Clinical Outcomes after Additional Dynamic Renal® Stent Implantation for Stent Recoil in Ostial Coronary Lesions
Abstract
1. Introduction
2. Experimental Section
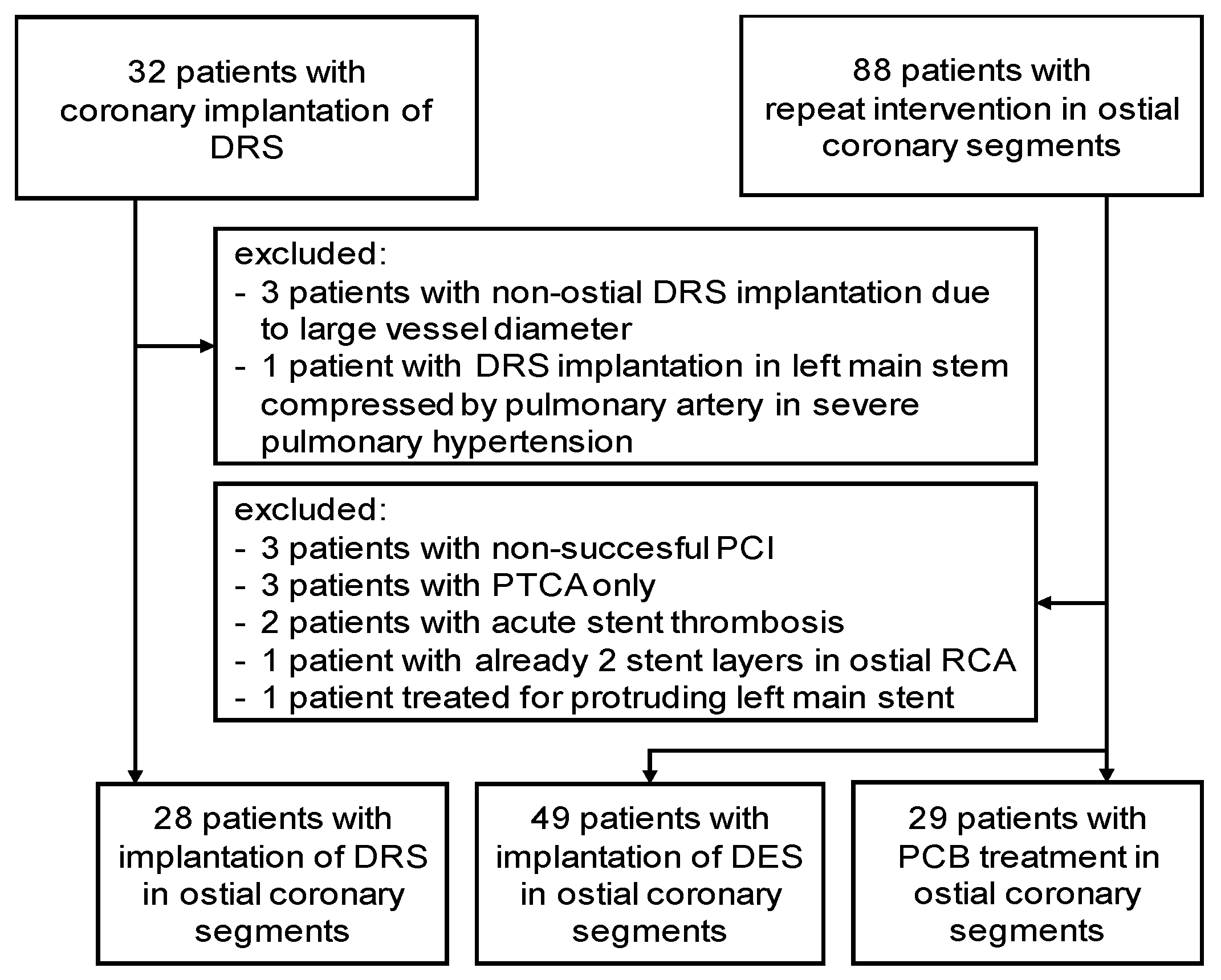
2.1. Study Population
2.2. Collection of Data
2.3. Definition of Outcomes
2.4. Statistical Analysis
2.5. Ethics Statement
3. Results
3.1. Characteristics of the Study Population
3.2. Clinical Outcomes according to Treatment Strategy
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Tsunoda, T.; Nakamura, M.; Wada, M.; Ito, N.; Kitagawa, Y.; Shiba, M.; Yajima, S.; Iijima, R.; Nakajima, R.; Yamamoto, M.; et al. Chronic stent recoil plays an important role in restenosis of the right coronary ostium. Coron. Artery Dis. 2004, 15, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Wohrle, J.; Markovic, S. Percutaneus coronary interventions for ostial lesions. Herz 2016, 41, 579. [Google Scholar] [CrossRef] [PubMed]
- Al-Lamee, R.; Ielasi, A.; Latib, A.; Godino, C.; Mussardo, M.; Arioli, F.; Figin, F.; Piraino, D.; Carlino, M.; Montorfano, M.; et al. Comparison of long-term clinical and angiographic outcomes following implantation of bare metal stents and drug-eluting stents in aorto-ostial lesions. Am. J. Cardiol. 2011, 108, 1055–1060. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.; Natsuaki, M.; Toyofuku, M.; Morimoto, T.; Matsumura, Y.; Oi, M.; Motohashi, Y.; Takahashi, K.; Kawase, Y.; Tanaka, M.; et al. Sirolimus-eluting stent implantation for ostial right coronary artery lesions: Five-year outcomes from the j-Cypher registry. Cardiovasc. Interv. Ther. 2014, 29, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Jurado-Roman, A.; Lopez-Melgar, B.; Garcia-Tejada, J.; Hernandez-Hernandez, F.; Velazquez-Martin, M.T.; Albarran-Gonzalez-Trevilla, A.; Rubio-Alonso, B.; Díaz-Anton, B.; Andreu-Dussac, J.; Tascón-Pérez, J.C. Percutaneous coronary intervention in aorto-ostial lesions. Immediate and medium-term results in a real world cohort. Int. J. Cardiol. 2013, 168, 3067–3069. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Takagi, K.; Naganuma, T.; Nakamura, S. Comparison of early- and new-generation drug-eluting stent implantations for ostial right coronary artery lesions. Cardiovasc. Ther. 2017, 35, e12247. [Google Scholar] [CrossRef] [PubMed]
