Usefulness of Machine Learning-Based Gut Microbiome Analysis for Identifying Patients with Irritable Bowels Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Fecal Sampling, DNA Extraction, and Sequencing
2.3. Taxonomy Assignment Based on the 16S rRNA Gene Sequence
2.4. Analysis of Bacterial Diversity
2.5. Measurement of Fecal Short-Chain Fatty Acids
2.6. Group Differences in Taxonomic Abundance
2.7. Prediction Model for IBS and Statistical Analyses of IBS Biomarkers
2.8. Statistical Analyses of the Fecal Microbiome to Determine the Featured Taxa in IBS Patients
3. Results
3.1. Patient Characteristics and Clinical Status
3.2. Biodiversity of IBS Subgroups and Healthy Controls
3.3. Short-Chain Fatty Acids in Feces Samples from IBS Patients
3.4. Distance of Microbial Composition between IBS and Healthy Controls
3.5. Comparisons of Relative Abundance of Each Taxon between Healthy Controls and IBS Patients
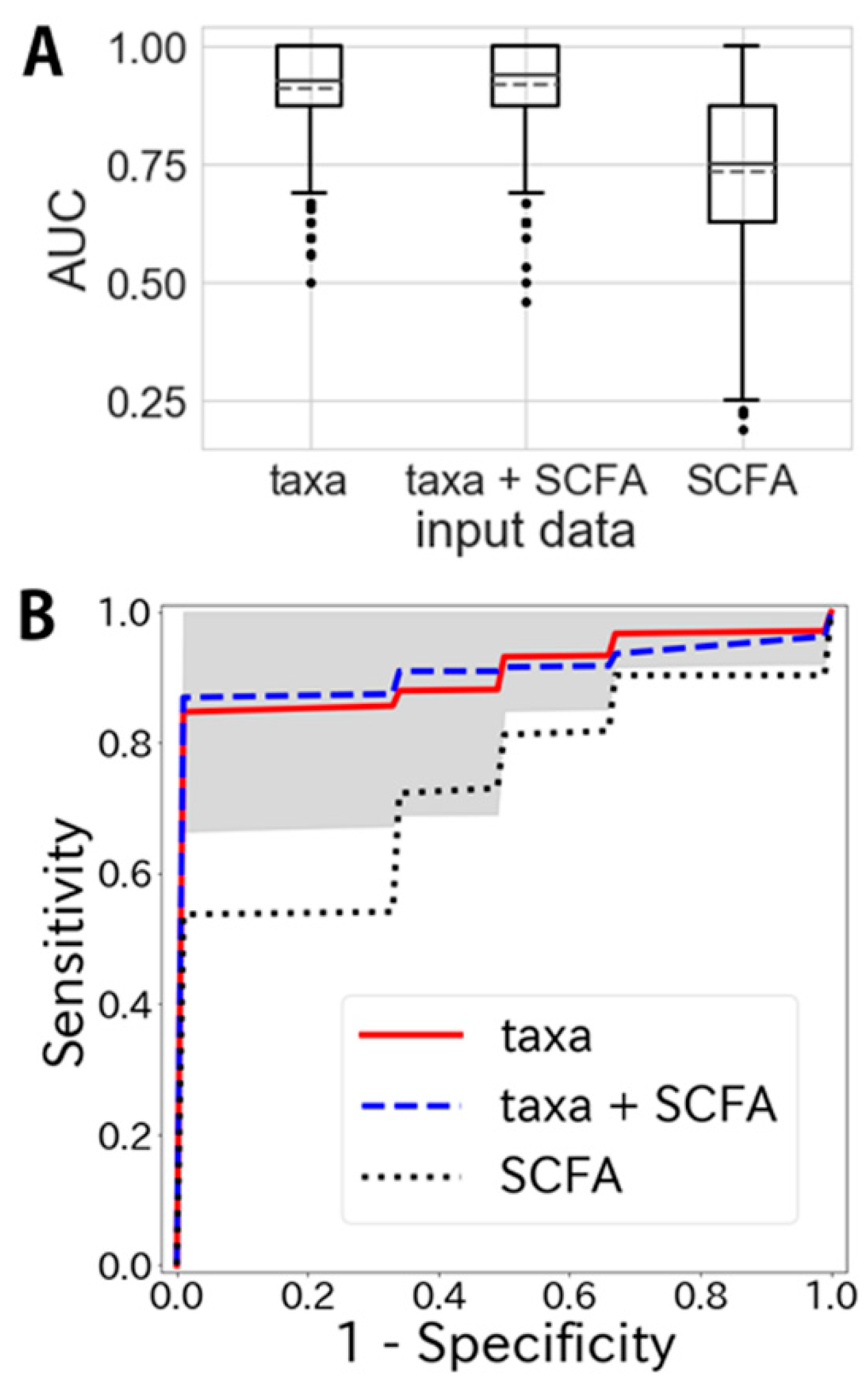
3.6. Classification of IBS and Healthy Controls by Machine Learning with Featured Taxa and Short-Chain Fatty Acids
3.7. Comparison of Japanese IBS Featured Taxa with Swedish IBS
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Longstreth, G.F.; Thompson, W.G.; Chey, W.D.; Houghton, L.A.; Mearin, F.; Spiller, R.C. Functional bowel disorders. Gastroenterology 2006, 130, 480–1491. [Google Scholar] [CrossRef] [PubMed]
- Enck, P.; Aziz, Q.; Barbara, G.; Farmer, A.D.; Fukudo, S.; Mayer, E.A.; Niesler, B.; Quigley, E.M.; Rajilić-Stojanović, M.; Schemann, M.; et al. Irritable bowel syndrome. Nat. Rev. Dis. Primers 2016, 2, 16014. [Google Scholar] [CrossRef] [PubMed]
- Plavšić, I.; Hauser, G.; Tkalčić, M.; Pletikosić, S.; Salkić, N. Diagnosis of irritable bowel syndrome: Role of potential biomarkers. Gastroenterol. Res. Pract. 2015, 2015, 490183. [Google Scholar] [CrossRef] [PubMed]
- Mearin, F.; Lacy, B.E.; Chang, L.; Chey, W.D.; Lembo, A.J.; Simren, M.; Spiller, R. Bowel disorders. Gastroenterology 2016, 150, 1393–1407. [Google Scholar]
- Ford, A.C.; Bercik, P.; Morgan, D.G.; Bolino, C.; Pintos-Sanchez, M.I.; Moayyedi, P. Validation of the Rome III criteria for the diagnosis of irritable bowel syndrome in secondary care. Gastroenterology 2013, 145, 1262–1270. [Google Scholar] [CrossRef]
