The Role of Foot-Loading Factors and Their Associations with Ulcer Development and Ulcer Healing in People with Diabetes: A Systematic Review
Abstract
1. Introduction
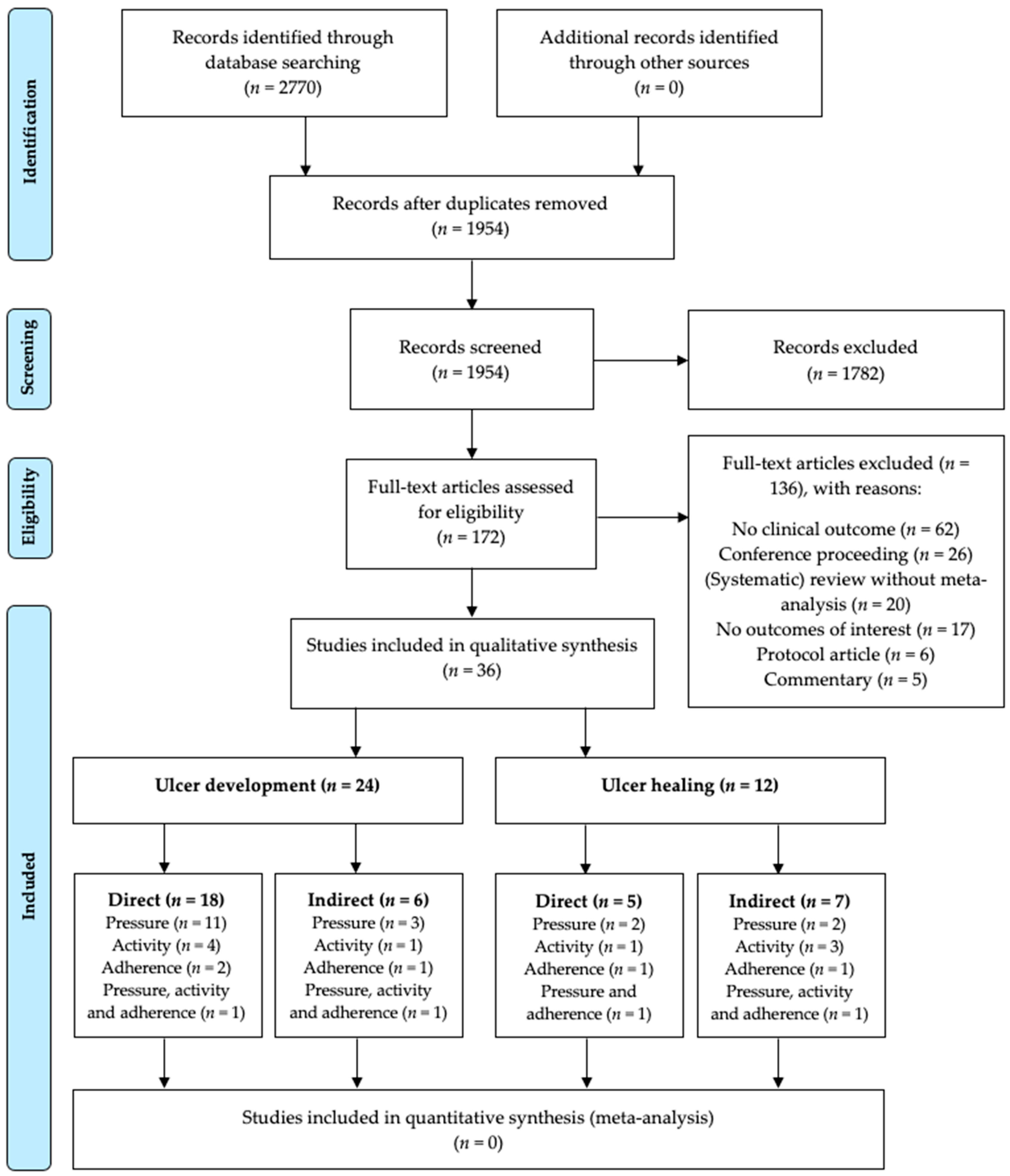
2. Methods
2.1. Population Characteristics
2.2. Factors
- Plantar pressure, consisting of objectively measured barefoot and in-shoe plantar pressure measurements, usually represented as peak plantar pressure or pressure-time integral [16].
- Weight-bearing activity, consisting of objective measurements of weight-bearing activities in daily life, and expressed as daily steps or strides, bouts of activity, duration of bouts and intensity of daily activities.
- Adherence to wearing an offloading modality for ulcer prevention or treatment (e.g., custom-made footwear, walker or cast), assessed either objectively with measurement systems or subjectively via self-report (e.g., logbook or questionnaire), and expressed as percentage or hours of weight-bearing activity duration or of number of steps.
