Sperm Antioxidant Biomarkers and Their Correlation with Clinical Condition and Lifestyle with Regard to Male Reproductive Potential
Abstract
:1. Introduction
2. Experimental Section
2.1. Lipid Peroxidation Product; MDA—Malonyldialdehyde
2.2. Total Redox Antioxidant Potential (TRAP)
2.3. Reduced Glutathione (GSH)
2.4. Total Protein Levels
2.5. Statistical Analysis
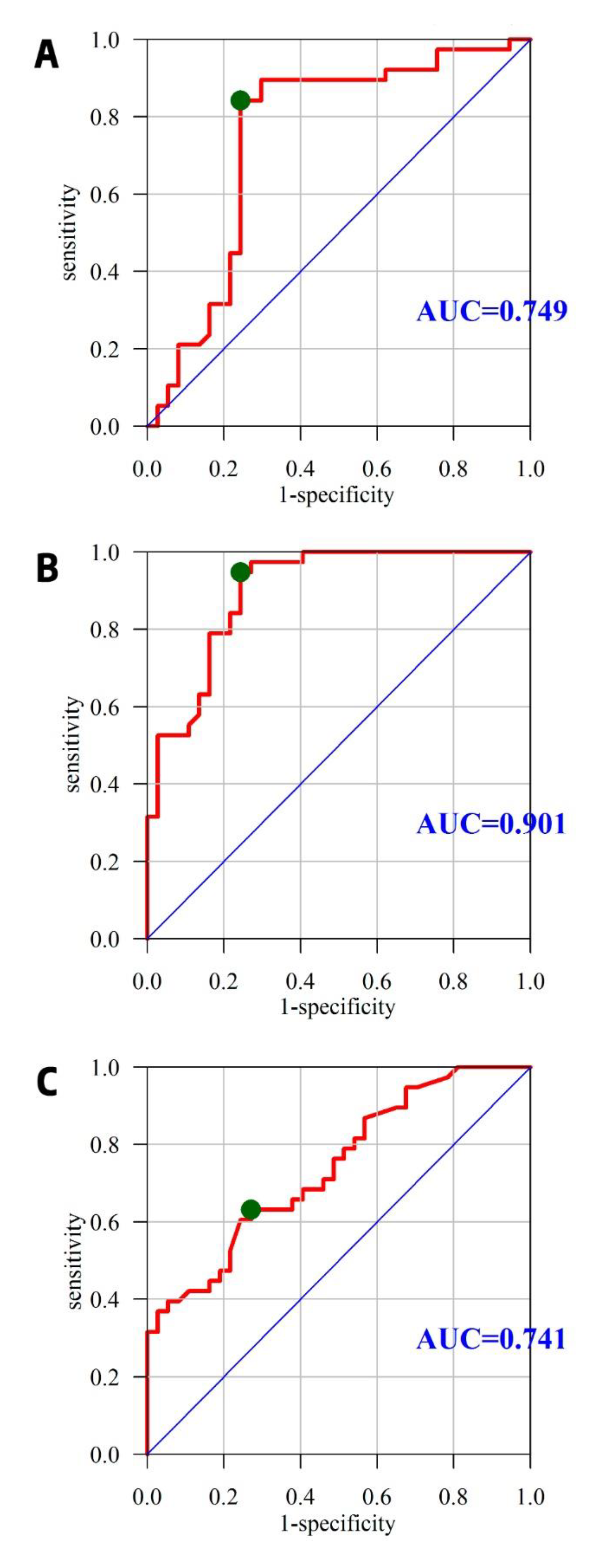
3. Results
3.1. Demographic Analysis
3.2. Questionnaire Data
3.3. Analysis of Basic Semen Parameters
3.4. Analysis of Selected OxS Indices
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zegers-Hochschild, F.; Adamson, G.D.; de Mouzon, J.; Ishihara, O.; Mansour, R.; Nygren, K.; Sullivan, E.; Vanderpoel, S. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil. Steril. 2009, 92, 1520–1524. [Google Scholar] [CrossRef]
- World Health Organization, Department of Reproductive Health and Research. WHO Laboratory Manual for the Examination and Processing of Human Semen, 5th ed.; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Agarwal, A.; Mulgund, A.; Hamada, A.; Chyatte, M.R. A unique view on male infertility around the globe. Reprod. Biol. Endocrinol. 2015, 13, 37. [Google Scholar] [CrossRef] [Green Version]
- Jaslow, C.R.; Carney, J.L.; Kutteh, W.H. Diagnostic factors identified in 1020 women with two versus three or more recurrent pregnancy losses. Fertil. Steril. 2010, 93, 1234–1243. [Google Scholar] [CrossRef]
- Lotti, F.; Maggi, M. Sexual dysfunction and male infertility. Nat. Rev. Urol. 2018, 15, 287–307. [Google Scholar] [CrossRef]
- Messerlian, C.; Williams, P.L.; Ford, J.B.; Chavarro, J.E.; Minguez-Alarcon, L.; Dadd, R.; Braun, J.M.; Gaskins, A.J.; Meeker, J.D.; James-Todd, T.; et al. The Environment and Reproductive Health (EARTH) Study: A Prospective Preconception Cohort. Hum. Reprod. Open 2018, 2018. [Google Scholar] [CrossRef]
- Kuczynski, W.; Kurzawa, R.; Oszukowski, P.; Pawelczyk, L.; Poreba, R.; Radowicki, S.; Szamatowicz, M.; Wolczynski, S. Polish Gynecological Society and Polish Society for Reproductive Medicine recommendations for the diagnosis and treatment of infertility. Ginekol. Pol. 2012, 83, 149–154. [Google Scholar] [PubMed]
- Central Statistical Office. Główny Urząd Statystyczny/Obszary Tematyczne/Ludność/Ludność/Powierzchnia i Ludność w Przekroju Terytorialnym w 2016 r. Available online: https://stat.gov.pl/obszary-tematyczne/ludnosc/ludnosc/malzenstwa-i-dzietnosc-w-polsce,23,1.html (accessed on 25 February 2018).