- Sood, R.; Law, G.R.; Ford, A.C. Diagnosis of IBS: Symptoms, symptom-based criteria, biomarkers or ‘psychomarkers’? Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 683–691. [Google Scholar] [CrossRef]
- Canavan, C.; Card, T.; West, J. The incidence of other gastroenterological disease following diagnosis of irritable bowel syndrome in the UK: A cohort study. PLoS ONE 2014, 9, e106478. [Google Scholar] [CrossRef]
- Pimentel, M.; Purdy, C.; Magar, R.; Rezaie, A. A predictive model to estimate cost savings of a novel diagnostic blood panel for diagnosis of diarrhea-predominant irritable bowel syndrome. Clin. Ther. 2016, 38, 1638–1652. [Google Scholar] [CrossRef]
- Fukui, H.; Xu, X.; Miwa, H. Role of Gut microbiota-gut hormone axis in the pathophysiology of functional gastrointestinal disorders. J. Neurogastroenterol. Motil. 2018, 24, 367–386. [Google Scholar] [CrossRef]
- Simrén, M.; Barbara, G.; Flint, H.J.; Spiegel, B.M.; Spiller, R.C.; Vanner, S.; Verdu, E.F.; Whorwell, P.J.; Zoetendal, E.G. Intestinal microbiota in functional bowel disorders: A Rome foundation report. Gut 2013, 62, 159–176. [Google Scholar] [CrossRef]
- Tap, J.; Derrien, M.; Törnblom, H.; Brazeilles, R.; Cools-Portier, S.; Doré, J.; Störsrud, S.; Le Nevé, B.; Öhman, L.; Simrén, M. Identification of an intestinal microbiota signature associated with severity of irritable bowel syndrome. Gastroenterology 2017, 152, 111–123. [Google Scholar] [CrossRef] [PubMed]
- Nishijima, S.; Suda, W.; Oshima, K.; Kim, S.W.; Hirose, Y.; Morita, H.; Hattori, M. The gut microbiome of healthy Japanese and its microbial and functional uniqueness. DNA Res. 2016, 23, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Heaton, K.W.; O’Donnell, L.J. An office guide to whole-gut transit time. Patients’ recollection of their stool form. J. Clin. Gastroenterol. 1994, 19, 28–30. [Google Scholar] [CrossRef] [PubMed]
- NCBI Sequence Read Archive, SRA Accession: PRINA637763. Available online: https://www.ncbi.nlm.nih.gov/bioproject/PRJNA637763/ (accessed on 27 July 2020).
