High TSH Level within Normal Range Is Associated with Obesity, Dyslipidemia, Hypertension, Inflammation, Hypercoagulability, and the Metabolic Syndrome: A Novel Cardiometabolic Marker
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection
2.4. Definition of Cardiometabolic Risk Factors
2.5. Statistical Analyses
2.6. Mediation Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Silva, J.E. Thyroid hormone control of thermogenesis and energy balance. Thyroid 1995, 5, 481–492. [Google Scholar] [CrossRef] [PubMed]
- Wikström, L.; Johansson, C.; Saltó, C.; Barlow, C.; Campos Barros, A.; Baas, F.; Forrest, D.; Thorén, P.; Vennström, B. Abnormal heart rate and body temperature in mice lacking thyroid hormone receptor alpha 1. EMBO J. 1998, 17, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Mullur, R.; Liu, Y.Y.; Brent, G.A. Thyroid hormone regulation of metabolism. Physiol. Rev. 2014, 94, 355–382. [Google Scholar] [CrossRef] [PubMed]
- Klieverik, L.P.; Coomans, C.P.; Endert, E.; Sauerwein, H.P.; Havekes, L.M.; Voshol, P.J.; Rensen, P.C.; Romijn, J.A.; Kalsbeek, A.; Fliers, E. Thyroid hormone effects on whole-body energy homeostasis and tissue-specific fatty acid uptake in vivo. Endocrinology 2009, 150, 5639–5648. [Google Scholar] [CrossRef]
- Sinha, R.A.; Singh, B.K.; Yen, P.M. Thyroid hormone regulation of hepatic lipid and carbohydrate metabolism. Trends Endocrinol. Metab. 2014, 25, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Klieverik, L.P.; Janssen, S.F.; van Riel, A.; Foppen, E.; Bisschop, P.H.; Serlie, M.J.; Boelen, A.; Ackermans, M.T.; Sauerwein, H.P.; Fliers, E.; et al. Thyroid hormone modulates glucose production via a sympathetic pathway from the hypothalamic paraventricular nucleus to the liver. Proc. Natl. Acad. Sci. USA 2009, 106, 5966–5971. [Google Scholar] [CrossRef]
- Gullberg, H.; Rudling, M.; Saltó, C.; Forrest, D.; Angelin, B.; Vennström, B. Requirement for thyroid hormone receptor beta in T3 regulation of cholesterol metabolism in mice. Mol. Endocrinol. 2002, 16, 1767–1777. [Google Scholar] [CrossRef] [PubMed]
- Mehran, L.; Amouzegar, A.; Rahimabad, P.K.; Tohidi, M.; Tahmasebinejad, Z.; Azizi, F. Thyroid Function and Metabolic Syndrome: A Population-Based Thyroid Study. Horm. Metab. Res. 2017, 49, 192–200. [Google Scholar] [CrossRef]
- Waring, A.C.; Rodondi, N.; Harrison, S.; Kanaya, A.M.; Simonsick, E.M.; Miljkovic, I.; Satterfield, S.; Newman, A.B.; Bauer, D.C.; Health, Ageing, and Body Composition (Health ABC) Study. Thyroid function and prevalent and incident metabolic syndrome in older adults: The Health, Ageing and Body Composition Study. Clin. Endocrinol. 2012, 76, 911–918. [Google Scholar] [CrossRef]
- Yang, L.; Lv, X.; Yue, F.; Wei, D.; Liu, W.; Zhang, T. Subclinical hypothyroidism and the risk of metabolic syndrome: A meta-analysis of observational studies. Endocr. Res. 2016, 41, 158–165. [Google Scholar] [CrossRef]
