The Role of Physical Activity as Conservative Treatment for Hip and Knee Osteoarthritis in Older People: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Criteria for Considering Studies for This Review
2.2. Search Methods for Identification of Studies
2.3. Data Collection, Analysis, and Outcomes
2.4. Risk of Bias Assessment
2.5. Statistical Analysis
2.6. Quality Assessment
3. Results
3.1. Results of the Search
3.2. Included and Excluded Studies
3.3. Demographic Data
3.4. Clinical Outcome Data
3.5. Methodological Evaluation
3.6. Studies Included
3.6.1. Double Study Group
3.6.2. Land-Based Exercise
3.6.3. Aquatic Exercise
3.6.4. Sport
3.7. Effect of Intervention
3.7.1. Pain
3.7.2. Physical Function
3.7.3. Quality of Life
3.7.4. Stiffness
3.7.5. Dynamic Balance
3.8. Quality Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Glyn-Jones, S.; Palmer, A.J.R.; Agricola, R.; Price, A.J.; Vincent, T.L.; Weinans, H.; Carr, A.J. Osteoarthritis. Lancet 2015, 386, 376–387. [Google Scholar] [CrossRef]
- van Dijk, G.M.; Dekker, J.; Veenhof, C.; van den Ende, C.H.M. Carpa Study Group Course of functional status and pain in osteoarthritis of the hip or knee: A systematic review of the literature. Arthritis Rheum. 2006, 55, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Ojoawo, A.O.; Olaogun, M.O.B.; Hassan, M.A. Comparative effects of proprioceptive and isometric exercises on pain intensity and difficulty in patients with knee osteoarthritis: A randomised control study. Technol. Health Care 2016, 24, 853–863. [Google Scholar] [CrossRef] [PubMed]
- Clynes, M.A.; Jameson, K.A.; Edwards, M.H.; Cooper, C.; Dennison, E.M. Impact of osteoarthritis on activities of daily living: Does joint site matter? Aging Clin. Exp. Res. 2019, 31, 1049–1056. [Google Scholar] [CrossRef] [PubMed]
- Johnson, V.L.; Hunter, D.J. The epidemiology of osteoarthritis. Best Pract. Res. Clin. Rheumatol. 2014, 28, 5–15. [Google Scholar] [CrossRef]
- Segal, N.A.; Glass, N.A.; Teran-Yengle, P.; Singh, B.; Wallace, R.B.; Yack, H.J. Intensive Gait Training for Older Adults with Symptomatic Knee Osteoarthritis. Am. J. Phys. Med. Rehabil. 2015, 94, 848–858. [Google Scholar] [CrossRef]
- Papalia, R.; Zampogna, B.; Torre, G.; Lanotte, A.; Vasta, S.; Albo, E.; Tecame, A.; Denaro, V. Sarcopenia and its relationship with osteoarthritis: Risk factor or direct consequence? Musculoskelet. Surg. 2014, 98, 9–14. [Google Scholar] [CrossRef]
- Litwic, A.; Edwards, M.H.; Dennison, E.M.; Cooper, C. Epidemiology and burden of osteoarthritis. Br. Med. Bull. 2013, 105, 185–199. [Google Scholar] [CrossRef]
- Kamaruzaman, H.; Kinghorn, P.; Oppong, R. Cost-effectiveness of surgical interventions for the management of osteoarthritis: A systematic review of the literature. BMC Musculoskelet. Disord. 2017, 18, 183. [Google Scholar] [CrossRef]
- Rodriguez-Merchan, E.C. Conservative treatment of acute knee osteoarthritis: A review of the Cochrane Library. J. Acute Dis. 2016, 5, 190–193. [Google Scholar] [CrossRef][Green Version]
- Vaishya, R.; Pariyo, G.B.; Agarwal, A.K.; Vijay, V. Non-operative management of osteoarthritis of the knee joint. J. Clin. Orthop. Trauma 2016, 7, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Papalia, R.; Zampogna, B.; Russo, F.; Torre, G.; De Salvatore, S.; Nobile, C.; Tirindelli, M.C.; Grasso, A.; Vadalà, G.; Denaro, V.; et al. The combined use of platelet rich plasma and hyaluronic acid: Prospective results for the treatment of knee osteoarthritis. J. Biol. Regul. Homeost. Agents 2019, 33, 21–28. [Google Scholar] [PubMed]
- Wellsandt, E.; Golightly, Y. Exercise in the management of knee and hip osteoarthritis. Curr. Opin. Rheumatol. 2018, 30, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Fernandopulle, S.; Perry, M.; Manlapaz, D.; Jayakaran, P. Effect of Land-Based Generic Physical Activity Interventions on Pain, Physical Function, and Physical Performance in Hip and Knee Osteoarthritis. Am. J. Phys. Med. Rehabil. 2017, 96, 773–792. [Google Scholar] [CrossRef]