- DeSantis, T.Z.; Hugenholtz, P.; Larsen, N.; Rojas, M.; Brodie, E.L.; Keller, K.; Huber, T.; Dalevi, D.; Hu, P.; Andersen, G.L. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB. Appl. Environ. Microbiol. 2006, 72, 5069–5072. [Google Scholar] [CrossRef]
- Caporaso, J.G.; Kuczynski, J.; Stombaugh, J.; Bittinger, K.; Bushman, F.D.; Costello, E.K.; Fierer, N.; Peña, A.G.; Goodrich, J.K.; Gordon, J.I.; et al. QIIME allows analysis of high-throughput community sequencing data. Nat. Methods 2010, 7, 335–336. [Google Scholar] [CrossRef]
- Edgar, R.C. Search and clustering orders of magnitude faster than BLAST. Bioinformatics 2010, 26, 2460–2461. [Google Scholar] [CrossRef]
- Cole, J.R.; Wang, Q.; Cardenas, E.; Fish, J.; Chai, B.; Farris, R.J.; Kulam-Syed-Mohideen, A.S.; McGarrell, D.M.; Marsh, T.; Garrity, G.M.; et al. The Ribosomal Database Project: Improved alignments and new tools for rRNA analysis. Nucleic Acids Res. 2009, 37, D141–D145. [Google Scholar] [CrossRef]
- R Core Team. R: Language and Environment for Statistical Computing. 2016. Available online: https://www.R-project.org/ (accessed on 27 July 2020).
- Millman, K.J.; Aivazis, M. Python for scientists and engineers. Comput. Sci. Eng. 2011, 13, 9–12. [Google Scholar] [CrossRef]
- Miyamoto, J.; Watanabe, K.; Taira, S.; Kasubuchi, M.; Li, X.; Irie, J.; Itoh, H.; Kimura, I. Barley β-glucan improves metabolic condition via short-chain fatty acids produced by gut microbial fermentation in high fat diet fed mice. PLoS ONE 2018, 13, e0196579. [Google Scholar] [CrossRef]
- Tibshirani, R. Regression shrinkage and selection via the lasso: A retrospective. J. R. Stat. Soc. Ser. B Stat. Methodol. 2011, 73, 273–282. [Google Scholar] [CrossRef]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, B.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-learn: Machine Learning in Python. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- The Source Code for the IBS Prediction Model is Available from GitHub. Available online: https://github.com/Cykinso/paper_supplements-ibs-classifier (accessed on 27 July 2020).
