Characteristics of Patients Showing Discrepancy Between Bruch’s Membrane Opening-Minimum Rim Width and Peripapillary Retinal Nerve Fiber Layer Thickness
Abstract
:1. Introduction
2. Experimental Section
2.1. Subjects
2.2. Optical Coherence Tomography
2.3. Confocal Scanning Laser Ophthalmoscopy and Perimetry
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
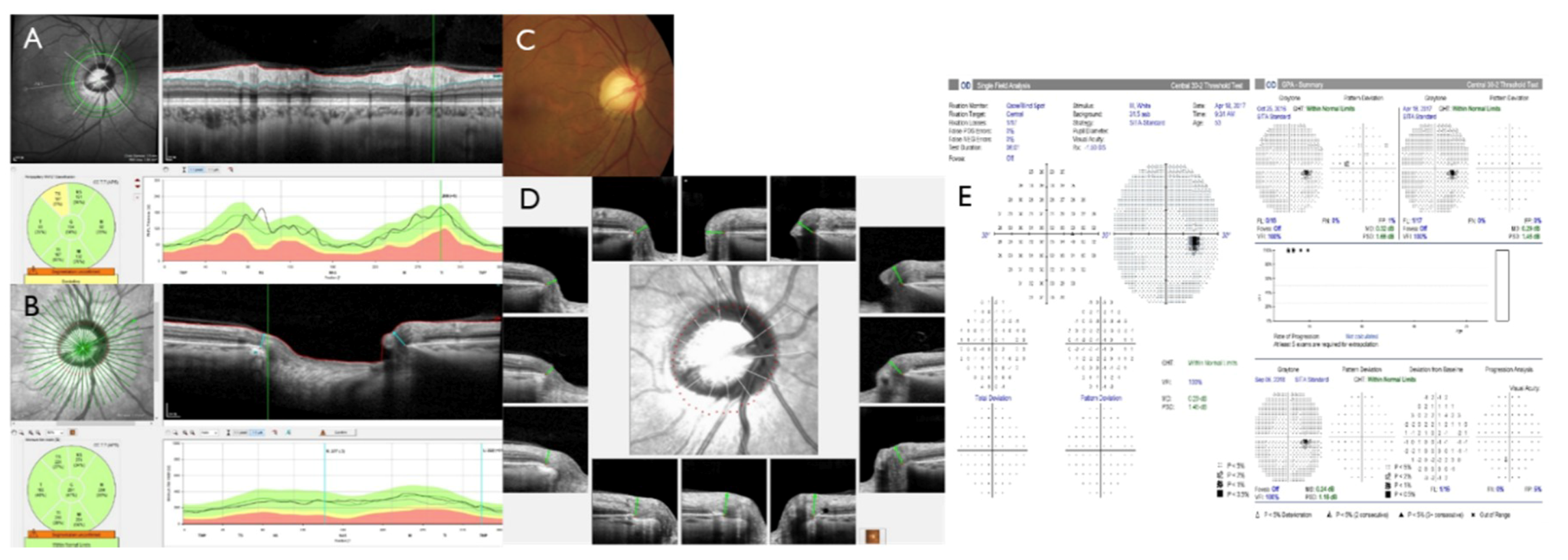
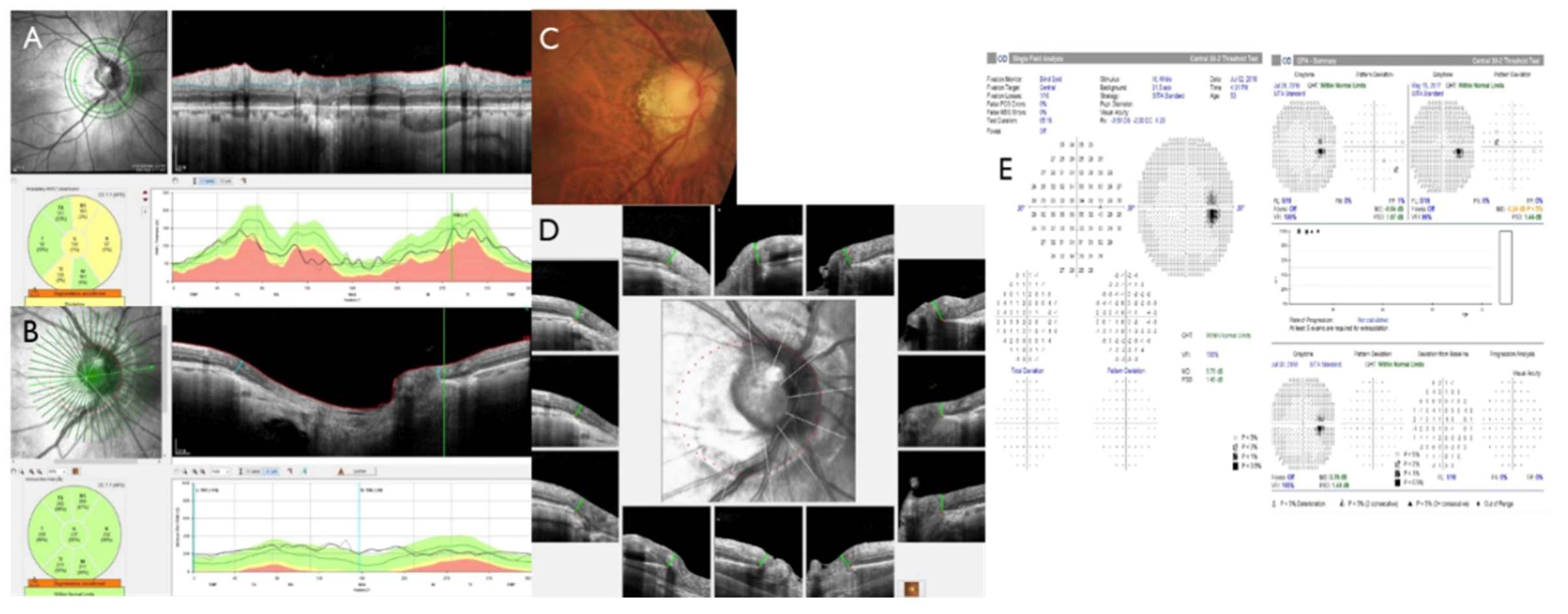
3.2. Retinal Nerve Fiber Layer and Bruch’s Membrane Opening Minimum Rim Width
3.3. Retinal Nerve Fiber Layer According to Optic Disc Size
3.4. Retinal Nerve Fiber Layer According to Myopia
3.5. Retinal Nerve Fiber Layer According to Visual Field Test Results
4. Discussion
Author Contributions
Conflicts of Interest
References
- Weinreb, R.N.; Khaw, P.T. Primary open-angle glaucoma. Lancet 2004, 363, 1711–1720. [Google Scholar] [CrossRef]
- AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am. J. Ophthalmol. 2000, 130, 429–440. [Google Scholar] [CrossRef]
- Kass, M.A.; Heuer, D.K.; Higginbotham, E.J.; Johnson, C.A.; Keltner, J.L.; Miller, J.P.; Parrish, R.K.; Wilson, M.R.; Gordon, M.O. The Ocular Hypertension Treatment Study: A randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch. Ophthalmol. 2002, 120, 701–713, discussion 829–830. [Google Scholar] [CrossRef] [PubMed]
- Malik, R.; Swanson, W.H.; Garway-Heath, D.F. ‘Structure-function relationship’ in glaucoma: Past thinking and current concepts. Clin. Exp. Ophthalmol. 2012, 40, 369–380. [Google Scholar] [CrossRef] [PubMed]
- Keltner, J.L.; Johnson, C.A.; Anderson, D.R.; Levine, R.A.; Fan, J.; Cello, K.E.; Quigley, H.A.; Budenz, D.L.; Parrish, R.K.; Kass, M.A. The Association between Glaucomatous Visual Fields and Optic Nerve Head Features in the Ocular Hypertension Treatment Study. Ophthalmology 2006, 113, 1603–1612. [Google Scholar] [CrossRef] [PubMed]
- Hood, D.C.; Kardon, R.H. A framework for comparing structural and functional measures of glaucomatous damage. Prog. Retin. Eye Res. 2007, 26, 688–710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chauhan, B.C.; Burgoyne, C.F. From clinical examination of the optic disc to clinical assessment of the optic nerve head: A paradigm change. Am. J. Ophthalmol. 2013, 156, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.C. Spectral domain optical coherence tomography in glaucoma: Qualitative and quantitative analysis of the optic nerve head and retinal nerve fiber layer (an AOS thesis). Trans. Am. Ophthalmol. Soc. 2009, 107, 254–281. [Google Scholar] [PubMed]