2.3. Outcomes
2.4. Eligibility Criteria
2.5. Search Strategy
2.6. Eligibility Assessment
2.7. Risk of Bias Assessment
2.8. Data Extraction
2.9. Evidence Statement
3. Results
3.1. Ulcer Development
3.1.1. Plantar Pressure
3.1.2. Weight-Bearing Activity
3.1.3. Footwear Adherence
3.1.4. Cumulative Plantar Tissue Stress
3.2. Ulcer Healing
3.2.1. Plantar Pressure
3.2.2. Weight-Bearing Activity
3.2.3. Device Adherence
3.2.4. Cumulative Plantar Tissue Stress
4. Discussion
4.1. Evidences for Underlying Foot-Loading Factors for Ulcer Outcomes
4.1.1. Ulcer Development
4.1.2. Ulcer Healing
4.1.3. Limitations in Associations Found
4.2. Strengths and Limitations of Included Studies
4.3. Cumulative Plantar Tissue Stress
4.4. Alternative Approaches on Understanding the Foot-Loading Pathways of Ulcer Outcomes
4.5. Methodological Reflection
4.6. Implications for Clinical Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Armstrong, D.G.; Boulton, A.J.M.; Bus, S.A. Diabetic foot ulcers and their recurrence. N. Engl. J. Med. 2017, 376, 2367–2375. [Google Scholar] [CrossRef]
- Zhang, Y.; Lazzarini, P.A.; Mcphail, S.M.; Van Netten, J.J.; Armstrong, D.G.; Pacella, R.E. Global Disability Burdens of Extremity Complications in 1990 and 2016. Diabetes Care 2020, 43, 964–974. [Google Scholar] [CrossRef]
- Boulton, A.J.M.; Vileikyte, L.; Ragnarson-Tennvall, G.; Apelqvist, J. The global burden of diabetic foot disease. Lancet 2005, 366, 1719–1724. [Google Scholar] [CrossRef]
- Raghav, A.; Khan, Z.A.; Labala, R.K.; Ahmad, J.; Noor, S.; Mishra, B.K. Financial burden of diabetic foot ulcers to world: A progressive topic to discuss always. Ther. Adv. Endocrinol. Metab. 2018, 9, 29–31. [Google Scholar] [CrossRef] [PubMed]
- Lavery, L.A.; Armstrong, D.G.; Wunderlich, R.P.; Mohler, M.J.; Wendel, C.S.; Lipsky, B.A. Risk factors for foot infections in individuals with diabetes. Diabetes Care 2006, 29, 1288–1293. [Google Scholar] [CrossRef] [PubMed]
- Van Schie, C.H.M. A review of the biomechanics of the diabetic foot. Int. J. Low. Extrem. Wounds 2005, 4, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Chatwin, K.E.; Abbott, C.A.; Boulton, A.J.M.; Bowling, F.L.; Reeves, N.D. The role of foot pressure measurement in the prediction and prevention of diabetic foot ulceration—A comprehensive review. Diabetes Metab. Res. Rev. 2019, 36, 1–14. [Google Scholar] [CrossRef]
- Cavanagh, P.R.; Bus, S.A. Off-loading the diabetic foot for ulcer prevention and healing. J. Vasc. Surg. 2010, 52, 37S–43S. [Google Scholar] [CrossRef]
- Lazzarini, P.A.; Crews, R.T.; van Netten, J.J.; Bus, S.A.; Fernando, M.E.; Chadwick, P.J.; Najafi, B. Measuring Plantar Tissue Stress in People With Diabetic Peripheral Neuropathy: A Critical Concept in Diabetic Foot Management. J. Diabetes Sci. Technol. 2019, 13, 869–880. [Google Scholar] [CrossRef] [PubMed]
- Arts, M.L.J.; Waaijman, R.; de Haart, M.; Keukenkamp, R.; Nollet, F.; Bus, S.A. Offloading effect of therapeutic footwear in patients with diabetic neuropathy at high risk for plantar foot ulceration. Diabet. Med. 2012, 29, 1534–1541. [Google Scholar] [CrossRef]
- Maluf, K.S.; Mueller, M.J. Comparison of physical activity and cumulative plantar tissue stress among subjects with and without diabetes mellitus and a history of recurrent plantar ulcers. Clin. Biomech. 2003, 18, 567–575. [Google Scholar] [CrossRef]
