The Use of Diaphragm Ultrasonography in Pulmonary Physiotherapy of COPD Patients: A Literature Review
Abstract
:1. Introduction
2. Materials and Methods
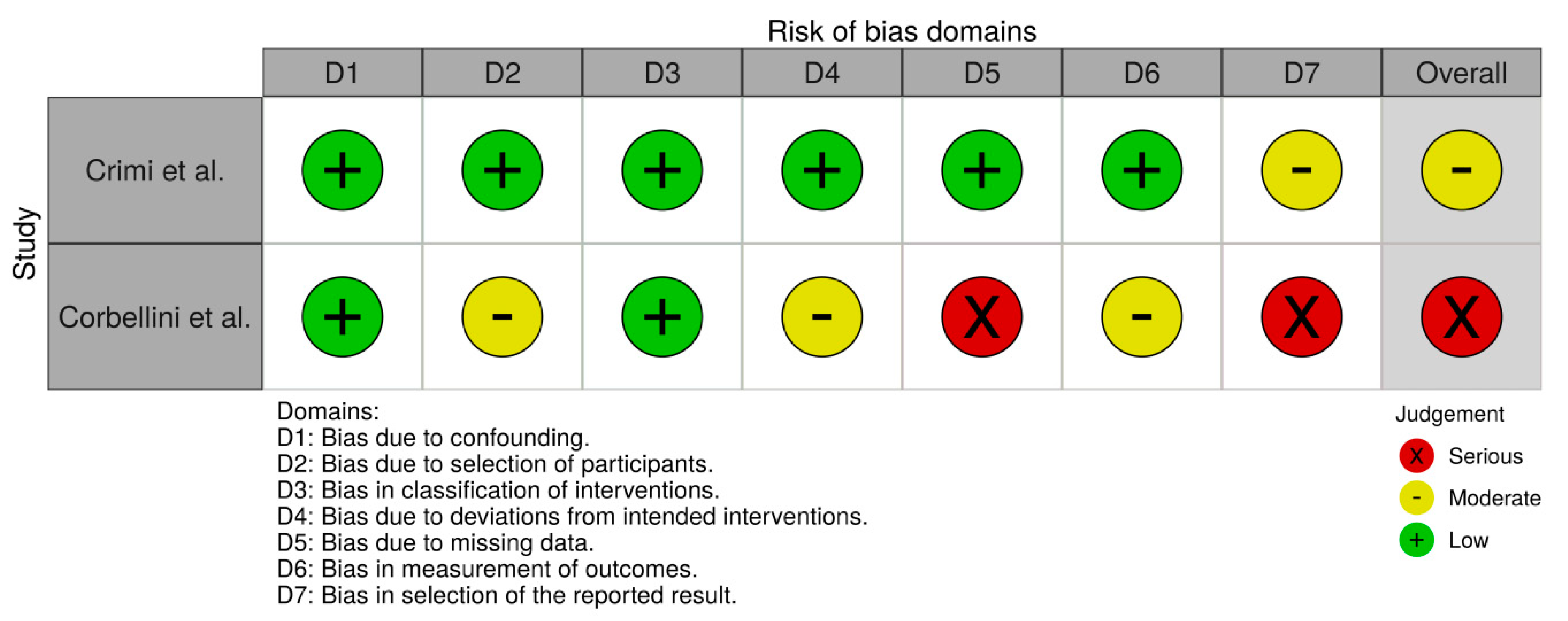
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. Search Strategies
- physiotherap*.ti,ab.
- rehabilitat*.ti,ab.
- “physical therapy”.ti,ab.
- “manual therapy”.ti,ab.
- “kinesio* taping”.ti,ab.
- “exercise training”.ti,ab.
- “respiratory muscle training”.ti,ab.
- 1 or 2 or 3 or 4 or 5 or 6
- diaphragm.ti,ab.
- copd.ti,ab.
- “chronic obstructive pulmonary disease”.ti,ab.
- “obstructive lung disease”.ti,ab.
- 10 or 11 or 12
- ultrasonograph*.ti,ab.
- ultrasound.ti,ab.
- ultrason*.ti,ab.
- 14 or 15 or 16
- 8 and 9 and 13 and 17
- physiotherap*.ti,ab.
- rehabilitat*.ti,ab.
- “physical therapy”.ti,ab.
- “manual therapy”.ti,ab.
- “kinesio* taping”.ti,ab.
- “exercise training”.ti,ab.