- Altschul, S.F.; Gish, W.; Miller, W.; Myers, E.W.; Lipman, D.J. Basic local alignment search tool. J. Mol. Biol. 1990, 215, 403–410. [Google Scholar] [CrossRef]
- Ley, R.E.; Turnbaugh, P.J.; Klein, S.; Gordon, J.I. Microbial ecology: Human gut microbes associated with obesity. Nature 2006, 444, 1022–1023. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.; Li, R.; Raes, J.; Arumugam, M.; Burgdorf, K.S.; Manichanh, C.; Nielsen, T.; Pons, N.; Levenez, F.; Yamada, T.; et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 2010, 464, 59–65. [Google Scholar] [CrossRef]
- Labus, J.S.; Hollister, E.B.; Jacobs, J.; Kirbach, K.; Oezguen, N.; Gupta, A.; Acosta, J.; Luna, R.A.; Aagaard, K.; Versalovic, J.; et al. Differences in gut microbial composition correlate with regional brain volumes in irritable bowel syndrome. Microbiome 2017, 5, 49. [Google Scholar] [CrossRef]
- Chong, P.P.; Chin, V.K.; Looi, C.Y.; Wong, W.F.; Madhavan, P.; Yong, V.C. The microbiome and irritable bowel syndrome—A review on the pathophysiology, current research and future therapy. Front. Microbiol. 2019, 10, 1136. [Google Scholar] [CrossRef]
- Li, J.; Jia, H.; Cai, X.; Zhong, H.; Feng, Q.; Sunagawa, S.; Arumugam, M.; Kultima, J.R.; Prifti, E.; Nielsen, T.; et al. An integrated catalog of reference genes in the human gut microbiome. Nat. Biotechnol. 2014, 32, 834–841. [Google Scholar] [CrossRef]
- Crouzet, L.; Gaultier, E.; Del’Homme, C.; Cartier, C.; Delmas, E.; Dapoigny, M.; Fioramonti, J.; Bernalier-Donadille, A. The hypersensitivity to colonic distension of IBS patients can be transferred to rats through their fecal microbiota. Neurogastroenterol. Motil. 2013, 25, e272–e282. [Google Scholar] [CrossRef]
- De Palma, G.; Lynch, M.D.; Lu, J.; Dang, V.T.; Deng, Y.; Jury, J.; Umeh, G.; Miranda, P.M.; Pigrau Pastor, M.; Sidani, S.; et al. Transplantation of fecal microbiota from patients with irritable bowel syndrome alters gut function and behavior in recipient mice. Sci. Transl. Med. 2017, 9, eaaf6397. [Google Scholar] [CrossRef]
- Halkjær, S.I.; Christensen, A.H.; Lo, B.Z.S.; Browne, P.D.; Günther, S.; Hansen, L.H.; Petersen, A.M. Faecal microbiota transplantation alters gut microbiota in patients with irritable bowel syndrome: Results from a randomised, double-blind placebo-controlled study. Gut 2018, 67, 2107–2115. [Google Scholar] [CrossRef] [PubMed]
- El-Salhy, M.; Hatlebakk, J.G.; Hausken, T. Diet in irritable bowel syndrome (IBS): Interaction with gut microbiota and gut hormones. Nutrients 2019, 11, 1824. [Google Scholar] [CrossRef] [PubMed]
- Hills, R.D., Jr.; Pontefract, B.A.; Mishcon, H.R.; Black, C.A.; Sutton, S.C.; Theberge, C.R. Gut microbiome: Profound implications for diet and disease. Nutrients 2019, 11, 1613. [Google Scholar] [CrossRef] [PubMed]
