Efficacy and Efficiency of Nutritional Support Teams
Abstract
1. Introduction
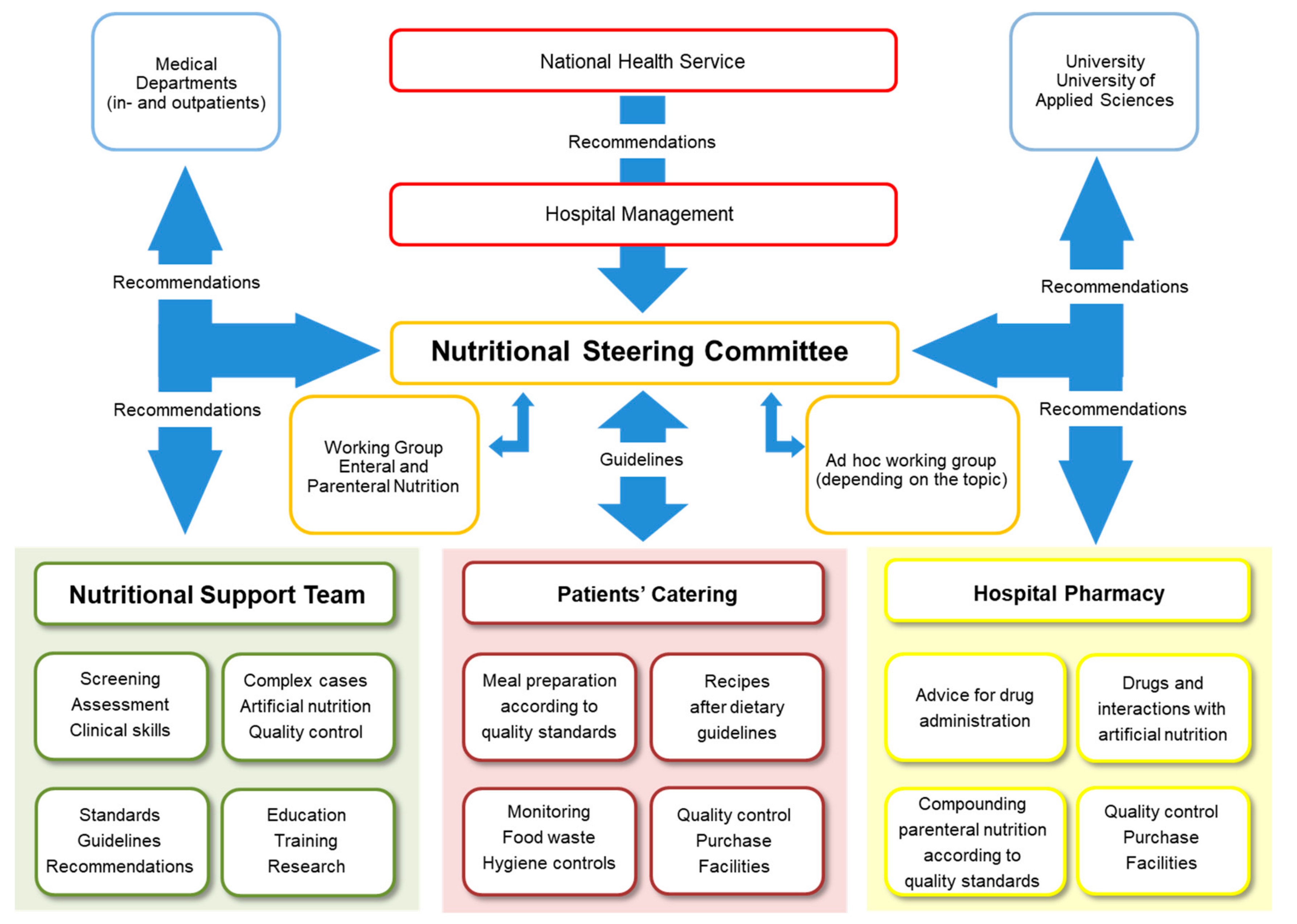
2. Development of NSTs
3. NST Composition and Collaboration
4. Tasks and Challenges of NSTs
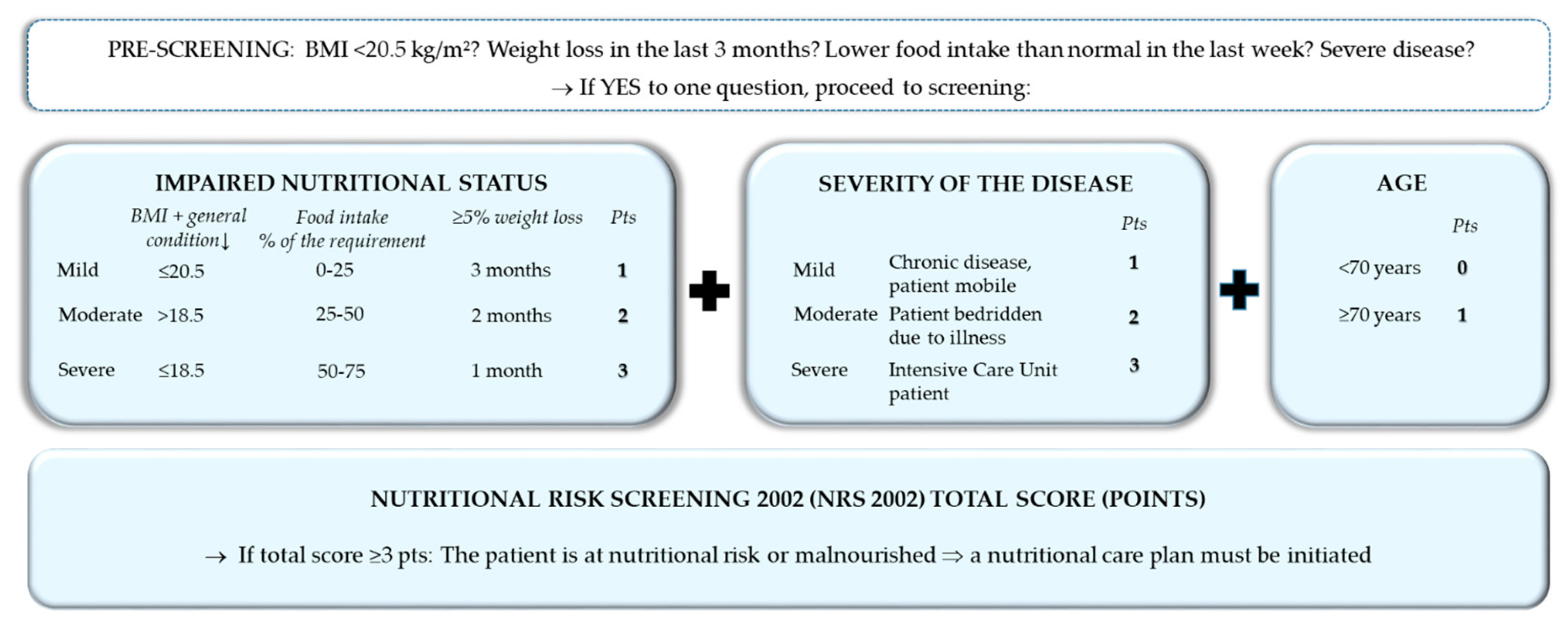
4.1. Screening and Assessment
4.2. Nutritional Therapy
4.3. Monitoring and Safety
4.4. Outpatient Management
4.5. Standards and Processes
4.6. Education, Training, and Research
5. Efficacy, Efficiency, and Positive Outcomes
6. Strength of Evidence Regarding Nutritional Support Teams
7. Conclusions and Outlook
Author Contributions
Funding
Conflicts of Interest
References
- Aeberhard, C.; Birrenbach, T.; Joray, M.; Muhlebach, S.; Perrig, M.; Stanga, Z. Simple training tool is insufficient for appropriate diagnosis and treatment of malnutrition: A pre-post intervention study in a tertiary center. Nutrition 2016, 32, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Felder, S.; Lechtenboehmer, C.; Bally, M.; Fehr, R.; Deiss, M.; Faessler, L.; Kutz, A.; Steiner, D.; Rast, A.C.; Laukemann, S.; et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition 2015, 31, 1385–1393. [Google Scholar] [CrossRef] [PubMed]
- McWhirter, J.P.; Pennington, C.R. Incidence and recognition of malnutrition in hospital. BMJ 1994, 308, 945–948. [Google Scholar] [CrossRef] [PubMed]
- Pirlich, M.; Schutz, T.; Norman, K.; Gastell, S.; Lubke, H.J.; Bischoff, S.C.; Bolder, U.; Frieling, T.; Güldenzoph, H.; Hahn, K.; et al. The German hospital malnutrition study. Clin. Nutr. 2006, 25, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, J.; Kondrup, J.; Prokopowicz, J.; Schiesser, M.; Krahenbuhl, L.; Meier, R.; Liberda, M. EuroOOPS: An international, multicentre study to implement nutritional risk screening and evaluate clinical outcome. Clin. Nutr. 2008, 27, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Rinninella, E.; Cintoni, M.; De Lorenzo, A.; Anselmi, G.; Gagliardi, L.; Addolorato, G.; Miggiano, G.A.; Gasbarrini, A.; Mele, M.C. May nutritional status worsen during hospital stay? A sub-group analysis from a cross-sectional study. Intern. Emerg. Med. 2019, 14, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Boitano, M.; Bojak, S.; McCloskey, S.; McCaul, D.S.; McDonough, M. Improving the safety and effectiveness of parenteral nutrition: Results of a quality improvement collaboration. Nutr. Clin. Pract. 2010, 25, 663–671. [Google Scholar] [CrossRef]
- ChrisAnderson, D.; Heimburger, D.C.; Morgan, S.L.; Geels, W.J.; Henry, K.L.; Conner, W.; Hensrud, D.D.; Thompson, G.; Weinsier, R.L. Metabolic complications of total parenteral nutrition: Effects of a nutrition support service. JPEN J. Parenter. Enteral. Nutr. 1996, 20, 206–210. [Google Scholar] [CrossRef]
- Curry, C.R.; Quie, P.G. Fungal septicemia in patients receiving parenteral hyperalimentation. N. Engl. J. Med. 1971, 285, 1221–1225. [Google Scholar] [CrossRef]
- Deutz, N.E.; Matheson, E.M.; Matarese, L.E.; Luo, M.; Baggs, G.E.; Nelson, J.L.; Hegazi, R.A.; Tappenden, K.A.; Ziegler, T.R. NOURISH Study Group. Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: A randomized clinical trial. Clin. Nutr. 2016, 35, 18–26. [Google Scholar] [CrossRef]
