Role of the Triceps Surae Muscles in Patients Undergoing Anterior Cruciate Ligament Reconstruction: A Matched Case-Control Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Enrollment
2.2. Surgical Technique
2.3. Postoperative Rehabilitation
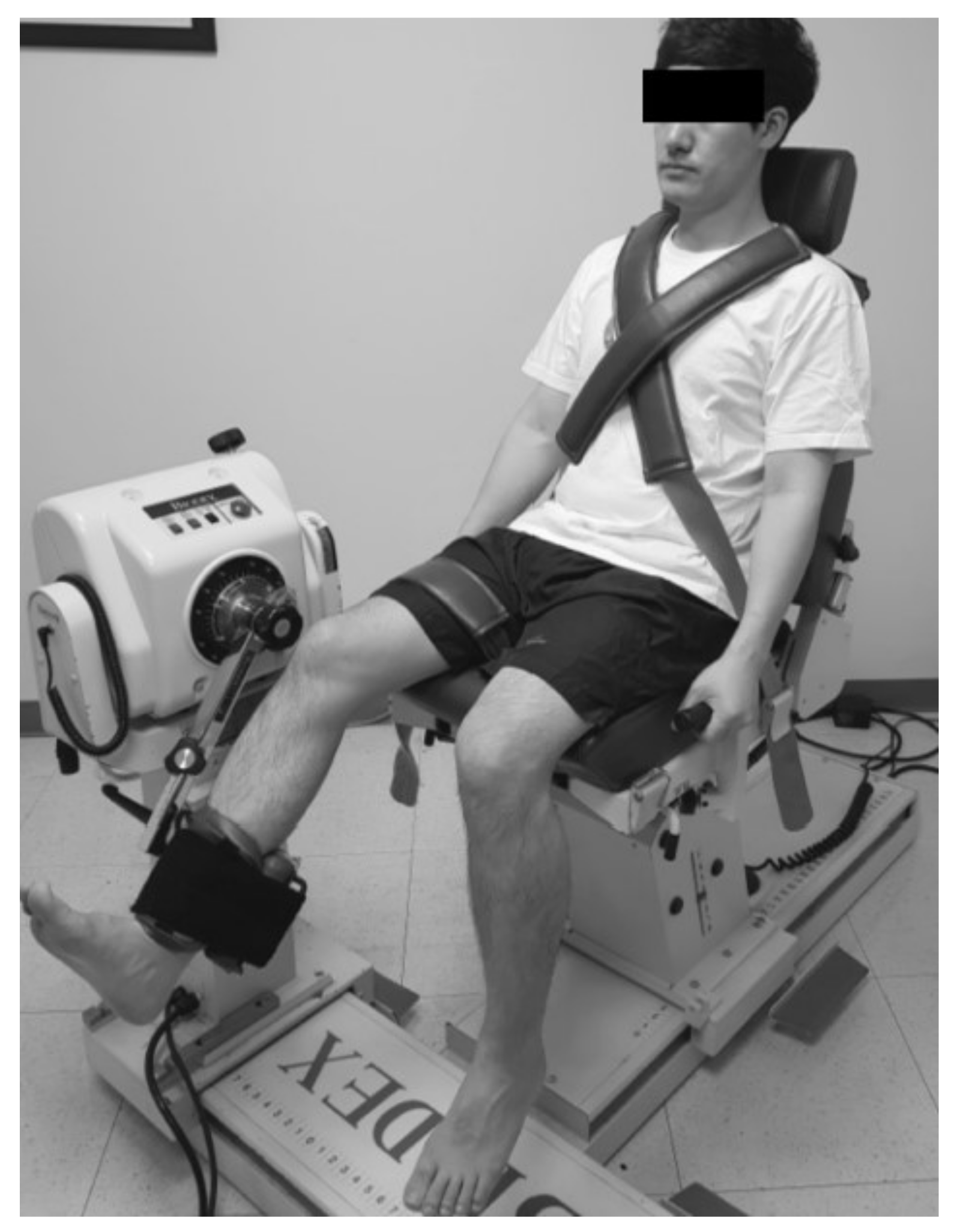
2.4. Assessment of Isokinetic Muscle Performances
2.4.1. Triceps Surae Strength
2.4.2. Hamstring and Quadriceps Strength
2.5. Assessment of Muscle Reaction Time (Acceleration Time)
2.6. Statistical Analysis
3. Results
3.1. Isokinetic Muscle Strength
3.2. Muscle Reaction Time (AT)
4. Discussion
4.1. Strength of Gastrocnemius and Soleus
4.2. Muscle Reaction Time
4.3. Clinical Implications
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Patel, R.R.; Hurwitz, D.E.; Bush-Joseph, C.A.; Bach, B.R., Jr.; Andriacchi, T.P. Comparison of clinical and dynamic knee function in patients with anterior cruciate ligament deficiency. Am. J. Sports Med. 2003, 31, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Mokhtarzadeh, H.; Yeow, C.H.; Hong Goh, J.C.; Oetomo, D.; Malekipour, F.; Lee, P.V. Contributions of the soleus and gastrocnemius muscles to the anterior cruciate ligament loading during single-leg landing. J. Biomech. 2013, 46, 1913–1920. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Han, S.B.; Park, J.H.; Choi, J.H.; Suh, D.K.; Jang, K.M. Impaired neuromuscular control up to postoperative 1 year in operated and nonoperated knees after anterior cruciate ligament reconstruction. Medicine 2019, 98, e15124. [Google Scholar] [CrossRef] [PubMed]
- Myer, G.D.; Ford, K.R.; Hewett, T.E. The effects of gender on quadriceps muscle activation strategies during a maneuver that mimics a high ACL injury risk position. J. Electromyogr. Kinesiol. 2005, 15, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Markolf, K.L.; O’Neill, G.; Jackson, S.R.; McAllister, D.R. Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments. Am. J. Sports Med. 2004, 32, 1144–1149. [Google Scholar] [CrossRef]
- Mesfar, W.; Shirazi-Adl, A. Knee joint mechanics under quadriceps--hamstrings muscle forces are influenced by tibial restraint. Clin. Biomech. 2006, 21, 841–848. [Google Scholar] [CrossRef]
- Fleming, B.C.; Renstrom, P.A.; Ohlen, G.; Johnson, R.J.; Peura, G.D.; Beynnon, B.D.; Badger, G.J. The gastrocnemius muscle is an antagonist of the anterior cruciate ligament. J. Orthop. Res. 2001, 19, 1178–1184. [Google Scholar] [CrossRef]