- Waaijman, R.; De Haart, M.; Arts, M.L.J.; Wever, D.; Verlouw, A.J.W.E.; Nollet, F.; Bus, S.A. Risk factors for plantar foot ulcer recurrence in neuropathic diabetic patients. Diabetes Care 2014, 37, 1697–1705. [Google Scholar] [CrossRef] [PubMed]
- van Netten, J.J.; van Baal, J.G.; Bril, A.; Wissink, M.; Bus, S.A. An exploratory study on differences in cumulative plantar tissue stress between healing and non-healing plantar neuropathic diabetic foot ulcers. Clin. Biomech. 2018, 53, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Schaper, N.C.; van Netten, J.J.; Apelqvist, J.; Bus, S.A.; Hinchliffe, R.J.; Lipsky, B.A. Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab. Res. Rev. 2020, 36, e3266. [Google Scholar] [CrossRef]
- van Netten, J.J.; Bus, S.A.; Apelqvist, J.; Lipsky, B.A.; Hinchliffe, R.J.; Game, F.; Rayman, G.; Lazzarini, P.A.; Forsythe, R.O.; Peters, E.J.G.; et al. Definitions and criteria for diabetic foot disease. Diabetes Metab. Res. Rev. 2020, 36, e3268. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Hayden, J.A.; van der Windt, D.A.; Cartwright, J.L.; Côté, P.; Bombardier, C. Assessing bias in studies of prognostic factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef]
- Jeffcoate, W.J.; Bus, S.A.; Game, F.L.; Hinchliffe, R.J.; Price, P.E.; Schaper, N.C. Reporting standards of studies and papers on the prevention and management of foot ulcers in diabetes: Required details and markers of good quality. Lancet Diabetes Endocrinol. 2016, 4, 781–788. [Google Scholar] [CrossRef]
- Harbour, R.; Miller, J. A new system for grading recommendations in evidence based guidelines. Br. Med. J. 2001, 323, 334–336. [Google Scholar] [CrossRef] [PubMed]
- Pham, H.; Armstrong, D.G.; Harvey, C.; Harkless, L.B.; Giurini, J.M.; Veves, A. Screening techniques to identify people at high risk for diabetic foot ulceration: A prospective multicenter trial. Diabetes Care 2000, 23, 606–611. [Google Scholar] [CrossRef]
- Caselli, A.; Pham, H.; Giurini, J.M.; Armstrong, D.G.; Veves, A. The forefoot-to-rearfoot plantar pressure ratio is increased in severe diabetic neuropathy and can predict foot ulceration. Diabetes Care 2002, 25, 1066–1071. [Google Scholar] [CrossRef]
- Lavery, L.A.; Armstrong, D.G.; Wunderlich, R.P.; Tredwell, J.; Boulton, A.J.M. Predictive value of foot pressure assessment as part of a population based diabetes disease management program. Diabetes Care 2003, 26, 1069–1073. [Google Scholar] [CrossRef] [PubMed]
- Kästenbauer, T.; Sauseng, S.; Sokol, G.; Auinger, M.; Irsigler, K. A prospective study of predictors for foot ulceration in type 2 diabetes. J. Am. Podiatr. Med. Assoc. 2001, 91, 343–350. [Google Scholar] [CrossRef]
- Grimm, A.; Kastenbauer, T.; Sauseng, S.; Sokol, G.; Irsigler, K. Progression and distribution of plantar pressure in Type 2 diabetic patients. Diabetes Nutr. Metab. 2004, 17, 108–113. [Google Scholar]
- Ulbrecht, J.S.; Hurley, T.; Mauger, D.T.; Cavanagh, P.R. Prevention of recurrent foot ulcers with plantar pressure-based in-shoe orthoses: The CareFUL prevention multicenter randomized controlled trial. Diabetes Care 2014, 37, 1982–1989. [Google Scholar] [CrossRef]