- Lu, Y.H.; Xia, Z.L.; Ma, Y.Y.; Chen, H.J.; Yan, L.P.; Xu, H.F. Subclinical hypothyroidism is associated with metabolic syndrome and clomiphene citrate resistance in women with polycystic ovary syndrome. Gynecol. Endocrinol. 2016, 32, 852–855. [Google Scholar] [CrossRef] [PubMed]
- Delitala, A.P.; Fanciulli, G.; Maioli, M.; Delitala, G. Subclinical hypothyroidism, lipid metabolism and cardiovascular disease. Endocr. Res. 2016, 41, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Floriani, C.; Gencer, B.; Collet, T.H.; Rodondi, N. Subclinical thyroid dysfunction and cardiovascular diseases: 2016 update. Eur. Heart J. 2018, 39, 503–507. [Google Scholar] [CrossRef] [PubMed]
- Tseng, F.Y.; Lin, W.Y.; Lin, C.C.; Lee, L.T.; Li, T.C.; Sung, P.K.; Huang, K.C. Subclinical hypothyroidism is associated with increased risk for all-cause and cardiovascular mortality in adults. J. Am. Coll. Cardiol. 2012, 60, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.M.; Pai, L.; Chu, N.F.; Sung, P.K.; Lee, M.S.; Tsai, J.T.; Hsu, L.L.; Lee, M.C.; Sun, C.A. Prevalence and clustering of cardiovascular risk factors among healthy adults in a Chinese population: The MJ Health Screening Center Study in Taiwan. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 1189–1195. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wen, C.P.; Cheng, T.Y.; Tsai, M.K.; Chang, Y.C.; Chan, H.T.; Tsai, S.P.; Chiang, P.H.; Hsu, C.C.; Sung, P.K.; Hsu, Y.H.; et al. All-cause mortality attributable to chronic kidney disease: A prospective cohort study based on 462 293 adults in Taiwan. Lancet 2008, 371, 2173–2182. [Google Scholar] [CrossRef]
- Ho-Pham, L.T.; Lai, T.Q.; Nguyen, M.T.; Nguyen, T.V. Relationship between Body Mass Index and Percent Body Fat in Vietnamese: Implications for the Diagnosis of Obesity. PLoS ONE 2015, 10, e0127198. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J. Metabolic syndrome—A new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef]
- Yin, J.; Li, M.; Xu, L.; Wang, Y.; Cheng, H.; Zhao, X.; Mi, J. Insulin resistance determined by Homeostasis Model Assessment (HOMA) and associations with metabolic syndrome among Chinese children and teenagers. Diabetol. Metab. Syndr. 2013, 5, 71. [Google Scholar] [CrossRef]
- Song, D.K.; Hong, Y.S.; Sung, Y.A.; Lee, H. Insulin resistance according to β-cell function in women with polycystic ovary syndrome and normal glucose tolerance. PLoS ONE 2017, 12, e0178120. [Google Scholar] [CrossRef]
- Gaziano, J.M.; Hennekens, C.H.; O’Donnell, C.J.; Breslow, J.L.; Buring, J.E. Fasting triglycerides, high-density lipoprotein, and risk of myocardial infarction. Circulation 1997, 96, 2520–2525. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Wang, Y.; Shen, B. An elevated preoperative plasma fibrinogen level is associated with poor overall survival in Chinese gastric cancer patients. Cancer Epidemiol. 2016, 42, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Shih, S.; Huang, Y.T.; Yang, H.I. A multiple mediator approach to quantify the effects of ADH1B and ALDH2 genes on hepatocellular carcinoma risk. Genet. Epidemiol. 2018, 42, 394–404. [Google Scholar] [CrossRef] [PubMed]