- Adouni, M.; Shirazi-Adl, A.; Marouane, H. Role of gastrocnemius activation in knee joint biomechanics: Gastrocnemius acts as an ACL antagonist. Comput. Methods Biomech. Biomed. Eng. 2016, 19, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.; Andersen, M.S.; Rasmussen, J.; Robertson, D.G.; Rouhi, G. The application of musculoskeletal modeling to investigate gender bias in non-contact ACL injury rate during single-leg landings. Comput. Methods Biomech. Biomed. Eng. 2014, 17, 1602–1616. [Google Scholar] [CrossRef]
- Morgan, K.D.; Donnelly, C.J.; Reinbolt, J.A. Elevated gastrocnemius forces compensate for decreased hamstrings forces during the weight-acceptance phase of single-leg jump landing: Implications for anterior cruciate ligament injury risk. J. Biomech. 2014, 47, 3295–3302. [Google Scholar] [CrossRef] [PubMed]
- Elias, J.J.; Faust, A.F.; Chu, Y.H.; Chao, E.Y.; Cosgarea, A.J. The soleus muscle acts as an agonist for the anterior cruciate ligament. An in vitro experimental study. Am. J. Sports Med. 2003, 31, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Svantesson, E.; Senorski, E.H.; Alentorn-Geli, E.; Westin, O.; Sundemo, D.; Grassi, A.; Čustović, S.; Samuelsson, K. Increased risk of ACL revision with non-surgical treatment of a concomitant medial collateral ligament injury: A study on 19,457 patients from the Swedish National Knee Ligament Registry. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2450–2459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Syam, K.; Chouhan, D.K.; Dhillon, M.S. Outcome of ACL reconstruction for chronic ACL injury in knees without the posterior horn of the medial meniscus: Comparison with ACL reconstructed knees with an intact medial meniscus. Knee Surg. Relat. Res. 2017, 29, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carvalho, H.M.; Silva, C.E.; Manuel, J.; Ronque, E.R.V.; Goncalves, R.S.; Philippaerts, R.M.; Malina, R.M. Assessment of reliability in isokinetic testing among adolescent basketball players. Medicina 2011, 47, 446. [Google Scholar] [CrossRef] [PubMed]
- Möller, M.; Lind, K.; Styf, J.; Karlsson, J. The reliability of isokinetic testing of the ankle joint and a heel-raise test for endurance. Knee Surg. Sports Traumatol. Arthrosc. 2005, 13, 60–71. [Google Scholar] [CrossRef] [PubMed]
- Noyes, F.R.; Barber, S.D.; Mooar, L.A. A rationale for assessing sports activity levels and limitations in knee disorders. Clin. Orthop. Relat. Res. 1989, 246, 238–249. [Google Scholar] [CrossRef]
- Roberts, D.; Friden, T.; Stomberg, A.; Lindstrand, A.; Moritz, U. Bilateral proprioceptive defects in patients with a unilateral anterior cruciate ligament reconstruction: A comparison between patients and healthy individuals. J. Orthop. Res. 2000, 18, 565–571. [Google Scholar] [CrossRef]
