Cervical Myelopathy in Patients Suffering from Rheumatoid Arthritis—A Case Series of 9 Patients and A Review of the Literature
Abstract
:1. Introduction
2. Methods
3. Results
Illustrative Case (2)
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
Abbreviations
| RA | rheumatoid arthritis |
| CS | cranial settling |
| ASS | atlantoaxial subluxation |
| AAI | atlantoaxial instability |
| mJOA | modified Japanese orthopaedic association scale |
| SAS | subaxial subluxation |
| AADI | anterior atlantodental Interval |
| PADI | posterior atlantodental interval |
| VT | vertical translocation |
| CT | computer tomography |
| MRI | magnetic resonance tomography |
References
- Carotti, M.; Salaffi, F.; di Carlo, M.; Sessa, F.; Giovagnoni, A. Magnetic resonance imaging of the craniovertebral junction in early rheumatoid arthritis. Skelet. Radiol. 2019, 48, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Certo, F.; Maione, M.; Visocchi, M.; Barbagallo, G.M.V. Retro-odontoid Degenerative Pseudotumour Causing Spinal Cord Compression and Myelopathy: Current Evidence on the Role of Posterior C1-C2 Fixation in Treatment. Acta Neurochir. Suppl. 2019, 125, 259–264. [Google Scholar] [PubMed]
- Gillick, J.L.; Wainwright, J.; Das, K. Rheumatoid Arthritis and the Cervical Spine: A Review on the Role of Surgery. Int. J. Rheumatol. 2015, 2015, 252456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joaquim, A.F.; Appenzeller, S. Cervical spine involvement in rheumatoid arthritis—A systematic review. Autoimmun. Rev. 2014, 13, 1195–1202. [Google Scholar] [CrossRef] [PubMed]
- Wasserman, B.R.; Moskovich, R.; Razi, A.E. Rheumatoid arthritis of the cervical spine—Clinical considerations. Bull. NYU Hosp. Joint. Dis. 2011, 69, 136–148. [Google Scholar]
- Joaquim, A.F.; Ghizoni, E.; Tedeschi, H.; Appenzeller, S.; Riew, K.D. Radiological evaluation of cervical spine involvement in rheumatoid arthritis. Neurosurg. Focus 2015, 38, E4. [Google Scholar] [CrossRef]
- Manczak, M.; Gasik, R. Cervical spine instability in the course of rheumatoid arthritis—Imaging methods. Reumatologia 2017, 55, 201–207. [Google Scholar] [CrossRef] [Green Version]
- Sunahara, N.; Matsunaga, S.; Mori, T.; Ijiri, K.; Sakou, T. Clinical course of conservatively managed rheumatoid arthritis patients with myelopathy. Spine 1997, 22, 2603–2607; discussion 2608. [Google Scholar] [CrossRef]
- Neva, M.H.; Kaarela, K.; Kauppi, M. Prevalence of radiological changes in the cervical spine—A cross sectional study after 20 years from presentation of rheumatoid arthritis. J. Rheumatol. 2000, 27, 90–93. [Google Scholar]
- Del Grande, M.; del Grande, F.; Carrino, J.; Bingham, C.O., 3rd; Louie, G.H. Cervical spine involvement early in the course of rheumatoid arthritis. Semin. Arthritis Rheum. 2014, 43, 738–744. [Google Scholar] [CrossRef]
- Kothe, R.; Wiesner, L.; Ruther, W. Rheumatoid arthritis of the cervical spine. Current concepts for diagnosis and therapy. Orthopade 2002, 31, 1114–1122. [Google Scholar] [CrossRef] [PubMed]
- Stein, B.E.; Hassanzadeh, H.; Jain, A.; Lemma, M.A.; Cohen, D.B.; Kebaish, K.M. Changing trends in cervical spine fusions in patients with rheumatoid arthritis. Spine 2014, 39, 1178–1182. [Google Scholar] [CrossRef] [PubMed]