- Kraus, V.B.; Sprow, K.; Powell, K.E.; Buchner, D.; Bloodgood, B.; Piercy, K.; George, S.M.; Kraus, W.E. Effects of Physical Activity in Knee and Hip Osteoarthritis: A Systematic Umbrella Review. Med. Sci. Sports Exerc. 2019, 51, 1324–1339. [Google Scholar] [CrossRef]
- Gademan, M.G.J.; Hofstede, S.N.; Vliet Vlieland, T.P.M.; Nelissen, R.G.H.H.; Marang-van de Mheen, P.J. Indication criteria for total hip or knee arthroplasty in osteoarthritis: A state-of-the-science overview. BMC Musculoskelet. Disord. 2016, 17, 463. [Google Scholar] [CrossRef]
- Van Ginckel, A.; Hall, M.; Dobson, F.; Calders, P. Effects of long-term exercise therapy on knee joint structure in people with knee osteoarthritis: A systematic review and meta-analysis. Semin. Arthritis Rheum. 2018, 48, 941–949. [Google Scholar] [CrossRef]
- Bartholdy, C.; Juhl, C.; Christensen, R.; Lund, H.; Zhang, W.; Henriksen, M. The role of muscle strengthening in exercise therapy for knee osteoarthritis: A systematic review and meta-regression analysis of randomized trials. Semin. Arthritis Rheum. 2017, 47, 9–21. [Google Scholar] [CrossRef]
- Ageberg, E.; Roos, E.M. Neuromuscular Exercise as Treatment of Degenerative Knee Disease. Exerc. Sport Sci. Rev. 2015, 43, 14–22. [Google Scholar] [CrossRef]
- Hurley, M.V.; Mitchell, H.L.; Walsh, N. In Osteoarthritis, the Psychosocial Benefits of Exercise Are as Important as Physiological Improvements. Exerc. Sport Sci. Rev. 2003, 31, 138–143. [Google Scholar] [CrossRef]
- Wang, T.-J.; Belza, B.; Elaine Thompson, F.; Whitney, J.D.; Bennett, K. Effects of aquatic exercise on flexibility, strength and aerobic fitness in adults with osteoarthritis of the hip or knee. J. Adv. Nurs. 2007, 57, 141–152. [Google Scholar] [CrossRef] [PubMed]
- Bartels, E.M.; Juhl, C.B.; Christensen, R.; Hagen, K.B.; Danneskiold-Samsøe, B.; Dagfinrud, H.; Lund, H. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef] [PubMed]
- Molloy, M.G.; Molloy, C.B. Contact sport and osteoarthritis. Br. J. Sports Med. 2011, 45, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Valderrabano, V.; Steiger, C. Treatment and Prevention of Osteoarthritis through Exercise and Sports. J. Aging Res. 2011, 2011, 1–6. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, 7. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Stiles, C.R.; Hagen, N.A.; Biondo, P.D.; Cummings, G.G. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research: Quality assessment for systematic reviews. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological Index for Non-Randomized Studies (Minors): Development And Validation of A New Instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Gopalakrishna, G.; Mustafa, R.A.; Davenport, C.; Scholten, R.J.P.M.; Hyde, C.; Brozek, J.; Schünemann, H.J.; Bossuyt, P.M.M.; Leeflang, M.M.G.; Langendam, M.W. Applying Grading of Recommendations Assessment, Development and Evaluation (GRADE) to diagnostic tests was challenging but doable. J. Clin. Epidemiol. 2014, 67, 760–768. [Google Scholar] [CrossRef]
- Bove, A.M.; Baker, N.; Livengood, H.; King, V.; Mancino, J.; Popchak, A.; Fitzgerald, G.K. Task-Specific Training for Adults With Chronic Knee Pain: A Case Series. J. Orthop. Sports Phys. Ther. 2017, 47, 548–556. [Google Scholar] [CrossRef]
- Fransen, M.; Nairn, L.; Winstanley, J.; Lam, P.; Edmonds, J. Physical activity for osteoarthritis management: A randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum. 2007, 57, 407–414. [Google Scholar] [CrossRef]