- Deschamps, K.; Matricali, G.A.; Desmet, D.; Roosen, P.; Keijsers, N.; Nobels, F.; Bruyninckx, H.; Staes, F. Efficacy measures associated to a plantar pressure based classification system in diabetic foot medicine. Gait Posture 2016, 49, 168–175. [Google Scholar] [CrossRef]
- Murray, H.J.; Young, M.J.; Hollis, S.; Boulton, A.J.M. The Association Between Callus Formation, High Pressures and Neuropathy in Diabetic Foot Ulceration. Diabet. Med. 1996, 13, 979–982. [Google Scholar] [CrossRef]
- Qiu, X.; Tian, D.H.; Han, C.L.; Chen, W.; Wang, Z.J.; Mu, Z.Y.; Liu, K.Z. Plantar pressure changes and correlating risk factors in Chinese patients with type 2 diabetes: Preliminary 2‑year results of a prospective study. Chin. Med. J. Engl. 2015, 128, 3283–3291. [Google Scholar] [CrossRef] [PubMed]
- Crawford, F.; Inkster, M.; Kleijnen, J.; Fahey, T. Predicting foot ulcers in patients with diabetes: A systematic review and meta-analysis. Q. J. Med. 2007, 100, 65–86. [Google Scholar] [CrossRef]
- Ledoux, W.R.; Shofer, J.B.; Cowly, M.S.; Ahroni, J.H.; Cohen, V.; Boyko, E.J. Diabetic foot ulcer incidence in relation to plantar pressure magnitude and measurement location. J. Diabetes Complicat. 2013, 27, 621–626. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Lavery, L.A.; Holtz-Neiderer, K.; Mohler, M.J.; Wendel, C.S.; Nixon, B.P.; Boulton, A.J.M.M. Variability in Activity May Precede Diabetic Foot Ulceration. Diabetes Care 2004, 27, 1980–1984. [Google Scholar] [CrossRef]
- Lemaster, J.W.; Reiber, G.E.; Smith, D.G.; Heagerty, P.J.; Wallace, C. Daily weight-bearing activity does not increase the risk of diabetic foot ulcers. Med. Sci. Sports Exerc. 2003, 35, 1093–1099. [Google Scholar] [CrossRef]
- Mueller, M.J.; Tuttle, L.J.; Lemaster, J.W.; Strube, M.J.; McGill, J.B.; Hastings, M.K.; Sinacore, D.R. Weight-bearing versus nonweight-bearing exercise for persons with diabetes and peripheral neuropathy: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2013, 94, 829–838. [Google Scholar] [CrossRef]
- Schneider, K.L.; Crews, R.T.; Subramanian, V.; Moxley, E.; Hwang, S.; DiLiberto, F.E.; Aylward, L.; Bean, J.; Yalla, S. Feasibility of a Low-Intensity, Technology-Based Intervention for Increasing Physical Activity in Adults at Risk for a Diabetic Foot Ulcer: A Mixed-Methods Study. J. Diabetes Sci. Technol. 2019, 13, 857–868. [Google Scholar] [CrossRef]
- Chantelau, E.; Haage, P. An Audit of Cushioned Diabetic Footwear: Relation to Patient Compliance. Diabet. Med. 1994, 11, 114–116. [Google Scholar] [CrossRef]
- Connor, H.; Mahdi, O.Z. Repetitive ulceration in neuropathic patients. Diabetes Metab. Res. Rev. 2004, 20, 23–28. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Lavery, L.A.; Bushman, T.R. Peak foot pressures influence the healing time of diabetic foot ulcers treated with total contact casts. J. Rehabil. Res. Dev. 1998, 35, 1–5. [Google Scholar] [PubMed]
- Jarl, G.; Tranberg, R. An innovative sealed shoe to off-load and heal diabetic forefoot ulcers–a feasibility study. Diabet. Foot Ankle 2017, 8, 1348178. [Google Scholar] [CrossRef]
- Najafi, B.; Grewal, G.S.; Bharara, M.; Menzies, R.; Talal, T.K.; Armstrong, D.G. Can’t Stand the Pressure: The Association between Unprotected Standing, Walking, and Wound Healing in People with Diabetes. J. Diabetes Sci. Technol. 2017, 11, 657–667. [Google Scholar] [CrossRef]
