Good to Excellent Functional Short-Term Outcome and Low Revision Rates Following Primary Anterior Cruciate Ligament Repair Using Suture Augmentation
Abstract
:1. Introduction
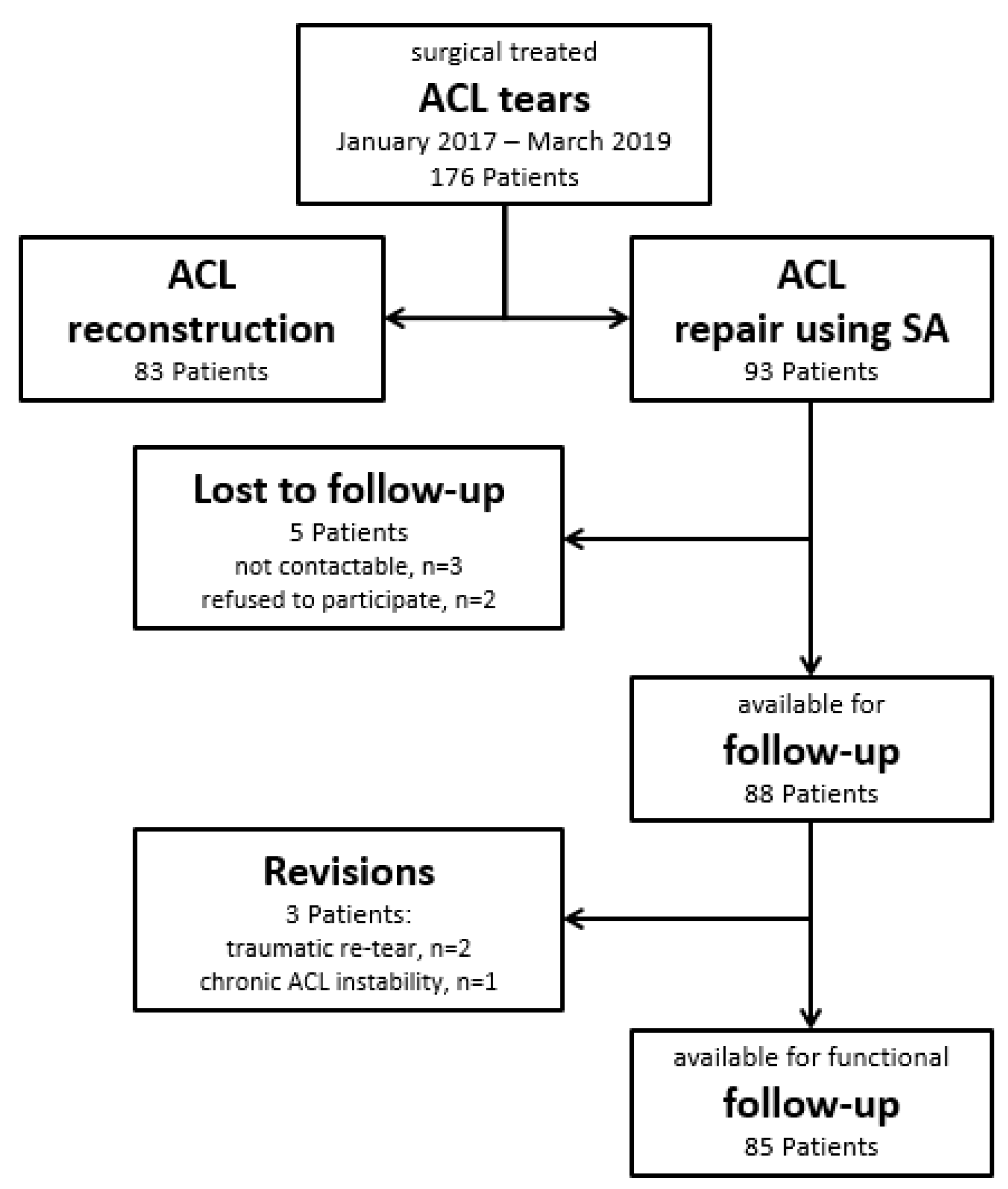
2. Patients and Methods
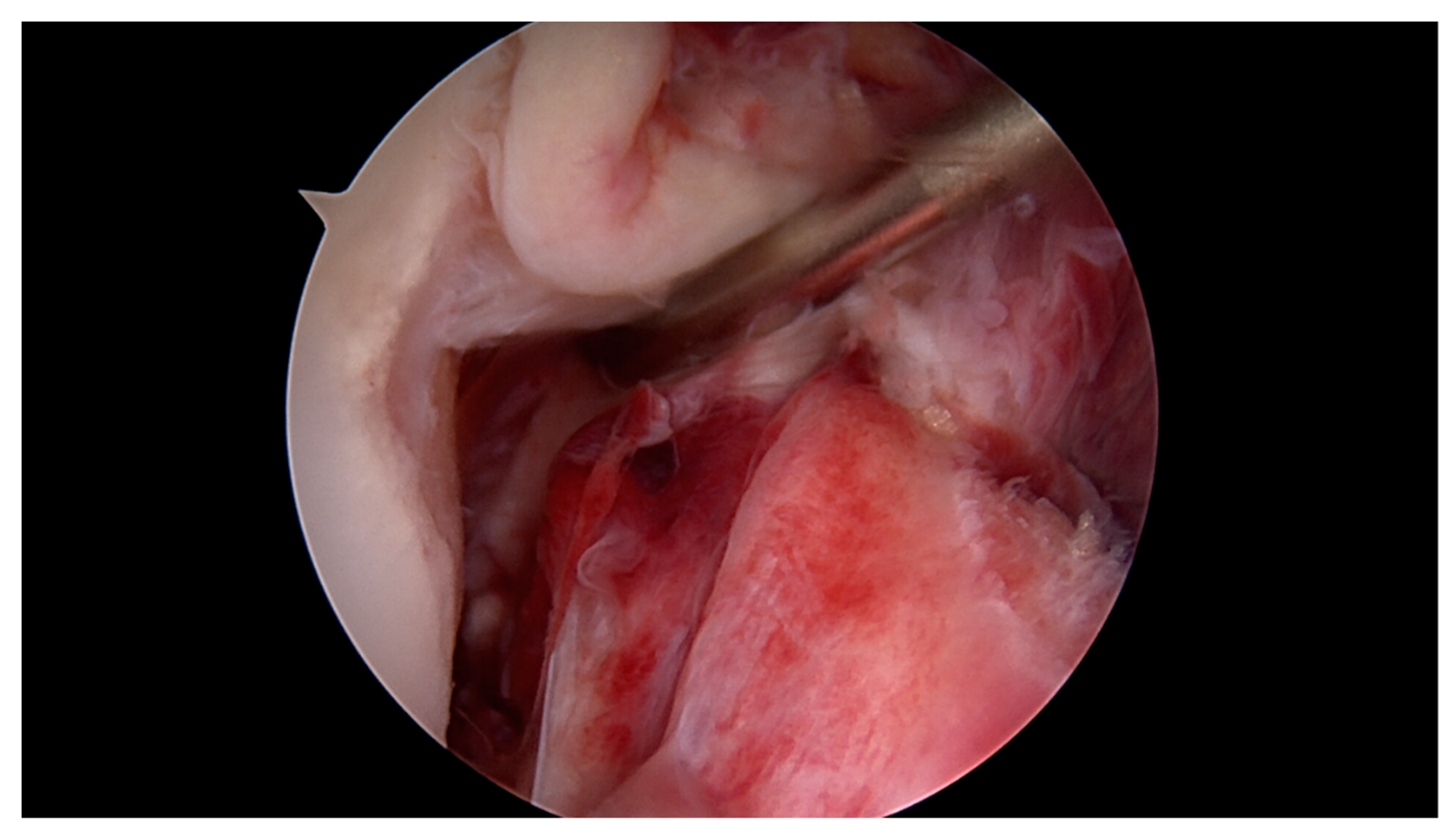
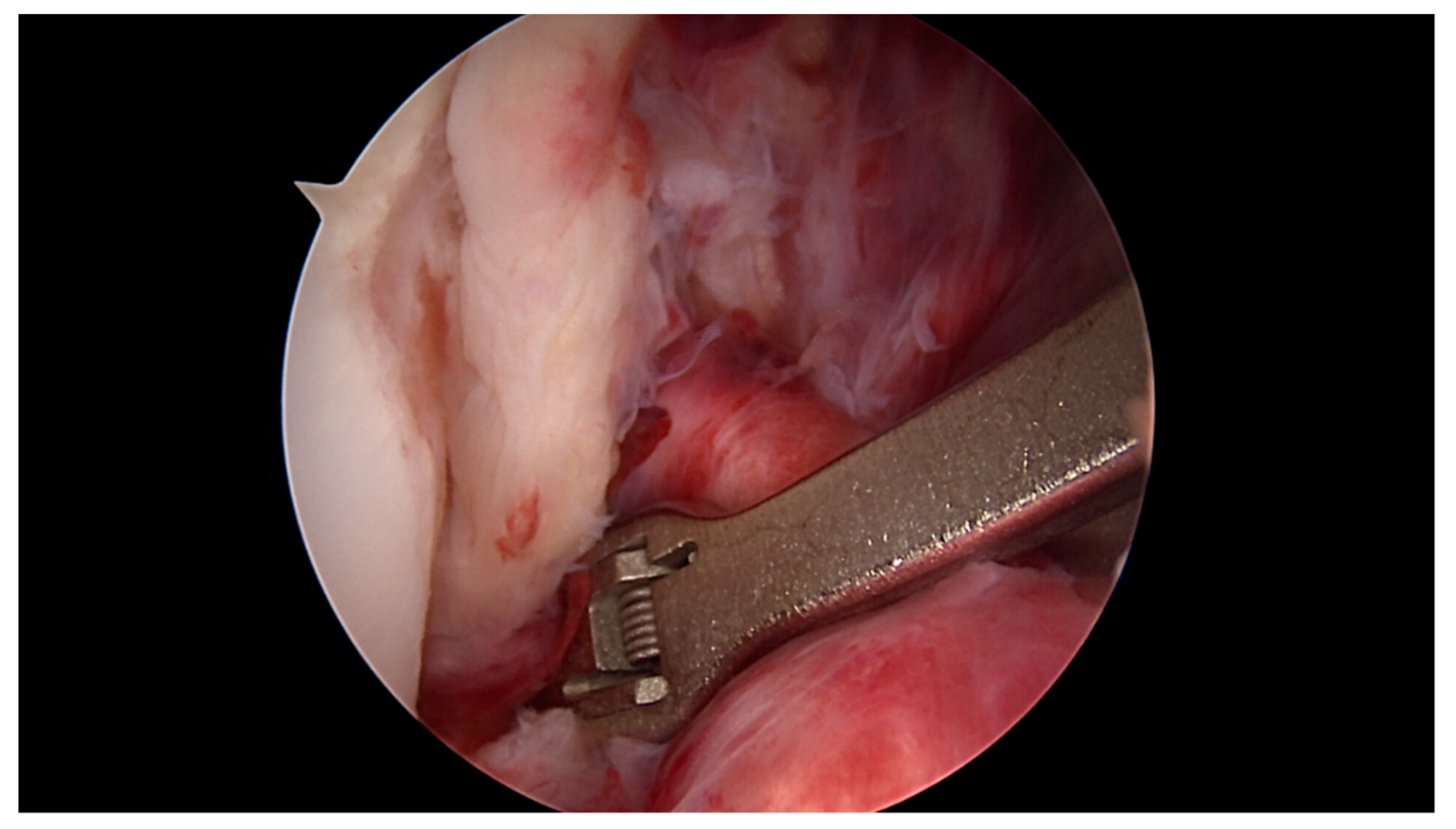
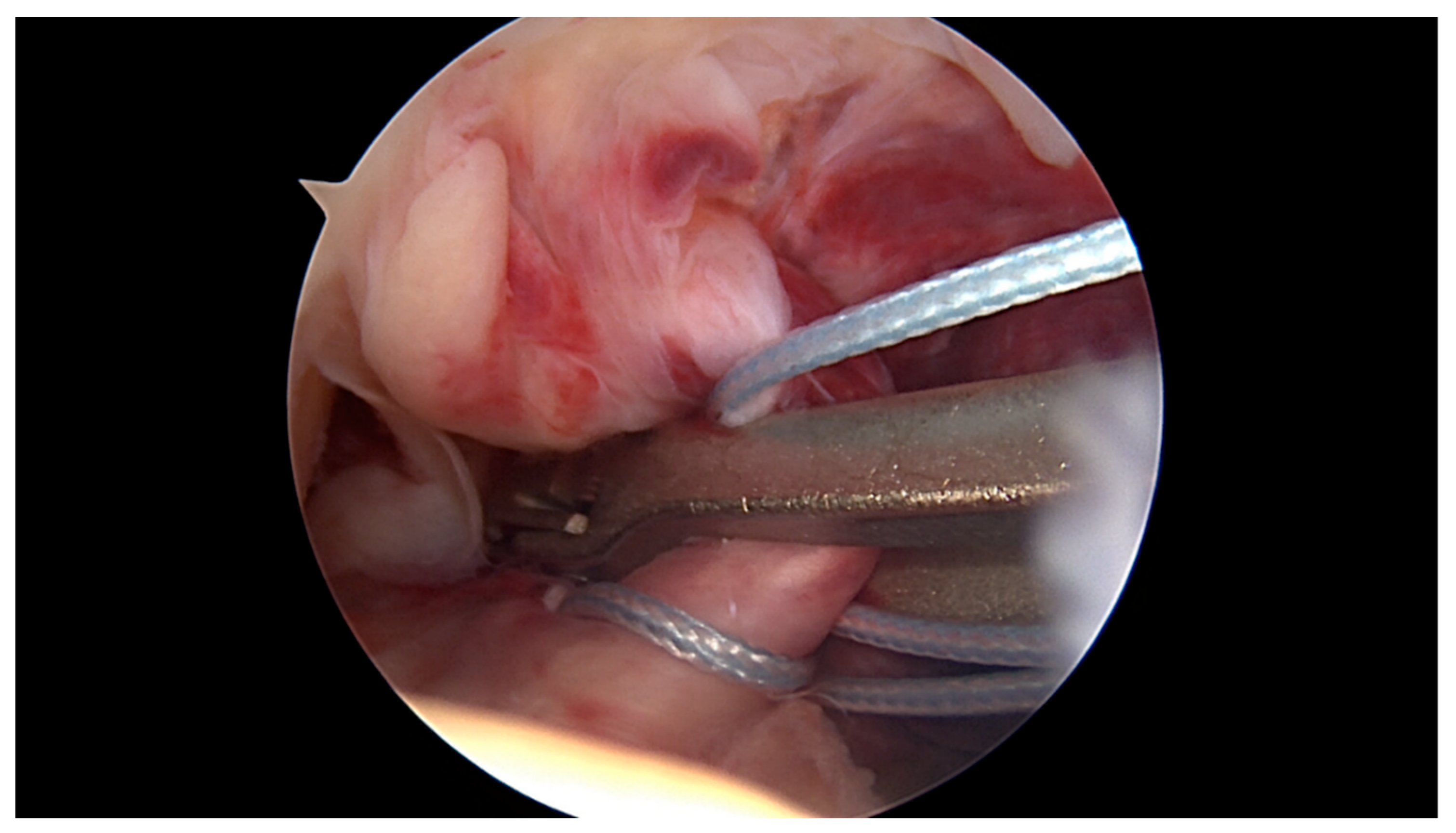
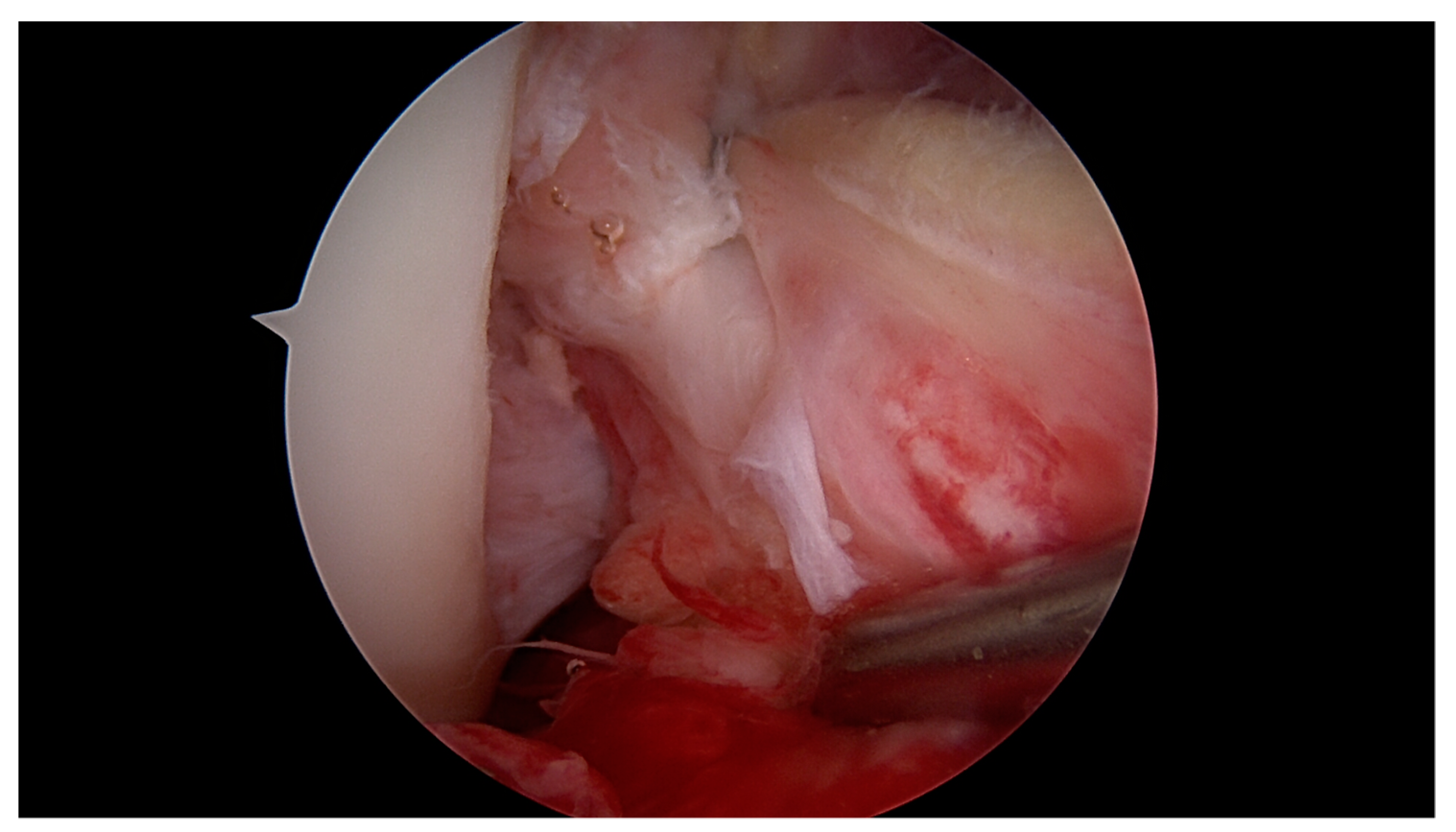
2.1. Surgical Technique and Rehabilitation
2.2. Follow-Up Examinations
2.3. Statistical Analysis and Clinical Relevance
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Aglietti, P.; Giron, F.; Buzzi, R.; Biddau, F.; Sasso, F. Anterior cruciate ligament reconstruction: Bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J. Bone Joint Surg. Am. 2004, 86-A, 2143–2155. [Google Scholar] [CrossRef]
- Fithian, D.C.; Paxton, E.W.; Stone, M.L.; Luetzow, W.F.; Csintalan, R.P.; Phelan, D.; Daniel, D.M. Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am. J. Sports Med. 2005, 33, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Krause, M.; Freudenthaler, F.; Frosch, K.-H.; Achtnich, A.; Petersen, W.; Akoto, R. Operative Versus Conservative Treatment of Anterior Cruciate Ligament Rupture. Dtsch. Arztebl. Int. 2018, 115, 855–862. [Google Scholar] [CrossRef] [PubMed]
- Mahapatra, P.; Horriat, S.; Anand, B.S. Anterior cruciate ligament repair—Past, present and future. J. Exp. Orthop. 2018, 5, 20. [Google Scholar] [CrossRef] [Green Version]
- Feagin, J.A.; Curl, W.W. Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am. J. Sports Med. 1976, 4, 95–100. [Google Scholar] [CrossRef]
- Sherman, M.F.; Bonamo, J.R. Primary repair of the anterior cruciate ligament. Clin. Sports Med. 1988, 7, 739–750. [Google Scholar] [CrossRef]
