Long-Term Surgical Results of Skip Pedicle Screw Fixation for Patients with Adolescent Idiopathic Scoliosis: A Minimum-Ten-Year Follow-Up Study
Abstract
:1. Introduction
2. Methods
2.1. Patients
2.2. Surgical Technique
2.3. Evaluation and Statistical Analysis
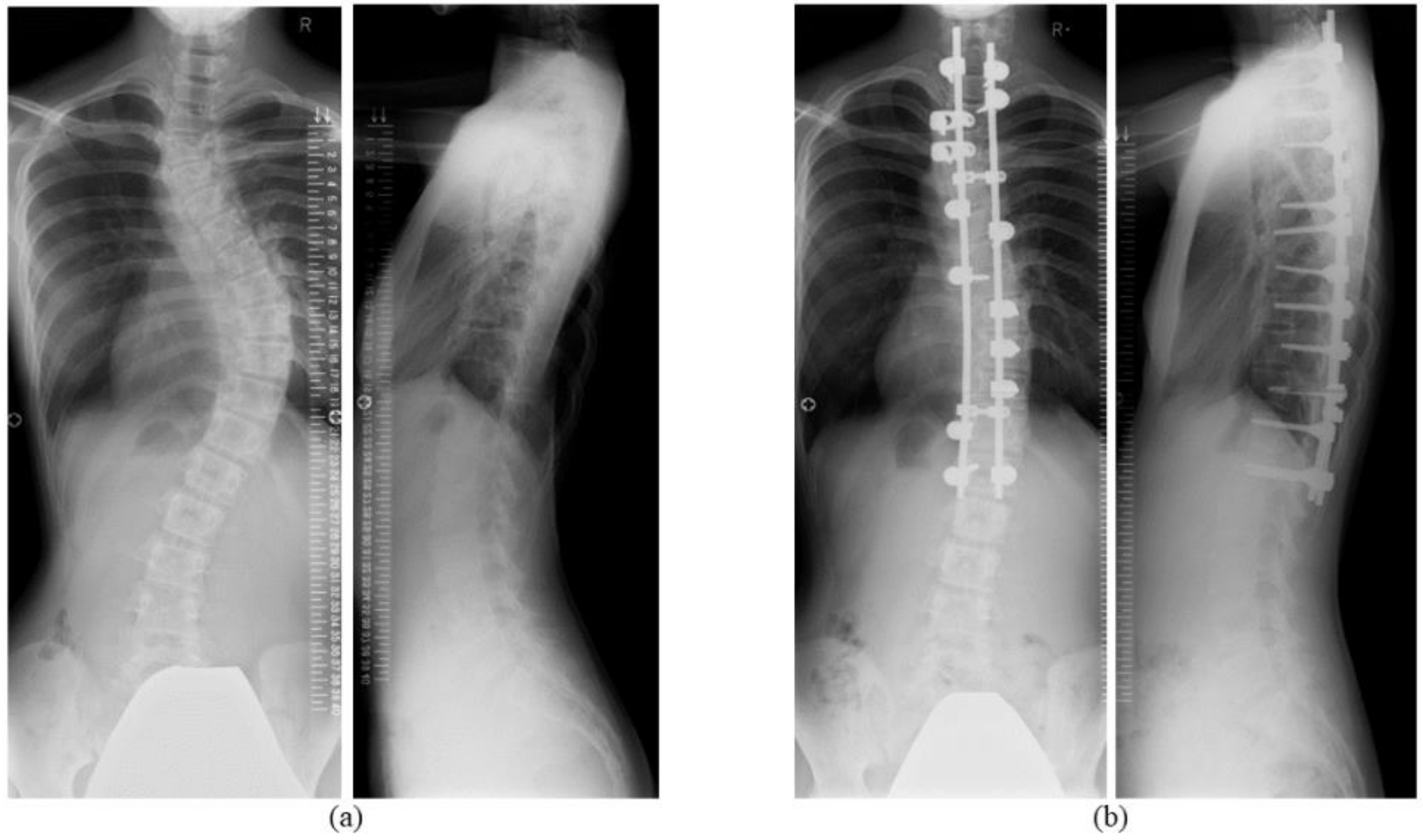
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Suk, S.I.; Lee, C.K.; Kim, W.J.; Chung, Y.J.; Park, Y.B. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 1995, 20, 1399–1405. [Google Scholar] [CrossRef] [PubMed]
- Halm, H.; Niemeyer, T.; Link, T.; Liljenqvist, U. Segmental pedicle screw instrumentation in idiopathic thoracolumbar and lumbar scoliosis. Eur. Spine J. 2000, 9, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Liljenqvist, U.R.; Halm, H.F.; Link, T.M. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine 1997, 22, 2239–2245. [Google Scholar] [CrossRef] [PubMed]
- Heini, P.; Scholl, E.; Wyler, D.; Eggli, S. Fatal cardiac tamponade associated with posterior spinal instrumentation. Spine 1998, 23, 2226–2230. [Google Scholar] [CrossRef] [PubMed]
- Papin, P.; Aebi, M. Unusual presentation of spinal cord compression related to misplaced pedicle screws in thoracic scoliosis. Eur. Spine J. 1999, 8, 156–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takahashi, J.; Hirabayashi, H.; Hashidate, H.; Ogihara, N.; Kato, H. Accuracy of multilevel registration in image-guided pedicle screw insertion for adolescent idiopathic scoliosis. Spine 2010, 35, 347–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takahashi, J.; Ikegami, S.; Kuraishi, S.; Shimizu, M.; Futatsugi, T.; Kato, H. Skip pedicle screw fixation combined with Ponte osteotomy for adolescent idiopathic scoliosis. Eur. Spine J. 2014, 23, 2689–2695. [Google Scholar] [CrossRef]
- Mukaiyama, K.; Takahashi, J.; Hirabayashi, H.; Ogihara, N.; Kuraishi, S.; Shimizu, M.; Kato, H. Factors influencing the residual rib hump after posterior spinal fusion for adolescent idiopathic scoliosis with Lenke 1 and 2 curves. J. Orthop. Sci. 2013, 18, 687–692. [Google Scholar] [CrossRef] [Green Version]
- Uehara, M.; Takahashi, J.; Kuraishi, S.; Shimizu, M.; Ikegami, S.; Futatsugi, T.; Oba, H.; Kato, H. Computer-assisted skip pedicle screw fixation for adolescent idiopathic scoliosis. J. Orthop. Sci. 2017, 22, 218–223. [Google Scholar] [CrossRef]
- Kotani, Y.; Abumi, K.; Ito, M.; Minami, A. Improved accuracy of computer-assisted cervical pedicle screw insertion. J. Neurosurg. 2003, 99 (Suppl. 3), 257–263. [Google Scholar] [CrossRef] [Green Version]
- Cobb, J.R. Outline for the study of scoliosis. Am. Acad. Orthop. Surg. Inst. Course Lect. 1948, 5, 261–275. [Google Scholar]
