Factors Affecting Total Treatment Time in Patients Treated with Orthognathic Surgery Using the Surgery-First Approach: Multivariable Analysis Using 3D CT and Scanned Dental Casts
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Sample
2.2. Treatment Protocols
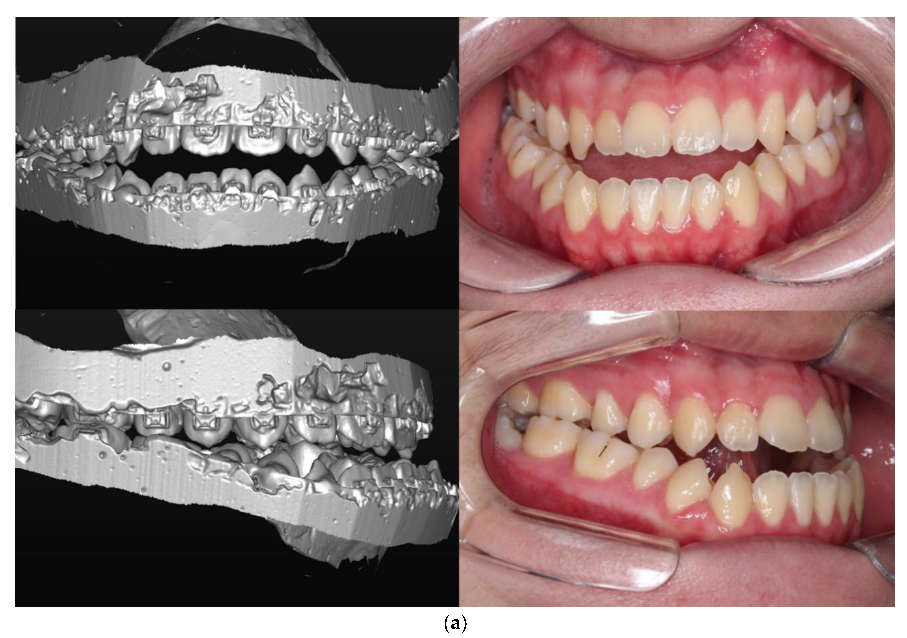
2.3. CBCT Imaging and Preoperative Planning
2.4. Study Variables
- (1)
- Demographic features
- (2)
- Surgical occlusion setup
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Beckwith, F.R.; Ackerman, R.J., Jr.; Cobb, C.M.; Tira, D.E. An evaluation of factors affecting duration of orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 439–447. [Google Scholar] [CrossRef]
- Nagasaka, H.; Sugawara, J.; Kawamura, H.; Nanda, R. “Surgery first” skeletal class iii correction using the skeletal anchorage system. J. Clin. Orthod. 2009, 43, 97–105. [Google Scholar] [PubMed]
- Baek, S.H.; Ahn, H.W.; Kwon, Y.H.; Choi, J.Y. Surgery-first approach in skeletal class III malocclusion treated with 2-jaw surgery: Evaluation of surgical movement and postoperative orthodontic treatment. J. Craniofac. Surg. 2010, 21, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Liou, E.J.; Chen, P.H.; Wang, Y.C.; Yu, C.C.; Huang, C.S.; Chen, Y.R. Surgery-first accelerated orthognathic surgery: Orthodontic guidelines and setup for model surgery. J. Oral. Maxillofac. Surg. 2011, 69, 771–780. [Google Scholar] [CrossRef]
- Liao, Y.F.; Chiu, Y.T.; Huang, C.S.; Ko, E.W.; Chen, Y.R. Presurgical orthodontics versus no presurgical orthodontics: Treatment outcome of surgical-orthodontic correction for skeletal class III open bite. Plast. Reconstr. Surg. 2010, 126, 2074–2083. [Google Scholar] [CrossRef]
- Jacobs, J.D.; Sinclair, P.M. Principles of orthodontic mechanics in orthognathic surgery cases. Am. J. Orthod. 1983, 84, 399–407. [Google Scholar] [CrossRef]
- Woods, M.; Wiesenfeld, D. A practical approach to presurgical orthodontic preparation. J. Clin. Orthod. 1998, 32, 350–358. [Google Scholar]
- Sabri, R. Orthodontic objectives in orthognathic surgery: State of the art today. World J. Orthod. 2006, 7, 177–191. [Google Scholar]
- Diaz, P.M.; Garcia, R.G.; Gias, L.N.; Aguirre-Jaime, A.; Perez, J.S.; de la Plata, M.M.; Navarro, E.V.; Gonzalez, F.J. Time used for orthodontic surgical treatment of dentofacial deformities in white patients. J. Oral. Maxillofac. Surg. 2010, 68, 88–92. [Google Scholar] [CrossRef]
- Liao, Y.F.; Lo, S.H. Surgical occlusion setup in correction of skeletal class iii deformity using surgery-first approach: Guidelines, characteristics and accuracy. Sci. Rep. 2018, 8, 11673. [Google Scholar] [CrossRef] [Green Version]