- Grøntvedt, T.; Engebretsen, L.; Benum, P.; Fasting, O.; Mølster, A.; Strand, T. A prospective, randomized study of three operations for acute rupture of the anterior cruciate ligament. Five-year follow-up of one hundred and thirty-one patients. J. Bone Joint Surg. Am. 1996, 78, 159–168. [Google Scholar] [CrossRef] [PubMed]
- DiFelice, G.S.; Villegas, C.; Taylor, S. Anterior Cruciate Ligament Preservation: Early Results of a Novel Arthroscopic Technique for Suture Anchor Primary Anterior Cruciate Ligament Repair. Arthroscopy 2015, 31, 2162–2171. [Google Scholar] [CrossRef] [PubMed]
- van Eck, C.F.; Limpisvasti, O.; ElAttrache, N.S. Is There a Role for Internal Bracing and Repair of the Anterior Cruciate Ligament? A Systematic Literature Review. Am. J. Sports Med. 2018, 46, 2291–2298. [Google Scholar] [CrossRef]
- van der List, J.P.; Jonkergouw, A.; van Noort, A.; Kerkhoffs, G.M.M.J.; DiFelice, G.S. Identifying candidates for arthroscopic primary repair of the anterior cruciate ligament: A case-control study. Knee 2019, 26, 619–627. [Google Scholar] [CrossRef]
- Heusdens, C.H.W.; Hopper, G.P.; Dossche, L.; Roelant, E.; Mackay, G.M. Anterior cruciate ligament repair with Independent Suture Tape Reinforcement: A case series with 2-year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 60–67. [Google Scholar] [CrossRef] [PubMed]
- MacKay, G.; Anthony, I.C.; Jenkins, P.J.; Blyth, M. Anterior Cruciate Ligament Repair Revisited. Preliminary Results of Primary Repair with Internal Brace Ligament Augmentation: A Case Series. Orthop. Muscul. Syst. 2015, 4, 1–5. [Google Scholar]
- Jonkergouw, A.; van der List, J.P.; DiFelice, G.S. Arthroscopic primary repair of proximal anterior cruciate ligament tears: Outcomes of the first 56 consecutive patients and the role of additional internal bracing. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Daniels, S.P.; van der List, J.P.; Kazam, J.J.; DiFelice, G.S. Arthroscopic primary repair of the anterior cruciate ligament: What the radiologist needs to know. Skeletal Radiol. 2018, 47, 619–629. [Google Scholar] [CrossRef]