- Faubion, W.C.; Wesley, J.R.; Khalidi, N.; Silva, J. Total parenteral nutrition catheter sepsis: Impact of the team approach. JPEN J. Parenter. Enteral. Nutr. 1986, 10, 642–645. [Google Scholar] [CrossRef]
- Gariballa, S.; Forster, S.; Walters, S.; Powers, H. A randomized, double-blind, placebo-controlled trial of nutritional supplementation during acute illness. Am. J. Med. 2006, 119, 693–699. [Google Scholar] [CrossRef]
- Goldmann, D.A.; Maki, D.G. Infection control in total parenteral nutrition. JAMA 1973, 223, 1360–1364. [Google Scholar] [CrossRef]
- Ha, L.; Hauge, T.; Spenning, A.B.; Iversen, P.O. Individual, nutritional support prevents undernutrition, increases muscle strength and improves QoL among elderly at nutritional risk hospitalized for acute stroke: A randomized, controlled trial. Clin. Nutr. 2010, 29, 567–573. [Google Scholar] [CrossRef]
- Hegerova, P.; Dedkova, Z.; Sobotka, L. Early nutritional support and physiotherapy improved long-term self-sufficiency in acutely ill older patients. Nutrition 2015, 31, 166–170. [Google Scholar] [CrossRef]
- Hickson, M.; Bulpitt, C.; Nunes, M.; Peters, R.; Cooke, J.; Nicholl, C.; Frost, G. Does additional feeding support provided by health care assistants improve nutritional status and outcome in acutely ill older in-patients?—A randomised control trial. Clin. Nutr. 2004, 23, 69–77. [Google Scholar] [CrossRef]
- National Institute for Health and Clinical Excellence. Nutrition Support for Adults: Oral Nutrition Support, Enteral Tube Feeding and Parenteral Nutrition (clinical guideline 32). Available online: https://www.nice.org.uk/Guidance/CG32 (accessed on 20 August 2019).