- Yu, H.B.; Mao, L.X.; Wang, X.D.; Fang, B.; Shen, S.G. The surgery-first approach in orthognathic surgery: A retrospective study of 50 cases. Int. J. Oral. Maxillofac. Surg. 2015, 44, 1463–1467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ko, E.W.; Hsu, S.S.; Hsieh, H.Y.; Wang, Y.C.; Huang, C.S.; Chen, Y.R. Comparison of progressive cephalometric changes and postsurgical stability of skeletal class iii correction with and without presurgical orthodontic treatment. J. Oral. Maxillofac. Surg. 2011, 69, 1469–1477. [Google Scholar] [CrossRef] [PubMed]
- Dowling, P.A.; Espeland, L.; Krogstad, O.; Stenvik, A.; Kelly, A. Duration of orthodontic treatment involving orthognathic surgery. Int. J. Adult Orthodon. Orthognath. Surg. 1999, 14, 146–152. [Google Scholar] [PubMed]
- Luther, F.; Morris, D.O.; Hart, C. Orthodontic preparation for orthognathic surgery: How long does it take and why? A retrospective study. Br. J. Oral. Maxillofac. Surg. 2003, 41, 401–406. [Google Scholar] [CrossRef]
- Luther, F.; Morris, D.O.; Karnezi, K. Orthodontic treatment following orthognathic surgery: How long does it take and why? A retrospective study. J. Oral. Maxillofac. Surg. 2007, 65, 1969–1976. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Jung, H.D.; Kim, S.Y.; Park, H.S.; Jung, Y.S. Postoperative stability for surgery-first approach using intraoral vertical ramus osteotomy: 12-month follow-up. Br. J. Oral. Maxillofac. Surg. 2014, 52, 539–544. [Google Scholar] [CrossRef]
- Min, B.K.; Choi, J.Y.; Baek, S.H. Comparison of treatment duration between conventional three-stage method and surgery-first approach in patients with skeletal class III malocclusion. J. Craniofac. Surg. 2014, 25, 1752–1756. [Google Scholar] [CrossRef]
- Park, H.M.; Lee, Y.K.; Choi, J.Y.; Baek, S.H. Maxillary incisor inclination of skeletal class III patients treated with extraction of the upper first premolars and two-jaw surgery: Conventional orthognathic surgery vs surgery-first approach. Angl. Orthod. 2014, 84, 720–729. [Google Scholar] [CrossRef] [Green Version]
- Ko, E.W.; Lin, S.C.; Chen, Y.R.; Huang, C.S. Skeletal and dental variables related to the stability of orthognathic surgery in skeletal class iii malocclusion with a surgery-first approach. J. Oral. Maxillofac. Surg. 2013, 71, e215–e223. [Google Scholar] [CrossRef]
- Villegas, C.; Uribe, F.; Sugawara, J.; Nanda, R. Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J. Clin. Orthod. 2010, 44, 97–103. [Google Scholar]