- Brismée, J.-M.; Paige, R.L.; Chyu, M.-C.; Boatright, J.D.; Hagar, J.M.; McCaleb, J.A.; Quintela, M.M.; Feng, D.; Xu, K.T.; Shen, C.-L. Group and home-based tai chi in elderly subjects with knee osteoarthritis: A randomized controlled trial. Clin. Rehabil. 2007, 21, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-J.; Park, H.-J.; Chae, Y.; Kim, S.-Y.; Kim, S.-N.; Kim, S.-T.; Kim, J.-H.; Yin, C.-S.; Lee, H. Tai Chi Qigong for the quality of life of patients with knee osteoarthritis: A pilot, randomized, waiting list controlled trial. Clin. Rehabil. 2009, 23, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Tsai, P.-F.; Chang, J.Y.; Beck, C.; Kuo, Y.-F.; Keefe, F.J. A Pilot Cluster-Randomized Trial of a 20-Week Tai Chi Program in Elders With Cognitive Impairment and Osteoarthritic Knee: Effects on Pain and Other Health Outcomes. J. Pain Symptom Manag. 2013, 45, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Cheung, C.; Wyman, J.F.; Resnick, B.; Savik, K. Yoga for managing knee osteoarthritis in older women: A pilot randomized controlled trial. BMC Complementary Altern. Med. 2014, 14, 160. [Google Scholar] [CrossRef] [PubMed]
- Cheung, C.; Wyman, J.F.; Bronas, U.; McCarthy, T.; Rudser, K.; Mathiason, M.A. Managing knee osteoarthritis with yoga or aerobic/strengthening exercise programs in older adults: A pilot randomized controlled trial. Rheumatol. Int. 2017, 37, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.-J.; Lee, S.-C.; Liang, S.-Y.; Tung, H.-H.; Wu, S.-F.V.; Lin, Y.-P. Comparing the efficacy of aquatic exercises and land-based exercises for patients with knee osteoarthritis: Efficacy of aquatic vs. land exercises for knee OA. J. Clin. Nurs. 2011, 20, 2609–2622. [Google Scholar] [CrossRef]
- Foley, A. Does hydrotherapy improve strength and physical function in patients with osteoarthritis--a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann. Rheum. Dis. 2003, 62, 1162–1167. [Google Scholar] [CrossRef]
- Lund, H.; Weile, U.; Christensen, R.; Rostock, B.; Downey, A.; Bartels, E.; Danneskiold-Samsøe, B.; Bliddal, H. A randomized controlled trial of aquatic and land-based exercise in patients with knee osteoarthritis. J. Rehabil. Med. 2008, 40, 137–144. [Google Scholar] [CrossRef]
- Hale, L.A.; Waters, D.; Herbison, P. A Randomized Controlled Trial to Investigate the Effects of Water-Based Exercise to Improve Falls Risk and Physical Function in Older Adults With Lower-Extremity Osteoarthritis. Arch. Phys. Med. Rehabil. 2012, 93, 27–34. [Google Scholar] [CrossRef]
- Casilda-López, J.; Valenza, M.C.; Cabrera-Martos, I.; Díaz-Pelegrina, A.; Moreno-Ramírez, M.P.; Valenza-Demet, G. Effects of a dance-based aquatic exercise program in obese postmenopausal women with knee osteoarthritis: A randomized controlled trial. Menopause 2017, 24, 768–773. [Google Scholar] [CrossRef]
- Taglietti, M.; Facci, L.M.; Trelha, C.S.; de Melo, F.C.; da Silva, D.W.; Sawczuk, G.; Ruivo, T.M.; de Souza, T.B.; Sforza, C.; Cardoso, J.R. Effectiveness of aquatic exercises compared to patient-education on health status in individuals with knee osteoarthritis: A randomized controlled trial. Clin. Rehabil. 2018, 32, 766–776. [Google Scholar] [CrossRef] [PubMed]
- Arnold, C.M.; Faulkner, R.A. The Effect of Aquatic Exercise and Education on Lowering Fall Risk in Older Adults With Hip Osteoarthritis. J. Aging Phys. Act. 2010, 18, 245–260. [Google Scholar] [CrossRef] [PubMed]
- Bearne, L.M.; Walsh, N.E.; Jessep, S.; Hurley, M.V. Feasibility of an Exercise-Based Rehabilitation Programme for Chronic Hip Pain: Exercise-Based Rehabilitation for Chronic Hip Pain. Musculoskelet. Care 2011, 9, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Bezalel, T.; Carmeli, E.; Katz-Leurer, M. The effect of a group education programme on pain and function through knowledge acquisition and home-based exercise among patients with knee osteoarthritis: A parallel randomised single-blind clinical trial. Physiotherapy 2010, 96, 137–143. [Google Scholar] [CrossRef]