- Jacobs, D.O.; Melnik, G.; Forlaw, L.; Gebhardt, C.; Settle, R.G.; DiSipio, M.; Rombeau, J.L. Impact of a nutritional support service on VA surgical patients. J. Am. Coll. Nutr. 1984, 3, 311–315. [Google Scholar] [CrossRef]
- Johansen, N.; Kondrup, J.; Plum, L.M.; Bak, L.; Norregaard, P.; Bunch, E.; Bærnthsen, H.; Andersen, J.R.; Larsen, I.H.; Martinsen, A. Effect of nutritional support on clinical outcome in patients at nutritional risk. Clin. Nutr. 2004, 23, 539–550. [Google Scholar] [CrossRef]
- Kennedy, J.F.; Nightingale, J.M. Cost savings of an adult hospital nutrition support team. Nutrition 2005, 21, 1127–1133. [Google Scholar] [CrossRef]
- Norman, K.; Kirchner, H.; Freudenreich, M.; Ockenga, J.; Lochs, H.; Pirlich, M. Three month intervention with protein and energy rich supplements improve muscle function and quality of life in malnourished patients with non-neoplastic gastrointestinal disease--a randomized controlled trial. Clin. Nutr. 2008, 27, 48–56. [Google Scholar] [CrossRef]
- Park, Y.E.; Park, S.J.; Park, Y.; Cheon, J.H.; Kim, T.I.; Kim, W.H. Impact and outcomes of nutritional support team intervention in patients with gastrointestinal disease in the intensive care unit. Medicine 2017, 96, e8776. [Google Scholar] [CrossRef]
- Piquet, M.A.; Bertrand, P.C.; Roulet, M. Role of a nutrition support team in reducing the inappropriate use of parenteral nutrition. Clin. Nutr. 2004, 23, 437, author reply 8. [Google Scholar] [CrossRef]
- Rufenacht, U.; Ruhlin, M.; Wegmann, M.; Imoberdorf, R.; Ballmer, P.E. Nutritional counseling improves quality of life and nutrient intake in hospitalized undernourished patients. Nutrition 2010, 26, 53–60. [Google Scholar] [CrossRef]
- Ryan, J.A., Jr.; Abel, R.M.; Abbott, W.M.; Hopkins, C.C.; Chesney, T.M.; Colley, R.; Phillips, K.; Fischer, J.E. Catheter complications in total parenteral nutrition: A prospective study of 200 consecutive patients. N. Engl. J. Med. 1974, 290, 757–761. [Google Scholar] [CrossRef]
- Sanders, R.A.; Sheldon, G.F. Septic complications of total parenteral nutrition: A five year experience. Am. J. Surg. 1976, 132, 214–220. [Google Scholar] [CrossRef]
- Somanchi, M.; Tao, X.; Mullin, G.E. The facilitated early enteral and dietary management effectiveness trial in hospitalized patients with malnutrition. JPEN J. Parenter. Enteral. Nutr. 2011, 35, 209–216. [Google Scholar] [CrossRef]
- Schuetz, P.; Fehr, R.; Baechli, V.; Geiser, M.; Gomes, F.; Kutz, A.; Tribolet, P.; Bregenzer, T.; Braun, N.; Hoess, C. Individualized nutritional support in medical inpatients at nutritional risk: A randomized clinical trial. Lancet 2019, 393, 2312–2321. [Google Scholar] [CrossRef]
- Sriram, K.; Cyriac, T.; Fogg, L.F. Effect of nutritional support team restructuring on the use of parenteral nutrition. Nutrition 2010, 26, 735–739. [Google Scholar] [CrossRef]
- Starke, J.; Schneider, H.; Alteheld, B.; Stehle, P.; Meier, R. Short-term individual nutritional care as part of routine clinical setting improves outcome and quality of life in malnourished medical patients. Clin. Nutr. 2011, 30, 194–201. [Google Scholar] [CrossRef]