- Central Statistical Office. Główny Urząd Statystyczny. Wyniki badań bieżących—Baza Demografia. Available online: http://demografia.stat.gov.pl/bazademografia/Tables.aspx (accessed on 25 February 2018).
- Bablok, L.; Dziadecki, W.; Szymusik, I.; Wolczynski, S.; Kurzawa, R.; Pawelczyk, L.; Jedrzejczak, P.; Hanke, W.; Kaminski, P.; Wielgos, M. Patterns of infertility in Poland—Multicenter study. Neuro Endocrinol. Lett. 2011, 32, 799–804. [Google Scholar] [PubMed]
- Tuncdemir, M.; Yenmis, G.; Tombulturk, K.; Arkan, H.; Soydas, T.; Burak Tek, R.; Altintas, O.; Ozkara, H.; Kanigur-Sultuybek, G. NFKB1 rs28362491 and pre-miRNA-146a rs2910164 SNPs on E-Cadherin expression in case of idiopathic oligospermia: A case-control study. Int. J. Reprod. Biomed. Yazd Iran 2018, 16, 247–254. [Google Scholar] [CrossRef]
- Martin-Hidalgo, D.; Bragado, M.J.; Batista, A.R.; Oliveira, P.F.; Alves, M.G. Antioxidants and Male Fertility: From Molecular Studies to Clinical Evidence. Antioxidants 2019, 8. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Cao, X.; Pang, D.; Li, C.; Luo, Q.; Zou, Y.; Feng, B.; Li, L.; Cheng, A.; Chen, Z. Is male infertility associated with increased oxidative stress in seminal plasma? A-meta analysis. Oncotarget 2018, 9, 24494–24513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pahune, P.P.; Choudhari, A.R.; Muley, P.A. The total antioxidant power of semen and its correlation with the fertility potential of human male subjects. J. Clin. Diagn. Res. 2013, 7, 991–995. [Google Scholar] [CrossRef]
- Cho, C.-L.; Agarwal, A. Role of sperm DNA fragmentation in male factor infertility: A systematic review. Arab J. Urol. 2018, 16, 21–34. [Google Scholar] [CrossRef] [Green Version]
- Majzoub, A.; Arafa, M.; Mahdi, M.; Agarwal, A.; Al Said, S.; Al-Emadi, I.; El Ansari, W.; Alattar, A.; Al Rumaihi, K.; Elbardisi, H. Oxidation-reduction potential and sperm DNA fragmentation, and their associations with sperm morphological anomalies amongst fertile and infertile men. Arab J. Urol. 2018, 16, 87–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panner Selvam, M.K.; Agarwal, A. A systematic review on sperm DNA fragmentation in male factor infertility: Laboratory assessment. Arab J. Urol. 2018, 16, 65–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aitken, R.J. Reactive oxygen species as mediators of sperm capacitation and pathological damage. Mol. Reprod. Dev. 2017, 84, 1039–1052. [Google Scholar] [CrossRef] [PubMed]
- Du Plessis, S.S.; Agarwal, A.; Halabi, J.; Tvrda, E. Contemporary evidence on the physiological role of reactive oxygen species in human sperm function. J. Assist. Reprod. Genet. 2015, 32, 509–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sabeti, P.; Pourmasumi, S.; Rahiminia, T.; Akyash, F.; Talebi, A.R. Etiologies of sperm oxidative stress. Int. J. Reprod. Biomed. Yazd Iran 2016, 14, 231–240. [Google Scholar] [CrossRef]
- Agarwal, A.; Said, T.M. Role of sperm chromatin abnormalities and DNA damage in male infertility. Hum. Reprod. Update 2003, 9, 331–345. [Google Scholar] [CrossRef] [Green Version]
- Kumar, N.; Singh, A.K. Reactive oxygen species in seminal plasma as a cause of male infertility. J. Gynecol. Obstet. Hum. Reprod. 2018, 47, 565–572. [Google Scholar] [CrossRef]
- Lee, G.S.; Park, J.C.; Rhee, J.H.; Kim, J.I. Etiologic characteristics and index pregnancy outcomes of recurrent pregnancy losses in Korean women. Obstet. Gynecol. Sci. 2016, 59, 379–387. [Google Scholar] [CrossRef] [Green Version]
- De Geyter, C.; Calhaz-Jorge, C.; Kupka, M.S.; Wyns, C.; Mocanu, E.; Motrenko, T.; Scaravelli, G.; Smeenk, J.; Vidakovic, S.; Goossens, V. ART in Europe, 2014: Results generated from European registries by ESHRE: The European IVF-monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). Hum. Reprod. 2018, 33, 1586–1601. [Google Scholar] [CrossRef] [PubMed]
- Jungwirth, A.; Diemer, T.; Kopa, Z.; Krausz, C.; Minhas, S.; Tournaye, H. Male Infertility. Available online: https://uroweb.org/guideline/male-infertility/ (accessed on 4 June 2020).