- Piccolo, R.; Pilgrim, T.; Heg, D.; Franzone, A.; Rat-Wirtzler, J.; Raber, L.; Silber, S.; Serruys, P.W.; Jüni, P.; Windecker, S. Comparative Effectiveness and Safety of New-Generation Versus Early-Generation Drug-Eluting Stents According to Complexity of Coronary Artery Disease: A Patient-Level Pooled Analysis of 6,081 Patients. JACC Cardiovasc. Interv. 2015, 8, 1657–1666. [Google Scholar] [CrossRef] [PubMed]
- Mitomo, S.; Jabbour, R.J.; Watanabe, Y.; Mangieri, A.; Ancona, M.; Regazzoli, D.; Tanaka, A.; Nakajima, A.; Naganuma, T.; Giannini, F.; et al. Comparison of mid-term clinical outcomes after treatment of ostial right coronary artery lesions with early and new generation drug-eluting stents: Insights from an international multicenter registry. Int. J. Cardiol. 2018, 254, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Nassar, H.; Gotsman, I.; Gerganski, P.; Moseri, M.; Lotan, C.; Gotsman, M. Cutting balloon angioplasty and stent implantation for aorto-ostial lesions: Clinical outcome and 1-year follow-up. Clin. Cardiol. 2009, 32, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Nasu, K.; Oikawa, Y.; Habara, M.; Shirai, S.; Abe, H.; Kadotani, M.; Gotoh, R.; Hozawa, H.; Ota, H.; Suzuki, T.; et al. Efficacy of biolimus A9-eluting stent for treatment of right coronary ostial lesion with intravascular ultrasound guidance: A multi-center registry. Cardiovasc. Interv. Ther. 2017, 33, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Luz, A.; Hughes, C.; Magalhães, R.; Bisceglia, T.; Descoutures, F.; Tamamm, K.; Tchetche, D.; Sauguet, A.; Farah, B.; Fajadet, J. Stent implantation in aorto-ostial lesions: Long-term follow-up and predictors of outcome. EuroIntervention 2012, 7, 1069–1076. [Google Scholar] [CrossRef] [PubMed]
- Battikh, K.; Rihani, R.; Lemahieu, J.M. Acute stent recoil in the left main coronary artery treated with additional stenting. J. Invasive Cardiol. 2003, 15, 39–42. [Google Scholar] [PubMed]