- Roos, A.; Bakker, S.J.; Links, T.P.; Gans, R.O.; Wolffenbuttel, B.H. Thyroid function is associated with components of the metabolic syndrome in euthyroid subjects. J. Clin. Endocrinol. Metab. 2007, 92, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.; Wang, J.; Jiang, F.; Wang, B.; Chen, Y.; Li, M.; Liu, H.; Li, C.; Xue, H.; Li, N.; et al. The relationship between serum thyrotropin and components of metabolic syndrome. Endocr. J. 2011, 58, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.Y.; Sung, Y.A.; Lee, H.J. Elevated thyroid stimulating hormone levels are associated with metabolic syndrome in euthyroid young women. Korean J. Intern. Med. 2013, 28, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Shinkov, A.; Borissova, A.M.; Kovatcheva, R.; Atanassova, I.; Vlahov, J.; Dakovska, L. The prevalence of the metabolic syndrome increases through the quartiles of thyroid stimulating hormone in a population-based sample of euthyroid subjects. Arq. Bras. Endocrinol. Metabol. 2014, 58, 926–932. [Google Scholar] [CrossRef]
- De Pergola, G.; Ciampolillo, A.; Paolotti, S.; Trerotoli, P.; Giorgino, R. Free triiodothyronine and thyroid stimulating hormone are directly associated with waist circumference, independently of insulin resistance, metabolic parameters and blood pressure in overweight and obese women. Clin. Endocrinol. (Oxf) 2007, 67, 265–269. [Google Scholar] [CrossRef]
- Ruhla, S.; Weickert, M.O.; Arafat, A.M.; Osterhoff, M.; Isken, F.; Spranger, J.; Schöfl, C.; Pfeiffer, A.F.; Möhlig, M. A high normal TSH is associated with the metabolic syndrome. Clin. Endocrinol. (Oxf) 2010, 72, 696–701. [Google Scholar] [CrossRef]
- De Jesus Garduño-Garcia, J.; Alvirde-Garcia, U.; López-Carrasco, G.; Padilla Mendoza, M.E.; Mehta, R.; Arellano-Campos, O.; Choza, R.; Sauque, L.; Garay-Sevilla, M.E.; Malacara, J.M. TSH and free thyroxine concentrations are associated with differing metabolic markers in euthyroid subjects. Eur. J. Endocrinol. 2010, 163, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Mehran, L.; Amouzegar, A.; Tohidi, M.; Moayedi, M.; Azizi, F. Serum free thyroxine concentration is associated with metabolic syndrome in euthyroid subjects. Thyroid 2014, 24, 1566–1574. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, L.; Zhou, L.; Song, Y.; Ma, S.; Yu, C.; Zhao, J.; Xu, C.; Gao, L. Thyroid stimulating hormone increases hepatic gluconeogenesis via CRTC2. Mol. Cell Endocrinol. 