- Nieschlag, E. Male reproductive health and dysfunction, in male reproductive health and dysfunction. In Andrology; Behre, H.M., Nieschlag, S., Eds.; Springer: Berlin, Germany, 2010. [Google Scholar]
- Łukaszuk, K.; Kozioł, K.; Jakiel, G.; Jakimiuk, A.; Jędrzejczak, P.; Kuczyński, W.; Kurzawa, R.; Pawelczyk, L.; Radwan, M.; Spaczyński, R.; et al. Diagnostyka i leczenie niepłodności—rekomendacje Polskiego Towarzystwa Medycyny Rozrodu i Embriologii (PTMRiE) oraz Polskiego Towarzystwa Ginekologów i Położników (PTGP). Ginekol. Perinatol. Praktyczna 2018, 3, 112–140. [Google Scholar]
- Nicopoullos, J.; Vicens-Morton, A.; Lewis, S.E.M.; Lee, K.; Larsen, P.; Ramsay, J.; Yap, T.; Minhas, S. Novel use of COMET parameters of sperm DNA damage may increase its utility to diagnose male infertility and predict live births following both IVF and ICSI. Hum. Reprod. 2019, 34, 1915–1923. [Google Scholar] [CrossRef] [PubMed]
- Garrido, N.; Hervas, I. Personalized Medicine in Infertile Men. Urol. Clin. N. Am. 2020, 47, 245–255. [Google Scholar] [CrossRef]
- Li, L.; Li, H.; Tian, Y.; Hu, M.; Le, F.; Wang, L.; Liu, X.; Jin, F. Differential microRNAs expression in seminal plasma of normospermic patients with different sperm DNA fragmentation indexes. Reprod. Toxicol. 2020, 94, 8–12. [Google Scholar] [CrossRef]
- Poli, D.; Andreoli, R.; Moscato, L.; Pela, G.; de Palma, G.; Cavallo, D.; Petyx, M.; Pelosi, G.; Corradi, M.; Goldoni, M. The Relationship Between Widespread Pollution Exposure and Oxidized Products of Nucleic Acids in Seminal Plasma and Urine in Males Attending a Fertility Center. Int. J. Environ. Res. Public Health 2020, 17. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.; Xu, X. scRNA-seq Profiling of Human Testes Reveals the Presence of the ACE2 Receptor, A Target for SARS-CoV-2 Infection in Spermatogonia, Leydig and Sertoli Cells. Cells 2020, 9. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Y.; Meng, T.; Wu, L.; Duan, Y.; Li, G.; Shi, C.; Zhang, H.; Peng, Z.; Fan, C.; Ma, J.; et al. Association between ambient temperature and semen quality: A longitudinal study of 10,802 men in China. Environ. Int. 2020, 135, 105364. [Google Scholar] [CrossRef]
- Buege, J.A.; Aust, S.D. Microsomal lipid peroxidation. Methods Enzymol. 1978, 52, 302–310. [Google Scholar]
- Gutteridge, J.M. Aspects to consider when detecting and measuring lipid peroxidation. Free Radic. Res. Commun. 1986, 1, 173–184. [Google Scholar] [CrossRef]
- Jentzsch, A.M.; Bachmann, H.; Furst, P.; Biesalski, H.K. Improved analysis of malondialdehyde in human body fluids. Free Radic. Biol. Med. 1996, 20, 251–256. [Google Scholar] [CrossRef]
- Benzie, I.F.; Strain, J.J. The ferric reducing ability of plasma (FRAP) as a measure of “antioxidant power”: The FRAP assay. Anal. Biochem. 1996, 239, 70–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riddles, P.W.; Blakeley, R.L.; Zerner, B. Reassessment of Ellman’s reagent. Methods Enzymol. 1983, 91, 49–60. [Google Scholar] [PubMed]
- Eyer, P.; Worek, F.; Kiderlen, D.; Sinko, G.; Stuglin, A.; Simeon-Rudolf, V.; Reiner, E. Molar absorption coefficients for the reduced Ellman reagent: Reassessment. Anal. Biochem. 2003, 312, 224–227. [Google Scholar] [CrossRef]
- Ellman, G.L. Tissue sulfhydryl groups. Arch. Biochem. Biophys. 1959, 82, 70–77. [Google Scholar] [CrossRef]
- Yan, X.; Dong, L.; Liu, Y.; Yang, F.; Tan, K.; Li, J.; Chang, D.; Yu, X. Effects of physical exercises on semen quality and reproductive outcomes in male infertility: A protocol for systematic review and meta-analysis of randomized controlled trials. Med. Baltim. 2019, 98, e17494. [Google Scholar] [CrossRef]