- Považay, B.; Hofer, B.; Hermann, B.M.; Unterhuber, A.; Morgan, J.E.; Glittenberg, C.; Binder, S.; Drexler, W. Minimum distance mapping using three-dimensional optical coherence tomography for glaucoma diagnosis. J. Biomed. Opt. 2007, 12, 041204. [Google Scholar] [CrossRef]
- Reis, A.S.C.; O’Leary, N.; Yang, H.; Sharpe, G.P.; Nicolela, M.T.; Burgoyne, C.F.; Chauhan, B.C. Influence of Clinically Invisible, but Optical Coherence Tomography Detected, Optic Disc Margin Anatomy on Neuroretinal Rim Evaluation. Investig. Opthalmol. Vis. Sci. 2012, 53, 1852–1860. [Google Scholar] [CrossRef] [Green Version]
- Strouthidis, N.G.; Fortune, B.; Yang, H.; Sigal, I.A.; Burgoyne, C.F. Longitudinal change detected by spectral domain optical coherence tomography in the optic nerve head and peripapillary retina in experimental glaucoma. Investig. Opthalmol. Vis. Sci. 2011, 52, 1206–1219. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, B.C.; Danthurebandara, V.M.; Sharpe, G.P.; Demirel, S.; Girkin, C.A.; Mardin, C.Y.; Scheuerle, A.F.; Burgoyne, C.F. Bruch’s Membrane Opening Minimum Rim Width and Retinal Nerve Fiber Layer Thickness in a Normal White Population: A Multicenter Study. Ophthalmology 2015, 122, 1786–1794. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, B.C.; O’Leary, N.; Almobarak, F.A.; Reis, A.S.; Yang, H.; Sharpe, G.P.; Hutchison, D.M.; Nicolela, M.T.; Burgoyne, C.F. Enhanced detection of open-angle glaucoma with an anatomically accurate optical coherence tomography-derived neuroretinal rim parameter. Ophthalmology 2013, 120, 535–543. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, K.; Gosho, M.; Zako, M. Correlation between optic nerve head structural parameters and glaucomatous visual field indices. Clin. Ophthalmol. 2014, 8, 1203–1208. [Google Scholar] [PubMed]
- Pollet-Villard, F.; Chiquet, C.; Romanet, J.P.; Noel, C.; Aptel, F. Structure-function relationships with spectral-domain optical coherence tomography retinal nerve fiber layer and optic nerve head measurements. Investig. Opthalmol. Vis. Sci. 2014, 55, 2953–2962. [Google Scholar] [CrossRef] [PubMed]
- Gardiner, S.K.; Ren, R.; Yang, H.; Fortune, B.; Burgoyne, C.F.; Demirel, S. A method to estimate the amount of neuroretinal rim tissue in glaucoma: Comparison with current methods for measuring rim area. Am. J. Ophthalmol. 2014, 157, 540–549. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.R. Automated Static Perimetry, 2nd ed.; Mosby–Year Book Inc.: Maryland Heights, MO, USA, 1999. [Google Scholar]
- Hoffmann, E.M.; Zangwill, L.M.; Crowston, J.G.; Weinreb, R.N. Optic disk size and glaucoma. Surv. Ophthalmol. 2007, 52, 32–49. [Google Scholar] [CrossRef] [PubMed]