- Huang, L.; Guo, B.; Xu, F.; Zhao, J. Effects of quadriceps functional exercise with isometric contraction in the treatment of knee osteoarthritis. Int. J. Rheum. Dis. 2018, 21, 952–959. [Google Scholar] [CrossRef]
- Doi, T.; Akai, M.; Fujino, K.; Iwaya, T.; Kurosawa, H.; Hayashi, K.; Marui, E. Effect of Home Exercise of Quadriceps on Knee Osteoarthritis Compared with Nonsteroidal Antiinflammatory Drugs: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2008, 87, 258–269. [Google Scholar] [CrossRef]
- Marconcin, P.; Espanha, M.; Teles, J.; Bento, P.; Campos, P.; André, R.; Yázigi, F. A randomized controlled trial of a combined self-management and exercise intervention for elderly people with osteoarthritis of the knee: The PLE 2 NO program. Clin. Rehabil. 2018, 32, 223–232. [Google Scholar] [CrossRef]
- Hurley, M.V.; Walsh, N.E.; Mitchell, H.L.; Pimm, T.J.; Patel, A.; Williamson, E.; Jones, R.H.; Dieppe, P.A.; Reeves, B.C. Clinical effectiveness of a rehabilitation program integrating exercise, self-management, and active coping strategies for chronic knee pain: A cluster randomized trial. Arthritis Rheum. 2007, 57, 1211–1219. [Google Scholar] [CrossRef]
- Takacs, J.; Krowchuk, N.M.; Garland, S.J.; Carpenter, M.G.; Hunt, M.A. Dynamic Balance Training Improves Physical Function in Individuals With Knee Osteoarthritis: A Pilot Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2017, 98, 1586–1593. [Google Scholar] [CrossRef]
- An, B.; Wang, Y.; Jiang, X.; Lu, H.; Fang, Z.; Wang, Y.; Dai, K. Effects of Baduanjin exercise on knee osteoarthritis: A one-year study. Chin. J. Integr. Med. 2013, 19, 143–148. [Google Scholar] [CrossRef]
- Cheung, C.; Park, J.; Wyman, J.F. Effects of Yoga on Symptoms, Physical Function, and Psychosocial Outcomes in Adults with Osteoarthritis: A Focused Review. Am. J. Phys. Med. Rehabil. 2016, 95, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Dong, R.; Wu, Y.; Xu, S.; Zhang, L.; Ying, J.; Jin, H.; Wang, P.; Xiao, L.; Tong, P. Is aquatic exercise more effective than land-based exercise for knee osteoarthritis? Medicine 2018, 97, e13823. [Google Scholar] [CrossRef] [PubMed]
- Goh, S.-L.; Persson, M.S.M.; Stocks, J.; Hou, Y.; Welton, N.J.; Lin, J.; Hall, M.C.; Doherty, M.; Zhang, W. Relative Efficacy of Different Exercises for Pain, Function, Performance and Quality of Life in Knee and Hip Osteoarthritis: Systematic Review and Network Meta-Analysis. Sports Med. 2019, 49, 743–761. [Google Scholar] [CrossRef]
- Lauche, R.; Langhorst, J.; Dobos, G.; Cramer, H. A systematic review and meta-analysis of Tai Chi for osteoarthritis of the knee. Complementary Ther. Med. 2013, 21, 396–406. [Google Scholar] [CrossRef]
- van Gool, C.H.; Penninx, B.W.J.H.; Kempen, G.I.J.M.; Rejeski, W.J.; Miller, G.D.; van Eijk, J.T.M.; Pahor, M.; Messier, S.P. Effects of exercise adherence on physical function among overweight older adults with knee osteoarthritis. Arthritis Rheum. 2005, 53, 24–32. [Google Scholar] [CrossRef]


















| Author (Year) | Type of Study | LOE | Study Group | Control Group | Joint/s | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Age | Sex | BMI | n | Age | Sex | BMI | ||||
| Arnold et al. (2010) [42] | RCT | I | Aquatic and education: 28 | 73.2 y | 71.4% F, 28.6% M | 29.2 | 25 | 75.8 y | 64% F, 36% M | 30 | hip OA |
| Aquatic: 26 | 74.4 y | 77% F, 23% M | 30.4 | ||||||||
| Bearne et al. (2011) [43] | RCT | I | 24 | 65 y | 62.5% F, 37.5% M | 27.3 | 24 | 67 y | 79% F, 21% M | 26.9 | hip OA |
| Bezalel et al. (2010) [44] | RCT | I | 25 | 73.8 y | 68% F, 32% M | / | 25 | 73.7 y | 80% F, 20% M | / | knee OA |
| Brismee et al. (2007) [31] | RCT | I | 22 | 70.8 y | 86.4% F, 13.6% M | 28 | 19 | 68.8 y | 78.9% F, 21.1% M | 27.7 | knee OA |