- Stratton, R.J.; Green, C.J.; Elia, M. Disease-Related Malnutrition: An Evidence-Based Approach to Treatment; CABI Publishing: Wallingford, UK, 2003. [Google Scholar]
- Trujillo, E.B.; Young, L.S.; Chertow, G.M.; Randall, S.; Clemons, T.; Jacobs, D.O.; Robinson, M.K. Metabolic and monetary costs of avoidable parenteral nutrition use. JPEN J. Parenter. Enteral. Nutr. 1999, 23, 109–113. [Google Scholar] [CrossRef]
- Casaer, M.P.; Hermans, G.; Wilmer, A.; Van den Berghe, G. Impact of early parenteral nutrition completing enteral nutrition in adult critically ill patients (EPaNIC trial): A study protocol and statistical analysis plan for a randomized controlled trial. Trials 2011, 12, 21. [Google Scholar] [CrossRef]
- Kubrak, C.; Jensen, L. Malnutrition in acute care patients: A narrative review. Int. J. Nurs. Stud. 2007, 44, 1036–1054. [Google Scholar] [CrossRef]
- Villet, S.; Chiolero, R.L.; Bollmann, M.D.; Revelly, J.P.; Cayeux, R.N.M.; Delarue, J.; Berger, M.M. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin. Nutr. 2005, 24, 502–509. [Google Scholar] [CrossRef]
- Iff, S.; Leuenberger, M.; Rosch, S.; Knecht, G.; Tanner, B.; Stanga, Z. Meeting the nutritional requirements of hospitalized patients: An interdisciplinary approach to hospital catering. Clin. Nutr. 2008, 27, 800–805. [Google Scholar] [CrossRef]
- Allison, S.; Stanga, Z.G.; Odlund Olin, A. Organization of nutritional care. In Basics in Clinical Nutrition, 3rd ed.; Sobotka, L., Ed.; Galen: Prague, Czechia, 2011; pp. 135–139. [Google Scholar]
- Barton, A.D.; Beigg, C.L.; Macdonald, I.A.; Allison, S.P. High food wastage and low nutritional intakes in hospital patients. Clin. Nutr. 2000, 19, 445–449. [Google Scholar] [CrossRef]
- Dias-Ferreira, C.; Santos, T.; Oliveira, V. Hospital food waste and environmental and economic indicators—A Portuguese case study. Waste Manag. 2015, 46, 146–154. [Google Scholar] [CrossRef]
- Elia, M.; Parsons, E.L.; Cawood, A.L.; Smith, T.R.; Stratton, R.J. Cost-effectiveness of oral nutritional supplements in older malnourished care home residents. Clin. Nutr. 2018, 37, 651–658. [Google Scholar] [CrossRef]
- Norman, K.; Pirlich, M.; Smoliner, C.; Kilbert, A.; Schulzke, J.D.; Ockenga, J.; Lochs, H.; Reinhold, T. Cost-effectiveness of a 3-month intervention with oral nutritional supplements in disease-related malnutrition: A randomised controlled pilot study. Eur. J. Clin. Nutr. 2011, 65, 735–742. [Google Scholar] [CrossRef]
- Zhong, Y.; Cohen, J.T.; Goates, S.; Luo, M.; Nelson, J.; Neumann, P.J. The Cost-Effectiveness of Oral Nutrition Supplementation for Malnourished Older Hospital Patients. Appl. Health Econ. Health Policy 2017, 15, 75–83. [Google Scholar] [CrossRef]
- ten Dam, S.; Droop, A.; Arjaans, W.; de Groot, S.; van Bokhorst-de van der Schueren, M. Organisation of Nutritional Care Ethical and Legal Aspects. Module 11.1 Organisation of a nutritional support team, 2012. Available online: https://lllnutrition.com/mod/page/view.php?id=3422 (accessed on 20 August 2019).