- Okimoto, S.; Yamashita, K.; Shibata, T.; Kiuchi, Y. Morphological Features and Important Parameters of Large Optic Discs for Diagnosing Glaucoma. PLoS ONE 2015, 10, e0118920. [Google Scholar] [CrossRef]
- Jonas, J.B.; Schmidt, A.M.; Müller-Bergh, J.A.; Schlötzer-Schrehardt, U.M.; Naumann, G.O. Human optic nerve fiber count and optic disc size. Investig. Ophthalmol. Vis. Sci. 1992, 33, 2012–2018. [Google Scholar]
- Enders, P.; Schaub, F.; Hermann, M.M.; Cursiefen, C.; Heindl, L.M. Neuroretinal rim in non-glaucomatous large optic nerve heads: A comparison of confocal scanning laser tomography and spectral domain optical coherence tomography. Br. J. Ophthalmol. 2017, 101, 138–142. [Google Scholar] [CrossRef]
- Mitchell, P.; Hourihan, F.; Sandbach, J.; Wang, J.J. The relationship between glaucoma and myopia. Ophthalmology 1999, 106, 2010–2015. [Google Scholar] [CrossRef]
- Xu, L.; Wang, Y.; Wang, S.; Wang, Y.; Jonas, J.B. High myopia and glaucoma susceptibility: The Beijing eye study. Ophthalmology 2007, 114, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.K.; Kee, C. Population-based glaucoma prevalence studies in Asians. Surv. Ophthalmol. 2014, 59, 434–447. [Google Scholar] [CrossRef]
- Fechtner, R.D. Review of normative database construction in available OCT models highlighting differences. Presented at the FDA/American Glaucoma Society Workshop on the Validity, Reliability, and Usability of Glaucoma Imaging Devices, Silver Spring, MD, USA, 8 October 2012. [Google Scholar]
- Moraes, G.V. How does construction and statistical modeling within OCT normative databases compare with standard automated perimetry databases? Presented at the FDA/American Glaucoma Society Workshop on the Validity, Reliability, and Usability of Glaucoma Imaging Devices, Silver Spring, MD, USA, 8 October 2012. [Google Scholar]
- Melo, G.B.; Libera, R.D.; Barbosa, A.S.; Pereira, L.M.; Doi, L.M.; Melo, L.J. Comparison of optic disk and retinal nerve fiber layer thickness in nonglaucomatous and glaucomatous patients with high myopia. Am. J. Ophthalmol. 2006, 142, 858–860. [Google Scholar] [CrossRef] [PubMed]
- Huynh, S.C.; Wang, X.Y.; Rochtchina, E.; Mitchell, P. Peripapillary retinal nerve fiber layer thickness in a population of 6-year-old children: Findings by optical coherence tomography. Ophthalmology 2006, 113, 1583–1592. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Hong, S.W.; Im, S.K.; Lee, S.H.; Ahn, M.D. Effect of myopia on the thickness of the retinal nerve fiber layer measured by Cirrus HD optical coherence tomography. Investig. Opthalmol. Vis. Sci. 2010, 51, 4075–4083. [Google Scholar] [CrossRef] [PubMed]
