A Multicenter Study into Burnout, Perceived Stress, Job Satisfaction, Coping Strategies, and General Health among Emergency Department Nursing Staff
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Settings
2.3. Participants and Sample
2.4. Data Collection
2.5. Ethical Considerations
2.6. Data Analysis
3. Results
3.1. Characteristics of Participants
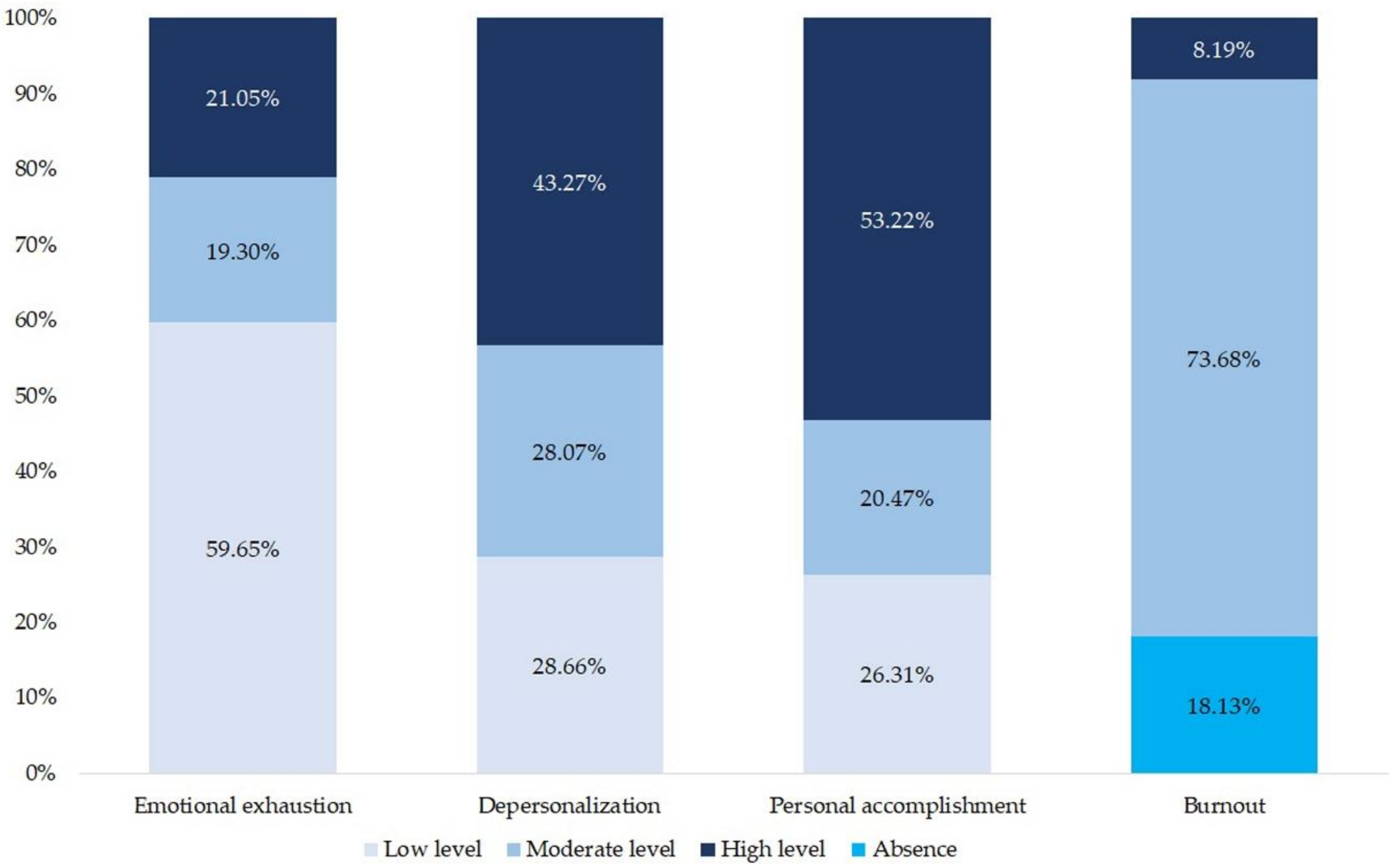
3.2. Descriptive Analysis of Burnout
3.3. Descriptive and Correlational Analysis of Burnout, Perceived Stress, Job Satisfaction, Coping Strategies, and General Health
3.4. Comparative Analysis of Sociodemographic, Occupational Characteristics, and The Dimensions of Burnout
3.5. Multivariate Linear Regression Models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef] [PubMed]
- International Classification of Diseases 11th Revision (ICD-11): The Global Standard for Diagnostic Health Information. Available online: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281 (accessed on 17 March 2020).