- Ockenga, J.; Valentini, L. Organisationsstruktur der ernährungsmedizinischen Kompetenz, Ernährungsteams und Ernährungskommissionen. In Ernährungsmedizin, 5th ed.; Biesalski, H.K., Bischoff, S.C., Pirlich, M., Weimann, A., Eds.; Georg Thieme Verlag KG: Stuttgart, Germany, 2017; pp. 469–476. [Google Scholar]
- Dudrick, S.J.; Wilmore, D.W.; Vars, H.M.; Rhoads, J.E. Long-term total parenteral nutrition with growth, development, and positive nitrogen balance. Surgery 1968, 64, 134–142. [Google Scholar]
- Fürst, P.; Stehle, P. Künstliche Ernährung–gestern, heute, morgen. Transfus. Med. Hemother. 1990, 17, 237–244. [Google Scholar] [CrossRef]
- Butterworth, C.E. The skeleton in the hospital closet. 1974. Nutrition 1994, 10, 435–441. [Google Scholar]
- Shang, E.; Hasenberg, T.; Schlegel, B.; Sterchi, A.B.; Schindler, K.; Druml, W.; Koletzko, B.; Meier, R. An European survey of structure and organisation of nutrition support teams in Germany, Austria and Switzerland. Clin. Nutr. 2005, 24, 1005–1013. [Google Scholar] [CrossRef]
- Aubry, E.; Mareschal, J.; Gschweitl, M.; Zvingelis, M.; Schuetz, P.; Stanga, Z. Facts zum Management der Klinischen Ernährung—Eine Online-Befragung. Aktuel. Ernahrungsmed. 2018, 42, 452–460. [Google Scholar] [CrossRef]
- NutritionDay Worldwide 2018. Available online: https://www.nutritionday.org/en/about-nday/national-reports/index.html (accessed on 20 August 2019).
- Allison, S.P. Nutritional support—Who needs it and who does it? Clin. Nutr. 1992, 11, 165–166. [Google Scholar] [CrossRef]
- Allison, S. Hospital food as treatment. In A Report by a Working Party of BAPEN; BAPEN: Maidenhead, UK, 1999. [Google Scholar]
- Delegge, M.; Wooley, J.A.; Guenter, P.; Wright, S.; Brill, J.; Andris, D.; Wagner, P.; Filibeck, D. ASPEN Board of Directors. The state of nutrition support teams and update on current models for providing nutrition support therapy to patients. Nutr. Clin. Pract. 2010, 25, 76–84. [Google Scholar]
- Nightingale, J. Nutrition support teams: How they work, are set up and maintained. Frontline Gastroenterol. 2010, 1, 171–177. [Google Scholar] [CrossRef]
- Payne-James, J. Cost-effectiveness of nutrition support teams. Are they necessary? Nutrition 1997, 13, 928–930. [Google Scholar] [CrossRef]
- Suchner, U.; Dormann, A.; Hund-Wissner, E.; Shang, E.; Senkal, M. Anforderungen an Struktur und Funktion eines Ernährungsteams. Anaesthesist 2000, 49, 675–684. [Google Scholar] [CrossRef]
- Council of Europe, Committee of Ministers. Resolution ResAP (2003) on Food and Nutritional Care in Hospitals. 2004. Available online: https://search.coe.int/cm/Pages/result_details.aspx?ObjectID=09000016805de855 (accessed on 20 August 2019).