- Mikulowski, P.; Wollheim, F.A.; Rotmil, P.; Olsen, I. Sudden death in rheumatoid arthritis with atlanto-axial dislocation. Acta Med. Scand. 1975, 198, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Keller, A.; von Ammon, K.; Klaiber, R.; Waespe, W. Spondylogenic cervical myelopathy: Conservative and surgical therapy. Schweiz. Med. Wochenschr. 1993, 123, 1682–1691. [Google Scholar] [PubMed]
- Bhatti, A.B.; Kim, S. Application of the Harms Technique to Treat Undiagnosed Intractable C1-C2 Unilateral Neck Pain: A Case Report. Cureus 2016, 8, e793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nannapaneni, R.; Behari, S.; Todd, N.V. Surgical outcome in rheumatoid Ranawat Class IIIb myelopathy. Neurosurgery 2005, 56, 706–715; discussion 706–715. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.I.; Han, M.H.; Cheong, J.H.; Kim, J.M.; Kim, C.H.; Chun, H.J.; HumBak, K. The Effects of Clinical Factors and Retro-Odontoid Soft Tissue Thickness on Atlantoaxial Instability in Patients with Rheumatoid Arthritis. World Neurosurg. 2017, 103, 364–370. [Google Scholar] [CrossRef]
- Nguyen, H.V.; Ludwig, S.C.; Silber, J.; Gelb, D.E.; Anderson, P.A.; Frank, L.; Vaccaro, A.R. Rheumatoid arthritis of the cervical spine. Spine J. 2004, 4, 329–334. [Google Scholar] [CrossRef]
- Dohzono, S.; Suzuki, A.; Koike, T.; Takahashi, S.; Yamada, K.; Yasuda, H.; Yasuda, H.; Nakamura, H. Factors associated with retro-odontoid soft-tissue thickness in rheumatoid arthritis. J. Neurosurg. Spine 2016, 25, 580–585. [Google Scholar] [CrossRef] [Green Version]
- Matsunaga, S.; Sakou, T.; Onishi, T.; Hayashi, K.; Taketomi, E.; Sunahara, N.; Komiya, S. Prognosis of patients with upper cervical lesions caused by rheumatoid arthritis: Comparison of occipitocervical fusion between c1 laminectomy and nonsurgical management. Spine 2003, 28, 1581–1587; discussion 1587. [Google Scholar] [CrossRef]
- Terashima, Y.; Yurube, T.; Hirata, H.; Sugiyama, D.; Sumi, M.; Spinal, D.H.O. Predictive Risk Factors of Cervical Spine Instabilities in Rheumatoid Arthritis: A Prospective Multicenter Over 10-Year Cohort Study. Spine 2017, 42, 556–564. [Google Scholar] [CrossRef]
- Zhu, S.; Xu, W.; Luo, Y.; Zhao, Y.; Liu, Y. Cervical spine involvement risk factors in rheumatoid arthritis: A meta-analysis. Int. J. Rheum. Dis. 2017, 20, 541–549. [Google Scholar] [CrossRef]
- Werle, S.; Ezzati, A.; ElSaghir, H.; Boehm, H. Is inclusion of the occiput necessary in fusion for C1-2 instability in rheumatoid arthritis? J. Neurosurg. Spine 2013, 18, 50–56. [Google Scholar] [CrossRef]
- Grob, D.; Jeanneret, B.; Aebi, M.; Markwalder, T.M. Atlanto-axial fusion with transarticular screw fixation. J. Bone Joint. Surg. Br. 1991, 73, 972–976. [Google Scholar] [CrossRef]
- Lee, S.H.; Kim, E.S.; Sung, J.K.; Park, Y.M.; Eoh, W. Clinical and radiological comparison of treatment of atlantoaxial instability by posterior C1-C2 transarticular screw fixation or C1 lateral mass-C2 pedicle screw fixation. J. Clin. Neurosci. 2010, 17, 886–892. [Google Scholar] [CrossRef]
- Goldschlager, T.; Hartl, R.; Greenfield, J.P.; Anand, V.K.; Schwartz, T.H. The endoscopic endonasal approach to the odontoid and its impact on early extubation and feeding. J. Neurosurg. 2015, 122, 511–518. [Google Scholar] [CrossRef] [Green Version]
- Komotar, R.J.; Starke, R.M.; Raper, D.M.; Anand, V.K.; Schwartz, T.H. Endoscopic endonasal compared with anterior craniofacial and combined cranionasal resection of esthesioneuroblastomas. World Neurosurg. 2013, 80, 148–159. [Google Scholar] [CrossRef]