- Cañadas de la Fuente, G.A.; San Luis, C.; Lozano, L.M.; Vargas, C.; García, I.; De la Fuente, E.I. Evidencia de validez factorial del Maslach Burnout Inventory y estudio de los niveles de burnout en profesionales sanitarios. Rev. Latinoam. Psicol. 2014, 46, 44–52. [Google Scholar] [CrossRef]
- Van Mol, M.M.C.; Kompanje, E.J.O.; Benoit, D.D.; Bakker, J.; Nijkamp, M.D. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: A systematic review. PLoS ONE 2015, 10, e0136955. [Google Scholar] [CrossRef] [PubMed]
- Ortega Ruiz, C.; López Ríos, F. El burnout o síndrome de estar quemado en los profesionales sanitarios: Revisión y perspectivas. Int. J. Clin. Health Psychol. 2004, 4, 137–160. [Google Scholar]
- Cañadas de la Fuente, G.A.; Vargas, C.; San Luis, C.; García, I.; Cañadas de la Fuente, G.R.; De la Fuente, E.I. Risk factors and prevalence of burnout syndrome in the nursing profession. Int. J. Nurs. Stud. 2015, 52, 240–249. [Google Scholar] [CrossRef]
- Wu, S.; Singh-Carlson, S.; Odell, A.; Reynolds, G.; Su, Y. Compassion fatigue, burnout, and compassion satisfaction among oncology nurses in the United States and Canada. Oncol. Nurs. Forum 2016, 43, E161–E169. [Google Scholar] [CrossRef]
- Ramírez Baena, L.; Ortega Campos, E.; Gómez Urquiza, J.L.; Cañadas de la Fuente, G.R.; De la Fuente, E.I. A multicentre study of burnout prevalence and related psychological variables in medical area hospital nurses. J. Clin. Med. 2019, 8, 92. [Google Scholar] [CrossRef]
- Albendín García, L.; Gómez Urquiza, J.L.; Cañadas de la Fuente, G.A.; San Luis, C.; Aguayo, R. Prevalencia bayesiana y niveles de burnout en enfermería de urgencias. Una revision sistemática. Rev. Latinoam. Psicol. 2016, 48, 137–145. [Google Scholar] [CrossRef]
- Gómez Urquiza, J.L.; De la Fuente, E.I.; Albendín García, L.; Vargas, C.; Ortega Campos, E.M.; Cañadas de la Fuente, G.A. Prevalence of burnout syndrome in emergency nurses: A meta-analysis. Crit. Care Nurse 2017, 37, e1–e9. [Google Scholar] [CrossRef]
- Adriaenssens, J.; De Gucht, V.; Maes, S. Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. Int. J. Nurs. Stud. 2015, 52, 649–661. [Google Scholar] [CrossRef] [PubMed]
- Gómez Urquiza, J.L.; Monsalve Reyes, C.S.; San Luis, C.; Fernández Castillo, R.; Aguayo, R.; Cañadas de la Fuente, G.A. Factores de riesgo y niveles de burnout en enfermeras de atención primaria: Una revisión sistemática. Aten. Primaria 2017, 49, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Pradas Hernández, L.; Ariza, T.; Gómez Urquiza, J.L.; Albendín García, L.; De la Fuente, E.I.; Cañadas de la Fuente, G.A. Prevalence of burnout in paediatric nurses: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0195039. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad Servicios Sociales e Igualdad; Instituto Nacional de Estadística. Encuesta Nacional de Salud España ENSE 2017; Madrid, Ministerio de Sanidad Servicios Sociales e Igualdad. 2018. Available online: https://www.ine.es/dynt3/inebase/es/index.htm?type=pcaxis&path=/t15/p419/a2017/p02/&file=pcaxis (accessed on 17 March 2020).
- Ministerio de Sanidad Servicios Sociales e Igualdad; Instituto Nacional de Estadística. Encuesta Nacional de Salud España ENSE 2011/12; Madrid, Ministerio de Sanidad Servicios Sociales e Igualdad. 2013. Available online: https://www.ine.es/dynt3/inebase/es/index.htm?type=pcaxis&path=/t15/p419/a2011/p02/&file=pcaxis (accessed on 17 March 2020).
- Elder, E.; Johnston, A.N.; Wallis, M.; Greenslade, J.H.; Crilly, J. Emergency clinician perceptions of occupational stressors and coping strategies: A multi-site study. Int. Emerg. Nurs. 2019, 45, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Howlett, M.; Doody, K.; Murray, J.; LeBlanc-Duchin, D.; Fraser, J.; Atkinson, P.R. Burnout in emergency department healthcare professionals is associated with coping style: A cross-sectional survey. Emerg. Med. J. 2015, 32, 722–727. [Google Scholar] [CrossRef] [PubMed]
- International Labour Organization: Workplace Stress: A Collective Challenge. Available online: https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---safework/documents/publication/wcms_466547.pdf (accessed on 24 March 2020).