- Hinkle, D.; Wiersma, W.; Jurs, S. Applied Statistics for the Behavioral Sciences, 5th ed.; Houghton Mifflin: Boston, MA, USA, 2003. [Google Scholar]
- Parikh, R.; Mathai, A.; Parikh, S.; Chandra Sekhar, G.; Thomas, R. Understanding and using sensitivity, specificity and predictive values. Indian J. Ophthalmol. 2008, 56, 45–50. [Google Scholar] [CrossRef]
- Alahmar, A.T. The effects of oral antioxidants on the semen of men with idiopathic oligoasthenoteratozoospermia. Clin. Exp. Reprod. Med. 2018, 45, 57–66. [Google Scholar] [CrossRef]
- Moraes, C.R.; Meyers, S. The sperm mitochondrion: Organelle of many functions. Anim. Reprod. Sci. 2018, 194, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Atig, F.; Raffa, M.; Habib, B.-A.; Kerkeni, A.; Saad, A.; Ajina, M. Impact of seminal trace element and glutathione levels on semen quality of Tunisian infertile men. BMC Urol. 2012, 12, 6. [Google Scholar] [CrossRef] [Green Version]
- Nenkova, G.; Petrov, L.; Alexandrova, A. Role of Trace Elements for Oxidative Status and Quality of Human Sperm. Balk. Med. J. 2017, 34, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, A.; Verma, A.; Majumdar, S.; Khanduja, K.L. Status of vitamin E and reduced glutathione in semen of oligozoospermic and azoospermic patients. Asian J. Androl. 2000, 2, 225–228. [Google Scholar] [PubMed]
- Ochsendorf, F.R.; Buhl, R.; Bastlein, A.; Beschmann, H. Glutathione in spermatozoa and seminal plasma of infertile men. Hum. Reprod. 1998, 13, 353–359. [Google Scholar] [CrossRef] [Green Version]
- Lenzi, A.; Culasso, F.; Gandini, L.; Lombardo, F.; Dondero, F. Placebo-controlled, double-blind, cross-over trial of glutathione therapy in male infertility. Hum. Reprod. 1993, 8, 1657–1662. [Google Scholar] [CrossRef]
- Ansari, M.S.; Rakha, B.A.; Andrabi, S.M.H.; Ullah, N.; Iqbal, R.; Holt, W.V.; Akhter, S. Glutathione-supplemented tris-citric acid extender improves the post-thaw quality and in vivo fertility of buffalo (Bubalus bubalis) bull spermatozoa. Reprod. Biol. 2012, 12, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Dong, S. Glutathione in combination with trehalose has supplementary beneficial effects on cryopreserved red deer (cervus elaphus) sperm. Am. J. Reprod. Immunol. 2017, 77, e12610. [Google Scholar] [CrossRef]
- Zhu, Z.; Ren, Z.; Fan, X.; Pan, Y.; Lv, S.; Pan, C.; Lei, A.; Zeng, W. Cysteine protects rabbit spermatozoa against reactive oxygen species-induced damages. PLoS ONE 2017, 12, e0181110. [Google Scholar] [CrossRef] [Green Version]
- Aydemir, B.; Onaran, I.; Kiziler, A.R.; Alici, B.; Akyolcu, M.C. Increased oxidative damage of sperm and seminal plasma in men with idiopathic infertility is higher in patients with glutathione S-transferase Mu-1 null genotype. Asian J. Androl. 2007, 9, 108–115. [Google Scholar] [CrossRef]
- Raijmakers, M.T.M.; Roelofs, H.M.J.; Steegers, E.A.P.; Steegers-Theunissen, R.; Regine, P.M.; Mulder, T.P.J.; Knapen, M.F.C.M.; Wong, W.Y.; Peters, W.H.M. Glutathione and glutathione S-transferases A1-1 and P1-1 in seminal plasma may play a role in protecting against oxidative damage to spermatozoa. Fertil. Steril. 2003, 79, 169–172. [Google Scholar] [CrossRef]
- Kiziler, A.R.; Aydemir, B.; Onaran, I.; Alici, B.; Ozkara, H.; Gulyasar, T.; Akyolcu, M.C. High levels of cadmium and lead in seminal fluid and blood of smoking men are associated with high oxidative stress and damage in infertile subjects. Biol. Trace Elem. Res. 2007, 120, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, L.; Jalali, S.; Shami, S.A.; Akram, Z.; Batool, S.; Kalsoom, O. Effects of cryopreservation on sperm DNA integrity in normospermic and four categories of infertile males. Syst. Biol. Reprod. Med. 2010, 56, 74–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shete, S.; Hulke, S.; Thakare, A.; Patil, P. Study of reduced glutathione in seminal plasma and spermatozoa nuclear chromatin decondensation test (NCDT) in human subjects with different fertility potential. Int. J. Biol. Med. Res. 2012, 3, 1636–1639. [Google Scholar]