2017, 446, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Jornayvaz, F.R.; Lee, H.Y.; Jurczak, M.J.; Alves, T.C.; Guebre-Egziabher, F.; Guigni, B.A.; Zhang, D.; Samuel, V.T.; Silva, J.E.; Shulman, G.I. Thyroid hormone receptor-α gene knockout mice are protected from diet-induced hepatic insulin resistance. Endocrinology 2012, 153, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Asvold, B.O.; Bjøro, T.; Vatten, L.J. Associations of TSH levels within the reference range with future blood pressure and lipid concentrations: 11-year follow-up of the HUNT study. Eur. J. Endocrinol. 2013, 169, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Tan, Y.; Wang, C.; Zhang, X.; Zhao, Y.; Song, X.; Zhang, B.; Guan, Q.; Xu, J.; Zhang, J.; et al. Thyroid-stimulating hormone levels within the reference range are associated with serum lipid profiles independent of thyroid hormones. J. Clin. Endocrinol. Metab. 2012, 97, 2724–2731. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.K.; Kim, J.E.; Oh, H.J.; Park, K.S.; Kim, S.K.; Park, S.W.; Kim, M.J.; Cho, Y.W. Serum TSH level in healthy Koreans and the association of TSH with serum lipid concentration and metabolic syndrome. Korean J. Intern. Med. 2011, 26, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Asvold, B.O.; Bjøro, T.; Nilsen, T.I.; Vatten, L.J. Association between blood pressure and serum thyroid-stimulating hormone concentration within the reference range: A population-based study. J. Clin. Endocrinol. Metab. 2007, 92, 841–845. [Google Scholar] [CrossRef] [PubMed]
- Peixoto de Miranda, É.J.F.; Bittencourt, M.S.; Santos, I.S.; Lotufo, P.A.; Benseñor, I.M. Thyroid Function and High-Sensitivity C-Reactive Protein in Cross-Sectional Results from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil): Effect of Adiposity and Insulin Resistance. Eur. Thyroid J. 2016, 5, 240–246. [Google Scholar] [CrossRef][Green Version]
- Tuzcu, A.; Bahceci, M.; Gokalp, D.; Tuzun, Y.; Gunes, K. Subclinical hypothyroidism may be associated with elevated high-sensitive c-reactive protein (low grade inflammation) and fasting hyperinsulinemia. Endocr. J. 2005, 52, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Chadarevian, R.; Bruckert, E.; Giral, P.; Turpin, G. Relationship between thyroid hormones and fibrinogen levels. Blood Coagul. Fibrinolysis. 1999, 10, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Dörr, M.; Robinson, D.M.; Wallaschofski, H.; Schwahn, C.; John, U.; Felix, S.B.; Völzke, H. Low serum thyrotropin is associated with high plasma fibrinogen. J. Clin. Endocrinol. Metab. 2006, 91, 530–534. [Google Scholar] [CrossRef] [PubMed]
- Park, S.B.; Choi, H.C.; Joo, N.S. The relation of thyroid function to components of the metabolic syndrome in Korean men and women. J. Korean Med. Sci. 2011, 26, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Bae, J.C.; Park, H.K.; Byun, D.W.; Suh, K.; Yoo, M.H.; Kim, J.H.; Min, Y.K.; Kim, S.W.; Chung, J.H. Triiodothyronine Levels Are Independently Associated with Metabolic Syndrome in Euthyroid Middle-Aged Subjects. Endocrinol. Metab. (Seoul) 2016, 31, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Alevizaki, M.; Saltiki, K.; Voidonikola, P.; Mantzou, E.; Papamichael, C.; Stamatelopoulos, K. Free thyroxine is an independent predictor of subcutaneous fat in euthyroid individuals. Eur. J. Endocrinol. 