- Ríos Risquez, M.I.; García Izquierdo, M. Patient satisfaction, stress and burnout in nursing personnel in emergency departments: A cross-sectional study. Int. J. Nurs. Stud. 2016, 59, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Loeppke, R.; Heron, R.; Bazas, T.; Beaumont, D.; Spanjaard, H.; Konicki, D.L.; Eisenberg, B.; Todd, H. Global trends in occupational medicine: Results of the International Occupational Medicine Society Collaborative Survey. J. Occup. Environ. Med. 2017, 59, e13–e16. [Google Scholar] [CrossRef]
- Johansen, M.L.; Cadmus, E. Conflict management style, supportive work environments and the experience of work stress in emergency nurses. J. Nurs. Manag. 2016, 24, 211–218. [Google Scholar] [CrossRef]
- Lu, D.M.; Sun, N.; Hong, S.; Fan, Y.Y.; Kong, F.Y.; Li, Q.J. Occupational stress and coping strategies among emergency department nurses of China. Arch. Psychiatr. Nurs. 2015, 29, 208–212. [Google Scholar] [CrossRef]
- Salvagioni, D.A.; Melanda, F.N.; Mesas, A.E.; González, A.D.; Gabani, F.L.; de Andrade, S.M. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLoS ONE 2017, 12, e0185781. [Google Scholar] [CrossRef]
- Khamisa, N.; Peltzer, K.; Ilic, D.; Oldenburg, B. Work related stress, burnout, job satisfaction and general health of nurses: A follow-up study. Int. J. Nurs. Pract. 2016, 22, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Zhao, Y.; While, A. Job satisfaction among hospital nurses: A literature review. Int. J. Nurs. Stud. 2019, 94, 21–31. [Google Scholar] [CrossRef]
- Locke, E.A. The nature and causes of job satisfaction. In Handbook of Industrial and Organizational Psychology, 1st ed.; Dunnette, M.D., Ed.; John Wiley & Sons: New York, NY, USA, 1976; pp. 1297–1349. [Google Scholar]
- Suárez, M.; Asenjo, M.; Sánchez, M. Job satisfaction among emergency department staff. Australas. Emerg. Nurs. J. 2017, 20, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Yasin, Y.M.; Kerr, M.S.; Wong, C.A.; Bélanger, C.H. Factors affecting nurses’ job satisfaction in rural and urban acute care settings: A PRISMA systematic review. In Proceedings of the Western Research Forum, London, ON, Canada, 22 March 2019; Society of Graduate Students (SOGS) at Western University: London, ON, Canada, 2019. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Shin, H.; Park, Y.M.; Ying, J.Y.; Kim, B.; Noh, H.; Lee, S.M. Relationships between coping strategies and burnout symptoms: A meta-analytic approach. Prof. Psychol. Res. Pract. 2014, 45, 44–56. [Google Scholar] [CrossRef]
- Frydenberg, E. Coping research: Historical background, links with emotion, and new research directions on adaptive processes. Aust. J. Psychol. 2014, 66, 82–92. [Google Scholar] [CrossRef]
- Umeh, K. Cognitive appraisals, maladaptive coping, and past behaviour in protection motivation. Psychol. Health 2004, 19, 719–735. [Google Scholar] [CrossRef]
- Trinkoff, A.M.; Storr, C.L. Substance use among nurses: Differences between specialties. Am. J. Public Health 1998, 10, 77–84. [Google Scholar]
- Hamilton, S.; Tran, V.; Jamieson, J. Compassion fatigue in emergency medicine: The cost of caring. Emerg. Med. Australas. 2016, 28, 100–103. [Google Scholar] [CrossRef] [PubMed]
- International Labour Office (ILO/BIT). Workplace Stress. A Collective Challenge; ILO: Turin, Italy, 2016. [Google Scholar]
- Maslach, C.; Jackson, S.E. MBI: Maslach Burnout Inventory. Manual, 1st ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1981. [Google Scholar]
- Seisdedos, N. MBI. Inventario Burnout de Maslach: Manual, 1st ed.; TEA Ediciones: Madrid, Spain, 1997. [Google Scholar]