- Benedetti, S.; Tagliamonte, M.C.; Catalani, S.; Primiterra, M.; Canestrari, F.; De Stefani, S.; Palini, S.; Bulletti, C. Differences in blood and semen oxidative status in fertile and infertile men, and their relationship with sperm quality. Reprod. Biomed. Online 2012, 25, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Moretti, E.; Collodel, G.; Fiaschi, A.I.; Micheli, L.; Iacoponi, F.; Cerretani, D. Nitric oxide, malondialdheyde and non-enzymatic antioxidants assessed in viable spermatozoa from selected infertile men. Reprod. Biol. 2017, 17, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, V.; Ravichandran, A.; Thiagarajan, N.; Govindarajan, M.; Dhandayuthapani, S.; Suresh, S. Seminal reactive oxygen species and total antioxidant capacity: Correlations with sperm parameters and impact on male infertility. Clin. Exp. Reprod. Med. 2018, 45, 88–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Layali, I.; Tahmasbpour, E.; Joulaei, M.; Jorsaraei, S.G.A.; Farzanegi, P. Total antioxidant capacity and lipid peroxidation in semen of patient with hyperviscosity. Cell J. 2015, 16, 554–559. [Google Scholar]
- Fazeli, F.; Salimi, S. Correlation of Seminal Plasma Total Antioxidant Capacity and Malondialdehyde Levels With Sperm Parameters in Men With Idiopathic Infertility. Avicenna J. Med. Biochem. 2016. [Google Scholar] [CrossRef] [Green Version]
- Li, K.; Shang, X.; Chen, Y. Determination of lipid peroxidation in human seminal plasma by high performance liquid chromatography and its diagnostic value of male infertility. Se Pu Chin. J. Chromatogr. 2004, 22, 412–415. [Google Scholar]
- Tavilani, H.; Doosti, M.; Saeidi, H. Malondialdehyde levels in sperm and seminal plasma of asthenozoospermic and its relationship with semen parameters. Clin. Chim. Acta 2005, 356, 199–203. [Google Scholar] [CrossRef]
- Nouri, M.; Aliyeh, G.; Laya, F.; Vahideh, S.; Novin, M. Vitamins C, E and lipid peroxidation levels in sperm and seminal plasma of asthenoteratozoospermic and normozoospermic men. Iran. J. Reprod. Med. 2008, 6, 1–5. [Google Scholar]
- Abdul-Rasheed, O.F.; Farid, Y.Y.; Al-Nasiri, U.S. Coenzyme Q10 and oxidative stress markers in seminal plasma of Iraqi patients with male infertility. Saudi Med. J. 2010, 31, 501–506. [Google Scholar] [PubMed]
- Badade, Z.; More, K.; Narshetty, J. Oxidative stress adversely affects spermatogenesis in male infertility. Biomed. Res. 2011, 22, 1–3. [Google Scholar]
- Mehrotra, A.; Katiyar, D.K.; Agarwal, A.; Das, V.; Pant, K.K. Role of total antioxidant capacity and lipid peroxidation in fertile and infertile men. Biomed. Res. 2013, 24, 347–352. [Google Scholar]
- Collodel, G.; Moretti, E.; Micheli, L.; Menchiari, A.; Moltoni, L.; Cerretani, D. Semen characteristics and malondialdehyde levels in men with different reproductive problems. Andrology 2015, 3, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Hosen, M.B.; Islam, M.R.; Begum, F.; Kabir, Y.; Howlader, M.Z.H. Oxidative stress induced sperm DNA damage, a possible reason for male infertility. Iran. J. Reprod. Med. 2015, 13, 525–532. [Google Scholar] [PubMed]
- El-Taieb, M.A.; Ali, M.A.; Nada, E.A. Oxidative stress and acrosomal morphology: A cause of infertility in patients with normal semen parameters. Middle East Fertil. Soc. J. 2015, 20, 79–85. [Google Scholar] [CrossRef]