- Faith, J.J.; McNulty, N.P.; Rey, F.E.; Gordon, J.I. Predicting a human gut microbiota’s response to diet in gnotobiotic mice. Science 2011, 333, 101–104. [Google Scholar] [CrossRef]
- Collins, S.M. A role for gut microbiota in IBS. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 497–505. [Google Scholar] [CrossRef]
- Staudacher, H.M.; Whelan, K. The low FODMAP diet: Recent advances in understanding its mechanisms and efficacy in IBS. Gut 2017, 66, 1517–1527. [Google Scholar] [CrossRef]
- Levy, M.; Blacher, E.; Elinav, E. Microbiome, metabolites and host immunity. Curr. Opin. Microbiol. 2017, 35, 8–15. [Google Scholar] [CrossRef]
- Priyadarshini, M.; Kotlo, K.U.; Dudeja, P.K.; Layden, B.T. Role of short chain fatty acid receptors in intestinal physiology and pathophysiology. Compr. Physiol. 2018, 8, 1091–1115. [Google Scholar]
- Tana, C.; Umesaki, Y.; Imaoka, A.; Handa, T.; Kanazawa, M.; Fukudo, S. Altered profiles of intestinal microbiota and organic acids may be the origin of symptoms in irritable bowel syndrome. Neurogastroenterol. Motil. 2010, 22, 512. [Google Scholar] [CrossRef]
- Pozuelo, M.; Panda, S.; Santiago, A.; Mendez, S.; Accarino, A.; Santos, J.; Guarner, F.; Azpiroz, F.; Manichanh, C. Reduction of butyrate- and methane-producing microorganisms in patients with irritable bowel syndrome. Sci. Rep. 2015, 5, 12693. [Google Scholar] [CrossRef]
- Farup, P.G.; Rudi, K.; Hestad, K. Faecal short-chain fatty acids—A diagnostic biomarker for irritable bowel syndrome? BMC Gastroenterol. 2016, 16, 51. [Google Scholar] [CrossRef] [PubMed]
- Staudacher, H.M.; Lomer, M.C.; Anderson, J.L.; Barrett, J.S.; Muir, J.G.; Irving, P.M.; Whelan, K. Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J. Nutr. 2012, 142, 1510–1518. [Google Scholar] [CrossRef]
- Halmos, E.P.; Christophersen, C.T.; Bird, A.R.; Shepherd, S.J.; Gibson, P.R.; Muir, J.G. Diets that differ in their FODMAP content alter the colonic luminal microenvironment. Gut 2015, 64, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Hustoft, T.N.; Hausken, T.; Ystad, S.O.; Valeur, J.; Brokstad, K.; Hatlebakk, J.G.; Lied, G.A. Effects of varying dietary content of fermentable short-chain carbohydrates on symptoms, fecal microenvironment, and cytokine profiles in patients with irritable bowel syndrome. Neurogastroenterol. Motil. 2017, 29, e12969. [Google Scholar] [CrossRef] [PubMed]
- Sood, R.; Gracie, D.J.; Law, G.R.; Ford, A.C. Systematic review with meta-analysis: The accuracy of diagnosing irritable bowel syndrome with symptoms, biomarkers and/or psychological markers. Aliment. Pharmacol. Ther. 2015, 42, 491–503. [Google Scholar] [CrossRef] [PubMed]