- Crews, R.T.; Shen, B.J.; Campbell, L.; Lamont, P.J.; Boulton, A.J.M.; Peyrot, M.; Kirsner, R.S.; Vileikyte, L. Role and determinants of Adherence to off-loading in diabetic foot ulcer healing: A prospective investigation. Diabetes Care 2016, 39, 1371–1377. [Google Scholar] [CrossRef]
- Veves, A.; Murray, H.J.; Young, M.J.; Boulton, A.J.M. The risk of foot ulceration in diabetic patients with high foot pressure: A prospective study. Diabetologia 1992, 35, 660–663. [Google Scholar] [CrossRef]
- Bus, S.A.; Waaijman, R.; Arts, M.; De Haart, M.; Busch-Westbroek, T.; Van Baal, J.; Nollet, F. Effect of custom-made footwear on foot ulcer recurrence in diabetes: A multicenter randomized controlled trial. Diabetes Care 2013, 36, 4109–4116. [Google Scholar] [CrossRef]
- Viswanathan, V.; Madhavan, S.; Gnanasundaram, S.; Gopalakrishna, G.; Nath Das, B.; Rajasekar, S.; Ramachandran, A. Effectiveness of Different Types of Footwear Insoles for the Diabetic Neuropathic Foot: A follow-up study. Diabetes Care 2004, 27, 474–477. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.L.G.; Lozano, R.M.; Diaz, M.I.G.-Q.; Jurado, M.A.G.; Hernandez, D.M.; Montesinos, J.V.B. How Effective Is Orthotic Treatment in Patients with Recurrent Diabetic Foot Ulcers? J. Am. Podiatr. Med. Assoc. 2013, 103, 281–290. [Google Scholar] [CrossRef]
- Lemaster, J.W.; Mueller, M.J.; Reiber, G.E.; Mehr, D.R.; Madsen, R.W.; Conn, V.S. Effect of Weight-Bearing Activity on Foot Ulcer Incidence in People With Diabetic Peripheral Neuropathy: Feet First Randomized Controlled Trial. Phys. Ther. 2008, 88, 1385–1398. [Google Scholar] [CrossRef]
- Lavery, L.A.; Lafontaine, J.; Higgins, K.R.; Lanctot, D.R.; Constantinides, G. Shear-reducing insoles to prevent foot ulceration in high-risk diabetic patients. Adv. Ski. Wound Care 2012, 25, 519–524. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.G.; Wieman, T.J. Effect of metatarsal head resection for diabetic foot ulcers on the dynamic plantar pressure distribution. Am. J. Surg. 1994, 167, 297–301. [Google Scholar] [CrossRef]
- Bus, S.A.; van Netten, J.J.; Kottink, A.I.R.; Manning, E.A.; Spraul, M.; Woittiez, A.J.; van Baal, J.G. The efficacy of removable devices to offload and heal neuropathic plantar forefoot ulcers in people with diabetes: A single-blinded multicentre randomised controlled trial. Int. Wound J. 2018, 15, 65–74. [Google Scholar] [CrossRef]
- Gutekunst, D.J.; Hastings, M.K.; Bohnert, K.L.; Strube, M.J.; Sinacore, D.R. Removable cast walker boots yield greater forefoot off-loading than total contact casts. Clin. Biomech. 2011, 26, 649–654. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Nguyen, H.C.; Lavery, L.A.; Van Schie, C.H.M.; Boulton, A.J.M.; Harkless, L.B. Off-loading the diabetic foot wound: A randomized clinical trial. Diabetes Care 2001, 24, 1019–1022. [Google Scholar] [CrossRef]
- Lavery, L.A.; Higgins, K.R.; La Fontaine, J.; Zamorano, R.G.; Constantinides, G.P.; Kim, P.J. Randomised clinical trial to compare total contact casts, healing sandals and a shear-reducing removable boot to heal diabetic foot ulcers. Int. Wound J. 2015, 12, 710–715. [Google Scholar] [CrossRef] [PubMed]
- Saltzman, C.L.; Zimmerman, M.B.; Holdsworth, R.L.; Beck, S.; Hartsell, H.D.; Frantz, R.A. Effect of initial weight-bearing in a total contact cast on healing of diabetic foot ulcers. J. Bone Jt. Surg. 2004, 86, 2714–2719. [Google Scholar] [CrossRef] [PubMed]