- Espejo-Baena, A.; Espejo-Reina, A. Anatomic outside-in anterior cruciate ligament reconstruction using a suspension device for femoral fixation. Arthrosc. Tech. 2014, 3, e265–e269. [Google Scholar] [CrossRef]
- Harato, K.; Niki, Y.; Toyoda, T.; Kamata, Y.; Masumoto, K.; Otani, T.; Suda, Y. Self-flip Technique of the TightRope RT Button for Soft-Tissue Anterior Cruciate Ligament Reconstruction. Arthrosc. Tech. 2016, 5, e391–e395. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Landin, D.; Grodesky, J.; Myers, J. The function of gastrocnemius as a knee flexor at selected knee and ankle angles. J. Electromyogr. Kinesiol. 2002, 12, 385–390. [Google Scholar] [CrossRef]
- Perry, J.; Easterday, C.S.; Antonelli, D.J. Surface versus intramuscular electrodes for electromyography of superficial and deep muscles. Phys. Ther. 1981, 61, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Wilkerson, G.B.; Nitz, A.J. Dynamic ankle stability: Mechanical and neuromuscular interrelationships. J. Sport Rehabil. 1994, 3, 43–57. [Google Scholar] [CrossRef]
- Heilman, A.E.; Braly, W.G.; Bishop, J.O.; Noble, P.C.; Tullos, H.S. An anatomic study of subtalar instability. Foot Ankle 1990, 10, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Van Cingel, R.E.; Kleinrensink, G.; Uitterlinden, E.J.; Rooijens, P.P.; Mulder, P.G.; Aufdemkampe, G.; Stoeckart, R. Repeated ankle sprains and delayed neuromuscular response: Acceleration time parameters. J. Orthop. Sports Phys. Ther. 2006, 36, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Luna, N.M.S.; Alonso, A.C.; Bocalini, D.; Borin, G.; Brech, G.C.; Greve, J.M.D.A. Analysis of acceleration time of ankle in long-distance runners and triathletes. Med. Express 2017, 4. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.H.; Park, J.S.; Hwang, H.J.; Jeong, W.K. Time to peak torque and acceleration time are altered in male patients following traumatic shoulder instability. J. Shoulder Elbow Surg. 2018, 27, 1505–1511. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, S.H.; Choi, G.W.; Jung, H.W.; Jang, W.Y. Individuals with recurrent ankle sprain demonstrate postural instability and neuromuscular control deficits in unaffected side. Knee Surg. Sports Traumatol. Arthrosc. 2018. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, S.H.; Jung, H.W.; Jang, W.Y. Modified Brostrom procedure in patients with chronic ankle instability is superior to conservative treatment in terms of muscle endurance and postural stability. Knee Surg. Sports Traumatol. Arthrosc. 2019. [Google Scholar] [CrossRef]
- Lee, D.H.; Lee, J.H.; Jeong, H.J.; Lee, S.J. Serial changes in knee muscle strength after anterior cruciate ligament reconstruction using hamstring tendon autografts. Arthroscopy 2015, 31, 890–895. [Google Scholar] [CrossRef]