2009, 161, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.J.; Kim, T.Y.; Koh, J.M.; Kim, H.K.; Park, J.Y.; Lee, K.U.; Shong, Y.K.; Kim, W.B. Relationship between serum free T4 (FT4) levels and metabolic syndrome (MS) and its components in healthy euthyroid subjects. Clin. Endocrinol. (Oxf) 2009, 70, 152–160. [Google Scholar] [CrossRef]
- Roef, G.; Lapauw, B.; Goemaere, S.; Zmierczak, H.G.; Toye, K.; Kaufman, J.M.; Taes, Y. Body composition and metabolic parameters are associated with variation in thyroid hormone levels among euthyroid young men. Eur. J. Endocrinol. 2012, 167, 719–726. [Google Scholar] [CrossRef]
| Characteristics | Mean (SD) |
|---|---|
| Male (number, %) | 11,811 (47.69) |
| Age (years) | 44.43 (12.41) |
| High-sensitive thyroid stimulating hormone (hsTSH) (mIU/L) | 1.74 (1.08) |
| Free T4 (µU/mL) | 1.06 (0.13) |
| Body mass index (kg/m2) | 23.77 (3.97) |
| Body fat (%) | 27.55 (7.31) |
| Waist circumference (cm) | 78.57 (10.95) |
| Systolic blood pressure (mmHg) | 115.64 (17.80) |
| Diastolic blood pressure (mmHg) | 73.86 (11.21) |
| Fasting glucose (mg/dL) | 104.69 (23.30) |
| Hemoglobin A1c (%) | 5.34 (0.78) |
| Fasting Insulin (mIU/L) | 7.94 (6.61) |
| Homeostasis model assessment of insulin resistance (HOMA-IR) (mU/L·mM) | 2.13 (2.29) |
| Homeostasis model assessment of beta-cell (HOMA-β) (mU/L/mM) | 72.44 (51.91) |
| Triglycerides (mg/dL) | 118.23 (105.00) |
| Total cholesterol (mg/dL) | 199.06 (36.46) |
| High-density lipoprotein cholesterol (mg/dL) | 58.57 (15.11) |
| Low-density lipoprotein cholesterol (mg/dL) | 117.95 (33.55) |
| Triglycerides/High-density lipoprotein cholesterol ratio | 2.33 (3.27) |
| High-sensitive C-reactive protein (mg/L) | 1.97 (4.38) |
| Fibrinogen (mg/dL) | 289.64 (56.42) |
| Uric acid (mg/dL) | 5.68 (1.54) |
| Alcohol consumption (number, %) | 4151 (17.39) |
| Cigarette smoking (number, %) | 4004 (16.75) |
| Physical inactivity (number, %) | 15,538 (65.77) |
| History of diabetes mellitus (number, %) | 1017 (4.11) |
| History of hypertension (number, %) | 2736 (11.07) |
| History of dyslipidemia (number, %) | 769 (3.11) |
| History of cardiovascular diseases (number, %) | 1211 (4.9) |
| Characteristic | hsTSH Level (mIU/L) | Crude p Value for Trend | Adjusted p Value for Trend * | |||||
|---|---|---|---|---|---|---|---|---|
| <50th Percentile 0.47–1.48 | 50–60th Percentile 1.49–1.68 | 60–70 thPercentile 1.69–1.94 | 70–80th Percentile 1.95–2.3 | 80–90th Percentile 2.31–2.93 | >90th Percentile >2.93 | |||
| Number | 12,004 | 2676 | 2510 | 2646 | 2506 | 2423 | - | - |
| Male (number, %) | 6161 (51.32) | 1320 (49.33) | 1203 (47.93) | 1216 (45.96) | 1025 (40.90) | 886 (36.57) | <0.0001 | - |