- Ratib, K.; Doshi, S.N.; Townend, J.N. Double-stenting of an ostial left main-stem lesion for elastic recoil. Int. J. Cardiol. 2005, 102, 357–358. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.D.; Appleby, C.E.; Chowdhary, S.; Fraser, D.G. Double stenting: A method for treating acute stent recoil and luminal filling defects. EuroIntervention 2011, 6, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Patel, Y.; Depta, J.P.; Patel, J.S.; Masrani, S.K.; Novak, E.; Zajarias, A.; I Kurz, H.; LaSala, J.M.; Bach, R.G.; Singh, J. Impact of intravascular ultrasound on the long-term clinical outcomes in the treatment of coronary ostial lesions. Catheter. Cardiovasc. Interv. 2015, 87, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Rubinshtein, R.; Ben-Dov, N.; Halon, D.A.; Lavi, I.; Finkelstein, A.; Lewis, B.S.; Jaffe, R. Geographic miss with aorto-ostial coronary stent implantation: Insights from high-resolution coronary computed tomography angiography. EuroIntervention 2015, 11, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Morales-Ponce, F.J.; Blasco-Turrion, S.; Casquero-Dominguez, S.; Collado-Moreno, C.; Lobo-Torres, I.; Gomez-Lopez, A. Coronary lithotripsy in a severely calcified, cutting-balloon undilatable aorto-ostial lesion. Rev. Esp. Cardiol. (Engl. Ed.) 2020, 73, 173–175. [Google Scholar] [CrossRef]
- Hill, J.M.; Kereiakes, D.J.; Shlofmitz, R.A.; Klein, A.J.; Riley, R.F.; Price, M.J.; Herrmann, H.C.; Bachinsky, W.; Waksman, R.; Stone, G.W. Intravascular Lithotripsy for Treatment of Severely Calcified Coronary Artery Disease: The Disrupt CAD III Study. J. Am. Coll. Cardiol. 2020, 76, 2635–2646. [Google Scholar] [CrossRef] [PubMed]

| DRS (n = 28) | DES (n = 49) | PCB (n = 29) | p-Value | |
|---|---|---|---|---|
| Median Follow-up (days) | 992 (514–1108) | 1312 (1110–2137) | 1550 (111–2140) | <0.01 |
| Follow-up at 2 years complete | 21 (75%) | 48 (98%) | 29 (100%) | <0.01 |
| Follow-up at 1 year complete | 27 (96%) | 49 (100%) | 29 (100%) | 0.25 |
| Right coronary ostial lesion | 22 (78%) | 39 (80%) | 18 (62%) | 0.20 |
| Age (years) | 75.5 (70.2–80.0) | 71.0 (60.5–77.0) | 71.0 (63.5–78.0) | 0.09 |
| Female sex | 8 (28.6%) | 9 (18.4%) | 7 (24.1%) | 0.57 |
| BMI (kg/m²) | 27.8 (25.7–30.9) | 27.3 (24.8–30.8) | 26.8 (23.8–30.0) | 0.44 |
| Risk factors | ||||
| Arterial hypertension | 26 (92.9%) | 43 (87.8%) | 27 (93.1%) | 0.65 |
| Diabetes mellitus | 8 (28.6%) | 16 (32.7%) | 13 (44.8%) | 0.39 |
| Family history of CVD | 6 (21.4%) | 24 (49%) | 11 (37.9%) | 0.05 |
| Current smoking | 2 (7.1%) | 7 (14.3%) | 3 (10.3%) | 0.62 |
| Cardiac history | ||||