- Daniel, D.M.; Stone, M.L.; Sachs, R.; Malcom, L. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am. J. Sports Med. 1985, 13, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Collins, N.J.; Misra, D.; Felson, D.T.; Crossley, K.M.; Roos, E.M. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res. (Hoboken) 2011, 63 (Suppl. S11), S208–S228. [Google Scholar]
- Briggs, K.K.; Lysholm, J.; Tegner, Y.; Rodkey, W.G.; Kocher, M.S.; Steadman, J.R. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am. J. Sports Med. 2009, 37, 890–897. [Google Scholar] [CrossRef]
- Harris, J.D.; Brand, J.C.; Cote, M.P.; Faucett, S.C.; Dhawan, A. Research Pearls: The Significance of Statistics and Perils of Pooling. Part 1: Clinical Versus Statistical Significance. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 1102–1112. [Google Scholar] [CrossRef]
- Schneider, K.N.; Weller, J.F.; K Buddhdev, P.; Ahlbäumer, G. Arthroscopic Anterior Cruciate Ligament Re-Repair Using Internal Brace Augmentation—A Case Report. J. Orthop. Case Rep. 2019, 10, 11–15. [Google Scholar]
- Meister, M.; Koch, J.; Amsler, F.; Arnold, M.P.; Hirschmann, M.T. ACL suturing using dynamic intraligamentary stabilisation showing good clinical outcome but a high reoperation rate: A retrospective independent study. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 655–659. [Google Scholar] [CrossRef]
- Henle, P.; Bieri, K.S.; Brand, M.; Aghayev, E.; Bettfuehr, J.; Haeberli, J.; Kess, M.; Eggli, S. Patient and surgical characteristics that affect revision risk in dynamic intraligamentary stabilization of the anterior cruciate ligament. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1182–1189. [Google Scholar] [CrossRef] [PubMed]