| Age (year) | 44.05 (12.07) | 44.34 (12.42) | 44.96 (12.3) | 44.61 (12.68) | 44.97 (12.72) | 45.09 (13.43) | <0.0001 | - |
| Free T4 (ng/dL) | 1.068 (0.134) | 1.063 (0.118) | 1.058 (0.114) | 1.056 (0.1165) | 1.0522 (0.119) | 1.0365 (0.121) | <0.0001 | <0.0001 |
| BMI (kg/m2) | 23.60 (3.78) | 23.88 (4.08) | 23.88 (3.96) | 24 (4.16) | 23.89 (4.18) | 24.02 (4.24) | <0.0001 | <0.0001 |
| Body fat (%) | <0.0001 | <0.0001 | ||||||
| Man | 24.38 (5.82) | 24.74 (6.19) | 25.02 (5.98) | 25.06 (6.37) | 25.13 (6.19) | 25.01 (6.47) | ||
| Women | 29.59 (7.07) | 30.30 (7.63) | 30.08 (7.11) | 30.56 (7.53) | 30.96 (7.76) | 31.33 (7.85) | ||
| Waist circumference (cm) | 0.46 | <0.0001 | ||||||
| Men | 84.40 (9.07) | 85.02 (9.58) | 85.54 (9.50) | 85.59 (10.03) | 86.01 (9.80) | 85.95 (10.33) | ||
| Woman | 72.17 (8.43) | 72.63 (8.68) | 72.60 (8.52) | 73.15 (8.73) | 73.32 (8.86) | 73.97 (9.74) | ||
| Systolic blood pressure (mmHg) | 115.1 (17.34) | 116.4 (18.04) | 115.7 (17.57) | 116.14 (18.27) | 115.95 (18.34) | 116.35 (18.77) | 0.0383 | <0.0001 |
| Diastolic blood pressure (mmHg) | 73.76 (11.08) | 74.10 (11.35) | 73.89 (11.14) | 74.03 (11.44) | 73.7 (11.19) | 74.02 (11.5) | 0.88 | <0.0001 |
| Fasting glucose (mg/dL) | 104.78 (23.19) | 104.69 (22.24) | 104.6 (21.77) | 104.48 (23.78) | 104.51 (24) | 104.74 (25.19) | 0.78 | 0.24 |
| HbA1c (%) | 5.33 (0.77) | 5.33 (0.75) | 5.33 (0.75) | 5.35 (0.77) | 5.36 (0.81) | 5.36 (0.81) | 0.034 | 0.0002 |
| Fasting Insulin (mIU/L) | 7.78 (7.02) | 7.98 (5.84) | 8.01 (5.43) | 7.99 (5.26) | 8.14 (5.86) | 8.39 (8.29) | 0.0002 | <0.0001 |
| HOMA-IR (mU/L·mM ) | 2.09 (2.50) | 2.13 (1.78) | 2.15 (1.82) | 2.14 (1.89) | 2.18 (2.02) | 2.27 (2.73) | 0.0015 | <0.0001 |
| HOMA-β(mU/L/mM ) | 70.58 (54.02) | 72.99 (54.39) | 72.74 (41.95) | 73.42 (42.39) | 74.93 (47.05) | 77.12 (60.83) | <0.0001 | <0.0001 |
| TG (mg/dL) | 113.67 (95.68) | 117.25 (93.75) | 122.97 (111.16) | 121.91 (147.42) | 124.42 (103.92) | 126.59 (98.4) | <0.0001 | <0.0001 |
| Total cholesterol (mg/dL) | 197.44 (35.66) | 199.81 (37.65) | 199.6 (35.04) | 199.32 (37.71) | 202.27 (37.84) | 202.1 (37.19) | <0.0001 | <0.0001 |
| HDL-C (mg/dL) | 58.54 (15.24) | 58.67 (14.81) | 58.09 (15) | 57.92 (14.48) | 59.16 (15.42) | 59.2 (15.23) | 0.031 | <0.0001 |
| LDL-C (mg/dL) | 117.03 (33.25) | 118.72 (33.92) | 118.33 (32.96) | 118.49 (34.51) | 119.6 (33.96) | 118.96 (33.68) | 0.0088 | <0.0001 |
| TG/HDL-C | 2.24 (3.06) | 2.28 (2.34) | 2.45 (3.01) | 2.45 (5.53) | 2.42 (2.66) | 2.47 (2.57) | 0.0008 | <0.0001 |
| hs-CRP (mg/L) | 1.94 (4.95) | 1.93 (3.82) | 2.01 (4.06) | 2.05 (3.95) | 1.95 (3.14) | 2.08 (3.7) | 0.1850 | 0.0883 |
| Fibrinogen (mg/dL) | 287.67 (56.23) | 289.8 (56.54) | 289.84 (56.89) | 291.94 (55.99) | 292.8 (56.71) | 293.24 (56.57) | <0.0001 | 0.0188 |
| Uric acid (mg/dL) | 5.67 (1.52) | 5.71 (1.57) | 5.71 (1.56) | 5.73 (1.58) | 5.65 (1.53) | 5.68 (1.57) | 0.6316 | <0.0001 |
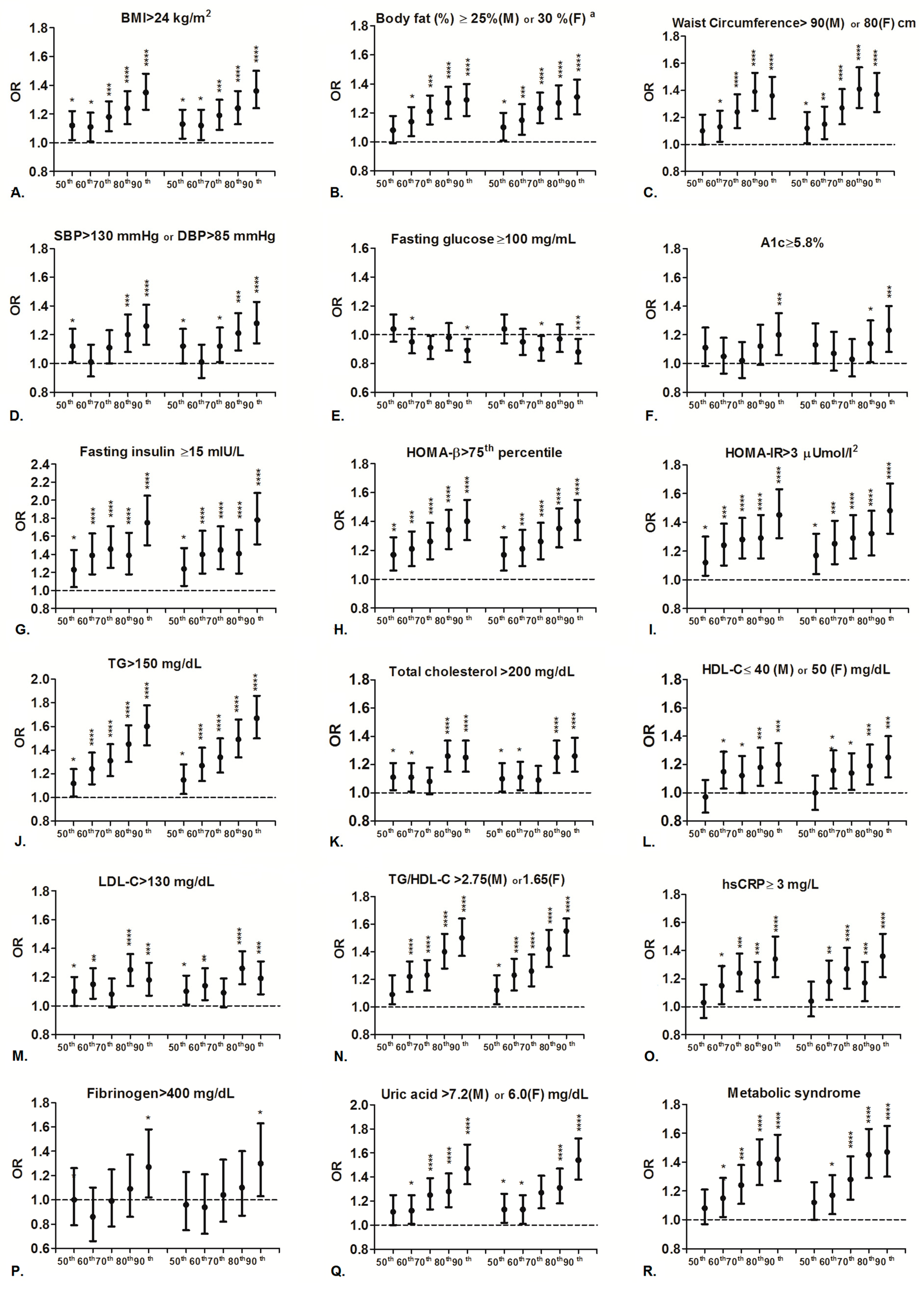