- Haher, T.R.; Gorup, J.M.; Shin, T.M.; Homel, P.; Merola, A.A.; Grogan, D.P.; Pugh, L.; Lowe, T.G.; Murray, M. Results of the Scoliosis Research Society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis, A multicenter study of 244 patients. Spine 1999, 24, 1435–1440. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, H.; Sase, T.; Arai, Y.; Maruyama, T.; Isobe, K.; Shouno, Y. Validation of a Japanese version of the Scoliosis Research Society-22 Patient Questionnaire among idiopathic scoliosis patients in Japan. Spine 2007, 32, E141–E146. [Google Scholar] [CrossRef]
- Fukui, M.; Chiba, K.; Kawakami, M.; Kikuchi, S.; Konno, S.; Miyamoto, M.; Seichi, A.; Shimamura, T.; Shirado, O.; Taguchi, T.; et al. Subcommittee of the Clinical Outcome Committee of the Japanese Orthopaedic Association on Low Back Pain and Cervical Myelopathy Evaluation. JOA back pain evaluation questionnaire (JOABPEQ)/JOA Cervical Myelopathy evaluation questionnaire (JOACMEQ), The report on the development of revised versions, April 16, 2007, The Subcommittee of the clinical outcome committee of the Japanese orthopaedic association on low back pain and Cervical Myelopathy evaluation. J. Orthop. Sci. 2009, 14, 348–365. [Google Scholar] [PubMed]
- Li, S.; Chen, Z.H.; Qiu, Y.; Xu, L.; Chen, X.; Du, C.Z.; Zhu, Z.Z.; Sun, X. Coronal decompensation after posterior-only thoracolumbar hemivertebra resection and short fusion in young children with congenital scoliosis. Spine 2018, 43, 654–660. [Google Scholar] [CrossRef] [PubMed]
- Kwan, M.K.; Chiu, C.K.; Tan, P.H.; Chian, X.H.; Ler, X.Y.; Ng, Y.H.; Ng, S.J.; Goh, S.H.; Chan, C.Y.W. Radiological and clinical outcome of selective thoracic fusion for patients with Lenke 1C and 2C adolescent idiopathic scoliosis with a minimum follow-up of 2 years. Spine J. 2018, 18, 2239–2246. [Google Scholar] [CrossRef] [PubMed]
- Cho, R.H.; Yaszay, B.; Bartley, C.E.; Bastrom, T.P.; Newton, P.O. Which Lenke 1A curves are at the greatest risk for adding-on… and why? Spine 2012, 37, 1384–1390. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, M.; Takahashi, J.; Ikegami, S.; Kuraishi, S.; Futatsugi, T.; Kato, H. Are pedicle screw perforation rates influenced by registered or unregistered vertebrae in multilevel registration using a CT-based navigation system in the setting of scoliosis? Eur. Spine J. 2014, 23, 2211–2217. [Google Scholar] [CrossRef]
- Belmont, P.J., Jr.; Klemme, W.R.; Dhawan, A.; Polly, D.W., Jr. In vivo accuracy of thoracic pedicle screws. Spine 2001, 26, 2340–2346. [Google Scholar] [CrossRef]
- Suk, S.I.; Kim, W.J.; Lee, S.M.; Kim, J.H.; Chung, E.R. Thoracic pedicle screw fixation in spinal deformities: Are they really safe? Spine 2001, 26, 2049–2057. [Google Scholar] [CrossRef]