| Casilda-López et al. ( 2017) [40] | RCT | I | 17 | 65.62 y | 100% F | 31.69 | 17 | 66 y | 100% F | 33.65 | knee OA |
| Cheung et al. (2014) [34] | RCT | I | 18 | 71.9 y | 100% F | 29.1 | 18 | 71.9 y | 100% F | 28.8 | knee OA |
| Cheung et al. (2016) [35] | RCT | I | Yog: 32 | 68.9 y | / | 29.8 | 23 | 71.8 y | / | 27.8 | knee OA |
| Exercises: 28 | 74.4 y | / | 29.2 | ||||||||
| Doi et al. (2008) [46] | RCT | I | 63 | 67.4 y | 76% F, 24% M | 24.8 | 58 | 71.2 y | 72% F, 28% M | 24.3 | knee OA |
| Foley et al. (2003) [37] | RCT | I | Aquatic: 35 | 73 y | 43% F, 57% M | / | 35 | 6.8 y | 57% F, 43% M | / | hip and knee OA |
| Land-based: 35 | 69.8 y | 49% F, 51% M | / | ||||||||
| Fransen et al. (2007) [30] | RCT | I | Aquatic: 55 | 70 y | 73% F, 27% M | 30 | 41 | 69.6 y | 83% F, 17% M | 30.7 | hip and knee OA |
| Tai chi: 56 | 70.8 y | 68% F, 32% M | 29.6 | ||||||||
| Hale et al. (2012) [39] | RCT | I | 23 | 73.6 y | 74% F, 26% M | / | 16 | 75.7 y | 75% F, 25% M | / | hip and knee OA |
| Huang et al. (2017) [45] | RCT | I | 128 | 68.07 y | 79% F, 21% M | 24.11 | 122 | 67.42 y | 80% F, 20% M | 25.01 | knee OA |
| Hurley et al. (2007) [48] | RCT | I | Individual rehabilitation: 146 | 66 y | 71% F, 29% M | 30 | 140 | 67 y | 68.5% F, 31.5% M | 30.3 | knee OA |
| Group rehabilitation: 132 | 68 y | 71% F, 29% M | 30.18 | ||||||||
| Lee et al. (2009) [32] | RCT | I | 29 | 70.2 y | 93.1% F, 6.9% M | 26 | 15 | 66.9 y | 93.3% F, 6.7% M | 26 | knee OA |
| Lund et al. (2008) [38] | RCT | I | Aquatic: 27 | 65 y | 83% F, 17% M | 27.4 | 27 | 70 y | 66% F, 34% M | 26.1 | knee OA |
| Land-based: 25 | 68 y | 88% F, 12% M | 23.7 | ||||||||
| Marconcin et al. (2017) [47] | RCT | I | 35 | 70.3 y | 80% F, 20% M | 32.3 | 32 | 67.8 y | 59.4% F, 40.6% M | 30.1 | knee OA |
| Taglietti et al. (2018) [41] | RCT | I | 31 | 67.3 y | 74.2% F, 25.8% M | 29.2 | 29 | 68.7 y | 62.1% F, 37.9% M | 30.4 | knee OA |
| Takacs et al. (2017) [49] | RCT | I | 20 | 66,1 y | 95% F, 5% M | 28.5 | 20 | 67.1 y | 65% F, 35% M | 28.9 | knee OA |
| Tsai et al. (2013) [33] | RCT | I | 28 | 78.89 y | 78.6% F, 21.4% M | / | 27 | 78.93 y | 66.7% F, 33.3% M | / | knee OA |
| Wang et al. (2011) [36] | RCT | I | Aquatic: 26 | 66.7 y | 84.6% F, 15.4% M | / | 26 | 67.9 y | 84.6% F, 15.4% M | / | knee OA |
| Land-based: 26 | 68.3 y | 88.5% F, 11.5% M | / | ||||||||
| An et al. (2013) [50] | CS | IV | 22 | 66 y | 86% F, 14% M | 25 | / | knee OA | |||
| Bove et al. (2017) [29] | CS | IV | 7 | 66 y | 71.5% F, 28.5% M | 30.5 | / | knee OA | |||
| Author (Year) | Intervention(s) | Control | Primary Outcome Measure | Secondary Outcome Measure | Follow-Up | Results |
|---|---|---|---|---|---|---|
| Arnold et al. (2010) [42] | Aquatic and education: aquatic exercise twice a week with once-a-week group education for 11 weeks; Aquatic: two weeks aquatic exercise for 11 weeks | no intervention | Berg Balance Scale, 6-MWT, Timed Up and Go Test | PASE score, AIMS-2 score | 11 weeks | Significant improvement in fall risk factors (p = 0.038) with the combination of aquatic exercise and education. |
| Bearne et al. (2011) [43] | Ten 75-min group exercise and self-management sessions (twice a week for five weeks) | no intervention | WOMAC physical function | WOMAC pain, WOMAC total score | Six weeks and six months | No between-group differences in any outcome measure. |
| Bezalel et al. (2010) [44] | Group education program once a week for four weeks, followed by a self-executed home-based exercise program | six 20-min sessions of short-wave diathermy | WOMAC total score | Sit to stand test, Timed up and go test | four and eight weeks | Significant improvement in the timed up and go test and WOMAC total (p < 0.01) in the exercise group. |