- Gempt, J.; Lehmberg, J.; Grams, A.E.; Berends, L.; Meyer, B.; Stoffel, M. Endoscopic transnasal resection of the odontoid: Case series and clinical course. Eur. Spine J. 2011, 20, 661–666. [Google Scholar] [CrossRef] [Green Version]
- Neva, M.H.; Hakkinen, A.; Makinen, H.; Hannonen, P.; Kauppi, M.; Sokka, T. High prevalence of asymptomatic cervical spine subluxation in patients with rheumatoid arthritis waiting for orthopaedic surgery. Ann. Rheum. Dis. 2006, 65, 884–888. [Google Scholar] [CrossRef] [Green Version]


| Type of Instability | Definition and Diagnostics of Cervical Instabilities | |
|---|---|---|
| Definition | Diagnostic in Radiograph/Scan in Lateral/Sagittal Projection | |
| AAS (atlantoaxial subluxation) | weakening or rupture of ligaments and subchondral bone erosion in the atlantoaxial joints | anterior atlantodental Interval (AADI) > 3 mm posterior atlantodental interval (PADI) < 14 mm |
| SAS (subaxial subluxation) | subluxation in the joints C3-7 due to destruction of the joint surface and the ligaments between the processes spinosis | horizontal displacement of vertebrae with irreducible translation > 3.5 mm |
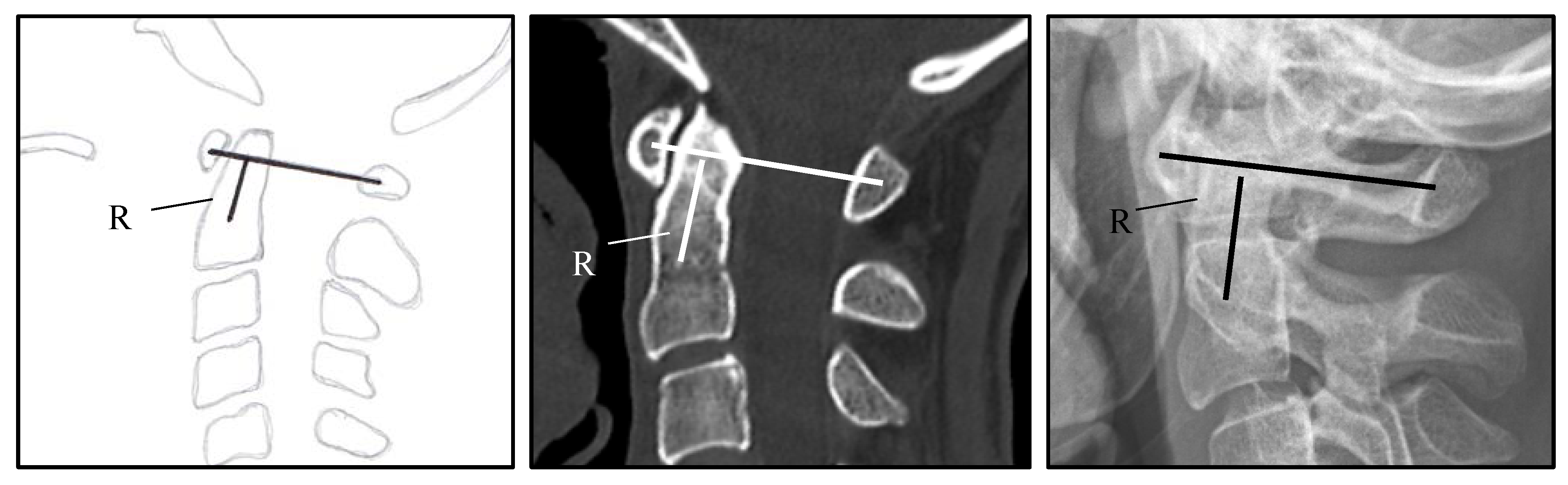
| CS (Cranial Settling) | vertical translocation of dens into the foramen magnum | see Figure 1 and Figure 2 |
| Prevalence of Cervical Involvement in RA | % |
|---|---|
| Pain in the cranio-cervical junction | 69% of patients with cervical instability |
| Muscular atrophy, paresis, bladder rectal disorders, pathological reflexes and spasticity | present in up to 58% of all cases |
| Involvement of the cranial nerves | reported in about 20% |
| Initially asymptomatic | 33–50% |
| Atlantoaxial subluxation with myelopathy | circa 2.5% of patients with RA for more than 14 years |
| Locked-in syndrome or sudden death | rare but reported up to 10% in a postmortem study [13] |
| Vertebrobasilar insufficiency with tinnitus and dizziness due to Mechanical compression/ vertebrobasilar thromboembolic events due to kinking of vertebral arteries | rare |
| Aseptic discitis and atraumatic dens fractures | rare |
| Class | Description |
|---|---|
| I | Pain, no neurological deficit |
| II | Subjective weakness, hyperreflexia, dysesthesia |
| III | Objective weakness, long-tract signs III A—Ambulatory, III B—Non-ambulatory |
| Case | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 |
|---|---|---|---|---|---|---|---|---|---|
| Sex/age | m/80 | w/22 | w/82 | m/76 | m/73 | w/71 | m/48 | w/81 | w/50 |
| Cervical pathology | AAI, retrodental pannus | AAS | AAI, retrodental pannus | CS | AAI, retrodental pannus, cervical spinal stenosis subaxial | AAI, retrodental pannus | AAS, retrodental pannus | CS | CS |
| Pre-operative mJOA - score | 9 | 12 | 15 | 8 | 15 | 16 | 14 | 11 | 14 |
| Ranawat - criteria | 15.5 | 10.7 | 12 | 8.3 | 12.1 | * | 13.5 | 9.5 | * |
| Smallest diameter of canal anterior - posterior (mm) | 1.9 | 4 | 5.4 | 5.9 | 7.2 | * | 5.1 | 5.5 | * |
| ADI (mm) | 0.2 | 9.7 | 0.3 | 1.3 | 1.4 | * | 13.0 | 0.8 | * |
| Ranawat classification | IIIA | IIIA | IIIA | IIIB | IIIA | II | II | IIIB | IIIA |
| Rheumatoid arthritis/treatment | suspicion of RA | RA/Adalimumab every 2 weeks | suspicion of RA | RA/MTX every week, folic acid, steroids | suspicion of RA | suspicion of RA | RA (ED 1995)/MTX 1 every week, steroids | RA since 30 years/steroids | suspicion of RA |
