestion and mechanical dissociation of human testicular tissues. Fertil. Steril. 2015, 104, 302–311. [Google Scholar] [CrossRef]
- Kliesch, S. Androprotect and prospects for fertility treatment. Urologe A 2016, 55, 898–903. [Google Scholar] [CrossRef]
- Cerwanka, S.; Nieder, T.O.; Cohen-Kettenis, P.; de Cuypere, G.; Haraldsen, I.R.; Kreukels, B.P.; Richter-Appelt, H. Sexual behavior of gender dysphoric individuals before gender-confirming interventions: A European multicenter study. J. Sex. Maritial Ther. 2014, 40, 457–471. [Google Scholar] [CrossRef]



© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schneider, F.; Scheffer, B.; Dabel, J.; Heckmann, L.; Schlatt, S.; Kliesch, S.; Neuhaus, N. Options for Fertility Treatments for Trans Women in Germany. J. Clin. Med. 2019, 8, 730. https://doi.org/10.3390/jcm8050730
Schneider F, Scheffer B, Dabel J, Heckmann L, Schlatt S, Kliesch S, Neuhaus N. Options for Fertility Treatments for Trans Women in Germany. Journal of Clinical Medicine. 2019; 8(5):730. https://doi.org/10.3390/jcm8050730
Chicago/Turabian StyleSchneider, Florian, Bettina Scheffer, Jennifer Dabel, Laura Heckmann, Stefan Schlatt, Sabine Kliesch, and Nina Neuhaus. 2019. "Options for Fertility Treatments for Trans Women in Germany" Journal of Clinical Medicine 8, no. 5: 730. https://doi.org/10.3390/jcm8050730
APA StyleSchneider, F., Scheffer, B., Dabel, J., Heckmann, L., Schlatt, S., Kliesch, S., & Neuhaus, N. (2019). Options for Fertility Treatments for Trans Women in Germany. Journal of Clinical Medicine, 8(5), 730. https://doi.org/10.3390/jcm8050730