- Osti, M.; El Attal, R.; Doskar, W.; Höck, P.; Smekal, V. High complication rate following dynamic intraligamentary stabilization for primary repair of the anterior cruciate ligament. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Borchers, J.R.; Kaeding, C.C.; Pedroza, A.D.; Huston, L.J.; Spindler, K.P.; Wright, R.W. MOON Consortium and the MARS Group Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: A comparison of the MOON and MARS study groups. Am. J. Sports Med. 2011, 39, 1889–1893. [Google Scholar] [CrossRef] [Green Version]
- Brambilla, L.; Pulici, L.; Carimati, G.; Quaglia, A.; Prospero, E.; Bait, C.; Morenghi, E.; Portinaro, N.; Denti, M.; Volpi, P. Prevalence of Associated Lesions in Anterior Cruciate Ligament Reconstruction: Correlation With Surgical Timing and With Patient Age, Sex, and Body Mass Index. Am. J. Sports Med. 2015, 43, 2966–2973. [Google Scholar] [CrossRef]
- Shelbourne, K.D.; Gray, T. Minimum 10-year results after anterior cruciate ligament reconstruction: How the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am. J. Sports Med. 2009, 37, 471–480. [Google Scholar] [CrossRef] [PubMed]
- Webster, K.E.; Feller, J.A.; Kimp, A.; Devitt, B.M. Medial meniscal and chondral pathology at the time of revision anterior cruciate ligament reconstruction results in inferior mid-term patient-reported outcomes. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1059–1064. [Google Scholar] [CrossRef]
- LaPrade, C.M.; Dornan, G.J.; Granan, L.-P.; LaPrade, R.F.; Engebretsen, L. Outcomes After Anterior Cruciate Ligament Reconstruction Using the Norwegian Knee Ligament Registry of 4691 Patients: How Does Meniscal Repair or Resection Affect Short-term Outcomes? Am. J. Sports Med. 2015, 43, 1591–1597. [Google Scholar] [CrossRef]