| Brismee et al. (2007) [31] | Six weeks of group Tai Chi sessions, 40 min/session, three times a week, followed by another six weeks of home-based Tai Chi training | three 40-min group sessions per week for six weeks | WOMAC pain, VAS | WOMAC stiffness and physical function | 3, 6, 9, 12, 15, and 18 weeks | Less overall pain and better WOMAC physical function with Tai Chi (p = 0.0089 and 0.0157, respectively). |
| Casilda-López et al. ( 2017) [40] | Eight-week dance-based aquatic exercise program | global aquatic exercise program | WOMAC total score | 6-MWT and VAS | Eight weeks and Three months | Postintervention differences in the WOMAC pain and aggregate (p = 0.002 and p = 0.048) in favor of the experimental group. |
| Cheung et al. (2014) [34] | Eight-week Hatha yoga intervention involving group and home-based exercise sessions | no intervention | WOMAC total score | SPPB, SF-12 | Four weeks, eight weeks and 20 weeks | Improvement in WOMAC pain p = 0.01) and stiffness (p = 0.02) in the intervention group. |
| Cheung et al. (2016) [35] | Yoga: one 45-min class per week for eight weeks and additional 30 min/day, four times/week of yoga practice at home; Exercises: eight weekly group-based classes | no intervention | WOMAC total score, VAS | SPPB, SF-12 | Four and eight weeks | Yoga group presented improvements in WOMAC TOTAL (p = 0.001) and VAS scores (p = 0.03) compared to exercises group. |
| Doi et al. (2008) [46] | Four sets of 20 repetitions of quadriceps exercise every day (knee extension movements while sitting on a chair or in a supine position) | NSAIDs | WOMAC total score and VAS | SF-36 | Eight weeks | Improvements in total WOMAC, SF-36 and VAS: all p < 0.001 in the exercises group; WOMAC and VAS at p < 0.001 and SF-36 at P < 0.03 in the control group. |
| Foley et al. (2003) [37] | Three water based, or three gym-based exercise sessions a week for six weeks, including a short warm up period, lower limb stretches, and a set of resistance exercises | no intervention | WOMAC total score, 6-MWT | SF-12 | Six weeks | Walking speed and distance increased in the hydrotherapy and gym groups (both p < 0.001). No significant changes for WOMAC function or stiffness. |
| Fransen et al. (2007) [30] | Aquatic or Tai Chi program (with a preliminary 10-min warm-up session): 1 h, twice a week for 12 weeks | no intervention | WOMAC pain and physical function | SF-12, DASS21 | 12 and 24 weeks | Improvements of 6.5 and 10.5 for pain and physical function scores with hydrotherapy and improvements of 5.2 and 9.7 with Tai Chi. |
| Hale et al. (2012) [44] | Water-based exercise classes twice weekly for 12 weeks | community-based computer-skills training program | PPA | Step Test, Timed Up and Go Test, WOMAC total score | 12 weeks | No statistically significant between-group differences were found for any outcome measured. |
| Huang et al. (2017) [45] | Quadriceps isometric contraction exercise (two sets of exercises in the morning and evening) | local physiotherapy and oral NSAIDs | WOMAC total score, VAS | / | One and three months | Significant improvement of WOMAC and VAS score in the experimental group (p < 0.05). |
| Hurley et al. (2007) [48] | 12 supervised sessions that combined discussion on specific topics regarding self-management and coping, with an individualized, progressive exercise regimen | no intervention | WOMAC physical function | WOMAC pain, WOMAC total score | Six weeks and six months | Individual and group rehabilitated participants had better WOMAC score (p = 0.01) than control group. |
| Lee et al. (2009) [32] | Eight weeks of group Tai Chi Qigong sessions, with 60 min per session twice a week | no intervention | SF-36 | WOMAC total score, 6-MWT | Eight weeks | Improvements in SF-36 (p = 0.010) and 6- MWT (p = 0.005) in the Tai Chi group. |