- Ha Van, G.; Siney, H.; Hartmann-Heurtier, A.; Jacqueminet, S.; Greau, F.; Grimaldi, A. Nonremovable, Windowed, Fiberglass Cast Boot in the Treatment of Diabetic Plantar Ulcers. Diabetes Care 2003, 26, 2848–2852. [Google Scholar] [CrossRef][Green Version]
- van Netten, J.J.; Raspovic, A.; Lavery, L.A.; Monteiro-Soares, M.; Rasmussen, A.; Sacco, I.C.N.; Bus, S.A. Prevention of foot ulcers in the at-risk patient with diabetes: A systematic review. Diabetes Metab. Res. Rev. 2020, 1–22. [Google Scholar] [CrossRef]
- Lazzarini, P.A.; Jarl, G.; Gooday, C.; Viswanathan, V.; Caravaggi, C.F.; Armstrong, D.G.; Bus, S.A. Effectiveness of offloading interventions to heal foot ulcers in persons with diabetes: A systematic review. Diabetes Metab. Res. Rev. 2020, 36, 1–28. [Google Scholar] [CrossRef]
- Alahakoon, C.; Fernando, M.; Galappaththy, C.; Matthews, E.O.; Lazzarini, P.; Moxon, J.V.; Golledge, J. Meta-analyses of randomized controlled trials reporting the effect of home foot temperature monitoring, patient education or offloading footwear on the incidence of diabetes-related foot ulcers. Diabet. Med. 2020, 37, 1266–1279. [Google Scholar] [CrossRef]
- Fernando, M.E.; Crowther, R.G.; Lazzarini, P.A.; Yogakanthi, S.; Sangla, K.S.; Buttner, P.; Jones, R.; Golledge, J. Plantar pressures are elevated in people with longstanding diabetes-related foot ulcers during follow-up. PLoS ONE 2017, 12, e0181916. [Google Scholar] [CrossRef]
- van Netten, J.J.; Jannink, M.J.A.; Hijmans, J.M.; Geertzen, J.H.B.; Postema, K. Long-term use of custom-made orthopedic shoes: 1.5-year follow-up study. J. Rehabil. Res. Dev. 2010, 47, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Golledge, J.; Fernando, M.; Lazzarini, P.; Najafi, B.; Armstrong, D.G. The potential role of sensors, wearables and telehealth in the remote management of diabetes-related foot disease. Sensors (Switzerland) 2020, 20, 4527. [Google Scholar] [CrossRef] [PubMed]
- Yavuz, M.; Master, H.; Garrett, A.; Lavery, L.A.; Adams, L.S. Peak plantar shear and pressure and foot ulcer locations: A call to revisit ulceration pathomechanics. Diabetes Care 2015, 38, e184–e185. [Google Scholar] [CrossRef]
- Yavuz, M.; Ersen, A.; Hartos, J.; Schwarz, B.; Garrett, A.G.; Lavery, L.A.; Wukich, D.K.; Adams, L.S. Plantar shear stress in individuals with a history of diabetic foot ulcer: An emerging predictive marker for foot ulceration. Diabetes Care 2017, 40, e14–e15. [Google Scholar] [CrossRef]
- Guldemond, N.A.; Leffers, P.; Sanders, A.P.; Schaper, N.C.; Nieman, F.; Walenkamp, G.H.I.M. Daily-life activities and in-shoe forefoot plantar pressure in patients with diabetes. Diabetes Res. Clin. Pract. 2007, 77, 203–209. [Google Scholar] [CrossRef]
- Maluf, K.S.; Morley, R.E.; Richter, E.J.; Klaesner, J.W.; Mueller, M.J. Foot Pressures during Level Walking Are Strongly Associated with Pressures during Other Ambulatory Activities in Subjects with Diabetic Neuropathy. Arch. Phys. Med. Rehabil. 2004, 85, 253–260. [Google Scholar] [CrossRef]
- Shah, K.M.; Mueller, M.J. Effect of selected exercises on in-shoe plantar pressures in people with diabetes and peripheral neuropathy. Foot 2012, 22, 130–134. [Google Scholar] [CrossRef]