- Oh, J.Y.; Park, J.W.; Baek, S.H. Surgery-first approach in class iii open-bite. J. Craniofac. Surg. 2012, 23, e283–e287. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; Ko, E.W.; Huang, C.S.; Chen, Y.R.; Takano-Yamamoto, T. Comparison of transverse dimensional changes in surgical skeletal class iii patients with and without presurgical orthodontics. J. Oral. Maxillofac. Surg. 2010, 68, 1807–1812. [Google Scholar] [CrossRef] [PubMed]
- Gandedkar, N.H.; Chng, C.K.; Tan, W. Surgery-first orthognathic approach case series: Salient features and guidelines. J. Orthod. Sci. 2016, 5, 35–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Villegas, C.; Janakiraman, N.; Uribe, F.; Nanda, R. Rotation of the maxillomandibular complex to enhance esthetics using a “surgery first” approach. J. Clin. Orthod. 2012, 46, 85–91. [Google Scholar] [PubMed]






| Variables | N (%) or Mean ± SD | Treatment Time (Months) | p-Value |
|---|---|---|---|
| Age (years) | 22.0 ± 3.4 | 15.0 ± 8.0 | |
| Sex | 0.147 | ||
| Female | 28 (56.0%) | 13.1 ± 6.5 | |
| Male | 22 (44.0%) | 17.3 ± 9.2 | |
| Facial asymmetry | 0.938 | ||
| Asymmetry | 28 (56.0%) | 15.1 ± 8.3 | |
| Non-asymmetry | 22 (44.0%) | 14.7 ± 7.7 | |
| Preoperative anterior open bite | 0.021 * | ||
| No | 41 (82.0%) | 14.1 ± 8.4 | |
| Yes | 9 (18.0%) | 19.0 ± 4.4 | |
| Maxillary canting (mm) | 0.884 | ||
| Mild (<2) | 34 (68.0%) | 14.7 ± 7.3 | |
| Severe (≥2) | 16 (32.0%) | 15.5 ± 9.5 | |
| Maxilla ALD (mm) | |||
| Spacing (<0) | 8 (16.0%) | 14.1 ± 3.9 | 0.209 (1 vs. 2) |
| Mild crowded (<3, ≥0) | 32 (64.0%) | 12.5 ± 6.5 | 0.009 ** (1 vs. 3) |
| Severe Crowded (≥3) | 10 (20.0%) | 23.7 ± 9.2 | 0.001 ** (2 vs. 3) |
| Mandible ALD (mm) | |||
| Spacing (<0) | 5 (10.0%) | 18.6 ± 13.8 | 0.266 (1 vs. 2) |
| Mild crowded (<3, ≥0) | 32 (64.0%) | 12.9 ± 6.9 | 0.387 (1 vs. 3) |
| Severe crowded (≥3) | 13 (26.0%) | 18.6 ± 6.5 | 0.009 ** (2 vs. 3) |
| Curve of Spee (mm) | 0.126 | ||
| Mild (<2) | 13 (26.0%) | 12.2 ± 6.4 | |
| Severe (≥2) | 37 (74.0%) | 15.9 ± 8.4 | |
| Total ALD (mm) | 2.5 ± 2.3 | <0.001 ** | |
| Non-extraction | 41 (82.0%) | 12.8 ± 6.2 | |
| Extraction | 9 (18.0%) | 25.0 ± 7.8 | |
| Preoperative overbite (mm) | −1.8 ± 2.4 | ||
| Preoperative overjet (mm) | 0.53 ± 1.6 | ||
| IMW difference (mm) | 5.7 ± 2.6 | ||
| ICW difference (mm) | 8.9 ± 2.4 |
| Variables | N (%) or Mean ± SD | Treatment Time (Months) | p-Value |
|---|---|---|---|
| Anteroposterior relationship | |||
| Postoperative overjet (mm) | 3.6 ± 1.6 | 0.378 | |
| Mild (>4) | 31 (62.0%) | 14.6 ± 9.0 | |
| Severe (≤4) | 19 (38.0%) | 15.6 ± 6.2 | |
| Postoperative molar key | |||
| Class I | 25 (50.0%) | 10.8 ± 5.2 | 0.002 ** (1 vs. 2) |
| Class II | 15 (30.0%) | 16.6 ± 6.3 | <0.001 ** (1 vs. 3) |
| Class III | 10 (20.0%) | 23.0 ± 9.5 | 0.062 (2 vs. 3) |