- Van der List, J.P.; DiFelice, G.S. Arthroscopic Primary Anterior Cruciate Ligament Repair with Suture Augmentation. Arthrosc. Tech. 2017, 6, e1529–e1534. [Google Scholar] [CrossRef]
- Ateschrang, A.; Schreiner, A.J.; Ahmad, S.S.; Schröter, S.; Hirschmann, M.T.; Körner, D.; Kohl, S.; Stöckle, U.; Ahrend, M.-D. Improved results of ACL primary repair in one-part tears with intact synovial coverage. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 37–43. [Google Scholar] [CrossRef]
- Murray, M.M.; Martin, S.D.; Martin, T.L.; Spector, M. Histological changes in the human anterior cruciate ligament after rupture. J. Bone Joint Surg. Am. 2000, 82, 1387–1397. [Google Scholar] [CrossRef]
- Magarian, E.M.; Fleming, B.C.; Harrison, S.L.; Mastrangelo, A.N.; Badger, G.J.; Murray, M.M. Delay of 2 or 6 weeks adversely affects the functional outcome of augmented primary repair of the porcine anterior cruciate ligament. Am. J. Sports Med. 2010, 38, 2528–2534. [Google Scholar] [CrossRef] [Green Version]
- Kohl, S.; Evangelopoulos, D.S.; Kohlhof, H.; Hartel, M.; Bonel, H.; Henle, P.; von Rechenberg, B.; Eggli, S. Anterior crucial ligament rupture: Self-healing through dynamic intraligamentary stabilization technique. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 599–605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schliemann, B.; Lenschow, S.; Domnick, C.; Herbort, M.; Häberli, J.; Schulze, M.; Wähnert, D.; Raschke, M.J.; Kösters, C. Knee joint kinematics after dynamic intraligamentary stabilization: Cadaveric study on a novel anterior cruciate ligament repair technique. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1184–1190. [Google Scholar] [CrossRef] [PubMed]