- Durselen, L.; Claes, L.; Kiefer, H. The influence of muscle forces and external loads on cruciate ligament strain. Am. J. Sports Med. 1995, 23, 129–136. [Google Scholar] [CrossRef]
- O’Connor, J.J. Can muscle co-contraction protect knee ligaments after injury or repair? J. Bone Jt. Surg. Br. 1993, 75, 41–48. [Google Scholar] [CrossRef] [Green Version]
- Pflum, M.A.; Shelburne, K.B.; Torry, M.R.; Decker, M.J.; Pandy, M.G. Model prediction of anterior cruciate ligament force during drop-landings. Med. Sci. Sports Exerc. 2004, 36, 1949–1958. [Google Scholar] [CrossRef] [PubMed]
- Sherbondy, P.S.; Queale, W.S.; McFarland, E.G.; Mizuno, Y.; Cosgarea, A.J. Soleus and gastrocnemius muscle loading decreases anterior tibial translation in anterior cruciate ligament intact and deficient knees. J. Knee Surg. 2003, 16, 152–158. [Google Scholar] [PubMed]
- Delmas, S.; Casamento-Moran, A.; Park, S.H.; Yacoubi, B.; Christou, E.A. Motor planning perturbation: Muscle activation and reaction time. J. Neurophysiol. 2018, 120, 2059–2065. [Google Scholar] [CrossRef] [PubMed]
- Richie, D.H., Jr. Functional instability of the ankle and the role of neuromuscular control: A comprehensive review. J. Foot Ankle Surg 2001, 40, 240–251. [Google Scholar] [CrossRef]
- Arnold, P.; Vantieghem, S.; Gorus, E.; Lauwers, E.; Fierens, Y.; Pool-Goudzwaard, A.; Bautmans, I. Age-related differences in muscle recruitment and reaction-time performance. Exp. Gerontol. 2015, 70, 125–130. [Google Scholar] [CrossRef]
- Thain, P.K.; Bleakley, C.M.; Mitchell, A.C. Muscle Reaction Time During a Simulated Lateral Ankle Sprain After Wet-Ice Application or Cold-Water Immersion. J. Athl. Train. 2015, 50, 697–703. [Google Scholar] [CrossRef] [Green Version]
- Wojtys, E.M.; Huston, L.J. Neuromuscular performance in normal and anterior cruciate ligament-deficient lower extremities. Am. J. Sports Med. 1994, 22, 89–104. [Google Scholar] [CrossRef] [Green Version]
- Lloyd, D.G.; Buchanan, T.S. Strategies of muscular support of varus and valgus isometric loads at the human knee. J. Biomech. 2001, 34, 1257–1267. [Google Scholar] [CrossRef]
- Pamukoff, D.N.; Pietrosimone, B.G.; Ryan, E.D.; Lee, D.R.; Blackburn, J.T. Quadriceps Function and Hamstrings Co-Activation After Anterior Cruciate Ligament Reconstruction. J. Athl. Train. 2017, 52, 422–428. [Google Scholar] [CrossRef] [Green Version]
- Norte, G.E.; Hertel, J.; Saliba, S.A.; Diduch, D.R.; Hart, J.M. Quadriceps Neuromuscular Function in Patients With Anterior Cruciate Ligament Reconstruction With or Without Knee Osteoarthritis: A Cross-Sectional Study. J. Athl. Train. 2018, 53, 475–485. [Google Scholar] [CrossRef] [PubMed]