- Fernández, O.; Hidalgo, C.; Martín, A.; Moreno, S.; García del Río, B. Burnout en médicos residentes que realizan guardias en un servicio de urgencias. Emergencias 2007, 19, 116–121. [Google Scholar]
- Merces, M.C.D.; Coelho, J.M.; Lua, I.; Silva, D.D.; Gomes, A.M.T.; Erdmann, A.L.; Oliveira, D.C.; Lago, S.B.; Santana, A.I.C.; Silva, D.A.R.D.; et al. Prevalence and factors associated with burnout syndrome among primary health care nursing professionals: A cross-sectional study. Int. J. Environ. Res. Public Health 2020, 17, e474. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarch, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Remor, E.; Carrobles, J.A. Versión Española de la escala de estrés percibido (PSS-14): Estudio psicométrico en una muestra de VIH+. Ansiedad y Estrés 2001, 7, 195–201. [Google Scholar]
- Aranaz, J.M.; Mira, J.J. Cuestionario Font-Roja. Un instrumento de medida de la satisfacción en el medio hospitalario. Todo Hosp. 1988, 52, 63–68. [Google Scholar]
- Morán, C.; Landero, R.; González, M.T. COPE-28: Un análisis psicométrico de la versión en español del Brief COPE. Univ. Psychol. 2009, 9, 543–552. [Google Scholar] [CrossRef]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Hillier, V.F. A scaled version of the General Health Questionnaire. Psychol. Med. 1979, 9, 139–145. [Google Scholar] [CrossRef]
- Lobo, A.; Pérez Echeverría, M.J.; Artal, J. Validity of the scaled version of the General Health Questionnaire (GHQ-28) in a Spanish population. Psychol. Med. 1986, 16, 135–140. [Google Scholar] [CrossRef]
- Zou, Z.; Zhou, B.; Huang, Y.; Wang, J.; Xinghong, L.I.; Ying, H.E. The relationship between job burnout and social support in medical staff. Chin. J. Behav. Med. Brain Sci. 2015, 24, 169–172. [Google Scholar]
- Mirhaghi, M.; Sarabien, S. Relationship between perceived stress and personality traits in emergency medical personnel. J. Fund. Ment. Health 2016, 18, 265–271. [Google Scholar]
- Hutchinson, T.A.; Haase, S.; French, S.; McFarlane, T.A. Stress, burnout and coping among emergency physicians at a major hospital in Kingston, Jamaica. West Indian Med. J. 2014, 63, 262–266. [Google Scholar] [CrossRef]
- Wong, M.; Anderson, J.; Knorr, T.; Joseph, J.; Sánchez, L. Grit, anxiety, and stress in emergency physicians. Am. J. Emerg. Med. 2018, 36, 1036–1039. [Google Scholar] [CrossRef] [PubMed]
- Basu, S.; Yap, C.; Mason, S. Examining the sources of occupational stress in an emergency department. Occup. Med. (Lond.) 2016, 66, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Nespereira Campuzano, T.; Vázquez Campo, M. Emotional intelligence and stress management in Nursing professionals in a hospital emergency department. Enferm. Clin. 2017, 27, 172–178. [Google Scholar] [CrossRef]
- Hunsaker, S.; Chen, H.C.; Maughan, D.; Heaston, S. Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. J. Nurs. Scholarsh. 2015, 47, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Rozo, J.A.; Olson, D.M.; Thu, H.S.; Stutzman, S.E. Situational factors associated with burnout among emergency department nurses. Workplace Health Saf. 2017, 65, 262–265. [Google Scholar] [CrossRef]
- Adriaenssens, J.; De Gucht, V.; Maes, S. Causes and consequences of occupational stress in emergency nurses, a longitudinal study. J. Nurs. Manag. 2015, 23, 346–358. [Google Scholar] [CrossRef]
- Xiao, Y.; Wang, J.; Chen, S.; Wu, Z.; Cai, J.; Weng, Z.; Li, C.; Zhang, X. Psychological distress, burnout level and job satisfaction in emergency medicine: A cross-sectional study of physicians in China. Emerg. Med. Australas. 2014, 26, 538–542. [Google Scholar] [CrossRef]