| Multinomial Logistic Regression | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | hsTSH Level (mIU/L) | |||||||||
| 1.49–1.68 vs. 0.47–1.48 | 1.69–1.94 vs. 0.47–1.48 | 1.95–2.3 vs. 0.47–1.48 | 2.31–2.93 vs. 0.47–1.48 | >2.93 vs. 0.47–1.48 | ||||||
| adjOR (95% CI) | p Value | adjOR (95% CI) | p Value | adjOR (95% CI) | p Value | adjOR (95% CI) | p Value | adjOR (95% CI) | p Value | |
| BMI > 24 kg/m2 | 1.13 (1.03, 1.23) | 0.01 | 1.12 (1.02, 1.23) | 0.02 | 1.19 (1.09, 1.30) | 0.0002 | 1.24 (1.13, 1.36) | <0.0001 | 1.36 (1.24, 1.50) | <0.0001 |
| Body fat (%): ≤30 years: male ≥20%; female ≥25% >30 years: male ≥25%; female ≥30% | 1.10 (1.01, 1.20) | 0.03 | 1.15 (1.05, 1.26) | 0.0022 | 1.23 (1.13, 1.34) | <0.0001 | 1.27 (1.16, 1.39) | <0.0001 | 1.31 (1.19, 1.43) | <0.0001 |
| Waist circumference: Men > 90 cm; women > 80 cm | 1.12 (1.01, 1.24) | 0.03 | 1.15 (1.04, 1.28) | 0.0082 | 1.27 (1.15, 1.41) | <0.0001 | 1.41 (1.27, 1.57) | <0.0001 | 1.37 (1.24, 1.53) | <0.0001 |
| Systolic blood pressure > 130 mmHg or Diastolic blood pressure > 85 mmHg | 1.12 (1.00, 1.24) | 0.04 | 1.01 (0.90, 1.13) | 0.86 | 1.12 (1.01, 1.25) | 0.03 | 1.21 (1.09, 1.35) | 0.0006 | 1.28 (1.14, 1.43) | <0.0001 |
| Fasting glucose ≥ 100 mg/dL | 1.04 (0.94, 1.14) | 0.45 | 0.95 (0.86, 1.04) | 0.26 | 0.90 (0.82, 0.99) | 0.03 | 0.97 (0.88, 1.07) | 0.54 | 0.88 (0.80, 0.97) | 0.0091 |
| HbA1c ≥ 5.8 % | 1.13 (1.00, 1.28) | 0.05 | 1.07 (0.95, 1.22) | 0.28 | 1.03 (0.91, 1.17) | 0.68 | 1.14 (1.01, 1.30) | 0.04 | 1.23 (1.08, 1.40) | 0.0015 |
| Fasting insulin ≥ 15 mIU/L | 1.24 (1.05, 1.47) | 0.01 | 1.40 (1.19, 1.66) | <0.0001 | 1.45 (1.24, 1.71) | <0.0001 | 1.41 (1.19, 1.67) | <0.0001 | 1.78 (1.51, 2.08) | <0.0001 |
| HOMA-β > 75th percentile | 1.17 (1.06, 1.29) | 0.0022 | 1.21 (1.09, 1.34) | 0.0003 | 1.26 (1.14, 1.39) | <0.0001 | 1.35 (1.22, 1.49) | <0.0001 | 1.40 (1.27, 1.55) | <0.0001 |
| HOMA-IR > 3.0 (mU/L·mM) | 1.17 (1.04, 1.32) | 0.0082 | 1.25 (1.11, 1.41) | 0.0002 | 1.29 (1.15, 1.45) | <0.0001 | 1.32 (1.17, 1.48) | <0.0001 | 1.48 (1.32, 1.67) | <0.0001 |
| TG ≥ 150 mg/dL | 1.15 (1.03, 1.28) | 0.01 | 1.27 (1.14, 1.42) | <0.0001 | 1.34 (1.21, 1.50) | <0.0001 | 1.49 (1.34, 1.66) | <0.0001 | 1.67 (1.50, 1.86) | <0.0001 |
| Total Cholesterol > 200 mg/dL | 1.10 (1.01, 1.21) | 0.03 | 1.11 (1.02, 1.22) | 0.02 | 1.09 (1.00, 1.19) | 0.06 | 1.25 (1.14, 1.37) | <0.0001 | 1.26 (1.15, 1.39) | <0.0001 |
| HDL-C: men ≤ 40 or women ≤ 50 mg/dL | 1.00 (0.88, 1.12) | 0.96 | 1.16 (1.03, 1.30) | 0.01 | 1.14 (1.02, 1.28) | 0.02 | 1.19 (1.06, 1.34) | 0.0037 | 1.25 (1.11, 1.40) | 0.0002 |
| LDL-C ≥ 130 mg/dL | 1.10 (1.01, 1.21) | 0.04 | 1.14 (1.04, 1.26) | 0.0051 | 1.09 (0.99, 1.19) | 0.08 | 1.26 (1.15, 1.38) | <0.0001 | 1.19 (1.08, 1.31) | 0.0005 |
| TG/HDL-C: men > 2.75 or women > 1.65 | 1.12 (1.02, 1.23) | 0.01 | 1.23 (1.12, 1.35) | <0.0001 | 1.26 (1.15, 1.38) | <0.0001 | 1.42 (1.29, 1.56) | <0.0001 | 1.55 (1.41, 1.70) | <0.0001 |