- “respiratory muscle training”.ti,ab.
- 1 or 2 or 3 or 4 or 5 or 6
- diaphragm.ti,ab.
- copd.ti,ab.
- “chronic obstructive pulmonary disease”.ti,ab.
- “obstructive lung disease”.ti,ab.
- 10 or 11 or 12
- ultrasonograph*.ti,ab.
- ultrasound.ti,ab.
- ultrason*.ti,ab.
- 14 or 15 or 16
- 8 and 9 and 13 and 17
- Abstract & Title: Diaphragm
- Therapy: respiratory therapy
- When Searching: AND
- #1.
- physiotherap* or rehabilitat* or physical therapy or manual therapy or kinesio* taping or exercise training or respiratory muscle training
- #2.
- diaphragm
- #3.
- copd or chronic obstructive pulmonary disease or obstructive lung disease
- #4.
- ultrasonograph* or ultrasound or ultrason*
- #5.
- #1 and #2 and #3 and #4
References
- Dos Santos Yamaguti, W.P.; Paulin, E.; Shibao, S.; Chammas, M.C.; Salge, J.M.; Ribeiro, M.; Cukier, A.; Carvalho, C.R. Air trapping: The major factor limiting diaphragm mobility in chronic obstructive pulmonary disease patients. Respirology 2008, 13, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Rocha, F.R.; Brüggemann, A.K.; Francisco, D.S.; Medeiros, C.S.; Rosal, D.; Paulin, E. Diaphragmatic mobility: Relationship with lung function, respiratory muscle strength, dyspnea, and physical activity in daily life in patients with COPD. J. Bras. Pneumol. 2017, 43, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Souza, H.; Rocha, T.; Pessoa, M.; Rattes, C.; Brandão, D.; Fregonezi, G.; Campos, S.; Aliverti, A.; Dornelas, A. Effects of inspiratory muscle training in elderly women on respiratory muscle strength, diaphragm thickness and mobility. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2014, 69, 1545–1553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vieira Ramos, G.; Choqueta de Toledo-Arruda, A.; Maria Pinheiro-Dardis, C.; Liyoko Suehiro, C.; Luiz de Russo, T.; Vieira, R.P.; Arruda Martins, M.; Salvini, T.F.; Durigan, J.L.Q. Exercise Prevents Diaphragm Wasting Induced by Cigarette Smoke through Modulation of Antioxidant Genes and Metalloproteinases. BioMed Res. Int. 2018, 2018, 5909053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mangner, N.; Bowen, T.S.; Werner, S.; Fischer, T.; Kullnick, Y.; Oberbach, A.; Linke, A.; Steil, L.; Schuler, G.; Adams, V. Exercise Training Prevents Diaphragm Contractile Dysfunction in Heart Failure. Med. Sci. Sports Exerc. 2016, 48, 2118–2124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polastri, M.; Venturini, E.; Pastore, S.; Dell’Amore, A. Do Chest Expansion Exercises Aid Re-shaping the Diaphragm Within the First 72 Hours Following Lung Transplantation in a Usual Interstitial Pneumonia Patient? Physiother. Res. Int. J. Res. Clin. Phys. Ther. 2015, 20, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Shang, W.; Wang, Z.; Liu, X.; Fang, X.; Ke, M. Short-term and long-term effect of diaphragm biofeedback training in gastroesophageal reflux disease: An open-label, pilot, randomized trial. Dis. Esophagus J. Int. Soc. Dis. Esophagus 2016, 29, 829–836. [Google Scholar] [CrossRef] [PubMed]
- Rocha, T.; Muniz, H.; Drandao, D.; Campos, S.; Aliverti, A.; De Andrade, A.D. Effects of diaphragm release manual technique on diaphragm mobility, chest Wall kinematics and functional exercise capacity of COPD patients. Eur. Respir. J. 2013, 42, 3165. [Google Scholar]
- Wang, J.S.; Cho, K.H.; Park, S.J. The immediate effect of diaphragm taping with breathing exercise on muscle tone and stiffness of respiratory muscles and SpO(2) in stroke patient. J. Phys. Ther. Sci. 2017, 29, 970–973. [Google Scholar] [CrossRef] [Green Version]
- Bataille, B.; Nucci, B.; De Selle, J.; Mora, M.; Moussot, P.E.; Cocquet, P.; Silva, S. Paravertebral block restore diaphragmatic motility measured by ultrasonography in patients with multiple rib fractures. J. Clin. Anesth. 2017, 42, 55–56. [Google Scholar] [CrossRef]