- Klyne, D.M.; Keays, S.L.; Bullock-Saxton, J.E.; Newcombe, P.A. The effect of anterior cruciate ligament rupture on the timing and amplitude of gastrocnemius muscle activation: A study of alterations in EMG measures and their relationship to knee joint stability. J. Electromyogr. Kinesiol. 2012, 22, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, J.T.; Ingersoll, C.D.; Krause, B.A.; Edwards, J.E.; Cordova, M.L. Effect of knee joint effusion on quadriceps and soleus motoneuron pool excitability. Med. Sci. Sports Exerc. 2001, 33, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Coats-Thomas, M.S.; Miranda, D.L.; Badger, G.J.; Fleming, B.C. Effects of ACL reconstruction surgery on muscle activity of the lower limb during a jump-cut maneuver in males and females. J. Orthop. Res. 2013, 31, 1890–1896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alentorn-Geli, E.; Alvarez-Diaz, P.; Ramon, S.; Marin, M.; Steinbacher, G.; Rius, M.; Seijas, R.; Ares, O.; Cugat, R. Assessment of gastrocnemius tensiomyographic neuromuscular characteristics as risk factors for anterior cruciate ligament injury in male soccer players. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 2502–2507. [Google Scholar] [CrossRef]
- Van Grinsven, S.; Van Cingel, R.; Holla, C.; Van Loon, C. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1128–1144. [Google Scholar] [CrossRef]
- Kvist, J. Sagittal plane translation during level walking in poor-functioning and well-functioning patients with anterior cruciate ligament deficiency. Am. J. Sports Med. 2004, 32, 1250–1255. [Google Scholar] [CrossRef]
- Perelli, S.; Erquicia, J.I.; Marin, C.M.; Salgado, W.T.B.; Masferrer-Pino, A.; Perez-Prieto, D.; Monllau, J.C. Central Transpatellar Tendon Portal Is Safe When Used for Anterior Cruciate Ligament Reconstruction. J. Knee Surg. 2020. [Google Scholar] [CrossRef]

| ACL Reconstruction (n = 32) | Normal Control (n = 32) | p Value | |
|---|---|---|---|
| Gender (male/female) | 12/20 | 15/17 | 0.448 |
| Age (years) a | 30 ± 7 (23–44) | 29 ± 8 (21–43) | 0.384 |
| Height (cm) a | 174 ± 7 (162–184) | 173 ± 3 (157–187) | 0.397 |
| Weight (kg) a | 68 ± 10 (48–87) | 69 ± 9 (54–84) | 0.538 |
| Body mass index (kg/m2) a | 22 ± 2 (17–29) | 23 ± 1 (20–28) | 0.217 |
| Sports and activity (n, low:high) | 13:40 | 9:31 | 0.736 |
| Operated Knees | Non-Operated Knees | |||||
|---|---|---|---|---|---|---|
| Pre-OP | Post-OP 1 Year | p Value | Pre-OP | Post-OP 1 Year | p Value | |
| Gastrocnemius strength | 21 ± 13.9 | 77 ± 22.9 | <0.001a | 72 ± 22.2 | 78 ± 22.6 | 0.635 |