- Behrbalk, E.; Uri, O.; Parks, R.M.; Grevitt, M.P.; Rickert, M.; Boszczyk, B.M. Posterior-only correction of Scheuermann kyphosis using pedicle screws: Economical optimization through screw density reduction. Eur. Spine J. 2014, 23, 2203–2210. [Google Scholar] [CrossRef] [PubMed]
- Cheung, K.M.; Natarajan, D.; Samartzis, D.; Wong, Y.W.; Cheung, W.Y.; Luk, K.D. Predictability of the fulcrum bending radiograph in scoliosis correction with alternate-level pedicle screw fixation. J. Bone Joint Surg. Am. 2010, 92, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Uehara, M.; Takahashi, J.; Ikegami, S.; Oba, H.; Kuraishi, S.; Futatsugi, T.; Takizawa, T.; Munakata, R.; Koseki, M.; Kato, H. Determination of optimal screw number based on correction angle for main thoracic curve in adolescent idiopathic scoliosis. J. Orthop. Sci. 2019, 24, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Crawford, A.H.; Lykissas, M.G.; Gao, X.; Eismann, E.; Anadio, J. All-pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery: A comparative radiographical study with a minimum 2-year follow-up. Spine 2013, 38, 1199–1208. [Google Scholar] [CrossRef] [Green Version]
- Hwang, C.J.; Lee, C.K.; Chang, B.S.; Kim, M.S.; Yeom, J.S.; Choi, J.M. Minimum 5-year follow-up results of skipped pedicle screw fixation for flexible idiopathic scoliosis. J. Neurosurg. Spine 2011, 15, 146–150. [Google Scholar] [CrossRef]
- Ishikawa, M.; Cao, K.; Pang, L.; Watanabe, K.; Yagi, M.; Hosogane, N.; Machida, M.; Shiono, Y.; Nishiyama, M.; Fukui, Y.; et al. Postoperative behavior of thoracolumbar/lumbar curve and coronal balance after posterior thoracic fusion for Lenke 1C and 2C adolescent idiopathic scoliosis. J. Orthop. Sci. 2015, 20, 31–37. [Google Scholar] [CrossRef] [Green Version]
- Skaggs, D.L.; Seehausen, D.A.; Yamaguchi, K.T., Jr.; Hah, R.J.; Wright, M.L.; Bumpass, D.B.; Kim, H.J.; Andras, L.M.; Vitale, M.G.; Lenke, L.G. Assessment of Lowest Instrumented Vertebra Tilt on Radiographic Measurements in Lenke “C” Modifier Curves Undergoing Selective Thoracic Fusion in Adolescent Idiopathic Scoliosis. Spine Deform. 2016, 4, 125–130. [Google Scholar] [CrossRef]
- Tominaga, R.; Sekiguchi, M.; Yonemoto, K.; Kakuma, T.; Konno, S.I. Establishment of reference scores and interquartile ranges for the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) in patients with low back pain. J. Orthop. Sci. 2018, 23, 643–648. [Google Scholar] [CrossRef]
- Ogura, Y.; Ogura, K.; Kobayashi, Y.; Kitagawa, T.; Yonezawa, Y.; Takahashi, Y.; Yoshida, K.; Yasuda, A.; Shinozaki, Y.; Ogawa, J. Minimally clinically important differences for the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) following decompression surgery for lumbar spinal stenosis. J. Clin. Neurosci. 2019, 69, 93–96. [Google Scholar] [CrossRef]
