Accuracy of Panoramic Radiograph for Diagnosing Periodontitis Comparing to Clinical Examination
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Eligibility Criteria
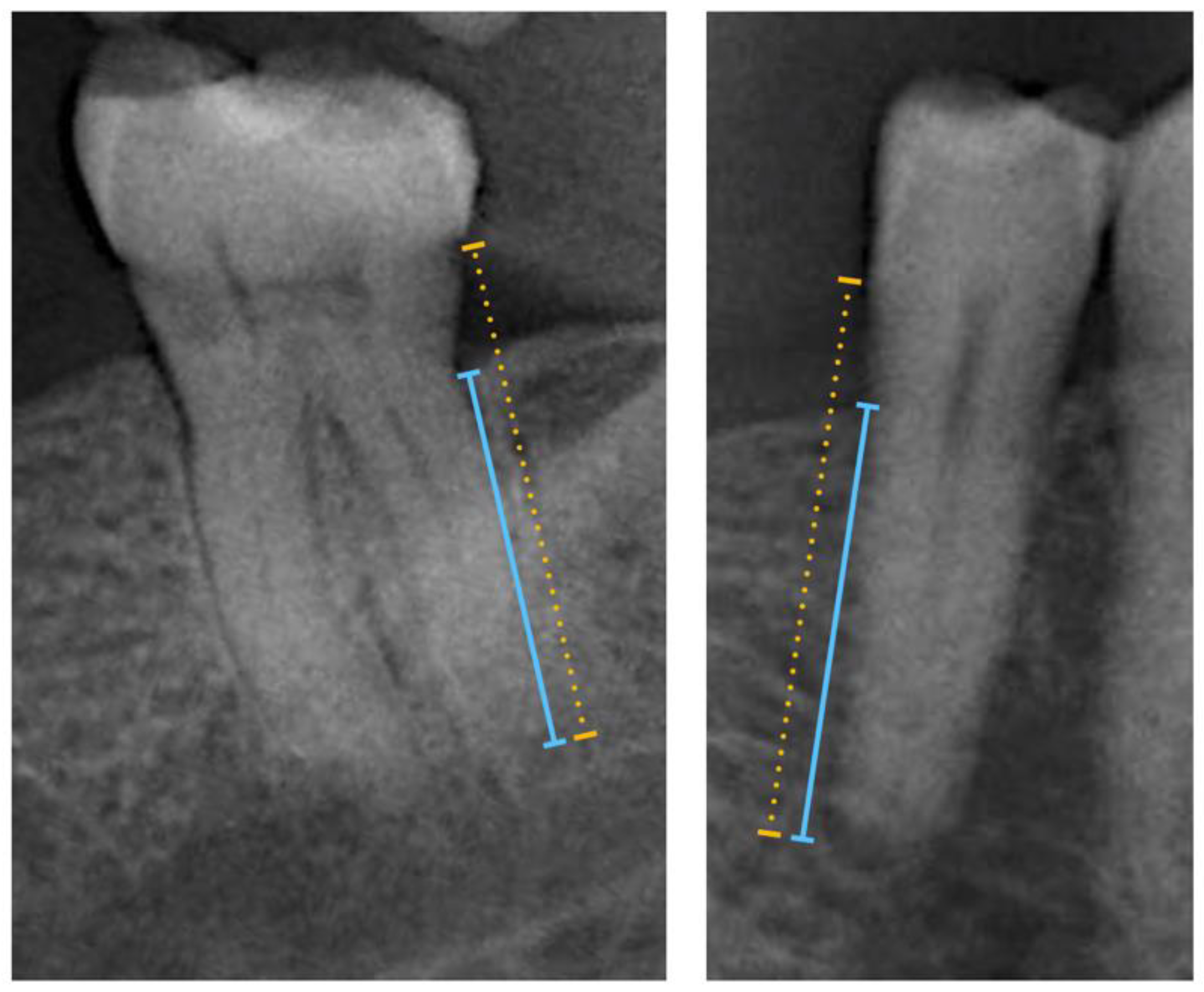
2.2. Radiographic-Based Periodontal Bone Loss (PBL) Method
2.3. Panoramic Radiographs Quality Assessment
2.4. Measurement Reliability and Reproducibility
2.5. Data Management, Test Methods and Analysis
3. Results
3.1. Participant Characteristics
3.2. Accuracy Performance of R-PBL for the Presence of Periodontitis
3.3. Accuracy Performance of R-PBL for the Staging of Periodontitis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Section & Topic | No | Item | Reported on Page |
|---|---|---|---|
| Title or Abstract | |||
| 1 | Identification as a study of diagnostic accuracy using at least one measure of accuracy (such as sensitivity, specificity, predictive values, or AUC) | 1 | |
| Abstract | |||
| 2 | Structured summary of study design, methods, results, and conclusions (for specific guidance, see STARD for Abstracts) | 1 | |
| Introduction | |||
| 3 | Scientific and clinical background, including the intended use and clinical role of the index test | 1–2 | |
| 4 | Study objectives and hypotheses | 2 | |
| Methods | |||
| Study design | 5 | Whether data collection was planned before the index test and reference standard were performed (prospective study) or after (retrospective study) | 2 |
| Participants | 6 | Eligibility criteria | 2 |
| 7 | On what basis potentially eligible participants were identified (such as symptoms, results from previous tests, inclusion in registry) | 2 | |
| 8 | Where and when potentially eligible participants were identified (setting, location and dates) | 2 | |
| 9 | Whether participants formed a consecutive, random or convenience series | 2 | |
| Test methods | 10a | Index test, in sufficient detail to allow replication | 2–3 |
| 10b | Reference standard, in sufficient detail to allow replication | 2–3 | |
| 11 | Rationale for choosing the reference standard (if alternatives exist) | 2–3 | |
| 12a | Definition of and rationale for test positivity cut-offs or result categories of the index test, distinguishing pre-specified from exploratory | NA | |
| 12b | Definition of and rationale for test positivity cut-offs or result categories of the reference standard, distinguishing pre-specified from exploratory | NA | |
| 13a | Whether clinical information and reference standard results were available to the performers/readers of the index test | NA | |
| 13b | Whether clinical information and index test results were available to the assessors of the reference standard | NA | |
| Analysis | 14 | Methods for estimating or comparing measures of diagnostic accuracy | 3–4 |
| 15 | How indeterminate index test or reference standard results were handled | 3–4 | |
| 16 | How missing data on the index test and reference standard were handled | 3–4 | |
| 17 | Any analyses of variability in diagnostic accuracy, distinguishing pre-specified from exploratory | 3–4 | |
| 18 | Intended sample size and how it was determined | 3–4 | |
| Results | |||