- Caricati, L.; Sala, R.L.; Marletta, G.; Pelosi, G.; Ampollini, M.; Fabbri, A.; Ricchi, A.; Scardino, M.; Artioli, G.; Mancini, T. Work climate, work values and professional commitment as predictors of job satisfaction in nurses. J. Nurs. Manag. 2014, 22, 984–994. [Google Scholar] [CrossRef] [PubMed]
- Atefi, N.; Abdullah, K.L.; Wong, L.P.; Mazlom, R. Factors influencing registered nurses’ perception of their overall job satisfaction: A qualitative study. Int. Nurs Rev. 2014, 61, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Hooper, C.; Craig, J.; Janvrin, D.R.; Wetsel, M.A.; Reimels, E. Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected inpatient specialties. J. Emerg. Nurs. 2010, 36, 420–427. [Google Scholar] [CrossRef]
- Choi, S.E.; Kim, S.D. A meta-analysis of the variables related to job satisfaction among Korean nurses. Contemp. Nurse 2016, 52, 462–476. [Google Scholar] [CrossRef] [PubMed]
- Tavakoli, N.; Shaker, S.H.; Soltani, S.; Abbasi, M.; Amini, M.; Tahmasebi, A.; Kasnavieh, S.M.H. Job burnout, stress, and satisfaction among emergency nursing staff after health system transformation plan in Iran. Emerg. (Tehran). 2018, 6, e41. [Google Scholar]
- Ríos Rísquez, M.I.; Godoy Fernández, C.; Sánchez Meca, J. Síndrome de quemarse por el trabajo, personalidad resistente y malestar psicológico en personal de enfermería. An. Psicol. 2011, 27, 71–79. [Google Scholar]
- Abraham, L.J.; Thom, O.; Greenslade, J.H.; Wallis, M.; Johnston, A.N.B.; Carlström, E.; Mills, D.; Crilly, J. Morale, stress and coping strategies of staff working in the emergency department: A comparison of two different-sized departments. Emerg. Med. Australas. 2018, 30, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Marco, C.A.; Broderick, K.; Smith Coggins, R.; Goyal, D.G.; Joldersma, K.B.; Coombs, A.B. Health and wellness among emergency physicians: Results of the 2014 ABEM longitudinal study. Am. J. Emerg. Med. 2016, 34, 1715–1716. [Google Scholar] [CrossRef]
- Ianello, P.; Balzarotti, S. Stress and coping strategies in the emergency room. Emerg. Care J. 2014, 10, 72–75. [Google Scholar] [CrossRef]
- Kerai, S.M.; Khan, U.R.; Islam, M.; Asad, N.; Razzak, J.; Pasha, O. Post-traumatic stress disorder and its predictors in emergency medical service personnel: A cross-sectional study from Karachi, Pakistan. BMC Emerg. Med. 2017, 17, 26–32. [Google Scholar] [CrossRef]
- Mendonça Ribeiro, R.; Alcalá Pompeo, D.; Pinto, M.H.; Mendonça Ribeiro, R.C.H. Coping strategies of nurses in hospital emergency care services. Acta Paul. Enferm. 2015, 28, 216–223. [Google Scholar] [CrossRef]
- Hershcovis, M.S.; Cameron, A.F.; Gervais, L.; Bozeman, J. The effects of confrontation and avoidance coping in response to workplace incivility. J. Occup. Health Psychol. 2018, 23, 163–174. [Google Scholar] [CrossRef]
- Friganović, A.; Selič, P.; Ilić, B.; Sedić, B. Stress and burnout syndrome and their associations with coping and job satisfaction in critical care nurses: A literature review. Psychiatr. Danub. 2019, 31, 21–31. [Google Scholar]
- Cordes, C.L.; Dougherty, T.W. A review and an integration of research on job burnout. Acad. Manag. Rev. 1993, 18, 621–656. [Google Scholar] [CrossRef]
- Wallace, J.E.; Brinkerhoff, M.B. The measurement of burnout revisited. J. Soc. Serv. Res. 1991, 14, 85–111. [Google Scholar] [CrossRef]