| Soleus strength | 41 ± 10.9 | 54 ± 15.9 | <0.001a | 50 ± 18.7 | 49 ± 15.0 | 0.866 |
| Quadriceps strengths | 98 ± 55.1 | 159 ± 63.7 | <0.001a | 198 ± 67.7 | 214 ± 54.1 | 0.245 |
| Hamstring strengths | 49 ± 36.4 | 80 ± 31.3 | 0.001 a | 90 ± 29.5 | 100 ± 25.9 | 0.112 |
| Gastrocnemius AT | 24 ± 10.8 | 26 ± 9.8 | 0.635 | 31 ± 11.3 | 29 ± 10.4 | 0.500 |
| Soleus AT | 22 ± 8.7 | 18 ± 6.7 | 0.070 | 23 ± 10.1 | 20 ± 7.1 | 0.244 |
| Quadriceps AT | 94 ± 76.6 | 63 ± 17.6 | 0.044 a | 61 ± 15.0 | 66 ± 54.9 | 0.555 |
| Hamstrings AT | 89 ± 39.1 | 72 ± 18 | 0.027 a | 69 ± 16.1 | 81 ± 75.2 | 0.355 |
| Operated Knees | Non-Operated Knees | |||||
|---|---|---|---|---|---|---|
| ACL Reconstruction | Normal Control | p Value | ACL Reconstruction | Normal Control | p Value | |
| Gastrocnemius strength | 77 ± 22.9 | 81 ± 22.5 | 0.425 | 78 ± 22.6 | 81 ± 23.1 | 0.649 |
| Soleus strength | 54 ± 15.9 | 47 ± 16.1 | 0.109 | 49 ± 15.0 | 49 ± 15.9 | 0.967 |
| Quadriceps strength | 159 ± 63.7 | 238 ± 35.3 | <0.001a | 214 ± 54.1 | 247 ± 26.4 | 0.001 a |
| Hamstrings strength | 80 ± 31.3 | 142 ± 26.4 | <0.001a | 100 ± 25.9 | 168 ± 26.6 | 0.001 a |
| Gastrocnemius AT | 26 ± 9.8 | 31 ± 9 | 0.030 a | 29 ± 10.4 | 31 ± 7.3 | 0.273 |
| Soleus AT | 18 ± 6.7 | 22 ± 8.5 | 0.026 a | 20 ± 7.1 | 22 ± 8.6 | 0.109 |
| Quadriceps AT | 63 ± 17.6 | 47 ± 17 | <0.001a | 66 ± 54.9 | 42 ± 16 | 0.017 |
| Hamstrings AT | 72 ± 18 | 55 ± 12.4 | <0.001a | 81 ± 75.2 | 52 ± 15.8 | 0.033 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rhim, H.C.; Lee, J.H.; Han, S.-B.; Shin, K.-H.; Suh, D.W.; Jang, K.-M. Role of the Triceps Surae Muscles in Patients Undergoing Anterior Cruciate Ligament Reconstruction: A Matched Case-Control Study. J. Clin. Med. 2020, 9, 3215. https://doi.org/10.3390/jcm9103215
Rhim HC, Lee JH, Han S-B, Shin K-H, Suh DW, Jang K-M. Role of the Triceps Surae Muscles in Patients Undergoing Anterior Cruciate Ligament Reconstruction: A Matched Case-Control Study. Journal of Clinical Medicine. 2020; 9(10):3215. https://doi.org/10.3390/jcm9103215
Chicago/Turabian StyleRhim, Hye Chang, Jin Hyuck Lee, Seung-Beom Han, Kyun-Ho Shin, Dong Won Suh, and Ki-Mo Jang. 2020. "Role of the Triceps Surae Muscles in Patients Undergoing Anterior Cruciate Ligament Reconstruction: A Matched Case-Control Study" Journal of Clinical Medicine 9, no. 10: 3215. https://doi.org/10.3390/jcm9103215
APA StyleRhim, H. C., Lee, J. H., Han, S. -B., Shin, K. -H., Suh, D. W., & Jang, K. -M. (2020). Role of the Triceps Surae Muscles in Patients Undergoing Anterior Cruciate Ligament Reconstruction: A Matched Case-Control Study. Journal of Clinical Medicine, 9(10), 3215. https://doi.org/10.3390/jcm9103215