| Participants | 19 | Flow of participants, using a diagram | 4 |
| 20 | Baseline demographic and clinical characteristics of participants | for more details see [12,18] | |
| 21a | Distribution of severity of disease in those with the target condition | 4 | |
| 21b | Distribution of alternative diagnoses in those without the target condition | 4–5 | |
| 22 | Time interval and any clinical interventions between index test and reference standard | NA | |
| Test results | 23 | Cross tabulation of the index test results (or their distribution) by the results of the reference standard | 5–6 |
| 24 | Estimates of diagnostic accuracy and their precision (such as 95% confidence intervals) | 5–6 | |
| 25 | Any adverse events from performing the index test or the reference standard | NA | |
| Discussion | |||
| 26 | Study limitations, including sources of potential bias, statistical uncertainty, and generalisability | 6–8 | |
| 27 | Implications for practice, including the intended use and clinical role of the index test | 6–8 | |
| Other Information | |||
| 28 | Registration number and name of registry | NA | |
| 29 | Where the full study protocol can be accessed | NA | |
| 30 | Sources of funding and other support; role of funders | 7 |
References
- Beltrán-Aguilar, E.D.; Malvitz, D.M.; Lockwood, S.A.; Rozier, R.G.; Tomar, S.L. Oral Health Surveillance: Past, Present, and Future Challenges. J. Public Health Dent. 2003, 63, 141–149. [Google Scholar] [CrossRef]
- Beltrán-Aguilar, E.D.; Eke, P.I.; Thornton-Evans, G.; Petersen, P.E. Recording and surveillance systems for periodontal diseases. Periodontol. 2000 2012, 60, 40–53. [Google Scholar] [CrossRef]
- Kingman, A.; Susin, C.; Albandar, J.M. Effect of partial recording protocols on severity estimates of periodontal disease. J. Clin. Periodontol. 2008, 35, 659–667. [Google Scholar] [CrossRef]
- Tran, D.T.; Gay, I.; Du, X.L.; Fu, Y.; Bebermeyer, R.D.; Neumann, A.S.; Streckfus, C.; Chan, W.; Walji, M.F. Assessing periodontitis in populations: A systematic review of the validity of partial-mouth examination protocols. J. Clin. Periodontol. 2013, 40, 1064–1071. [Google Scholar] [CrossRef]
- Tran, D.T.; Gay, I.; Du, X.L.; Fu, Y.; Bebermeyer, R.D.; Neumann, A.S.; Streckfus, C.; Chan, W.; Walji, M.F. Assessment of partial-mouth periodontal examination protocols for periodontitis surveillance. J. Clin. Periodontol. 2014, 41, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Machado, V.; Botelho, J.; Mascarenhas, P.; Cavacas, M.A.; Alves, R.; Mendes, J.J. Partial recording protocols performance on the assessment of periodontitis severity and extent: Bias magnitudes, sensibility, and specificity. Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 2018, 59, 1. [Google Scholar] [CrossRef]
- Botelho, J.; Machado, V.; Proença, L.; Mendes, J.J. The 2018 periodontitis case definition improves accuracy performance of full-mouth partial diagnostic protocols. Sci. Rep. 2020, 10, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Clin. Periodontol. 2018, 45, 149–161. [Google Scholar] [CrossRef]