| Lund et al. (2008) [38] | Aquatic and land-based exercise programs for eight weeks with 2 sessions per week | no intervention | KOOS function and pain, VAS | Muscle Strength | Eight weeks and three months | Only in the land-based exercise group a decrease of pain was detected (p = 0.039). There were no significant differences between groups for KOOS. |
| Marconcin et al. (2017) [47] | PLE2NO program: 90-min intervention twice a week for 12 weeks | no intervention | KOOS pain | KOOS function and total score, 6-MWT | 12 weeks | Significant clinical improvement was found for all KOOS (larger than 10 points) and in the 6 MWT (p = 0.035) in the exercise group. |
| Taglietti et al. (2018) [41] | Aquatic program twice a week for eight weeks | educational program: once a week for eight weeks | WOMAC total score, VAS | SF-36, Timed up and go test, Yesavage Geriatric Depression Scale | Three months | WOMAC pain reduced in favour of the aquatic exercise group (p = 0.021). No differences for the outcome’s functional mobility or depression. |
| Takacs et al. (2017) [49] | Ten weeks of exercises targeting dynamic balance and strength performed four times per week | no intervention | CB&M, WOMAC physical function | Muscle Strength | 10 weeks | Improvements in self-reported pain (p = 0.005), physical function (p = 0.002), and fear of movement (p = 0.01) in the training group. |
| Tsai et al. (2013) [33] | Three sessions a week of Tai Chi exercise (12-form Sun Tai Chi) for 20 weeks | no intervention | WOMAC pain | WOMAC physical function and stiffness, timed up and go test and Sit to stand test | 21 weeks | WOMAC pain (p < 0.001), physical function (p = 0.001) and stiffness scores (p = 0.001) improved in the Tai Chi group. |
| Wang et al. (2011) [36] | Aquatic/land-based exercise protocol with a 60-min flexibility and aerobic training class, three times a week for 12 weeks | no intervention | KOOS total score, 6-MWT | knee ROMs | Six and 12 weeks | Aquatic and land group presented less pain than control group (respectively p < 0.001 and p = 0.002). |
| An et al. (2013) [50] | Short-term Baduanjin exercise: 30-min sessions five times a week for one year | / | WOMAC total score, SF-36 | 6-MWT | one year | WOMAC pain, stiffness and physical function subscales, SF-36 body pain and 6-MWT were significantly improved. |
| Bove et al. (2017) [29] | 16 sessions of task-specific training at a frequency of two visits per week | / | KOOS total score | 30-Second Chair Rise, Timed Stair Climb Test, Floor Transfer Test | Four, six, and eight weeks | Improvements in patient-rated and performance-based outcomes. |
| Study | Sequence Generation | Allocation Concealment | Blinding | Incomplete Data Addressed | Free of Selective Reporting | Free of Other Bias | Risk of Bias |
|---|---|---|---|---|---|---|---|
| Arnold et al. (2010) | L | L | H | L | U | L | B |
| Bearne et al. (2011) | L | U | H | L | U | U | C |
| Bezalel et al. (2010) | L | L | H | U | U | U | C |
| Brismee et al. (2007) | L | U | H | L | L | U | B |
| Casilda-López et al. ( 2017) | L | L | U | L | U | U | B |
| Cheung et al. (2014) | L | L | H | L | L | U | B |
| Cheung et al. (2016) | L | L | H | L | L | L | A |
| Doi e al. (2008) | L | L | H | H | L | U | B |
| Foley et al. (2003) | L | L | U | L | L | U | B |
| Fransen et al. (2007) | L | L | U | L | L | U | B |
| Hale et al. (2012) | L | L | U | U | L | L | B |
| Huang et al. (2017) | U | U | H | L | H | H | C |
| Hurley et al. (2007) | U | L | H | U | L | L | B |
| Lee et al. (2009) | L | L | H | L | L | L | A |
| Lund et al. (2008) | U | L | U | L | L | L | B |
| Marconcin et al. (2017) | H | U | H | L | L | U | C |
| Taglietti et al. (2018) | L | L | H | L | L | L | A |
| Takacs et al. (2017) | L | L | H | L | U | L | B |
| Tsai et al. (2013) | L | L | H | L | L | L | A |
| Wang et al. (2011) | L | U | H | L | L | L | B |