| Acute coronary syndrome | 5 (17.9%) | 5 (10.2%) | 9 (31%) | 0.06 |
| Coronary artery bypass grafting | 7 (25%) | 8 (16.3%) | 10 (34.5%) | 0.18 |
| Previous myocardial infarction | 6 (21.4%) | 15 (30.6%) | 14 (48.3%) | 0.08 |
| Reduced left ventricular function | 9 (32.1%) | 13 (26.5%) | 8 (27.6%) | 0.86 |
| Medication | ||||
| Length of P2Y12 inhibition | 12 (6.0–12) | 6 (6.0–6.0) | 6 (3.75–11.5) | <0.01 |
| Insulin | 3 (10.7%) | 8 (16.3%) | 6 (20.7%) | 0.58 |
| Oral antidiabetics | 6 (21.4%) | 12 (24.5%) | 9 (31%) | 0.69 |
| Laboratory parameters | ||||
| eGFR (mLmin) | 68.6 (55.2–78.0) | 72.6 (55.1–77.7) | 72.8 (56.9–85.5) | 0.56 |
| Hemoglobin (g/dL) | 13.3 (12.0–14.3) | 14.3 (13.1–15.3) | 13.9 (12.0–14.5) | 0.12 |
| Total cholesterol (mg/dL) | 150 (134–168) | 169 (142–204) | 156 (141–188) | 0.06 |
| LDL cholesterol (mg/dL) | 93 (65–110) | 100 (82–133) | 89 (72–107) | 0.07 |
| HDL cholesterol (mg/dL) | 50.0 (42.0–65.7) | 49.0 (40.0–60.5) | 50.0 (43.5–64.0) | 0.52 |
| C-reactive protein (mg/dL) | 0.3 (0.1–0.8) | 0.3 (0.1–0.5) | 0.2 (0.1–0.4) | 0.69 |
| DRS (n = 28) | |
|---|---|
| Severity of recoil (mild/moderate/severe) | 15/12/1 |
| Recoil after DRS (unchanged/improved/resolved) | 7/11/10 |
| Procedural optimization and auxiliary devices | |
| Guide catheter extension | 3 |
| Cutting-Balloon | 5 |
| Ultra-high pressure balloon (OPN) | 7 |
| Intravascular ultrasound | 3 |
| Rotational atherectomy | 2 |
| DRS (n = 28) | DES (n = 49) | PCB (n = 29) | p-Value | |
|---|---|---|---|---|
| Predilatation performed | 28 (100%) | 39 (78%) | 28 (97%) | 0.007 |
| Diameter (mm) | 4.0 (3.0–4.0) | 3.0 (2.5–3.5) | 3.25 (3.0–3.5) | 0.001 |
| Maximal pressure (bar) | 22 (18.5–26) | 17 (16–22) | 20 (13.25–23.5) | 0.014 |
| Stent/PCB diameter (mm) | 5.0 | 3.5 (3.5–4.0) | 3.5 (3.0–4.0) | <0.001 |
| Stent/PCB length (mm) | 12 | 16 (12–20) | 15 (15–20) | <0.001 |
| Maximal pressure (bar) | 16 (12.5–20) | 18 (14–20) | 14 (12–16) | <0.001 |
| Stent type | ||||
| Promus Element/Premier | 12 (25%) | |||
| Resolute Integrity | 12 (25%) | |||
| Xience Pro | 9 (18%) | |||
| Orsiro | 5 (10%) | |||
| Synergy II | 4 (8%) | |||
| Other | 7 (14%) | |||
| Postdilatation Performed | 24 (86%) | 28 (57%) | 0 (0%) | <0.001 |
| Diameter (mm) | 4.25 (4.0–5.0) | 4.0 (3.5–4.0) | n.a. | 0.003 |