| Symptoms | neck pain, ataxia, hemiparesie, not able to walk | fine motor disorders, monoparesis, bladder emptying disorders, ataxia | monoparesis | tertaparesis, not able to walk, dysphagia, loss of warm cold discrimination of the legs | monoparesie, ataxie | neck pain, ataxie | ataxie, sensory deficit | dysphagia, tetraparesie, not able to walk | ataxie, dysphagia, sensory deficit |
| Surgery | 1. posterior fixation C1-3 + laminectomy C1-2 2. transnasal endoscopic dens resection | closed reduction, osterior fixation C1-2 | posterior fixation C1-2, laminectomy C1 | posterior fixation C0-2-3-4 | posterior fixation C1-2-4-6 + laminectomy C1-6 | posterior fixation C1-2 | posterior fixation C1-2 | posterior fixation C0-3-4, laminectomy C1, decompression suboccipital | 1. posterior fixation C0-2, decompression suboccipital 2. transnasal endoscopic resection of dens and clivus (21 months later) |
| Complications | temporary hemiplegie postoperatively | no | no | deceased | No | no | no | no | no |
| Follow up | after 8 months, improvement of hemipaesis, walking possible with aide | after 12 months, no symptoms | no follow up | no follow up | no follow up | no follow up | 11 months | after 3 months, walking possible | after 5 years |
| Post-operative mJOA score | 12 | 17 | 15 | deceased | 15 | 16 | 16 | 12 | 16 |
| Number of Patients/Sex | n = 9 (Female n = 5; Male n = 4) |
|---|---|
| Mean age | 64.8 ± 20.5 years (range 22–82 years) |
| Cervical pathology | AAI with retrodental pannus, n = 4 Anterior AAS, n = 2 Basilar invagination, n = 3 Associated subaxial spinal stenosis n = 2 |
| Myelopathy | n = 9 |
| Additional neurological deficit | Tetraparesis (n = 2) Hemi-or monoparesis (n = 4) Incontinence (n = 1) Pain (n = 4) Dysphagia (n = 3) |
| Pre-operative mJOA- score (mean) | 12.67 ± 2.83 (range 8–16) |
| Ranawat classification | Class II n = 2 Class IIIA n = 5 Class IIIB n = 2 |
| Surgery | posterior fixation, n = 9 C1-2, n = 4; C1-6, n = 1 C1-3, n = 1; C0-2, n = 1 C0-3, n = 1; C0-4, n = 1 posterior decompression, n = 6 transnasal endoscopic dens resection, n = 2 |
| Follow up | mean follow-up at 18.8 ± 23.3 months (range 3–60 months) |
| Post-operative mJOA score (mean) * | 14.6 ± 1.89 (range 12–17) |
| Mortality | 11.1% (n = 1) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Janssen, I.; Nouri, A.; Tessitore, E.; Meyer, B. Cervical Myelopathy in Patients Suffering from Rheumatoid Arthritis—A Case Series of 9 Patients and A Review of the Literature. J. Clin. Med. 2020, 9, 811. https://doi.org/10.3390/jcm9030811
Janssen I, Nouri A, Tessitore E, Meyer B. Cervical Myelopathy in Patients Suffering from Rheumatoid Arthritis—A Case Series of 9 Patients and A Review of the Literature. Journal of Clinical Medicine. 2020; 9(3):811. https://doi.org/10.3390/jcm9030811
Chicago/Turabian StyleJanssen, Insa, Aria Nouri, Enrico Tessitore, and Bernhard Meyer. 2020. "Cervical Myelopathy in Patients Suffering from Rheumatoid Arthritis—A Case Series of 9 Patients and A Review of the Literature" Journal of Clinical Medicine 9, no. 3: 811. https://doi.org/10.3390/jcm9030811
APA StyleJanssen, I., Nouri, A., Tessitore, E., & Meyer, B. (2020). Cervical Myelopathy in Patients Suffering from Rheumatoid Arthritis—A Case Series of 9 Patients and A Review of the Literature. Journal of Clinical Medicine, 9(3), 811. https://doi.org/10.3390/jcm9030811