- Yates, P.; Benson, E.V.; Harris, A.; Baron, R. An investigation of factors supporting the psychological health of staff in a UK emergency department. Emerg. Med. J. 2012, 29, 533–535. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, A.; Segesten, K. Guilt, shame and need for a container: A study of post-traumatic stress among ambulance personnel. Accid. Emerg. Nurs. 2004, 12, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Schooley, B.; Hikmet, N.; Tarcan, M.; Yorgancioglu, G. Comparing burnout across emergency physicians, nurses, technicians, and health information technicians working for the same organization. Medicine (Baltimore) 2016, 95, e2856. [Google Scholar] [CrossRef]
- Tarcan, M.; Hikmet, N.; Schooley, B.; Top, M.; Tarcan, G.Y. An analysis of the relationship between burnout, socio-demographic and workplace factors and job satisfaction among emergency department health professionals. Appl. Nurs. Res. 2017, 34, 40–47. [Google Scholar] [CrossRef]
- Kimo Takayesu, J.; Ramoska, E.A.; Clark, T.R.; Hansoti, B.; Dougherty, J.; Freeman, W.; Weaver, K.R.; Chang, Y.; Gross, E. Factors associated with burnout during emergency medicine residency. Acad. Emerg. Med. 2014, 21, 1031–1035. [Google Scholar] [CrossRef]
- Kim, J.S.; Choi, J.S. Factors influencing emergency nurses’ burnout during an outbreak of Middle East respiratory syndrome coronavirus in Korea. Asian Nurs. Res. 2016, 10, 295–299. [Google Scholar] [CrossRef]
- Soltanifar, A.; Pishbin, E.; Attaran Mashhadi, N.; Najaf Najafi, M.; Siahtir, M. Burnout among female emergency medicine physicians: A nationwide study. Emerg. Med. Australas. 2018, 30, 517–522. [Google Scholar] [CrossRef]
- Arora, M.; Asha, S.; Chinnappa, J.; Diwan, A.D. Review article: Burnout in emergency medicine physicians. Emerg. Med. Australas. 2013, 25, 491–495. [Google Scholar] [CrossRef]
- Gökçen, C.; Zengin, S.; Oktay, M.M.; Alpak, G.; Al, B.; Yildirim, C. Burnout, job satisfaction and depression in the healthcare personnel who work in the emergency department. Anadolu. Psikiyatri. Derg. 2013, 14, 112–128. [Google Scholar] [CrossRef]
- Lloyd, S.; Streiner, D.; Shannon, S. Burnout, depression, life and job satisfaction among Canadian emergency physicians. J. Emerg. Med. 1994, 12, 559–565. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Oreskovich, M.R. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch. Intern. Med. 2012, 172, 1377–1385. [Google Scholar] [CrossRef] [PubMed]
- Ben-Itzhak, S.; Dvash, J.; Maor, M.; Rosenberg, N.; Halpern, P. Sense of meaning as a predictor of burnout in emergency physicians in Israel: A national survey. Clin. Exp. Emerg. Med. 2015, 2, 217–225. [Google Scholar] [CrossRef]
- Goldberg, R.; Boss, R.W.; Chan, L.; Goldberg, J.; Mallon, W.K.; Moradzadeh, D.; Goodman, E.A.; McConkie, M.L. Burnout and its correlates in emergency physicians: Four years’ experience with a wellness booth. Acad. Emerg. Med. 1996, 3, 1156–1164. [Google Scholar] [CrossRef]
- Naczenski, L.M.; de Vries, J.D.; van Hooff, M.L.M.; Kompier, M.A.J. Systematic review of the association between physical activity and burnout. J. Occup. Health 2017, 59, 477–494. [Google Scholar] [CrossRef]
- Salazar, I.C.; Roldán, G.M.; Garrido, L.; Ramos-Navas Parejo, J.M. Assertiveness and its relationship to emotional problems and burnout in healthcare workers. Behav. Psychol. 2014, 22, 523–549. [Google Scholar]
- Popa, F.; Arafat, R.; Purcărea, V.L.; Lală, A.; Popa Velea, O.; Bobirnac, G. Occupational burnout levels in emergency medicine–a stage 2 nationwide study and analysis. J. Med. Life 2010, 3, 449–453. [Google Scholar]
- Atance, J.C. Aspectos epidemiológicos del síndrome de burnout en personal sanitario. Rev. Esp. Salud Publica 1997, 71, 293–303. [Google Scholar] [CrossRef]
- García Izquierdo, M.; Ríos Rísquez, M.I. The relationship between psychosocial job stress and burnout in emergency departments: An exploratory study. Nurs. Outlook 2012, 60, 322–329. [Google Scholar] [CrossRef]