| Maximal pressure (bar) | 21 (20–40) | 20 (20–24) | n.a. | 0.069 |
| DRS (n = 28) | DES (n = 49) | PCB (n = 29) | p-Value | |
|---|---|---|---|---|
| Stent diameter (mm) | 3.5 (3.5–4.0) | 3.5 (3.25–4.0) | 3.5 (3.0–3.5) | <0.001 |
| Stent length (mm) | 16 (15–24) | 18 (15–25) | 26 (18–33) | 0.015 |
| Maximal pressure (bar) | 18 (18–20) | 16 (14–18) | 16 (16–17) | <0.001 |
| Stent type | ||||
| Promus Element/Premier | 10 (36%) | 6 (12%) | 9 (31%) | |
| Resolute Integrity | 2 (7%) | 10 (20%) | 8 (28%) | |
| Resolute Onyx | 7 (25%) | |||
| Xience Pro | 4 (14%) | 5 (10%) | 2 (7%) | |
| Orsiro | 0 | 1 (2%) | 1 (3%) | |
| Synergy II | 2 (7%) | 0 | 0 | |
| Other | 3 (11%) | 27 (55%) | 9 (31%) | |
| Postdilatation Performed | 28 (100%) | 20 (41%) | 13 (45%) | <0.001 |
| Diameter (mm) | 4.0 (3.5–4.5) | 3.5 (3.5–4.0) | 3.5 (3.5–4.5) | 0.004 |
| Maximal pressure (bar) | 24 (20–40) | 20 (16.5–22) | 20 (16.5–22) | 0.010 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdulrahman, B.; Mashayekhi, K.; Tajti, P.; Ferenc, M.; Valina, C.M.; Hochholzer, W.; Neumann, F.-J.; Nührenberg, T.G. Clinical Outcomes after Additional Dynamic Renal® Stent Implantation for Stent Recoil in Ostial Coronary Lesions. J. Clin. Med. 2020, 9, 3964. https://doi.org/10.3390/jcm9123964
Abdulrahman B, Mashayekhi K, Tajti P, Ferenc M, Valina CM, Hochholzer W, Neumann F-J, Nührenberg TG. Clinical Outcomes after Additional Dynamic Renal® Stent Implantation for Stent Recoil in Ostial Coronary Lesions. Journal of Clinical Medicine. 2020; 9(12):3964. https://doi.org/10.3390/jcm9123964
Chicago/Turabian StyleAbdulrahman, Bachir, Kambis Mashayekhi, Péter Tajti, Miroslaw Ferenc, Christian Marc Valina, Willibald Hochholzer, Franz-Josef Neumann, and Thomas Georg Nührenberg. 2020. "Clinical Outcomes after Additional Dynamic Renal® Stent Implantation for Stent Recoil in Ostial Coronary Lesions" Journal of Clinical Medicine 9, no. 12: 3964. https://doi.org/10.3390/jcm9123964
APA StyleAbdulrahman, B., Mashayekhi, K., Tajti, P., Ferenc, M., Valina, C. M., Hochholzer, W., Neumann, F.-J., & Nührenberg, T. G. (2020). Clinical Outcomes after Additional Dynamic Renal® Stent Implantation for Stent Recoil in Ostial Coronary Lesions. Journal of Clinical Medicine, 9(12), 3964. https://doi.org/10.3390/jcm9123964