| Study | Stated Aim | Inclusion of Patients | Collection of Data | Endpoints Appropriate to the Aim | Unbiased Assessment of the Study Endpoint | Follow-Up | Loss to Follow Up Less Than 5% | Prospective Calculation of the Study Size | Total |
|---|---|---|---|---|---|---|---|---|---|
| Am et al. (2013) | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 0 | 12 |
| Bove et al. (2017) | 2 | 1 | 2 | 2 | 1 | 1 | 2 | 0 | 11 |
| Outcomes | Comparisons | n of Participants (Studies) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Quality |
|---|---|---|---|---|---|---|---|---|
| Pain | Aquatic vs. Land-based | 174 (3 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Function | Aquatic vs. Land-based | 174 (3 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Quality of Life | Aquatic vs. Land-based | 174 (3 RCT) | serious | serious | not serious | not serious | not serious | ⨁⨁◯◯ low |
| Pain | Aquatic vs. Control | 367 (6 RCT) | serious | serious | not serious | not serious | not serious | ⨁⨁◯◯ low |
| Function | Aquatic vs. Control | 307 (5 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Quality of Life | Aquatic vs. Control | 272 (4 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Stiffness | Aquatic vs. Control | 105 (2 RCT) | serious | serious | not serious | not serious | not serious | ⨁⨁◯◯ low |
| Dynamic Balance | Aquatic vs. Control | 244 (4 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Pain | Land-based vs. Control | 682(7 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Function | Land-based vs. Control | 651 (7 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Quality of Life | Land-based vs. Control | 225 (4 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Stiffness | Land-based vs. Control | 121 (2 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Pain | Tai Chi vs. Control | 237 (4 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Function | Tai Chi vs. Control | 237 (4 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Stiffness | Tai Chi vs. Control | 140 (3 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
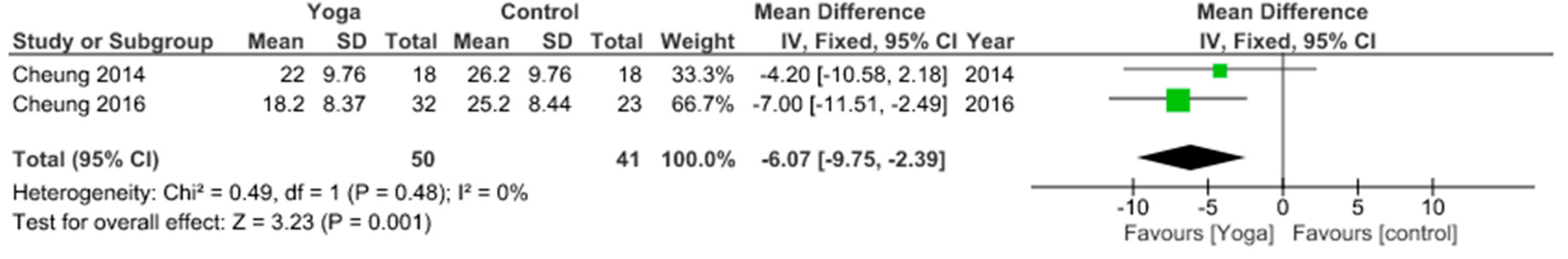
| Pain | Yoga vs. Control | 91 (2 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Function | Yoga vs. Control | 91 (2 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
| Stiffness | Yoga vs. Control | 91 (2 RCT) | serious | not serious | not serious | not serious | not serious | ⨁⨁⨁◯ moderate |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zampogna, B.; Papalia, R.; Papalia, G.F.; Campi, S.; Vasta, S.; Vorini, F.; Fossati, C.; Torre, G.; Denaro, V. The Role of Physical Activity as Conservative Treatment for Hip and Knee Osteoarthritis in Older People: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 1167. https://doi.org/10.3390/jcm9041167
Zampogna B, Papalia R, Papalia GF, Campi S, Vasta S, Vorini F, Fossati C, Torre G, Denaro V. The Role of Physical Activity as Conservative Treatment for Hip and Knee Osteoarthritis in Older People: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2020; 9(4):1167. https://doi.org/10.3390/jcm9041167
Chicago/Turabian StyleZampogna, Biagio, Rocco Papalia, Giuseppe Francesco Papalia, Stefano Campi, Sebastiano Vasta, Ferruccio Vorini, Chiara Fossati, Guglielmo Torre, and Vincenzo Denaro. 2020. "The Role of Physical Activity as Conservative Treatment for Hip and Knee Osteoarthritis in Older People: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 9, no. 4: 1167. https://doi.org/10.3390/jcm9041167
APA StyleZampogna, B., Papalia, R., Papalia, G. F., Campi, S., Vasta, S., Vorini, F., Fossati, C., Torre, G., & Denaro, V. (2020). The Role of Physical Activity as Conservative Treatment for Hip and Knee Osteoarthritis in Older People: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 9(4), 1167. https://doi.org/10.3390/jcm9041167