- Landry, R.; Jean, M. Periodontal Screening and Recording (PSR) Index: Precursors, utility and limitations in a clinical setting. Int. Dent. J. 2002, 52, 35–40. [Google Scholar] [CrossRef]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, 162–170. [Google Scholar] [CrossRef]
- Lang, N.P.; Bartold, P.M. Periodontal health. J. Clin. Periodontol. 2018, 45, 9–16. [Google Scholar] [CrossRef]
- Horner, K.; Rushton, V.; Walker, A.; Tsiklakis, K.; Hirschmann, P.N.; van der Stelt, P.F.; Glenny, A.-M.; Velders, X.L.; Pavitt, S. European Guidelines on Radiation Protection in Dental Radiology—The Safe Use of Radiographs in Dental Practice; The Publications Office of the European Union: Luxembourg, 2004; ISBN 9289459581.
- Krois, J.; Ekert, T.; Meinhold, L.; Golla, T.; Kharbot, B.; Wittemeier, A.; Dörfer, C.; Schwendicke, F. Deep Learning for the Radiographic Detection of Periodontal Bone Loss. Sci. Rep. 2019, 9, 8495. [Google Scholar] [CrossRef] [PubMed]
- Persson, R.E.; Tzannetou, S.; Feloutzis, A.G.; Brägger, U.; Persson, G.R.; Lang, N.P. Comparison between panoramic and intra-oral radiographs for the assessment of alveolar bone levels in a periodontal maintenance population. J. Clin. Periodontol. 2003, 30, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Hugoson, A.; Sjödin, B.; Norderyd, O. Trends over 30 years, 1973–2003, in the prevalence and severity of periodontal disease. J. Clin. Periodontol. 2008, 35, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Rydén, L.; Buhlin, K.; Ekstrand, E.; De Faire, U.; Gustafsson, A.; Holmer, J.; Kjellström, B.; Lindahl, B.; Norhammar, A.; Nygren, Å.; et al. Periodontitis Increases the Risk of a First Myocardial Infarction: A Report From the PAROKRANK Study. Circulation 2016, 133, 576–583. [Google Scholar] [CrossRef]
- Nordendahl, E.; Gustafsson, Å.; Norhammar, A.; Nasman, P.; Rydén, L.; Kjellström, B.; Kjellström, A.B. Severe Periodontitis Is Associated with Myocardial Infarction in Females. J. Dent. Res. 2018, 97, 1114–1121. [Google Scholar] [CrossRef] [PubMed]
- Botelho, J.; Machado, V.; Proença, L.; Alves, R.; Cavacas, M.A.; Amaro, L.; Mendes, J.J. Study of Periodontal Health in Almada-Seixal (SoPHiAS): A cross-sectional study in the Lisbon Metropolitan Area. Sci. Rep. 2019, 9, 15538–15610. [Google Scholar] [CrossRef]
- Bossuyt, P.M.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.; Irwig, L.; Lijmer, J.G.; Moher, D.; Rennie, U.; De Vet, H.C.W.; et al. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015, 351, 1–9. [Google Scholar] [CrossRef]
- Sabarudin, A.; Tiau, Y.J. Image quality assessment in panoramic dental radiography: A comparative study between conventional and digital systems. Quant. Imaging Med. Surg. 2013, 3, 43–48. [Google Scholar] [CrossRef]
- Eke, P.I.; Page, R.C.; Wei, L.; Thornton-Evans, G.; Genco, R.J. Update of the case definitions for population-based surveillance of periodontitis. J. Periodontol. 2012, 83, 1449–1554. [Google Scholar] [CrossRef]
- Glas, A.S.; Lijmer, J.G.; Prins, M.H.; Bonsel, G.J.; Bossuyt, P.M. The diagnostic odds ratio: A single indicator of test performance. J. Clin. Epidemiol. 2003, 56, 1129–1135. [Google Scholar] [CrossRef]