| hs-CRP ≥ 3 mg/dL | 1.04 (0.93, 1.18) | 0.49 | 1.18 (1.05, 1.33) | 0.0057 | 1.27 (1.13, 1.42) | <0.0001 | 1.17 (1.04, 1.32) | 0.0087 | 1.36 (1.21, 1.52) | <0.0001 |
| Fibrinogen > 400 mg/dL | 0.96 (0.75, 1.23) | 0.75 | 0.94 (0.72, 1.21) | 0.61 | 1.04 (0.82, 1.33) | 0.73 | 1.10 (0.87, 1.40) | 0.43 | 1.30 (1.03, 1.63) | 0.02 |
| Uric acid: men > 7.2 or women > 6.0 mg/dL | 1.13 (1.02, 1.26) | 0.03 | 1.13 (1.01, 1.27) | 0.03 | 1.27 (1.14, 1.41) | <0.0001 | 1.31 (1.18, 1.47) | <0.0001 | 1.54 (1.38, 1.72) | <0.0001 |
| Metabolic syndrome | 1.12 (1.00, 1.26) | 0.05 | 1.17 (1.04, 1.31) | 0.01 | 1.28 (1.14, 1.44) | <0.0001 | 1.45 (1.29, 1.63) | <0.0001 | 1.47 (1.30, 1.65) | <0.0001 |
| History of diabetes mellitus | 1.07 (0.85, 1.34) | 0.54 | 1.01 (0.80, 1.27) | 0.93 | 1.05 (0.83,1.31) | 0.68 | 1.16 (0.93, 1.45) | 0.18 | 1.32 (1.05, 1.63) | 0.013 |
| History of hypertension | 1.15 (0.99, 1.32) | 0.056 | 1.11 (0.95, 1.28) | 0.16 | 1.03 (0.89, 1.20) | 0.68 | 1.19 (1.03, 1.38) | 0.018 | 1.08 (0.92, 256) | 0.35 |
| History of dyslipidemia | 1.14 (0.88, 1.45) | 0.32 | 1.21 (0.94, 1.55) | 0.12 | 1.30 (1.03, 1.65) | 0.03 | 1.03 (0.79, 1.35) | 0.81 | 1.17 (0.91, 1.52) | 0.23 |
| History of cardiovascular diseases | 1.21 (0.99, 1.47) | 0.05 | 1.02 (0.82, 1.25) | 0.88 | 0.96 (0.78, 1.19) | 0.72 | 1.28 (1.06, 1.56) | 0.012 | 1.18 (0.96, 1.45) | 0.11 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, Y.-C.; Hua, S.-C.; Chang, C.-H.; Kao, W.-Y.; Lee, H.-L.; Chuang, L.-M.; Huang, Y.-T.; Lai, M.-S. High TSH Level within Normal Range Is Associated with Obesity, Dyslipidemia, Hypertension, Inflammation, Hypercoagulability, and the Metabolic Syndrome: A Novel Cardiometabolic Marker. J. Clin. Med. 2019, 8, 817. https://doi.org/10.3390/jcm8060817
Chang Y-C, Hua S-C, Chang C-H, Kao W-Y, Lee H-L, Chuang L-M, Huang Y-T, Lai M-S. High TSH Level within Normal Range Is Associated with Obesity, Dyslipidemia, Hypertension, Inflammation, Hypercoagulability, and the Metabolic Syndrome: A Novel Cardiometabolic Marker. Journal of Clinical Medicine. 2019; 8(6):817. https://doi.org/10.3390/jcm8060817
Chicago/Turabian StyleChang, Yi-Cheng, Shih-Che Hua, Chia-Hsuin Chang, Wei-Yi Kao, Hsiao-Lin Lee, Lee-Ming Chuang, Yen-Tsung Huang, and Mei-Shu Lai. 2019. "High TSH Level within Normal Range Is Associated with Obesity, Dyslipidemia, Hypertension, Inflammation, Hypercoagulability, and the Metabolic Syndrome: A Novel Cardiometabolic Marker" Journal of Clinical Medicine 8, no. 6: 817. https://doi.org/10.3390/jcm8060817
APA StyleChang, Y.-C., Hua, S.-C., Chang, C.-H., Kao, W.-Y., Lee, H.-L., Chuang, L.-M., Huang, Y.-T., & Lai, M.-S. (2019). High TSH Level within Normal Range Is Associated with Obesity, Dyslipidemia, Hypertension, Inflammation, Hypercoagulability, and the Metabolic Syndrome: A Novel Cardiometabolic Marker. Journal of Clinical Medicine, 8(6), 817. https://doi.org/10.3390/jcm8060817