- Micheli, L.; Cerretani, D.; Collodel, G.; Menchiari, A.; Moltoni, L.; Fiaschi, A.I.; Moretti, E. Evaluation of enzymatic and non-enzymatic antioxidants in seminal plasma of men with genitourinary infections, varicocele and idiopathic infertility. Andrology 2016, 4, 456–464. [Google Scholar] [CrossRef] [Green Version]
- Taken, K.; Alp, H.H.; Eryilmaz, R.; Donmez, M.I.; Demir, M.; Gunes, M.; Aslan, R.; Sekeroglu, M.R. Oxidative DNA Damage to Sperm Cells and Peripheral Blood Leukocytes in Infertile Men. Med. Sci. Monit. 2016, 22, 4289–4296. [Google Scholar] [CrossRef]
- Atig, F.; Kerkeni, A.; Saad, A.; Ajina, M. Effects of reduced seminal enzymatic antioxidants on sperm DNA fragmentation and semen quality of Tunisian infertile men. J. Assist. Reprod. Genet. 2017, 34, 373–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sahnoun, S.; Sellami, A.; Chakroun, N.; Mseddi, M.; Attia, H.; Rebai, T.; Lassoued, S. Human sperm Toll-like receptor 4 (TLR4) mediates acrosome reaction, oxidative stress markers, and sperm parameters in response to bacterial lipopolysaccharide in infertile men. J. Assist. Reprod. Genet. 2017, 34, 1067–1077. [Google Scholar] [CrossRef]
- Hassanin, A.M.; Ahmed, H.H.; Kaddah, A.N. A global view of the pathophysiology of varicocele. Andrology 2018, 6, 654–661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Musset, B.; Clark, R.A.; DeCoursey, T.E.; Petheo, G.L.; Geiszt, M.; Chen, Y.; Cornell, J.E.; Eddy, C.A.; Brzyski, R.G.; El Jamali, A. NOX5 in human spermatozoa: Expression, function, and regulation. J. Biol. Chem. 2012, 287, 9376–9388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suleiman, S.A.; Ali, M.E.; Zaki, Z.M.; el-Malik, E.M.; Nasr, M.A. Lipid peroxidation and human sperm motility: Protective role of vitamin E. J. Androl. 1996, 17, 530–537. [Google Scholar]
- Kodama, H.; Yamaguchi, R.; Fukuda, J.; Kasai, H.; Tanaka, T. Increased oxidative deoxyribonucleic acid damage in the spermatozoa of infertile male patients. Fertil. Steril. 1997, 68, 519–524. [Google Scholar] [CrossRef]
- Omu, A.E.; Al-Azemi, M.K.; Kehinde, E.O.; Anim, J.T.; Oriowo, M.A.; Mathew, T.C. Indications of the mechanisms involved in improved sperm parameters by zinc therapy. Med. Princ. Pract. 2008, 17, 108–116. [Google Scholar] [CrossRef]
- Greco, E.; Iacobelli, M.; Rienzi, L.; Ubaldi, F.; Ferrero, S.; Tesarik, J. Reduction of the incidence of sperm DNA fragmentation by oral antioxidant treatment. J. Androl. 2005, 26, 349–353. [Google Scholar] [CrossRef]
- Keskes-Ammar, L.; Feki-Chakroun, N.; Rebai, T.; Sahnoun, Z.; Ghozzi, H.; Hammami, S.; Zghal, K.; Fki, H.; Damak, J.; Bahloul, A. Sperm oxidative stress and the effect of an oral vitamin E and selenium supplement on semen quality in infertile men. Arch. Androl. 2003, 49, 83–94. [Google Scholar] [CrossRef]
- Hansen, J.M.; Watson, W.H.; Jones, D.P. Compartmentation of Nrf-2 redox control: Regulation of cytoplasmic activation by glutathione and DNA binding by thioredoxin-1. Toxicol. Sci. 2004, 82, 308–317. [Google Scholar] [CrossRef] [PubMed]
- Boitani, C.; Puglisi, R. Selenium, a key element in spermatogenesis and male fertility. Adv. Exp. Med. Biol. 2008, 636, 65–73. [Google Scholar]
- Kobayashi, T.; Miyazaki, T.; Natori, M.; Nozawa, S. Protective role of superoxide dismutase in human sperm motility: Superoxide dismutase activity and lipid peroxide in human seminal plasma and spermatozoa. Hum. Reprod. 1991, 6, 987–991. [Google Scholar] [CrossRef]
- Griveau, J.F.; Le Lannou, D. Effects of antioxidants on human sperm preparation techniques. Int. J. Androl. 1994, 17, 225–231. [Google Scholar] [CrossRef]
- Perumal, P. Effect of Superoxide Dismutase on Semen Parameters and Antioxidant Enzyme Activities of Liquid Stored (5 °C) Mithun (Bos frontalis) Semen. J. Anim. 2014, 2014, 821954. [Google Scholar] [CrossRef] [Green Version]