| Variables | N = 171 n (%) |
|---|---|
| Sex | |
| Male | 46 (26.90) |
| Female | 125 (73.10) |
| Marital status | |
| Married | 39 (22.81) |
| Single | 103 (60.23) |
| Separated/divorced | 22 (12.87) |
| Widowed | 7 (4.09) |
| Daily physical exercise | |
| Yes | 83 (48.54) |
| No | 88 (51.46) |
| Daily tobacco use | |
| Yes | 86 (50.29) |
| No | 85 (49.71) |
| Type of employment contract | |
| Permanent | 115 (67.25) |
| Indefinite | 33 (19.30) |
| Part-time | 23 (13.45) |
| Variables | Mean (Standard Deviation) |
| Age (years) | 47.85 (8.11) |
| Time of service at the emergency department (years) | 12.76 (9.77) |
| Work experience (years) | 22.83 (8.54) |
| M (SD) | EE | DP | PA | A | B | C | D | GHQ | PSS | FRQ | PFC | EFC | AC | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CC (p-Value) | CC (p-Value) | CC (p-Value) | CC (p-Value) | CC (p-Value) | CC (p-Value) | CC (p-Value) | CC (p-Value) | CC (p-Value) | CC (p-Value) | CC (p-Value) | CC (p-Value) | CC | ||
| EE | 17.04 (11.25) | 1 | ||||||||||||
| DP | 8.47 (6.34) | 0.62 (0.0001) | 1 | |||||||||||
| PA | 37.85 (8.39) | −0.39 (0.0001) | −0.38 (0.0001) | 1 | ||||||||||
| A | 7.96 (3.98) | 0.15 (0.06) | 0.008 (0.91) | −0.04 (0.64) | 1 | |||||||||
| B | 7.88 (4.18) | 0.08 (0.001) | −0.003 (0.97) | −0.06 (0.45) | 0.68 (0.0001) | 1 | ||||||||
| C | 8.70 (2.88) | 0.14 (0.002) | −0.04 (0.57) | −0.06 (0.42) | 0.50 (0.0001) | 0.46 (0.0001) | 1 | |||||||
| D | 5.50 (5.27) | 0.12 (0.11) | 0.01 (0.86) | 0.07 (0.35) | 0.62 (0.0001) | 0.64 (0.0001) | 0.50 (0.001) | 1 | ||||||
| GHQ | 30.04 (13.57) | 0.15 (0.06) | −0.008 (0.92) | −0.01 (0.86) | 0.85 (0.0001) | 0.85 (0.0001) | 0.70 (0.0001) | 0.87 (0.0001) | 1 | |||||
| PSS | 21.30 (5.94) | 0.007 (0.93) | 0.13 (0.10) | −0.05 (0.54) | −0.16 (0.003) | −0.12 (0.12) | −0.01 (0.86) | −0.04 (0.64) | −0.10 (0.19) | 1 | ||||
| FRQ | 67.19 (6.98) | −0.04 (0.57) | −0.003 (0.97) | −0.06 (0.41) | −0.07 (0.36) | −0.05 (0.56) | −0.03 (0.66) | −0.11 (0.14) | −0.07 (0.35) | −0.05 (0.0004) | 1 | |||
| PFC | 1.51 (0.51) | −0.10 (0.18) | −0.16 (0.07) | 0.07 (0.40) | −0.16 (0.004) | −0.20 (0.0002) | −0.25 (0.0002) | −0.25 (0.003) | −0.26 (0.0005) | 0.02 (0.81) | −0.07 (0.37) | 1 | ||
| EFC | 1.28 (0.36) | 0.04 (0.62) | 0.03 (0.73) | 0.01 (0.91) | 0.12 (0.13) | 0.10 (0.18) | 0.06 (0.43) | 0.21 (0.002) | 0.16 (0.0006) | −0.07 (0.39) | −0.10 (0.19) | 0.26 (0.0004) | 1 | |
| AC | 1.09 (0.45) | 0.13 (0.004) | 0.10 (0.0002) | 0.03 (0.66) | 0.44 (0.0001) | 0.52 (0.0001) | 0.42 (0.0001) | 0.65 (0.0001) | 0.63 (0.0001) | 0.003 (0.97) | −0.06 (0.44) | −0.12 (0.13) | 0.37 (0.0003) | 1 |
| Variables | EE (Points) | p-Value | DP (Points) | p-Value | PA (Points) | p-Value |
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | ||||
| Sex | ||||||
| Male | 15.80 (10.60) | 0.02 | 7.69 (5.99) | 0.007 | 38.18 (8.07) | 0.40 |
| Female | 20.39 (12.35) | 10.61 (6.80) | 36.96 (9.22) | |||
| Marital status | ||||||
| Married | 16.67 (10.25) | 9.23 (5.40) | 38.36 (8.37) | |||
| Single | 17.21 (11.38) | 8.89 (6.32) | 37.70 (8.34) | |||
| Separated/divorced | 15.91 (11.65) | 0.88 | 6.18 (7.12) | 0.13 | 37.32 (9.32) | 0.52 |
| Widowed | 20 (15.02) | 5.29 (7.67) | 39 (7.57) | |||
| Daily physical exercise | ||||||
| Yes | 15.22 (10.50) | 0.09 | 7.07 (5.56) | 0.005 | 38.33 (8.17) | 0.48 |
| No | 18.74 (11.71) | 9.80 (6.76) | 37.41 (8.61) | |||
| Daily tobacco use | ||||||
| Yes | 16.70 (10.87) | 0.69 | 8.47 (6.15) | 0.99 | 38.21 (8.11) | 0.58 |
| No | 17.38 (11.67) | 8.48 (6.56) | 37.49 (8.69) | |||
| Type of employment contract | ||||||
| Permanent | 17.28 (11.37) | 8.20 (6.40) | 37.44 (8.57) | |||