| Vertical relationship | |||
| Postoperative overbite (mm) | 0.9 ± 1.6 | ||
| Postoperative anterior open bite | 0.007 ** | ||
| No | 32 (64.0%) | 12.8 ± 6.8 | |
| Yes | 18 (36.0%) | 18.9 ± 8.7 | |
| No. of contact points | 4.3 ± 1.4 | ||
| Contact type | |||
| Bilateral anterior and posterior (>4 points) | 18 (36.0%) | 8.6 ± 3.4 | <0.001 ** (1 vs. 2) |
| Bilateral anterior and posterior (≤4 points) | 20 (40.0%) | 18.3 ± 8.4 | <0.001 ** (1 vs. 3) |
| Bilateral posterior | 12 (24.0%) | 19.1 ± 6.3 | 0.470 (2 vs. 3) |
| Transverse relationship | |||
| Postoperative dental midline | <0.001 ** | ||
| Non-deviated | 26 (52.0%) | 11.1 ± 5.6 | |
| Deviated | 24 (48.0%) | 19.2 ± 8.2 | |
| Maxillary expansion | 0.035 * | ||
| Not performed | 38 (76.0%) | 13.7 ± 7.8 | |
| Performed | 12 (24.0%) | 18.9 ± 7.7 |
| Model (Adjusted R2 = 0.79) | Unstandardized Coefficient | Standardized Coefficient | Collinearity Statistics | ||||
|---|---|---|---|---|---|---|---|
| B | SE | Beta | t | p | Tolerance | VIF | |
| (constant) | 21.21 | 3.37 | 6.29 | <0.001 ** | |||
| No. of contact points | −2.22 | 0.64 | −0.39 | −3.46 | 0.001 ** | 0.66 | 1.53 |
| No. of extracted teeth | 2.87 | 0.78 | 0.38 | 3.67 | 0.001 ** | 0.78 | 1.29 |
| Postoperative midline deviation (yes/no) | 4.50 | 1.56 | 0.29 | 2.88 | 0.006 ** | 0.82 | 1.21 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.-Y.; Park, J.H.; Jung, H.-D.; Jung, Y.-S. Factors Affecting Total Treatment Time in Patients Treated with Orthognathic Surgery Using the Surgery-First Approach: Multivariable Analysis Using 3D CT and Scanned Dental Casts. J. Clin. Med. 2020, 9, 641. https://doi.org/10.3390/jcm9030641
Kim J-Y, Park JH, Jung H-D, Jung Y-S. Factors Affecting Total Treatment Time in Patients Treated with Orthognathic Surgery Using the Surgery-First Approach: Multivariable Analysis Using 3D CT and Scanned Dental Casts. Journal of Clinical Medicine. 2020; 9(3):641. https://doi.org/10.3390/jcm9030641
Chicago/Turabian StyleKim, Jun-Young, Jin Hoo Park, Hwi-Dong Jung, and Young-Soo Jung. 2020. "Factors Affecting Total Treatment Time in Patients Treated with Orthognathic Surgery Using the Surgery-First Approach: Multivariable Analysis Using 3D CT and Scanned Dental Casts" Journal of Clinical Medicine 9, no. 3: 641. https://doi.org/10.3390/jcm9030641
APA StyleKim, J.-Y., Park, J. H., Jung, H.-D., & Jung, Y.-S. (2020). Factors Affecting Total Treatment Time in Patients Treated with Orthognathic Surgery Using the Surgery-First Approach: Multivariable Analysis Using 3D CT and Scanned Dental Casts. Journal of Clinical Medicine, 9(3), 641. https://doi.org/10.3390/jcm9030641