- Häberli, J.; Voumard, B.; Kösters, C.; Delfosse, D.; Henle, P.; Eggli, S.; Zysset, P. Implant preloading in extension reduces spring length change in dynamic intraligamentary stabilization: A biomechanical study on passive kinematics of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3582–3592. [Google Scholar] [CrossRef] [PubMed]
- Hoogeslag, R.A.G.; Brouwer, R.W.; de Vries, A.J.; Boer, B.C.; Huis In’t Veld, R. Efficacy of Nonaugmented, Static Augmented, and Dynamic Augmented Suture Repair of the Ruptured Anterior Cruciate Ligament: A Systematic Review of the Literature. Am. J. Sports Med. 2020, 26, 363546520904690. [Google Scholar] [CrossRef] [PubMed]
- Hoogeslag, R.A.G.; Brouwer, R.W.; Boer, B.C.; de Vries, A.J.; Huis In’t Veld, R. Acute Anterior Cruciate Ligament Rupture: Repair or Reconstruction? Two-Year Results of a Randomized Controlled Clinical Trial. Am. J. Sports Med. 2019, 47, 567–577. [Google Scholar] [CrossRef]
- Ahmad, S.S.; Schürholz, K.; Liechti, E.F.; Hirschmann, M.T.; Kohl, S.; Klenke, F.M. Seventy percent long-term survival of the repaired ACL after dynamic intraligamentary stabilization. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Kösters, C.; Glasbrenner, J.; Spickermann, L.; Kittl, C.; Domnick, C.; Herbort, M.; Raschke, M.J.; Schliemann, B. Repair With Dynamic Intraligamentary Stabilization Versus Primary Reconstruction of Acute Anterior Cruciate Ligament Tears: 2-Year Results From a Prospective Randomized Study. Am. J. Sports Med. 2020, 26, 363546520905863. [Google Scholar] [CrossRef]
- Weaver, J.K.; Derkash, R.S.; Freeman, J.R.; Kirk, R.E.; Oden, R.R.; Matyas, J. Primary knee ligament repair--revisited. Clin. Orthop. Relat. Res. 1985, 199, 185–191. [Google Scholar] [CrossRef]
- Bachmaier, S.; DiFelice, G.S.; Sonnery-Cottet, B.; Douoguih, W.A.; Smith, P.A.; Pace, L.J.; Ritter, D.; Wijdicks, C.A. Treatment of Acute Proximal Anterior Cruciate Ligament Tears—Part 2: The Role of Internal Bracing on Gap Formation and Stabilization of Repair Techniques. Orthop. J. Sports Med. 2020, 8, 2325967119897423. [Google Scholar] [CrossRef]