- Savini, G.; Barboni, P.; Parisi, V.; Carbonelli, M. The influence of axial length on retinal nerve fibre layer thickness and optic disc size measurements by spectral-domain OCT. Br. J. Ophthalmol. 2012, 96, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Gmeiner, J.M.; Schrems, W.A.; Mardin, C.Y.; Laemmer, R.; Kruse, F.E.; Schrems-Hoesl, L.M. Comparison of Bruch’s membrane opening minimum rim width and peripapillary retinal nerve fiber layer thickness in early glaucoma assessment. Investig. Ophthalmol. Vis. Sci. 2016, 57, 575–584. [Google Scholar] [CrossRef]
- Malik, R.; Belliveau, A.C.; Sharpe, G.P.; Shuba, L.M.; Chauhan, B.C.; Nicolela, M.T. Diagnostic Accuracy of Optical Coherence Tomography and Scanning Laser Tomography for Identifying Glaucoma in Myopic Eyes. Ophthalmology 2016, 123, 1181–1189. [Google Scholar] [CrossRef]
- Zheng, F.; Yu, M.; Leung, C.K. Diagnostic criteria for detection of retinal nerve fibre layer thickness and neuroretinal rim width abnormalities in glaucoma. Br. J. Ophthalmol. 2019. [Google Scholar] [CrossRef]
- Toshev, A.P.; Lamparter, J.; Pfeiffer, N.; Hoffmann, E.M. Bruch’s Membrane Opening Minimum Rim Width Assessment with Spectral-Domain Optical Coherence Tomography Performs Better Than Confocal Scanning Laser Ophthalmoscopy in Discriminating Early Glaucoma Patients From Control Subjects. J. Glaucoma 2017, 26, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Enders, P.; Schaub, F.; Adler, W.; Hermann, M.M.; Dietlein, T.S.; Cursiefen, C.; Heindl, L.M. Bruch’s membrane opening-based optical coherence tomography of the optic nerve head: A useful diagnostic tool to detect glaucoma in macrodiscs. Eye (Lond.) 2018, 32, 314–323. [Google Scholar] [CrossRef] [PubMed]
- Lopes, F.S.; Matsubara, I.; Almeida, I.; Dorairaj, S.K.; Vessani, R.M.; Paranhos, A., Jr.; Prata, T.S. Structure-function relationships in glaucoma using enhanced depth imaging optical coherence tomography-derived parameters: A cross-sectional observational study. BMC Ophthalmol. 2019, 19, 52. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.B.; Gusek, G.C.; Naumann, G.O. Optic disc, cup and neuroretinal rim size, configuration and correlations in normal eyes. Investig. Ophthalmol. Vis. Sci. 1988, 29, 1151–1158. [Google Scholar]
- Lee, E.J.; Han, J.C.; Kee, C. Nasalised distribution of peripapillary retinal nerve fibre layers in large discs. Br. J. Ophthalmol. 2017, 101, 1643–1648. [Google Scholar] [CrossRef] [PubMed]