- Bharucha, N.J.; Lonner, B.S.; Auerbach, J.D.; Kean, K.E.; Trobisch, P.D. Low-density versus high-density thoracic pedicle screw constructs in adolescent idiopathic scoliosis: Do more screws lead to a better outcome? Spine J. 2013, 13, 375–381. [Google Scholar] [CrossRef]
- Mariconda, M.; Galasso, O.; Barca, P.; Milano, C. Minimum 20-year follow-up results of Harrington rod fusion for idiopathic scoliosis. Eur. Spine J. 2005, 14, 854–861. [Google Scholar] [CrossRef]
- Akazawa, T.; Minami, S.; Kotani, T.; Nemoto, T.; Koshi, T.; Takahashi, K. Long-term clinical outcome of surgery for adolescent idiopathic scoliosis 21 to 41 years later. Spine 2012, 37, 402–405. [Google Scholar] [CrossRef] [PubMed]
- Götze, C.; Liljenqvist, U.R.; Slomka, A.; Götze, H.G.; Steinbeck, J. Quality of life and back pain: Outcome 16.7 years after Harrington instrumentation. Spine 2002, 27, 1456–1463. [Google Scholar] [CrossRef] [PubMed]
- Carreon, L.Y.; Sanders, J.O.; Diab, M.; Sucato, D.J.; Sturm, P.F.; Glassman, S.D.; Spinal Deformity Study Group. The minimum clinically important difference in Scoliosis Research Society-22 Appearance, Activity, and Pain domains after surgical correction of adolescent idiopathic scoliosis. Spine 2010, 35, 2079–2083. [Google Scholar] [CrossRef] [PubMed]
- Newton, P.O.; Yaszay, B.; Upasani, V.V.; Pawelek, J.B.; Bastrom, T.P.; Lenke, L.G.; Lowe, T.; Crawford, A.; Betz, R.; Harms Study Group; et al. Preservation of thoracic kyphosis is critical to maintain lumbar lordosis in the surgical treatment of adolescent idiopathic scoliosis. Spine 2010, 35, 1365–1370. [Google Scholar] [CrossRef] [PubMed]
- Solberg, T.K.; Sørlie, A.; Sjaavik, K.; Nygaard, Ø.P.; Ingebrigtsen, T. Would loss to follow-up bias the outcome evaluation of patients operated for degenerative disorders of the lumbar spine? Acta Orthop. 2011, 82, 56–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Mean ± Standard Deviation (Range) | |
|---|---|
| Age, years | 14.4 ± 2.1 (12–19) |
| Sex, male/female | 2:23 |
| Cobb angle of main thoracic curve, ° | 59.5 ± 15.1 (44–94) |
| Main curve flexibility, % | 38.2 ± 19.4 (6.3–96.1) |
| Cobb angle of lumbar curve, ° | 40.5 ± 19.9 (12–82) |
| Thoracic kyphotic angle (T5–T12), ° | 9.1 ± 8.3 (−8–29) |
| Clavicular angle, ° | 2.2 ± 1.9 (0–7.9) |
| C7PL, cm | 1.4 ± 1.1 (0–5.0) |
| Radiological and Physical Evaluation | Before Surgery | Immediately after Surgery | Two Years after Surgery | Ten Years after Surgery |
|---|---|---|---|---|
| Cobb angle of main thoracic curve, ° | 59.4 ± 3.0 | 23.4 ± 1.8 ** | 25.8 ± 1.7 ** | 25.6 ± 1.7 ** |
| Correction rate of Cobb angle (main thoracic curve), % | N/A | 60.8 ± 2.2 | 56.3 ± 2.5 | 56.8 ± 2.2 |