- Van Ancum, J.M.; van Schooten, K.S.; Jonkman, N.H.; Huijben, B.; van Lummel, R.C.; Meskers, C.G.M.; Maier, A.B.; Pijnappels, M. Gait speed assessed by a 4-m walk test is not representative of daily-life gait speed in community-dwelling adults. Maturitas 2019, 121, 28–34. [Google Scholar] [CrossRef]
- Gefen, A. How medical engineering has changed our understanding of chronic wounds and future prospects. Med. Eng. Phys. 2019, 72, 13–18. [Google Scholar] [CrossRef]
- Kluding, P.M.; Bareiss, S.K.; Hastings, M.; Marcus, R.L.; Sinacore, D.R.; Mueller, M.J. Physical Training and Activity in People With Diabetic Peripheral Neuropathy: Paradigm Shift. Phys. Ther. 2017, 97, 31–43. [Google Scholar] [CrossRef]
- Westby, M.; Norman, G.; Vedhara, K.; Game, F.; Cullum, N. Psychosocial and behavioural prognostic factors for diabetic foot ulcer development and healing: A systematic review. Diabet. Med. 2020, 37, 1244–1255. [Google Scholar] [CrossRef]
- Owings, T.M.; Apelqvist, J.; Stenström, A.; Becker, M.; Bus, S.A.; Kalpen, A.; Ulbrecht, J.S.; Cavanagh, P.R. Plantar pressures in diabetic patients with foot ulcers which have remained healed. Diabet. Med. 2009, 26, 1141–1146. [Google Scholar] [CrossRef]
- Lee, M.; van Netten, J.J.; Sheahan, H.; Lazzarini, P.A. Moderate-to-Vigorous-Intensity Physical Activity Observed in People With Diabetes-Related Foot Ulcers Over a One-Week Period. J. Diabetes Sci. Technol. 2019, 12–14. [Google Scholar] [CrossRef]
- Sheahan, H.; Canning, K.; Refausse, N.; Kinnear, E.M.; Jorgensen, G.; Walsh, J.R.; Lazzarini, P.A. Differences in the daily activity of patients with diabetic foot ulcers compared to controls in their free-living environments. Int. Wound J. 2017, 14, 1175–1182. [Google Scholar] [CrossRef] [PubMed]
- Bus, S.A.; van Deursen, R.W.M.; Kanade, R.V.; Wissink, M.; Manning, E.A.; van Baal, J.G.; Harding, K.G. Plantar pressure relief in the diabetic foot using forefoot offloading shoes. Gait Posture 2009, 29, 618–622. [Google Scholar] [CrossRef]

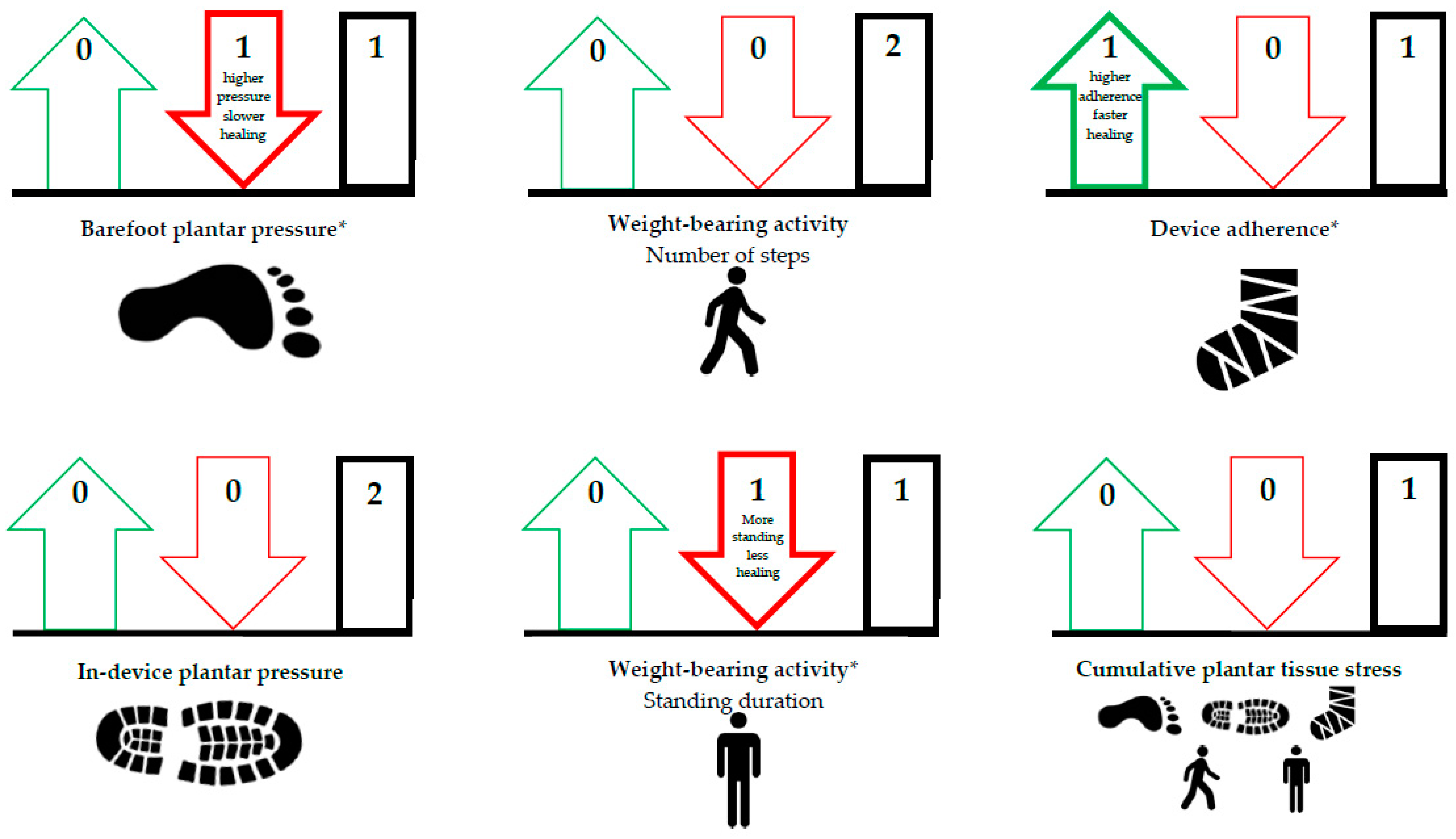
| Outcome | Factor | Evidence Statement | QoE | References |
|---|---|---|---|---|
| Ulcer development | Barefoot plantar pressure | Higher barefoot plantar pressure is associated with increased risk of ulcer development. | Moderate | Pham et al. [21], Caselli et al. [22], Lavery et al. [23], Kästenbauer et al. [24], Grimm et al. [25], Ulbrecht et al. [26], Deschamps et al. [27], Murray et al. [28], Qiu et al. [29], Waaijman et al. [12], Crawford et al. [30] |
| In-shoe plantar pressure | The association of in-shoe plantar pressure with risk of ulcer development seems unclear. | Low | Waaijman et al. [12], Ledoux et al. [31] | |
| Weight-bearing activity | The association of level and variation of weight-bearing activity with risk of ulcer development is unclear. | Low | Armstrong et al. [32], Lemaster et al. [33], Waaijman et al. [12], Mueller et al. [34], Schneider et al. [35] | |
| Footwear adherence | Lower footwear adherence seems associated with increased risk of ulcer development. | Low | Chantelau et al. [36], Connor et al. [37], Waaijman et al. [12] | |
| Cumulative plantar tissue stress | Higher cumulative plantar tissue stress seems to increase the risk of ulcer development. | Low | Waaijman et al. [12] | |