- Mujagic, Z.; Tigchelaar, E.F.; Zhernakova, A.; Ludwig, T.; Ramiro-Garcia, J.; Baranska, A.; Swertz, M.A.; Masclee, A.A.; Wijmenga, C.; van Schooten, F.J.; et al. A novel biomarker panel for irritable bowel syndrome and the application in the general population. Sci. Rep. 2016, 6, 26420. [Google Scholar] [CrossRef]
- Camilleri, M.; Halawi, H.; Oduyebo, I. Biomarkers as a diagnostic tool for irritable bowel syndrome: Where are we? Expert Rev. Gastroenterol. Hepatol. 2017, 11, 303–316. [Google Scholar] [CrossRef]



| Factors | Healthy (n = 26) | IBS (n = 85) | P (t) | IBS-C (n = 27) | P (t) | IBS-D (n = 33) | P (t) | IBS-M (n = 22) | P (t) | IBS-U (n = 3) |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 46.2 ± 10.6 | 51.3 ± 15.3 | 0.058 (1.93) | 56.3 ± 15.2 | 0.007 (2.82) | 49.7 ± 14.0 | 0.274 (1.10) | 46.8 ± 16.7 | 0.873 (0.16) | 56.7 ± 5.8 |
| Sex (M/F) | 9/17 | 37/48 | 0.562 | 8/19 | 0.925 | 17/16 | 0.301 | 11/11 | 0.433 | 1/2 |
| BMI | 22.2 ± 3.6 | 22.2 ± 4.2 (4 NA) | 0.987 (0.02) | 20.9 ± 3.5 (4 NA) | 0.182 (1.35) | 21.9 ± 3.2 | 0.742 (0.33) | 24.6 ± 5.3 | 0.079 (1.81) | 18.1 ± 1.1 |
| IBS-symptom frequency (1/2/3) | NA | 34/17/33 (1 NA) | NA | 13/3/11 | NA | 12/7/13 (1 NA) | NA | 9/7/6 | NA | 0/0/3 |
| Stool frequency (stool per day) | 1.48 ± 0.56 | 1.40 ± 0.91 (4 NA) | 0.614 (0.51) | 0.88 ± 0.72 (1 NA) | 0.003 (3.19) | 2.03 ± 0.82 (2 NA) | 0.005 (2.92) | 1.15 ± 0.80 (1 NA) | 0.124 (1.58) | 1.23 ± 0.46 |
| Stool consistency (Bristol Stool Form) | 4.15 ± 0.46 | 4.41 ± 1.61 (6 NA) | 0.223 (1.23) | 3.67 ± 1.88 (3 NA) | 0.259 (1.16) | 5.31 ± 0.71 (1 NA) | <0.001 (7.20) | 3.95 ± 1.82 (2 NA) | 0.630 (0.489) | 4.00 ± 0.00 |
| Factors | Healthy (n = 26) | IBS (n = 81) † | P (t) | IBS-C (n = 25) † | P (t) | IBS-D (n = 33) | P (t) | IBS-M (n = 20) † | P (t) | IBS-U (n = 3) |
|---|---|---|---|---|---|---|---|---|---|---|
| acetic acid | 42.0 ± 8.7 | 36.9 ± 12.9 | 0.025 (2.30) | 37.5 ± 11.2 | 0.114 (1.60) | 34.5 ± 13.0 | 0.011 (2.64) | 40.0 ± 14.2 | 0.516 (0.66) | 39.8 ± 17.5 |
| propionic acid | 8.3 ± 4.4 | 11.6 ± 6.4 | 0.004 (2.96) | 11.0 ± 6.6 | 0.096 (1.70) | 10.8 ± 6.7 | 0.095 (1.70) | 12.9 ± 5.5 | 0.004 (3.07) | 17.1 ± 4.0 |
| butyric acid | 7.0 ± 3.4 | 6.5 ± 3.2 | 0.574 (0.57) | 6.6 ± 3.1 | 0.668 (0.43) | 5.6 ± 2.8 | 0.109 (1.63) | 7.9 ± 3.9 | 0.402 (0.85) | 7.3 ± 1.5 |
| valerate | 1.0 ± 0.9 | 1.1 ± 1.0 | 0.593 (0.54) | 0.9 ± 0.8 | 0.797 (0.26) | 1.1 ± 1.2 | 0.628 (0.49) | 1.1 ± 0.9 | 0.726 (0.35) | 2.4 ± 0.7 |
| iso-butyric acid | 0.7 ± 0.6 | 0.8 ± 0.5 | 0.302 (1.05) | 0.9 ± 0.5 | 0.123 (1.57) | 0.7 ± 0.5 | 0.970 (0.04) | 0.8 ± 0.4 | 0.300 (1.05) | 1.1 ± 0.8 |
| iso-valerate | 0.7 ± 0.5 | 0.7 ± 0.5 | 0.821 (0.23) | 0.8 ± 0.6 | 0.456 (0.75) | 0.6 ± 0.5 | 0.639 (0.47) | 0.7 ± 0.4 | 0.873 (0.16) | 0.9 ± 0.8 |