- Kharma, N. Dysfunction of the diaphragm: Imaging as a diagnostic tool. Curr. Opin. Pulm. Med. 2013, 19, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Bordoni, B.; Morabito, B. The Diaphragm Muscle Manual Evaluation Scale. Cureus 2019, 11, e4569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schepens, T.; Fard, S.; Goligher, E.C. Assessing Diaphragmatic Function. Respir. Care 2020, 65, 807–819. [Google Scholar] [CrossRef]
- Tuinman, P.R.; Jonkman, A.H.; Dres, M.; Shi, Z.-H.; Goligher, E.C.; Goffi, A.; de Korte, C.; Demoule, A.; Heunks, L. Respiratory muscle ultrasonography: Methodology, basic and advanced principles and clinical applications in ICU and ED patients—a narrative review. Intensive Care Med. 2020, 46, 594–605. [Google Scholar] [CrossRef] [Green Version]
- Boussuges, A.; Rives, S.; Finance, J.; Brégeon, F. Assessment of diaphragmatic function by ultrasonography: Current approach and perspectives. World J. Clin. Cases 2020, 8, 2408–2424. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [Green Version]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2020. [Google Scholar] [CrossRef]
- Marques, A.; Jácome, C.; Rebelo, P.; Paixão, C.; Oliveira, A.; Cruz, J.; Freitas, C.; Rua, M.; Loureiro, H.; Peguinho, C.; et al. Improving access to community-based pulmonary rehabilitation: 3R protocol for real-world settings with cost-benefit analysis. BMC Public Health 2019, 19, 676. [Google Scholar] [CrossRef] [Green Version]
- Nair, A.; Alaparthi, G.K.; Krishnan, S.; Rai, S.; Anand, R.; Acharya, V.; Acharya, P. Comparison of Diaphragmatic Stretch Technique and Manual Diaphragm Release Technique on Diaphragmatic Excursion in Chronic Obstructive Pulmonary Disease: A Randomized Crossover Trial. Pulm. Med. 2019, 2019, 6364376. [Google Scholar] [CrossRef]
- Crimi, C.; Heffler, E.; Augelletti, T.; Campisi, R.; Noto, A.; Vancheri, C.; Crimi, N. Utility of ultrasound assessment of diaphragmatic function before and after pulmonary rehabilitation in COPD patients. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 3131–3139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corbellini, C.; Boussuges, A.; Villafañe, J.H.; Zocchi, L. Diaphragmatic Mobility Loss in Subjects With Moderate to Very Severe COPD May Improve After In-Patient Pulmonary Rehabilitation. Respir. Care 2018, 63, 1271–1280. [Google Scholar] [CrossRef] [Green Version]
- Rocha, T.; Souza, H.; Brandão, D.C.; Rattes, C.; Ribeiro, L.; Campos, S.L.; Aliverti, A.; de Andrade, A.D. The Manual Diaphragm Release Technique improves diaphragmatic mobility, inspiratory capacity and exercise capacity in people with chronic obstructive pulmonary disease: A randomised trial. J. Physiother. 2015, 61, 182–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhatt, S.P.; Luqman-Arafath, T.K.; Gupta, A.K.; Mohan, A.; Stoltzfus, J.C.; Dey, T.; Nanda, S.; Guleria, R. Volitional pursed lips breathing in patients with stable chronic obstructive pulmonary disease improves exercise capacity. Chron. Respir. Dis. 2013, 10, 5–10. [Google Scholar] [CrossRef] [Green Version]
- Yamaguti, W.P.; Claudino, R.C.; Neto, A.P.; Chammas, M.C.; Gomes, A.C.; Salge, J.M.; Moriya, H.T.; Cukier, A.; Carvalho, C.R. Diaphragmatic breathing training program improves abdominal motion during natural breathing in patients with chronic obstructive pulmonary disease: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2012, 93, 571–577. [Google Scholar] [CrossRef] [PubMed]
- Zanforlin, A.; Smargiassi, A.; Inchingolo, R.; Valente, S.; Ramazzina, E. Ultrasound in obstructive lung diseases: The effect of airway obstruction on diaphragm kinetics. A short pictorial essay. J. Ultrasound 2015, 18, 379–384. [Google Scholar] [CrossRef] [Green Version]