- Schneider, P.J. Nutrition support teams: An evidence-based practice. Nutr. Clin. Pract. 2006, 21, 62–67. [Google Scholar] [CrossRef]
- Reber, E.; Gomes, F.; Bally, L.; Schuetz, P.; Stanga, Z. Nutritional Management of Medical Inpatients. J. Clin. Med. 2019, 8, 1130. [Google Scholar] [CrossRef]
- Reber, E.; Gomes, F.; Vasiloglou, M.F.; Schuetz, P.; Stanga, Z. Nutritional Risk Screening and Assessment. J. Clin. Med. 2019, 8, 1065. [Google Scholar] [CrossRef]
- Kondrup, J.; Rasmussen, H.H.; Hamberg, O.; Stanga, Z. Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials. Clin. Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef]
- Soeters, P.B.; Reijven, P.L.; van Bokhorst-de van der Schueren, M.A.; Schols, J.M.; Halfens, R.J.; Meijers, J.M.; van Gemerta, W.G. A rational approach to nutritional assessment. Clin. Nutr. 2008, 27, 706–716. [Google Scholar] [CrossRef]
- Barbosa-Silva, M.C. Subjective and objective nutritional assessment methods: What do they really assess? Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 248–254. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Keller, U. Nutritional Laboratory Markers in Malnutrition. J. Clin. Med. 2019, 8, 775. [Google Scholar] [CrossRef]
- Leuenberger, M.; Nuoffer, J.-M.; Stanga, Z. Sinnvolle laborchemische Diagnostik in der Mangelernährung. Pipette 2007, 2, 15–19. [Google Scholar]
- Allison, S.P. Malnutrition, disease, and outcome. Nutrition 2000, 16, 590–593. [Google Scholar] [CrossRef]
- Kondrup, J.; Bak, L.; Hansen, B.S.; Ipsen, B.; Ronneby, H. Outcome from nutritional support using hospital food. Nutrition 1998, 14, 319–321. [Google Scholar] [CrossRef]
- Valentini, L.; Jadma, K. Zehn Jahre Ernährungsteam in Österreich: Definitionen, Aufgaben und Perspektiven. J. Ernärhrungsmed. 2004, 6, 17–23. [Google Scholar]
- Laesser, C.; Cumming, P.; Reber, E.; Stanga, Z.; Muka, T.; Bally, L. Management of Glucose Control in Noncritically Ill, Hospitalized Patients Receiving Parenteral and/or Enteral Nutrition: A Systematic Review. JCM 2019, 8, 935. [Google Scholar] [CrossRef]
- Burch, N.E.; Stewart, J.; Smith, N. Are nutrition support teams useful? Results from the NCEPOD study into parenteral nutrition. Gut 2011, 60 (Suppl. 1), A2. [Google Scholar] [CrossRef][Green Version]
- Rasmussen, N.M.L.; Belqaid, K.; Lugnet, K.; Nielsen, A.L.; Rasmussen, H.H.; Beck, A.M. Effectiveness of multidisciplinary nutritional support in older hospitalised patients: A systematic review and meta-analyses. Clin. Nutr. ESPEN 2018, 27, 44–52. [Google Scholar] [CrossRef]
- Riley, K.; Sulo, S.; Dabbous, F.; Partridge, J.; Kozmic, S.; Landow, W.; VanDerBosch, G.; Falson, M.K.; Sriram, K. Reducing Hospitalizations and Costs: A Home Health Nutrition-Focused Quality Improvement Program. JPEN J. Parenter. Enteral. Nutr. 2019. [Google Scholar] [CrossRef]
- Valentini, L.; Volkert, D.; Schütz, T.; Ockenga, J.; Pirlich, M.; Druml, W.; Schindler, K.; Ballmer, P.E.; Bischoff, S.C.; Weimann, A.; et al. Leitlinie der Deutschen Gesellschaft für Ernährungsmedizin (DGEM). Aktuelle Ernährungsmedizin 2013, 38, 97–111. [Google Scholar] [CrossRef]
- Bounoure, L.; Gomes, F.; Stanga, Z.; Keller, U.; Meier, R.; Ballmer, P.; Fehr, R.; Mueller, B.; Genton, L.; Bertrand, P.C.; et al. Detection and treatment of medical inpatients with or at-risk of malnutrition: Suggested procedures based on validated guidelines. Nutrition 2016, 32, 790–798. [Google Scholar] [CrossRef]