| butyric acid- valerate | 1.4 ± 2.6 | 5.1 ± 5.8 | <0.001 (4.52) | 4.4 ± 6.9 | 0.044 (2.10) | 5.2 ± 5.7 | 0.001 (3.43) | 5.0 ± 4.8 | 0.004 (3.10) | 9.9 ± 4.3 |
| Taxon genus level | Healthy Group (n = 26) | IBS Group (n = 85) | P (t) | IBS-C (n = 27) | P (t) | IBS-D (n = 33) | P (t) | IBS-M (n = 22) | P (t) | IBS-U (n = 3) |
|---|---|---|---|---|---|---|---|---|---|---|
| f_Halomonadaceae; g_Halomonas | 0.00 ± 0.00 | 0.12 ± 0.18 | <0.001 (15.38) | 0.07 ± 0.10 | <0.001 (5.53) | 0.18 ± 0.24 | <0.001 (12.86) | 0.12 ± 0.13 | <0.001 (9.33) | 0.04 ± 0.04 |
| f_Lachnospiraceae; g_Anaerostipes | 0.41 ± 0.39 | 0.23 ± 0.45 | <0.001 (5.67) | 0.42 ± 0.70 | 0.008 (2.82) | 0.08 ± 0.12 | <0.001 (5.94) | 0.21 ± 0.28 | 0.005 (3.07) | 0.24 ± 0.17 |
| f_Ruminococcaceae; g_Ruminococcus | 4.41 ± 3.26 | 2.64 ± 2.93 | <0.001 (3.99) | 3.37 ± 2.99 | 0.120 (1.59) | 1.72 ± 2.56 | <0.001 (4.54) | 2.94 ± 2.89 | 0.045 (2.08) | 4.00 ± 5.05 |
| f_Enterobacteriaceae; Other | 0.02 ± 0.04 | 0.16 ± 0.57 | 0.001 (2.61) | 0.12 ± 0.32 | 0.206 (1.28) | 0.13 ± 0.18 | 0.002 (3.32) | 0.28 ± 1.04 | 0.223 (1.23) | 0.06 ± 0.07 |
| f_Coriobacteriaceae; g_Collinsella | 1.76 ± 1.36 | 1.23 ± 1.59 | 0.05 (2.95) | 1.16 ± 1.50 | 0.022 (2.37) | 1.01 ± 1.45 | 0.004 (3.00) | 1.67 ± 1.95 | 0.304 (1.04) | 0.98 ± 0.95 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukui, H.; Nishida, A.; Matsuda, S.; Kira, F.; Watanabe, S.; Kuriyama, M.; Kawakami, K.; Aikawa, Y.; Oda, N.; Arai, K.; et al. Usefulness of Machine Learning-Based Gut Microbiome Analysis for Identifying Patients with Irritable Bowels Syndrome. J. Clin. Med. 2020, 9, 2403. https://doi.org/10.3390/jcm9082403
Fukui H, Nishida A, Matsuda S, Kira F, Watanabe S, Kuriyama M, Kawakami K, Aikawa Y, Oda N, Arai K, et al. Usefulness of Machine Learning-Based Gut Microbiome Analysis for Identifying Patients with Irritable Bowels Syndrome. Journal of Clinical Medicine. 2020; 9(8):2403. https://doi.org/10.3390/jcm9082403
Chicago/Turabian StyleFukui, Hirokazu, Akifumi Nishida, Satoshi Matsuda, Fumitaka Kira, Satoshi Watanabe, Minoru Kuriyama, Kazuhiko Kawakami, Yoshiko Aikawa, Noritaka Oda, Kenichiro Arai, and et al. 2020. "Usefulness of Machine Learning-Based Gut Microbiome Analysis for Identifying Patients with Irritable Bowels Syndrome" Journal of Clinical Medicine 9, no. 8: 2403. https://doi.org/10.3390/jcm9082403
APA StyleFukui, H., Nishida, A., Matsuda, S., Kira, F., Watanabe, S., Kuriyama, M., Kawakami, K., Aikawa, Y., Oda, N., Arai, K., Matsunaga, A., Nonaka, M., Nakai, K., Shinmura, W., Matsumoto, M., Morishita, S., Takeda, A. K., & Miwa, H. (2020). Usefulness of Machine Learning-Based Gut Microbiome Analysis for Identifying Patients with Irritable Bowels Syndrome. Journal of Clinical Medicine, 9(8), 2403. https://doi.org/10.3390/jcm9082403