- Toledo, N.S.; Kodaira, S.K.; Massarollo, P.C.; Pereira, O.I.; Mies, S. Right hemidiaphragmatic mobility: Assessment with US measurement of craniocaudal displacement of left branches of portal vein. Radiology 2003, 228, 389–394. [Google Scholar] [CrossRef]
- Paulin, E.; Yamaguti, W.P.; Chammas, M.C.; Shibao, S.; Stelmach, R.; Cukier, A.; Carvalho, C.R. Influence of diaphragmatic mobility on exercise tolerance and dyspnea in patients with COPD. Respir. Med. 2007, 101, 2113–2118. [Google Scholar] [CrossRef] [Green Version]
- Houston, J.G.; Angus, R.M.; Cowan, M.D.; McMillan, N.C.; Thomson, N.C. Ultrasound assessment of normal hemidiaphragmatic movement: Relation to inspiratory volume. Thorax 1994, 49, 500–503. [Google Scholar] [CrossRef] [Green Version]
- Okura, K.; Kawagoshi, A.; Iwakura, M.; Sugawara, K.; Takahashi, H.; Kashiwagura, T.; Homma, M.; Satake, M.; Shioya, T. Contractile capability of the diaphragm assessed by ultrasonography predicts nocturnal oxygen saturation in COPD. Respirology 2017, 22, 301–306. [Google Scholar] [CrossRef]
- Testa, A.; Soldati, G.; Giannuzzi, R.; Berardi, S.; Portale, G.; Gentiloni Silveri, N. Ultrasound M-mode assessment of diaphragmatic kinetics by anterior transverse scanning in healthy subjects. Ultrasound Med. Biol. 2011, 37, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.; Tseng, S.-C.; Mitchell, K.; Roddey, T. Body Position Affects Ultrasonographic Measurement of Diaphragm Contractility. Cardiopulm Phys. J. 2018, 29, 166–172. [Google Scholar] [CrossRef]
- Vetrugno, L.; Guadagnin, G.M.; Barbariol, F.; Langiano, N.; Zangrillo, A.; Bove, T. Ultrasound Imaging for Diaphragm Dysfunction: A Narrative Literature Review. J. Cardiothorac. Vasc. Anesth. 2019, 33, 2525–2536. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.I.; Jeong, D.K.; Choi, H. Correlation between diaphragm thickness and respiratory synergist muscle activity according to severity of chronic obstructive pulmonary disease. J. Phys. Ther. Sci. 2018, 30, 150–153. [Google Scholar] [CrossRef] [Green Version]
- Ubolnuar, N.; Tantisuwat, A.; Thaveeratitham, P.; Lertmaharit, S.; Kruapanich, C.; Mathiyakom, W. Effects of Breathing Exercises in Patients With Chronic Obstructive Pulmonary Disease: Systematic Review and Meta-Analysis. Ann. Rehabil. Med. 2019, 43, 509–523. [Google Scholar] [CrossRef]
- Zhang, X.; Yuan, J.; Zhan, Y.; Wu, J.; Liu, B.; Zhang, P.; Yu, T.; Wang, Z.; Jiang, X.; Lu, W. Evaluation of diaphragm ultrasound in predicting extubation outcome in mechanically ventilated patients with COPD. Ir. J. Med. Sci. 2020, 189, 661–668. [Google Scholar] [CrossRef] [PubMed]
- Goligher, E.C.; Dres, M.; Fan, E.; Rubenfeld, G.D.; Scales, D.C.; Herridge, M.S.; Vorona, S.; Sklar, M.C.; Rittayamai, N.; Lanys, A.; et al. Mechanical Ventilation–induced Diaphragm Atrophy Strongly Impacts Clinical Outcomes. Am. J. Respir. Crit. Care Med. 2017, 197, 204–213. [Google Scholar] [CrossRef]
- Bissett, B.; Gosselink, R.; van Haren, F.M.P. Respiratory Muscle Rehabilitation in Patients with Prolonged Mechanical Ventilation: A Targeted Approach. Crit. Care 2020, 24, 103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wormser, J.; Lebret, M.; Le Neindre, A. Diaphragm ultrasonography: Principles and applications ain physiotherapy. Kinesitherapie 2017, 17, 62–70. [Google Scholar] [CrossRef]
- See, K.; Ong, V.; Wong, S.; Leanda, R.; Santos, J.; Taculod, J.; Phua, J.; Teoh, C. Lung ultrasound training: Curriculum implementation and learning trajectory among respiratory therapists. Intensive Care Med. 2015, 42. [Google Scholar] [CrossRef]
- Khurana, J.; Gartner, S.; Naik, L.; Tsui, C.-H. Ultrasound Identification of Diaphragm by Novices Using ABCDE Technique. Reg. Anesth. Pain Med. 2018, 43, 161–165. [Google Scholar] [CrossRef]