- Sachs, M.C. plotROC: A Tool for Plotting ROC Curves. J. Stat. Softw. 2017, 79, 1–19. [Google Scholar] [CrossRef]
- Peres, M.A.; MacPherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Tugnait, A.; Clerehugh, V.; Hirschmann, P. The usefulness of radiographs in diagnosis and management of periodontal diseases: A review. J. Dent. 2000, 28, 219–226. [Google Scholar] [CrossRef]
- Walsh, T.; Al-Hokail, O.; Fosam, E.B. The relationship of bone loss observed on panoramic radiographs with clinical periodontal screening. J. Clin. Periodontol. 1997, 24, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Åkesson, L.; Håkansson, J.; Rohlin, M. Comparison of panoramic and intraoral radiography and pocket probing for the measurement of the marginal bone level. J. Clin. Periodontol. 1992, 19, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions—Introduction and key changes from the 1999 classification. J. Clin. Periodontol. 2018, 45, 1–8. [Google Scholar] [CrossRef]
- Graetz, C.; Mann, L.; Krois, J.; Sälzer, S.; Kahl, M.; Springer, C.; Schwendicke, F. Comparison of periodontitis patients’ classification in the 2018 versus 1999 classification. J. Clin. Periodontol. 2019, 46, 908–917. [Google Scholar] [CrossRef] [PubMed]
- WHO. Public Health Surveillance. Available online: https://www.who.int/immunization/monitoring_surveillance/burden/vpd/en/ (accessed on 13 July 2020).

| Sensitivity (True Positive Rate) | TP/(TP + FN) | Proportion Positive Test Results Among Diseased |
| Specificity (True negative rate) | TN/(TN + FP) | Proportion negative test results among the “healthy” |
| Accuracy | (TP + TN)/(TP + TN + FP + FN) | Proportion of correctly identified subjects |
| Precision—Positive Predictive Values (PPV) | TP/(TP + FP) | - |
| Youden’s index | Sensitivity + Specificity − 1 | Measures the performance of a dichotomous diagnostic test |
| DOR | (TP/FN)/(FP/TN) | Ratio of the odds of positivity in disease relative to the odds of positivity in the non-diseased |
| DOR (95% CI) | 95% CI = log DOR ± 1.96SE(log DOR), where | - |
| F1 Score | 2TP/(2TP + FP + FN) | Harmonic mean of precision and sensitivity |
| Matthews Correlation Coefficient (MCC) | (TP × TN − FP × FN)/ | Measure of quality of binary classifications |
| Variable | Result |
|---|---|
| Age, mean (SD) | 59.9 (15.7) |
| Gender, n (%) | |
| Female | 253 (55.5) |
| Male | 203 (44.5) |
| Periodontal status (EFP/AAP 2018), n (%) | |
| Healthy | 185 (40.6) |
| Periodontitis | 271 (59.4) |
| Mild–Moderate (Stage I/II) | 160 (35.1) |
| Severe–Advanced (Stage III/IV) | 111 (24.3) |
| Periodontal status (CDC/AAP 2012), n (%) | |
| Healthy | 110 (24.1) |
| Periodontitis | 346 (75.9) |
| Mild–Moderate | 218 (47.8) |
| Severe | 128 (28.1) |
| Missing teeth | 9.2 (6.7) |
| BoP (%) | 13.9 (20.0) |
| Mean PD | 1.95 (0.81) |
| Mean CAL | 2.71 (1.47) |
| Mean Recession | 0.77 (0.98) |
| Panoramic radiograph quality | |
| Low quality | 281 (61.6) |
| High quality | 175 (38.4) |
| EFP/AAP 2018 | CDC/AAP 2012 | |||||
|---|---|---|---|---|---|---|