- Chong, G.T.; Lee, R.K. Glaucoma versus red disease: Imaging and glaucoma diagnosis. Curr. Opin. Ophthalmol. 2012, 23, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.R.; Lim, H.; Kim, J.H.; Rho, S.S.; Seong, G.J.; Kim, C.Y. Factors associated with false positives in retinal nerve fiber layer color codes from spectral-domain optical coherence tomography. Ophthalmology 2011, 118, 1774–1781. [Google Scholar] [CrossRef] [PubMed]
- Rauscher, F.M.; Sekhon, N.; Feuer, W.J.; Budenz, D.L. Myopia affects retinal nerve fiber layer measurements as determined by optical coherence tomography. J. Glaucoma 2009, 18, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Hwang, Y.H.; Yoo, C.; Kim, Y.Y. Characteristics of peripapillary retinal nerve fiber layer thickness in eyes with myopic optic disc tilt and rotation. J Glaucoma 2012, 21, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Rebolleda, G.; Casado, A.; Oblanca, N.; Muñoz-Negrete, F.J. The new Bruch’s membrane opening—Minimum rim width classification improves optical coherence tomography specificity in tilted discs. Clin. Ophthalmol. 2016, 10, 2417–2425. [Google Scholar] [CrossRef] [PubMed]
- Morales-Fernandez, L.; Saenz-Frances, F.; Garcia-Feijoo, J. Utility of Bruch membrane opening-based optic nerve head parameters in myopic subjects. Eur. J. Ophthalmol. 2018, 28, 42–46. [Google Scholar]
- Reznicek, L.; Burzer, S.; Laubichler, A.; Nasseri, A.; Lohmann, C.P.; Feucht, N.; Ulbig, M.; Maier, M. Structure-function relationship comparison between retinal nerve fibre layer and Bruch’s membrane opening-minimum rim width in glaucoma. Int. J. Ophthalmol. 2017, 10, 1534–1538. [Google Scholar] [PubMed]
- Sawada, A.; Tomidokoro, A.; Araie, M.; Iwase, A.; Yamamoto, T.; Tajimi Study Group. Refractive errors in an elderly Japanese population: The Tajimi study. Ophthalmology 2008, 115, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.Y.; Foster, P.J.; Hee, J.; Ng, T.P.; Tielsch, J.M.; Chew, S.J.; Johnson, G.J.; Seah, S.K. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Investig. Ophthalmol. Vis. Sci. 2000, 41, 2486–2494. [Google Scholar]
- Xu, L.; Li, Y.; Wang, S.; Wang, Y.; Wang, Y.; Jonas, J.B. Characteristics of highly myopic eyes: The Beijing Eye Study. Ophthalmology 2007, 114, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.; Tielsch, J.M.; Sommer, A. Prevalence and risk factors for refractive errors in an adult inner city population. Investig. Opthalmol. Vis. Sci. 1997, 38, 334–340. [Google Scholar]
- The Eye Diseases Prevalence Research Group. The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Arch. Ophthalmol. 2004, 122, 495–505. [Google Scholar] [CrossRef] [PubMed]
- Tarczy-Hornoch, K.; Ying-Lai, M.; Varma, R. Myopic refractive error in adult Latinos: The Los Angeles Latino Eye Study. Investig. Opthalmol. Vis. Sci. 2006, 47, 1845–1852. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Values |