- DiFelice, G.S.; van der List, J.P. Clinical Outcomes of Arthroscopic Primary Repair of Proximal Anterior Cruciate Ligament Tears Are Maintained at Mid-term Follow-up. Arthroscopy 2018, 34, 1085–1093. [Google Scholar] [CrossRef] [PubMed]

| Concomitant Injury Present | ||||
|---|---|---|---|---|
| Yes vs. No (Estimated Median; 95% CI) | ||||
| Patients (%) | IKDC * | LS * | TSDiff * | |
| Concomitant injuries | 76 (86%) | 90.8 vs. 92.0 | 95 vs. 95 | 0 vs. 0 |
| (−3.4; −8, 2.3) | (0; −5, 1) | (0; 0, 0) | ||
| p = 0.239 | p = 0.384 | p = 0.858 | ||
| Posterolateral fracture | 10 (11%) | 85.7 vs. 90.8 | 95 vs. 95 | 0 vs. 0 |
| (4.6; −2.3, 12) | (5; 0, 11) | (0; −1, 0) | ||
| p = 0.226 | p = 0.108 | p = 0.103 | ||
| Meniscus | 49 (56%) | 90.8 vs. 89.7 | 95 vs. 95 | 0 vs. 0 |
| (0; −4.6, 2.3) | (0; −3, 2) | (0; 0, 0) | ||
| p = 0.741 | p = 0.946 | p = 0.968 | ||
| medial | 29 (33%) | 90.8 vs. 90.3 | 95 vs. 95 | 0 vs. 0 |
| (−2.3; −5.7, 1.2) | (0; −4, 2) | (0; 0, 0) | ||
| p = 0.22 | p = 0.731 | p = 0.419 | ||
| lateral | 27 (31%) | 90.8 vs. 89.7 | 95 vs. 95 | 0 vs. 0 |
| (0; −4.6, 3.5) | (0; −3, 4) | (0; 0, 0) | ||
| p = 0.925 | p = 0.882 | p = 0.953 | ||
| Collateral ligament | 54 (61%) | 88.5 vs. 93.1 | 95 vs. 95 | 0 vs. 0 |
| (3.5; 0, 6.9) | (0; −1, 4) | (0; 0, 0) | ||
| p = 0.053 | p = 0.578 | p = 0.95 | ||
| medial | 49 (56%) | 88.5 vs. 92.6 | 95 vs. 95 | 0 vs. 0 |
| (2.3; −1.1, 5.8) | (0; −4, 1) | (0; 0, 0) | ||
| p = 0.144 | p = 0.889 | p = 0.782 | ||
| Lateral † | 27 (31%) | 89.7 vs. 90.8 | 95 vs. 95 | 1 vs. 0 |
| (2.3; −1.2, 5.8) | (1; −1, 5) | (0; −1, 0) | ||
| p = 0.256 | P = 0.285 | p = 0.107 | ||
| Yes vs. No (Estimated Median; 95% CI) | ||||