| Ulcer healing | Barefoot plantar pressure | Lower barefoot plantar pressure seems associated with shorter ulcer healing times. | Low | Armstrong et al. [38] |
| In-device plantar pressure | In-device plantar pressure in already adequately offloading devices seems not associated with ulcer healing incidence and times. | Low | Van Netten et al. [13], Jarl et al. [39] | |
| Weight-bearing activity | The association of level of weight-bearing activity with ulcer healing incidence seems unclear. | Low | Van Netten et al. [13], Najafi et al. [40] | |
| Device adherence | Higher device adherence seems associated with shorter ulcer healing times. | Low | Crews et al. [41] | |
| Cumulative plantar tissue stress | Lower cumulative plantar tissue stress seems to increase the chance of ulcer healing. | Low | Van Netten et al. [13] |
| Total | Ulcer Development | Ulcer Healing | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 20) * | Barefoot Plantar Pressure (n = 8) | In-Shoe Plantar Pressure (n = 2) | Weight-Bearing Activity (n = 5) | Footwear Adherence (n = 3) | Cumulative Plantar Tissue Stress (n = 1) | Barefoot Plantar Pressure (n = 1) | In-Device Plantar Pressure (n = 2) | Weight-Bearing Activity (n = 2) | Device Adherence (n = 1) | Cumulative Plantar Tissue Stress (n = 1) | ||
| Study participation | L | 7 | 4 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | ||
| M | 6 | 3 | 1 | 1 | 1 | |||||||
| H | 7 | 1 | 2 | 1 | 1 | 1 | 1 | |||||
| Study attrition | L | 14 | 6 | 3 | 1 | 1 | 2 | 1 | 1 | 1 | ||
| M | 4 | 1 | 2 | 2 | 1 | 1 | 1 | |||||
| H | 2 | 1 | 1 | |||||||||
| Prognostic factor measurement | L | 10 | 5 | 2 | 1 | 1 | 1 | 1 | 1 | |||
| M | 9 | 3 | 2 | 3 | 2 | 1 | 1 | 1 | ||||
| H | 1 | 1 | ||||||||||
| Outcome measurement | L | 5 | 2 | 1 | 3 | 1 | 1 | 1 | ||||
| M | 7 | 3 | 1 | 2 | 1 | 1 | 1 | |||||
| H | 8 | 3 | 2 | 2 | 1 | |||||||
| Study confounding | L | 5 | 2 | 2 | 2 | 1 | 1 | 1 | ||||
| M | 5 | 3 | 1 | 1 | 1 | 1 | ||||||
| H | 10 | 3 | 3 | 2 | 1 | 1 | ||||||
| Statistical analysis and reporting | L | 5 | 2 | 2 | 2 | 1 | 1 | 1 | ||||
| M | 12 | 5 | 3 | 2 | 1 | 1 | 1 | 1 | ||||
| H | 3 | 1 | 1 | 1 | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hulshof, C.M.; van Netten, J.J.; Pijnappels, M.; Bus, S.A. The Role of Foot-Loading Factors and Their Associations with Ulcer Development and Ulcer Healing in People with Diabetes: A Systematic Review. J. Clin. Med. 2020, 9, 3591. https://doi.org/10.3390/jcm9113591
Hulshof CM, van Netten JJ, Pijnappels M, Bus SA. The Role of Foot-Loading Factors and Their Associations with Ulcer Development and Ulcer Healing in People with Diabetes: A Systematic Review. Journal of Clinical Medicine. 2020; 9(11):3591. https://doi.org/10.3390/jcm9113591
Chicago/Turabian StyleHulshof, Chantal M., Jaap J. van Netten, Mirjam Pijnappels, and Sicco A. Bus. 2020. "The Role of Foot-Loading Factors and Their Associations with Ulcer Development and Ulcer Healing in People with Diabetes: A Systematic Review" Journal of Clinical Medicine 9, no. 11: 3591. https://doi.org/10.3390/jcm9113591
APA StyleHulshof, C. M., van Netten, J. J., Pijnappels, M., & Bus, S. A. (2020). The Role of Foot-Loading Factors and Their Associations with Ulcer Development and Ulcer Healing in People with Diabetes: A Systematic Review. Journal of Clinical Medicine, 9(11), 3591. https://doi.org/10.3390/jcm9113591