| Thoracic kyphotic angle (T5–T12), ° | 9.1 ± 1.7 | 15.2 ± 1.6 ** | 17.9 ± 1.5 ** | 15.2 ± 1.5 ** |
| Clavicular angle, ° | 2.2 ± 0.4 | 3.2 ± 0.5 | 2.4 ± 0.4 | 2.2 ± 0.4 |
| C7PL, cm | 1.4 ± 0.2 | 1.3 ± 0.2 | 0.7 ± 0.2 * | 1.4 ± 0.4 |
| Cobb angle of lumbar curve, ° | 40.5 ± 4.0 | 18.6 ± 2.5 ** | 17.9 ± 2.2 ** | 18.8 ± 2.3 ** |
| LIV tilt, ° | 20.1 ± 1.5 | 7.8 ± 1.4 ** | 7.3 ± 1.4 ** | 7.7 ± 1.2 ** |
| SRS-22r Domain | Before Surgery | Two Years after Surgery | Ten Years after Surgery |
|---|---|---|---|
| Function | 4.31 ± 0.12 | 4.74 ± 0.05 ** | 4.65 ± 0.09 * |
| Pain | 4.01 ± 0.12 | 4.68 ± 0.07 ** | 4.40 ± 0.13 * |
| Self-image | 2.75 ± 0.11 | 3.88 ± 0.13 *** | 3.89 ± 0.15 *** |
| Mental health | 3.73 ± 0.18 | 4.62 ± 0.07 *** | 4.31 ± 0.12 * |
| Sub-total | 3.69 ± 0.10 | 4.48 ± 0.05 *** | 4.31 ± 0.09 *** |
| Satisfaction | N/A | 4.08 ± 0.15 | 4.02 ± 0.17 |
| Total | N/A | 4.44 ± 0.05 | 4.29 ± 0.09 |
| JOABPEQ Domain | Present Series | Reference Value [18] |
|---|---|---|
| Pain-related disorder | 86.8 ± 4.2 | 42.9 |
| Lumbar spine dysfunction | 94.0 ± 2.4 | 58.3 |
| Gait disturbance | 95.8 ± 2.7 | 50.0 |
| Social life disturbance | 84.4 ± 3.6 | 51.4 |
| Psychological disorder | 72.9 ± 3.4 | 47.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uehara, M.; Kuraishi, S.; Ikegami, S.; Oba, H.; Takizawa, T.; Munakata, R.; Hatakenaka, T.; Koseki, M.; Takahashi, J. Long-Term Surgical Results of Skip Pedicle Screw Fixation for Patients with Adolescent Idiopathic Scoliosis: A Minimum-Ten-Year Follow-Up Study. J. Clin. Med. 2020, 9, 4002. https://doi.org/10.3390/jcm9124002
Uehara M, Kuraishi S, Ikegami S, Oba H, Takizawa T, Munakata R, Hatakenaka T, Koseki M, Takahashi J. Long-Term Surgical Results of Skip Pedicle Screw Fixation for Patients with Adolescent Idiopathic Scoliosis: A Minimum-Ten-Year Follow-Up Study. Journal of Clinical Medicine. 2020; 9(12):4002. https://doi.org/10.3390/jcm9124002
Chicago/Turabian StyleUehara, Masashi, Shugo Kuraishi, Shota Ikegami, Hiroki Oba, Takashi Takizawa, Ryo Munakata, Terue Hatakenaka, Michihiko Koseki, and Jun Takahashi. 2020. "Long-Term Surgical Results of Skip Pedicle Screw Fixation for Patients with Adolescent Idiopathic Scoliosis: A Minimum-Ten-Year Follow-Up Study" Journal of Clinical Medicine 9, no. 12: 4002. https://doi.org/10.3390/jcm9124002
APA StyleUehara, M., Kuraishi, S., Ikegami, S., Oba, H., Takizawa, T., Munakata, R., Hatakenaka, T., Koseki, M., & Takahashi, J. (2020). Long-Term Surgical Results of Skip Pedicle Screw Fixation for Patients with Adolescent Idiopathic Scoliosis: A Minimum-Ten-Year Follow-Up Study. Journal of Clinical Medicine, 9(12), 4002. https://doi.org/10.3390/jcm9124002