| Indefinite | 17.85 (11.31) | 0.54 | 9.61 (6.06) | 0.52 | 38.18 (7.98) | 0.57 |
| Part-time | 14.65 (10.71) | 8.22 (6.49) | 39.43 (8.18) | |||
| Variables | EE | p-Value | DP | p-Value | PA | p-Value |
| CC | CC | CC | ||||
| Age (years) | 0.09 | 0.25 | -0.06 | 0.41 | -0.10 | 0.03 |
| Time of service at the ED (years) | 0.07 | 0.37 | 0.01 | 0.87 | -0.17 | 0.03 |
| Work experience (years) | 0.10 | 0.20 | -0.07 | 0.35 | -0.08 | 0.02 |
| 9 | EE * | DP ** | PA *** | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | p-Value | ß | p-Value | B | p-Value | ß | p-Value | B | p-Value | ß | p-Value | |
| Sex | ||||||||||||
| Male | Ref | 0.02 | Ref | 0.01 | Ref | 0.007 | Ref | 0.01 | Ref | 0.40 | ||
| Female | 4.59 | 4.59 | 2.92 | 2.74 | −1.23 | |||||||
| Marital status | ||||||||||||
| Married | Ref | 0.80 | Ref | 0.29 | Ref | 0.77 | ||||||
| Not married | 0.45 | −1.06 | −0.40 | |||||||||
| Daily physical exercise | ||||||||||||
| Yes | Ref | 0.09 | Ref | 0.005 | Ref | 0.006 | Ref | 0.48 | ||||
| No | 3.51 | 2.72 | 2.47 | −0.92 | ||||||||
| Daily tobacco use | ||||||||||||
| Yes | Ref | 0.69 | Ref | 0.99 | Ref | 0.58 | ||||||
| No | 0.68 | 0.02 | −0.72 | |||||||||
| Type of employment contract | ||||||||||||
| Ref | 0.69 | Ref | 0.42 | Ref | 0.36 | |||||||
| −0.74 | 0.84 | 1.25 | ||||||||||
| Age (years) | 0.12 | 0.25 | −0.05 | 0.41 | −0.10 | 0.02 | ||||||
| Time of service at the ED (years) | 0.08 | 0.37 | 0.008 | 0.87 | −0.14 | 0.03 | −0.14 | 0.03 | ||||
| Work experience (years) | 0.13 | 0.20 | −0.05 | 0.35 | −0.08 | 0.03 | ||||||
| Perceived stress (points) | 0.01 | 0.93 | 0.13 | 0.10 | −0.07 | 0.54 | ||||||
| Job satisfaction (points) | −0.07 | 0.57 | −0.003 | 0.97 | −0.08 | 0.41 | ||||||
| Somatic symptoms (points) | 0.44 | 0.06 | 0.01 | 0.91 | −0.08 | 0.64 | ||||||
| Anxiety (points) | 0.23 | 0.02 | 0.11 | 0.01 | −0.005 | 0.97 | −0.12 | 0.45 | ||||
| Social dysfunction (points) | 0.53 | 0.03 | 0.39 | 0.02 | −0.10 | 0.57 | −0.18 | 0.42 | ||||
| Depression (points) | 0.26 | 0.12 | 0.02 | 0.86 | 0.11 | 0.35 | ||||||
| Problem-focused coping (points) | −2.30 | 0.17 | −2.03 | 0.18 | 1.07 | 0.40 | ||||||
| Emotion-focused coping (points) | 1.17 | 0.62 | 0.46 | 0.73 | 0.21 | 0.91 | ||||||
| Avoidance coping (points) | 3.31 | 0.02 | 3.30 | 0.04 | 1.34 | 0.02 | 1.02 | 0.03 | 0.64 | 0.66 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Portero de la Cruz, S.; Cebrino, J.; Herruzo, J.; Vaquero-Abellán, M. A Multicenter Study into Burnout, Perceived Stress, Job Satisfaction, Coping Strategies, and General Health among Emergency Department Nursing Staff. J. Clin. Med. 2020, 9, 1007. https://doi.org/10.3390/jcm9041007
Portero de la Cruz S, Cebrino J, Herruzo J, Vaquero-Abellán M. A Multicenter Study into Burnout, Perceived Stress, Job Satisfaction, Coping Strategies, and General Health among Emergency Department Nursing Staff. Journal of Clinical Medicine. 2020; 9(4):1007. https://doi.org/10.3390/jcm9041007
Chicago/Turabian StylePortero de la Cruz, Silvia, Jesús Cebrino, Javier Herruzo, and Manuel Vaquero-Abellán. 2020. "A Multicenter Study into Burnout, Perceived Stress, Job Satisfaction, Coping Strategies, and General Health among Emergency Department Nursing Staff" Journal of Clinical Medicine 9, no. 4: 1007. https://doi.org/10.3390/jcm9041007
APA StylePortero de la Cruz, S., Cebrino, J., Herruzo, J., & Vaquero-Abellán, M. (2020). A Multicenter Study into Burnout, Perceived Stress, Job Satisfaction, Coping Strategies, and General Health among Emergency Department Nursing Staff. Journal of Clinical Medicine, 9(4), 1007. https://doi.org/10.3390/jcm9041007