|---|---|
| Number of subjects | 106 eyes (106 subjects) |
| Mean Age (year) | 52.79 ± 14.75 |
| Female gender (%) | 40 (37.7%) |
| Family history of glaucoma (%) | 11 (10.4%) |
| Spherical equivalent (D) | −2.52 ± 3.48 |
| <−6.0D | 26 eyes (24.5%) |
| <−5.0D | 34 eyes (32.1%) |
| CCT (um) | 551.19 ± 38.26 |
| Baseline IOP (mmHg) | 15.20 ± 3.17 |
| β-PPA (%) | 102 eyes (96.2%) |
| γ-PPA (%) | 80 eyes (75.5%) |
| VFI (%) | 96.72 ± 9.58 |
| MD (dB) | −1.74 ± 3.61 |
| PSD (dB) | 2.86 ± 1.89 |
| GHT | WNL: 72/101 eyes (71.3%) |
| BL: 15/101 eyes (14.9%) | |
| ONL: 14/101 eyes (13.8%) |
| Characteristics | Values |
|---|---|
| Disc area (mm2) | 2.35 ± 0.68 (1.63–2.43) |
| Large disc (>2.43 mm2) | 2.99 ± 0.51 (39/96 eyes, 40.6%) |
| Regular disc (1.63~2.43 mm2) | 2.06 ± 0.23 (45/96 eyes, 46.9%) |
| Small disc (<1.63 mm2) | 1.39 ± 0.22 (12/96 eyes, 12.5%) |
| Cup area (mm2) | 1.00 ± 0.65 (0.11–0.68) |
| Rim area (mm2) | 1.35 ± 0.32 (1.31–1.96) |
| Cup/disc area ratio | 0.39 ± 0.18 (0.07–0.30) |
| Rim/disc area ratio | 0.61 ± 0.18 (0.70–0.93) |
| Cup volume (mm3) | 0.28 ± 0.27 (0.01–0.18) |
| Rim volume (mm3) | 0.37 ± 0.15 (0.30–0.61) |
| Mean cup depth | 0.31 ± 0.11 (0.10–0.27) |
| Horizontal cup/disc ratio | 0.62 ± 0.22 |
| Vertical cup/disc ratio | 0.56 ± 0.20 |
| Characteristics | RNFL Thickness | RNFL Classification | Superior Peak Location | Inferior Peak Location | ||
|---|---|---|---|---|---|---|
| WNL | BL | ONL | ||||
| RNFL G (µm) | 93.07 ± 10.09 | 80 (75.5%) | 14 (13.2%) | 12 (11.3%) | 79.29 ± 15.04 | 297.67 ± 15.98 |
| RNFL T | 80.01 ± 17.38 | 102 (96.3%) | 3 (2.8%) | 1 (0.9%) | (75–85) | (295–300) |
| RNFL TS | 124.13 ± 27.05 | 75 (70.7%) | 18 (17.0%) | 13 (12.3%) | ||
| RNFL TI | 132.91 ± 24.24 | 46 (43.4%) | 34 (32.1%) | 26 (24.5%) | ||
| RNFL N | 69.76 ± 16.42 | 74 (69.8%) | 11 (10.4%) | 21 (19.8%) | ||
| RNFL NS | 112.26 ± 28.25 | 89 (84.0%) | 14 (13.2%) | 3 (2.8%) | ||
| RNFL NI | 96.89 ± 27.22 | 75 (70.7%) | 19 (18.0%) | 12 (11.3%) | ||
| Quality score | 30.17 ± 3.39 | |||||
| BMO-MRW | BMO-MRW Classification | |||||
| BMO area (mm2) | 2.68 ± 0.74 | |||||
| BMO-MRW G (um) | 262.04 ± 52.87 | 106 (100%) | ||||
| BMO-MRW T | 200.81 ± 45.01 | 106 (100%) | ||||
| BMO-MRW TS | 257.54 ± 62.45 | 106 (100%) | ||||
| BMO-MRW TI | 291.85 ± 61.89 | 106 (100%) | ||||
| BMO-MRW N | 274.54 ± 65.69 | 106 (100%) | ||||
| BMO-MRW NS | 290.48 ± 62.19 | 106 (100%) | ||||
| BMO-MRW NI | 311.69 ± 65.62 | 106 (100%) | ||||
| BMO-fovea angle° | −5.78 ± 3.87 | |||||
| Quality score | 32.92 ± 2.81 | |||||