- Friedli, N.; Stanga, Z.; Sobotka, L.; Culkin, A.; Kondrup, J.; Laviano, A.; Mueller, B.; Schuetz, P. Revisiting the refeeding syndrome: Results of a systematic review. Nutrition 2017, 35, 151–160. [Google Scholar] [CrossRef]
- Friedli, N.; Stanga, Z.; Culkin, A.; Crook, M.; Laviano, A.; Sobotka, L.; Kressig, R.W.; Kondrup, J.; Mueller, B.; Schuetz, P. Management and prevention of refeeding syndrome in medical inpatients: An evidence-based and consensus-supported algorithm. Nutrition 2018, 47, 13–20. [Google Scholar] [CrossRef]
- Arends, J.; Baracos, V.; Bertz, H.; Bozzetti, F.; Calder, P.C.; Deutz, N.E.P.; Erickson, N.; Laviano, A.; Lisanti, M.P.; Lobo, D.N.; et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin. Nutr. 2017, 36, 1187–1196. [Google Scholar] [CrossRef]
- Fearon, K.; Strasser, F.; Anker, S.D.; Bosaeus, I.; Bruera, E.; Fainsinger, R.L.; Jatoi, A.; Loprinzi, C.; MacDonald, N.; Mantovani, G.; et al. Definition and classification of cancer cachexia: An international consensus. Lancet Oncol. 2011, 12, 489–495. [Google Scholar] [CrossRef]





| Professional Function | Nutritional Care Tasks |
|---|---|
| Nurse |
|
| Physician |
|
| Dietician |
|
| Pharmacist |
|
| Outcome | Correct Indication | Cost Savings | Decreased Complication Rates | Reduced Mortality | Improved Monitoring | Increased Dietary Intake | Positive Influence of Individualized Nutritional Support |
|---|---|---|---|---|---|---|---|
| Studies | Boitano et al. [7] Piquet et al. [23] Trujilo et al. [32] Sriram et al. [29] | Boitano et al. [7] ChrisAnderson et al. [8] Curry et al. [9] Faubion et al. [11] Goldmann et al. [13] Jacobs et al. [18] Kennedy et al. [20] Piquet et al. [23] Ryan et al. [25] Sanders et al. [26] Trujilo et al. [32] | Boitano et al. [7] Curry et al. [9] Faubion et al. [11] Gariballa et al. [12] Goldmann et al. [13] Ha et al. [14] Hegerova et al. [15] Hickson et al. [16] Jacobs et al. [18] Johansen et al. [19] Norman et al. [21,41] Piquet et al. [23] Ruefenacht et al. [24] Ryan et al. [25] Sanders et al. [26] Somanchi et al. [27] Schuetz et al. [28] Starke et al. [30] Stratton et al. [31] Trujilo et al. [32] ten Dam et al. [43] Dudrick et al. [45] Fürst et al. [46] Butterworth [47] Allison [51] Council of Europe [57] | Park et al. [22] Schuetz et al. [28] Deutz et al. [10] | Boitano et al. [7] Kennedy et al. [20] | Boitano et al. [7] Gariballa et al. [12] Ha et al. [14] Hegerova et al. [15] Hickson et al. [16] Johansen et al. [19] Norman et al. [21,41] Ruefenacht et al. [24] Somanchi et al. [27] Schuetz et al. [28] Starke et al. [30] Stratton et al. [31] ten Dam et al. [43] Dudrick et al. [45] Fürst et al. [46] Allison [51] Council of Europe [57] | Johansen et al. [19] Ruefenacht et al. [24] Schuetz et al. [28] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reber, E.; Strahm, R.; Bally, L.; Schuetz, P.; Stanga, Z. Efficacy and Efficiency of Nutritional Support Teams. J. Clin. Med. 2019, 8, 1281. https://doi.org/10.3390/jcm8091281
Reber E, Strahm R, Bally L, Schuetz P, Stanga Z. Efficacy and Efficiency of Nutritional Support Teams. Journal of Clinical Medicine. 2019; 8(9):1281. https://doi.org/10.3390/jcm8091281
Chicago/Turabian StyleReber, Emilie, Rachel Strahm, Lia Bally, Philipp Schuetz, and Zeno Stanga. 2019. "Efficacy and Efficiency of Nutritional Support Teams" Journal of Clinical Medicine 8, no. 9: 1281. https://doi.org/10.3390/jcm8091281
APA StyleReber, E., Strahm, R., Bally, L., Schuetz, P., & Stanga, Z. (2019). Efficacy and Efficiency of Nutritional Support Teams. Journal of Clinical Medicine, 8(9), 1281. https://doi.org/10.3390/jcm8091281