- Alsalman, A.R.S.; Almashhedy, L.A.; Hadwan, M.H. Effect of Oral Zinc Supplementation on the Thiol Oxido-Reductive Index and Thiol-Related Enzymes in Seminal Plasma and Spermatozoa of Iraqi Asthenospermic Patients. Biol. Trace Elem. Res. 2018, 184, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Hosseinzadeh Colagar, A.; Karimi, F.; Jorsaraei, S.G.A. Correlation of sperm parameters with semen lipid peroxidation and total antioxidants levels in astheno-and oligoasheno-teratospermic men. Iran. Red Crescent Med. J. 2013, 15, 780–785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yousefniapasha, Y.; Jorsaraei, G.; Gholinezhadchari, M.; Mahjoub, S.; Hajiahmadi, M.; Farsi, M. Nitric oxide levels and total antioxidant capacity in the seminal plasma of infertile smoking men. Cell J. 2015, 17, 129–136. [Google Scholar]
- N’Guessan, M.-F.; Coulibaly, F.; Kouassi, K.; Guillaume, Y.; Coulibaly, N.; Ayekoue, E.; Zi, K.; M’Boh, G.; Souleymane, M.; Yapi, H.; et al. Lipid peroxidation and total antioxidant capacity in azoospermic semen. Ann. Med. Biomed. Sci. 2016, 2, 1–46. [Google Scholar]
- Turk, S.; Mandar, R.; Mahlapuu, R.; Viitak, A.; Punab, M.; Kullisaar, T. Male infertility: Decreased levels of selenium, zinc and antioxidants. J. Trace Elem. Med. Biol. 2014, 28, 179–185. [Google Scholar] [CrossRef]
- Khosrowbeygi, A.; Zarghami, N. Levels of oxidative stress biomarkers in seminal plasma and their relationship with seminal parameters. BMC Clin. Pathol. 2007, 7, 6. [Google Scholar] [CrossRef] [Green Version]
- Agarwal, A.; Desai, N.R.; Makker, K.; Varghese, A.; Mouradi, R.; Sabanegh, E.; Sharma, R. Effects of radiofrequency electromagnetic waves (RF-EMW) from cellular phones on human ejaculated semen: An in vitro pilot study. Fertil. Steril. 2009, 92, 1318–1325. [Google Scholar] [CrossRef]
- De Iuliis, G.N.; Newey, R.J.; King, B.V.; Aitken, R.J. Mobile phone radiation induces reactive oxygen species production and DNA damage in human spermatozoa in vitro. PLoS ONE 2009, 4, e6446. [Google Scholar] [CrossRef]
- Mailankot, M.; Kunnath, A.P.; Jayalekshmi, H.; Koduru, B.; Valsalan, R. Radio frequency electromagnetic radiation (RF-EMR) from GSM (0.9/1.8GHz) mobile phones induces oxidative stress and reduces sperm motility in rats. Clinics 2009, 64, 561–565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Micillo, A.; Vassallo, M.R.C.; Cordeschi, G.; D’Andrea, S.; Necozione, S.; Francavilla, F.; Francavilla, S.; Barbonetti, A. Semen leukocytes and oxidative-dependent DNA damage of spermatozoa in male partners of subfertile couples with no symptoms of genital tract infection. Andrology 2016, 4, 808–815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agarwal, A.; Mulgund, A.; Alshahrani, S.; Assidi, M.; Abuzenadah, A.M.; Sharma, R.; Sabanegh, E. Reactive oxygen species and sperm DNA damage in infertile men presenting with low level leukocytospermia. Reprod. Biol. Endocrinol. 2014, 12, 126. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Parameter | Patients | Control | p ** | ||
|---|---|---|---|---|---|
| Mean (SD) | Median (Quartiles) | Mean (SD) | Median (Quartiles) | ||
| Age (years) | 34.53 (3.95) | 35 (32–37) | 37.05 (2.46) | 37 (36–39) | 0.001 p |
| Age of partner (years) | 32.13 (3.04) | 32 (30–34) | 34.59 (2.55) | 35 (34–36) | <0.001 p |
| Height (cm) | 179.21 (7.33) | 180 (173–183.5) | 179.03 (6.47) | 180 (174–184) | 0.909 p |
| Weight (kg) | 85.33 (11.6) | 89 (74–92.88) | 89.62 (7.89) | 90 (86–94) | 0.122 NP |
| BMI (kg/m2) | 26.5 (2.75) | 26.26 (24.25–27.99) | 28 (2.46) | 27.77 (26.88–29.8) | 0.016 p |
| Parameter | Patients | Control | P ** | ||
|---|---|---|---|---|---|
| Mean (SD) | Median (Quartil–es) | Mean (SD) | Median (Quartiles) | ||