| Characteristics | Subgroups categorized by CSLO | p Values | ||||
|---|---|---|---|---|---|---|
| Large Disc | Regular Disc | Small Disc | Among 3 Groups* | Post Hoc † | ||
| N (eyes) | Region | 39 | 45 | 12 | ||
| RNFL thickness (um) | G | 95.08 ± 11.41 | 92.02 ± 9.35 | 91.00 ± 7.01 | 0.016 | |
| T | 79.00 ± 15.09 | 77.38 ± 17.48 | 89.75 ± 14.44 | 0.023 | 0.019 (2 vs. 3) | |
| TS | 121.97 ± 26.13 | 123.44 ± 26.27 | 134.33 ± 31.28 | 0.378 | ||
| TI | 134.85 ± 20.81 | 134.53 ± 25.12 | 134.75 ± 28.46 | 0.941 | ||
| N | 75.13 ± 15.27 | 69.04 ± 13.85 | 52.75 ± 16.71 | <0.0001 | 0.015 (2 vs. 3), <0.0001 (1 vs. 3) | |
| NS | 114.79 ± 30.86 | 110.80 ± 28.23 | 107.33 ± 27.88 | 0.5089 | ||
| NI | 100.10 ± 23.23 | 96.00 ± 32.66 | 96.50 ± 22.20 | 0.196 | ||
| RNFL classification (WNL/BL/ONL) | G | 28/6/5 | 37/5/3 | 8/1/3 | 0.324 | |
| T | 37/2/0 | 44/0/1 | 12/0/0 | 0.614 | ||
| TS | 24/9/6 | 34/6/5 | 11/0/1 | 0.133 | ||
| TI | 14/15/10 | 25/9/11 | 6/4/2 | 0.379 | ||
| N | 30/4/5 | 31/6/8 | 5/0/7 | 0.026 | ||
| NS | 34/3/2 | 36/8/1 | 9/3/0 | 0.613 | ||
| NI | 29/5/5 | 32/9/4 | 7/3/2 | 0.594 | ||
| Superior peak location (deg) | 79.69 ± 16.26 | 79.76 ± 14.05 | 75.42 ± 10.73 | 0.552 | ||
| Inferior peak location (deg) | 298.92 ± 12.67 | 298.62 ± 12.49 | 286.50 ± 29.61 | 0.303 | ||
| HVF category (WNL/BL/ONL) | 29/5/5 | 33/6/6 | 6/4/2 | 0.317 | ||
| SE (D) | −2.74 ± 3.77 | −2.19 ± 3.27 | −4.28 ± 3.70 | 0.206 | ||
| Characteristics | Subgroups Categorized by SE | p-Values * | ||||
|---|---|---|---|---|---|---|
| SE > −2.0 D | SE −2.0–−5.0 D | SE < −5.0 D | Among 3 Groups | Post Hoc † | ||
| N (eyes) | Region | 54 | 18 | 34 | ||
| RNFL thickness (um) | G | 92.56 ± 9.21 | 89.50 ± 9.67 | 95.76 ±11.17 | 0.028 | 0.029 (2 vs. 3) |
| T | 75.59 ± 16.34 | 75.06 ± 7.74 | 89.65 ±18.98 | <0.0001 | <0.0001 (1 vs. 3), 0.017 (2 vs. 3) | |
| TS | 119.44 ± 25.15 | 121.50 ± 23.41 | 132.97 ±30.16 | 0.045 | 0.048 (1 vs. 3) | |
| TI | 126.07 ± 25.12 | 129.28 ± 25.30 | 145.68 ±16.60 | <0.0001 | <0.0001 (1 vs. 3) | |
| N | 73.48 ± 14.66 | 68.44 ± 13.42 | 64.56 ±19.18 | 0.061 | ||
| NS | 113.15 ± 25.49 | 113.61 ± 30.61 | 110.15 ±31.72 | 0.969 | ||
| NI | 102.65 ± 30.31 | 84.00 ± 23.50 | 94.56 ±21.13 | 0.020 | 0.017 (1 vs. 2) | |
| RNFL classification (WNL/BL/ONL) | G | 45/6/3 | 9/5/4 | 26/3/5 | 0.018 | |
| T | 51/2/1/ | 18/0/0 | 33/1/0 | 0.537 | ||
| TS | 36/10/8 | 12/4/2 | 27/4/3 | 0.421 | ||
| TI | 20/20/14 | 7/5/6 | 20/8/6 | 0.152 | ||
| N | 45/5/4 | 13/2/3 | 16/4/14 | 0.001 | ||
| NS | 48/6/0 | 14/3/1 | 27/5/2 | 0.327 | ||
| NI | 47/4/3 | 7/8/3 | 21/7/6 | <0.0001 | ||
| Superior peak location (deg) | 81.65 ± 14.69 | 81.33 ± 14.66 | 74.47 ±15.07 | |||