| Overall (n = 456) | High-Quality Radiography (n = 175) | Low-Quality Radiography (n = 281) | Overall (n = 456) | High-Quality Radiography (n = 175) | Low-Quality Radiography (n = 281) | |
| TP | 270 | 103 | 167 | 280 | 100 | 180 |
| FN | 1 | 0 | 1 | 42 | 12 | 30 |
| FP | 76 | 25 | 51 | 66 | 28 | 38 |
| TN | 109 | 47 | 62 | 68 | 35 | 33 |
| Sensitivity | 99.6 (99.1–100) | 100.0 (100–100) | 99.4 (98.7–100) | 87.0 (83.9–90.0) | 89.3 (86.4–92.1) | 85.7 (82.5–88.9) |
| Specificity | 58.9 (54.4–63.4) | 65.3 (60.9–69.6) | 54.9 (50.3–59.4) | 50.7 (46.2–55.3) | 55.6 (51–60.1) | 46.5 (41.9–51.1) |
| Accuracy | 83.1 (79.7–86.6) | 85.7 (82.5–88.9) | 81.5 (77.9–85.1) | 76.3 (72.4–80.2) | 77.1 (73.3–81) | 75.8 (71.9–79.7) |
| Youden’s index | 58.5 (54.0–63.1) | 65.3 (60.9–69.6) | 54.3 (49.7–58.8) | 37.7 (33.3–42.2) | 44.8 (40.3–49.4) | 32.2 (27.9–36.5) |
| Precision | 78.0 (74.2–81.8) | 80.5 (76.8–84.1) | 76.6 (72.7–80.5) | 80.9 (77.3–84.5) | 78.1 (74.3–81.9) | 82.6 (79.1–86.1) |
| F1 Score | 87.5 (84.5–90.6) | 89.2 (86.3–92.0) | 86.5 (83.4–89.7) | 83.8 (80.5–87.2) | 83.3 (79.9–86.8) | 84.1 (80.8–87.5) |
| MCC | 67.2 (62.9–71.5) | 72.5 (68.4–76.6) | 63.8 (59.4–68.2) | 40.1 (35.6–44.6) | 48.6 (44–53.2) | 33.5 (29.2–37.9) |
| AUC | 68.9 (64.7–73.2) | 74.9 (70.9–78.9) | 67.5 (63.2–71.8) | 71.4 (67.2–75.5) | 76.3 (72.4–80.2) | 65.1 (60.8–69.5) |
| EFP/AAP 2018 | CDC/AAP 2012 | |||||
|---|---|---|---|---|---|---|
| Overall (n = 456) | High-Quality Radiography (n = 175) | Low-Quality Radiography (n = 281) | Overall (n = 456) | High-Quality Radiography (n = 175) | Low-Quality Radiography (n = 281) | |
| AUC | 76.6 (72.7–80.5) | 80.7 (77.1–84.3) | 74.2 (70.2–78.2) | 75.9 (71.9–79.8) | 77.2 (73.3–81) | 75.2 (71.2–79.2) |
| Staging Precision (95% CI) | ||||||
| No disease | 51.9 (50.7–53.1) | 65.3 (64.2–66.4) | 43.4 (42.2–44.5) | 61.8 (60.7–63) | 74.5 (73.4–75.5) | 52.4 (51.2–53.6) |
| Mild–Moderate | 58.8 (57.6–59.9) | 66.2 (65.1–67.3) | 53.3 (52.1–54.4) | 55.5 (54.3–56.7) | 57.9 (56.7–59.1) | 54.2 (53.1–55.4) |
| Severe | 64.0 (62.8–65.1) | 65.7 (64.6–66.8) | 63.2 (62–64.3) | 53.9 (52.7–55.1) | 46.2 (45–47.3) | 59.2 (58.1–60.4) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Machado, V.; Proença, L.; Morgado, M.; Mendes, J.J.; Botelho, J. Accuracy of Panoramic Radiograph for Diagnosing Periodontitis Comparing to Clinical Examination. J. Clin. Med. 2020, 9, 2313. https://doi.org/10.3390/jcm9072313
Machado V, Proença L, Morgado M, Mendes JJ, Botelho J. Accuracy of Panoramic Radiograph for Diagnosing Periodontitis Comparing to Clinical Examination. Journal of Clinical Medicine. 2020; 9(7):2313. https://doi.org/10.3390/jcm9072313
Chicago/Turabian StyleMachado, Vanessa, Luís Proença, Mariana Morgado, José João Mendes, and João Botelho. 2020. "Accuracy of Panoramic Radiograph for Diagnosing Periodontitis Comparing to Clinical Examination" Journal of Clinical Medicine 9, no. 7: 2313. https://doi.org/10.3390/jcm9072313
APA StyleMachado, V., Proença, L., Morgado, M., Mendes, J. J., & Botelho, J. (2020). Accuracy of Panoramic Radiograph for Diagnosing Periodontitis Comparing to Clinical Examination. Journal of Clinical Medicine, 9(7), 2313. https://doi.org/10.3390/jcm9072313