|---|---|---|---|---|
| Number of Patients | IKDC * | LS * | TSDiff * | |
| Male vs. Female | 24 vs. 61 | 91.4 vs. 89.7 | 99.5 vs. 95 | 0 vs. 0 |
| (2.3; −1.2, 5.7) | (2; 0, 5) | (0; 0, 0) | ||
| p = 0.304 | p = 0.061 | p = 0.943 | ||
| Age > 40 years vs. ≤40 years | 56 vs. 29 | 90.8 vs. 90.8 | 95 vs. 95 | 0 vs. 0 |
| (−1.1; −4.6, 2.3) | (0; −4, 2) | (0, 0, 0) | ||
| p = 0.512 | p = 0.989 | p = 0.651 | ||
| BMI > 30 vs. ≤30 | 6 vs. 79 | 86.8 vs. 90.8 | 95 vs. 95 | 0.5 vs. 0 |
| (2.3; −3.4, 8) | (0; −5, 5) | (0; −1, 1) | ||
| p = 0.344 | p = 0.892 | p = 0.88 | ||
| Same-day surgery vs. Delay | 37 vs. 48 | 90.8 vs. 90.8 | 95 vs. 95 | 0 vs. 0 |
| (1.2; −2.3, 4.6) | (0; −4, 1) | (0; 0, 0) | ||
| p = 0.47 | p = 0.957 | p = 0.968 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schneider, K.N.; Schliemann, B.; Gosheger, G.; Theil, C.; Weller, J.; Buddhdev, P.K.; Ahlbäumer, G. Good to Excellent Functional Short-Term Outcome and Low Revision Rates Following Primary Anterior Cruciate Ligament Repair Using Suture Augmentation. J. Clin. Med. 2020, 9, 3068. https://doi.org/10.3390/jcm9103068
Schneider KN, Schliemann B, Gosheger G, Theil C, Weller J, Buddhdev PK, Ahlbäumer G. Good to Excellent Functional Short-Term Outcome and Low Revision Rates Following Primary Anterior Cruciate Ligament Repair Using Suture Augmentation. Journal of Clinical Medicine. 2020; 9(10):3068. https://doi.org/10.3390/jcm9103068
Chicago/Turabian StyleSchneider, Kristian Nikolaus, Benedikt Schliemann, Georg Gosheger, Christoph Theil, Jan Weller, Pranai K Buddhdev, and Georg Ahlbäumer. 2020. "Good to Excellent Functional Short-Term Outcome and Low Revision Rates Following Primary Anterior Cruciate Ligament Repair Using Suture Augmentation" Journal of Clinical Medicine 9, no. 10: 3068. https://doi.org/10.3390/jcm9103068