| Inferior peak location (deg) | 297.43 ± 13.90 | 299.94 ± 11.36 | 2.19 ±0.85 | |||
| Disc area (mm2) | 2.45 ± 0.58 | 2.40 ± 0.47 | 2.19 ±0.85 | |||
| HVF category (WNL/BL/ONL) | 35/7/8 | 12/1/5 | 24/7/2 | |||
| Characteristics | Subgroups Categorized by HVF | p-Values | |||
|---|---|---|---|---|---|
| WNL | BL | ONL | Among 3 Groups * | ||
| N (eyes) | Region | 72 | 14 | 15 | |
| RNFL thickness (um) | G | 93.56 ± 10.27 | 92.79 ± 9.05 | 91.43 ± 14.98 | 0.350 |
| T | 80.76 ± 17.27 | 81.43 ± 20.75 | 78.87 ± 18.89 | 0.414 | |
| TS | 124.94 ± 27.18 | 131.36 ± 24.63 | 122.75 ± 29.67 | 0.208 | |
| TI | 135.63 ± 23.95 | 131.36 ± 18.94 | 130.79 ± 28.22 | 0.557 | |
| N | 69.11 ± 17.00 | 64.36 ± 12.48 | 68.57 ± 17.65 | 0.095 | |
| NS | 112.22 ± 28.65 | 118.07 ± 31.50 | 110.11 ± 29.83 | 0.530 | |
| NI | 97.75 ± 29.69 | 94.36 ± 21.45 | 95.53 ± 28.70 | 0.924 | |
| RNFL classification (WNL/BL/ONL) | G | 52/12/8 | 12/1/1 | 12/1/2 | 0.562 |
| T | 70/2/0 | 13/0/1 | 15/0/0 | 0.506 | |
| TS | 51/12/9 | 13/0/1 | 8/5/2 | 0.100 | |
| TI | 29/24/19 | 7/5/2 | 9/2/4 | 0.481 | |
| N | 46/10/16 | 10/0/4 | 14/0/1 | 0.109 | |
| NS | 60/10/2 | 12/2/0 | 12/2/1 | 0.890 | |
| NI | 50/13/9 | 10/2/2 | 11/3/1 | 0.926 | |
| Superior peak location (deg) | 78.78 ± 14.28 | 79.36 ± 15.01 | 77.94 ± 17.14 | 0.741 | |
| Inferior peak location (deg) | 297.71 ± 17.00 | 299.86 ± 14.12 | 292.23 ± 42.41 | 0.883 | |
| Disc area (mm2) | 2.46 ± 0.70 | 1.99 ± 0.48 | 2.31 ± 0.72 | 0.055 | |
| SE (D) | −2.64 ± 3.62 | −3.04 ± 3.38 | −2.46 ± 3.57 | 0.537 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, H.-k.; Kee, C. Characteristics of Patients Showing Discrepancy Between Bruch’s Membrane Opening-Minimum Rim Width and Peripapillary Retinal Nerve Fiber Layer Thickness. J. Clin. Med. 2019, 8, 1362. https://doi.org/10.3390/jcm8091362
Cho H-k, Kee C. Characteristics of Patients Showing Discrepancy Between Bruch’s Membrane Opening-Minimum Rim Width and Peripapillary Retinal Nerve Fiber Layer Thickness. Journal of Clinical Medicine. 2019; 8(9):1362. https://doi.org/10.3390/jcm8091362
Chicago/Turabian StyleCho, Hyun-kyung, and Changwon Kee. 2019. "Characteristics of Patients Showing Discrepancy Between Bruch’s Membrane Opening-Minimum Rim Width and Peripapillary Retinal Nerve Fiber Layer Thickness" Journal of Clinical Medicine 8, no. 9: 1362. https://doi.org/10.3390/jcm8091362
APA StyleCho, H.-k., & Kee, C. (2019). Characteristics of Patients Showing Discrepancy Between Bruch’s Membrane Opening-Minimum Rim Width and Peripapillary Retinal Nerve Fiber Layer Thickness. Journal of Clinical Medicine, 8(9), 1362. https://doi.org/10.3390/jcm8091362