| Concentration (mln/mL) | 29.16 (10.57) | 35.3 (8.03) | 0.006 P | ||
| Plasma membrane integrity (%) | 53.96 (11.11) | 82.4 (68.6–90) | <0.001 NP | ||
| Viability with Eosin Staining (%) | 58.23 (12.31) | 84.6 (70–91) | <0.001 NP | ||
| Total sperm cell count (mL) | 70.8 (43.81–108.7) | 109.72 (56.31) | 0.063 NP | ||
| Volume (mL) | 2.5 (2–3.2) | 2.9 (1.02) | 0.186 NP | ||
| Motile sperm progressive cells (%) | 29 (21.25–33) | 48.97 (15.39) | <0.001 NP | ||
| Normal morphology (%) | 52.25 (41.25 - 60) | 65.21 (13.27) | <0.001 NP | ||
| Nonmoving motility of sperm (%) | 64 (59.25–71.5) | 43 (31–57) | <0.001 NP | ||
| Nonprogressive motility of sperm (%) | 5 (4–7.75) | 5 (3–12) | 0.987 NP | ||
| Parameter | Patients | Control | p ** | ||
|---|---|---|---|---|---|
| Mean (SD) | Median (Quartiles) | Mean (SD) | Median Quartiles) | ||
| TRAP (mmol/L) | 4.13 (1.77) | 6.93 (5.52–7.42) | <0.001 NP | ||
| GSH (µmol/L) | 44.14 (38.78–60.21) | 109.31 (39.26) | <0.001 NP | ||
| Protein (mg/mL) | 23.39 (21.94–25.04) | 22.31 (21.35–24.52) | 0.277 NP | ||
| MDA (µmol/mL) | 5.29 (4.63–6.89) | 4.57 (4.12–5.16) | <0.001 NP | ||
| Parameter | Correlation with the Period of Trying to Have a Child | |
|---|---|---|
| Correlation Coefficient | P | |
| Total sperm cell count (mL) | −0.358 | 0.002 |
| Sum of progressive and non-progressive cells (%) | −0.677 | <0.001 |
| Plasma membrane integrity (%) | −0.597 | <0.001 |
| Viability with Eosin Staining (%) | −0.506 | <0.001 |
| TRAP (mmol/L) | −0.509 | <0.001 |
| Protein (mg/mL) | 0.095 | 0.419 |
| GSH (µmol/L) | −0.578 | <0.001 |
| MDA (µmol/mL) | 0.421 | <0.001 |
| Parameter | Correlation with TRAP | |
|---|---|---|
| Correlation Coefficient | P | |
| Concentration (mln/mL) | 0.508 | <0.001 |
| Total sperm cell count (mL) | 0.476 | <0.001 |
| Motile sperm progressive cells (%) | 0.631 | <0.001 |
| Non-progressive motility of sperm (%) | 0.029 | 0.804 |
| Sum of progressive and non-progressive cells (%) | 0.608 | <0.001 |
| Plasma membrane integrity (%) | 0.759 | <0.001 |
| Viability with Eosin Staining (%) | 0.663 | <0.001 |
| Normal morphology (%) | 0.418 | <0.001 |
| Parameter | Correlation with GSH | |
|---|---|---|
| Correlation Coefficient | P | |
| Concentration (mln/mL) | 0.452 | <0.001 |
| Total sperm cell count (mL) | 0.394 | <0.001 |
| Motile sperm progressive cells (%) | 0.68 | <0.001 |
| Non-progressive motility of sperm (%) | 0.022 | 0.849 |
| Sum of progressive and non-progressive cells (%) | 0.661 | <0.001 |
| Plasma membrane integrity (%) | 0.795 | <0.001 |
| Viability with Eosin Staining (%) | 0.72 | <0.001 |
| Normal morphology (%) | 0.415 | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krzyściak, W.; Papież, M.; Bąk, E.; Morava, E.; Krzyściak, P.; Ligęzka, A.; Gniadek, A.; Vyhouskaya, P.; Janeczko, J. Sperm Antioxidant Biomarkers and Their Correlation with Clinical Condition and Lifestyle with Regard to Male Reproductive Potential. J. Clin. Med. 2020, 9, 1785. https://doi.org/10.3390/jcm9061785
Krzyściak W, Papież M, Bąk E, Morava E, Krzyściak P, Ligęzka A, Gniadek A, Vyhouskaya P, Janeczko J. Sperm Antioxidant Biomarkers and Their Correlation with Clinical Condition and Lifestyle with Regard to Male Reproductive Potential. Journal of Clinical Medicine. 2020; 9(6):1785. https://doi.org/10.3390/jcm9061785
Chicago/Turabian StyleKrzyściak, Wirginia, Monika Papież, Ewelina Bąk, Eva Morava, Paweł Krzyściak, Anna Ligęzka, Agnieszka Gniadek, Palina Vyhouskaya, and Jarosław Janeczko. 2020. "Sperm Antioxidant Biomarkers and Their Correlation with Clinical Condition and Lifestyle with Regard to Male Reproductive Potential" Journal of Clinical Medicine 9, no. 6: 1785. https://doi.org/10.3390/jcm9061785