- Østergaard, M.; Nielsen, K.; Albrecht-Beste, E.; Konge, L.; Nielsen, M.B. Development of a reliable simulation-based test for diagnostic abdominal ultrasound with a pass/fail standard usable for mastery learning. Eur. Radiol. 2017, 28. [Google Scholar] [CrossRef]
- O’Hara, D.N.; Pavlov, A.; Taub, E.; Ahmad, S. Ultrasonographic modeling of diaphragm function: A novel approach to respiratory assessment. PLoS ONE 2020, 15, e0229972. [Google Scholar] [CrossRef]
- Le Neindre, A.; Mongodi, S.; Philippart, F.; Bouhemad, B. Thoracic ultrasound: Potential new tool for physiotherapists in respiratory management. A narrative review. J. Crit. Care 2016, 31, 101–109. [Google Scholar] [CrossRef]
- Hayward, S.A.; Janssen, J. Use of thoracic ultrasound by physiotherapists: A scoping review of the literature. Physiotherapy 2018, 104, 367–375. [Google Scholar] [CrossRef] [PubMed]



| Author, Year | Study Design | Objective | Intervention | Participants | Techniques | Outcome Measure | Measure Details |
|---|---|---|---|---|---|---|---|
| Marques et al. 2019 [19] | Study protocol | To investigate the short-term effects of community based pulmonary rehabilitation programs | Pulmonary rehabilitation; 12-week | Recruited: 102 | Comprehensive program | Thickness, cross sectional area, echointensity, and excursion | Not specified |
| Nair et al. 2019 [20] | Randomized crossover trial | To compare the effects of Diaphragmatic Stretch and Diaphragm Release techniques | Manual therapy; single-session | Recruited: 20 Completed: 20 | Diaphragmatic Stretch Technique, Diaphragm Release Technique | Excursion |
|
| Crimi et al. 2018 [21] | Prospective observational study | To evaluate the changes in ultrasound measurements of diaphragmatic mobility and thickness | Exercise training; 12-week | Recruited: 37 Completed: 25 | Endurance and strength training | Excursion; Thickness |
|
| Corbelini et al. 2018 [22] | Prospective observational study | To verify diaphragmatic mobility improvement after in-patient pulmonary rehabilitation program and correlate the mobility loss to COPD severity | Pulmonary rehabilitation; 31 ± 8 days | Recruited: 46 Completed: 30 | Comprehensive program | Excursion |
|
| Rocha et al. 2015 [23] | Randomized controlled trial | To verify if the Manual Diaphragm Release Technique improve diaphragmatic mobility after a single treatment, or multiple sessions | Manual therapy; 2-week | Recruited: 20 Completed: 19 | Diaphragm Release Technique | Excursion |
|
| Bhatt et al. 2012 [24] | Randomized crossover study | To determine the effects of volitional Pursed Lips Breathing Technique on exercise capacity | Breathing exercise; single-session | Recruited: 14 Completed: 14 | Pursed Lips Breathing | Excursion |
|
| Yamaguti et al. 2012 [25] | Randomized controlled trial | To investigate the effects of Diaphragmatic Breathing technique on thoraco-abdominal motion and functional capacity | Breathing exercise; 4-week | Recruited: 30 Completed: 30 | Diaphragmatic Breathing | Excursion |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewińska, A.; Shahnazaryan, K. The Use of Diaphragm Ultrasonography in Pulmonary Physiotherapy of COPD Patients: A Literature Review. J. Clin. Med. 2020, 9, 3525. https://doi.org/10.3390/jcm9113525
Lewińska A, Shahnazaryan K. The Use of Diaphragm Ultrasonography in Pulmonary Physiotherapy of COPD Patients: A Literature Review. Journal of Clinical Medicine. 2020; 9(11):3525. https://doi.org/10.3390/jcm9113525
Chicago/Turabian StyleLewińska, Agnieszka, and Karen Shahnazaryan. 2020. "The Use of Diaphragm Ultrasonography in Pulmonary Physiotherapy of COPD Patients: A Literature Review" Journal of Clinical Medicine 9, no. 11: 3525. https://doi.org/10.3390/jcm9113525





