Metabolic Footprint, towards Understanding Type 2 Diabetes beyond Glycemia
Abstract
:1. Introduction
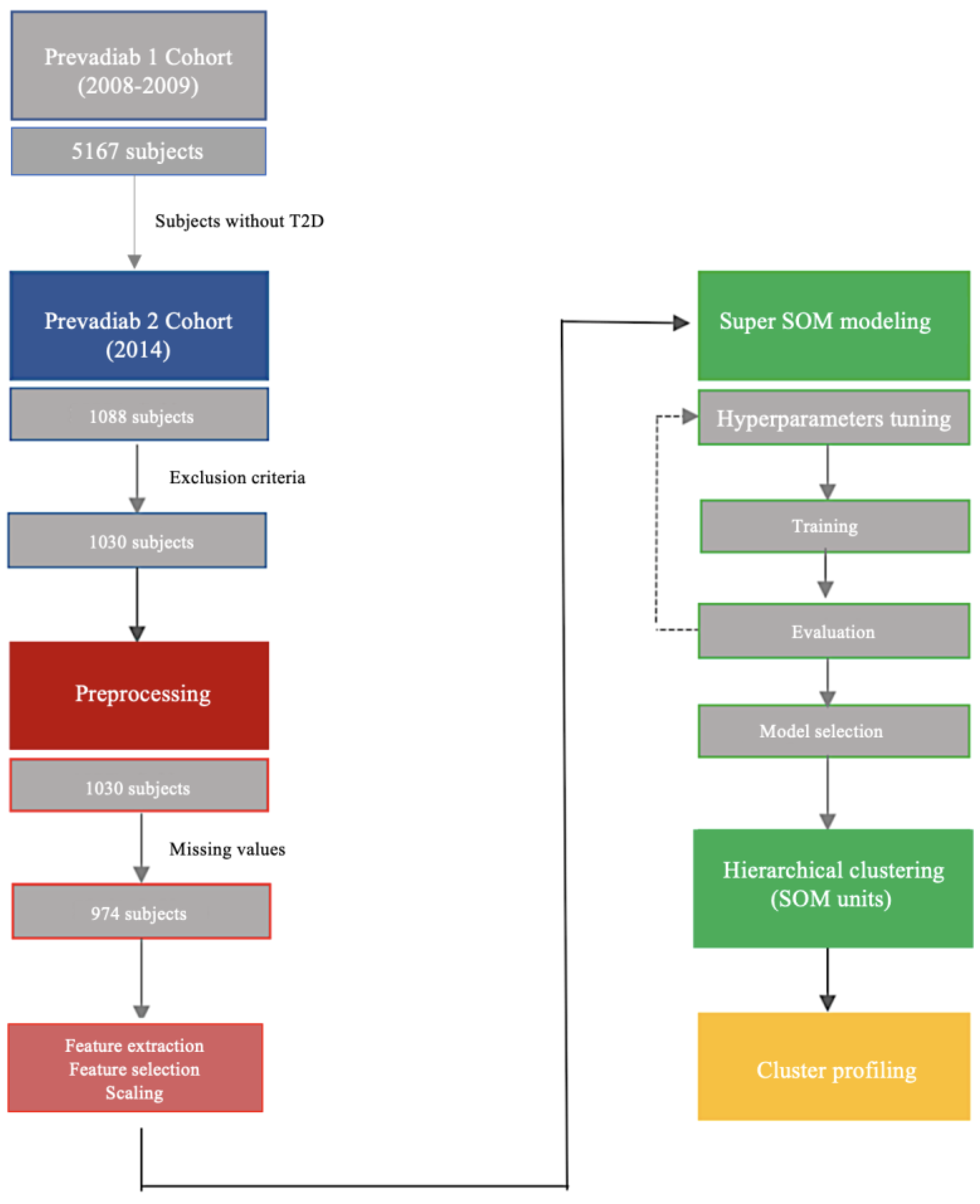
2. Experimental Section
2.1. Ethics Statement
2.2. Subjects
2.3. Clinical Measurements
2.4. Metabolic And Functional Indexes
2.5. Statistical Analysis
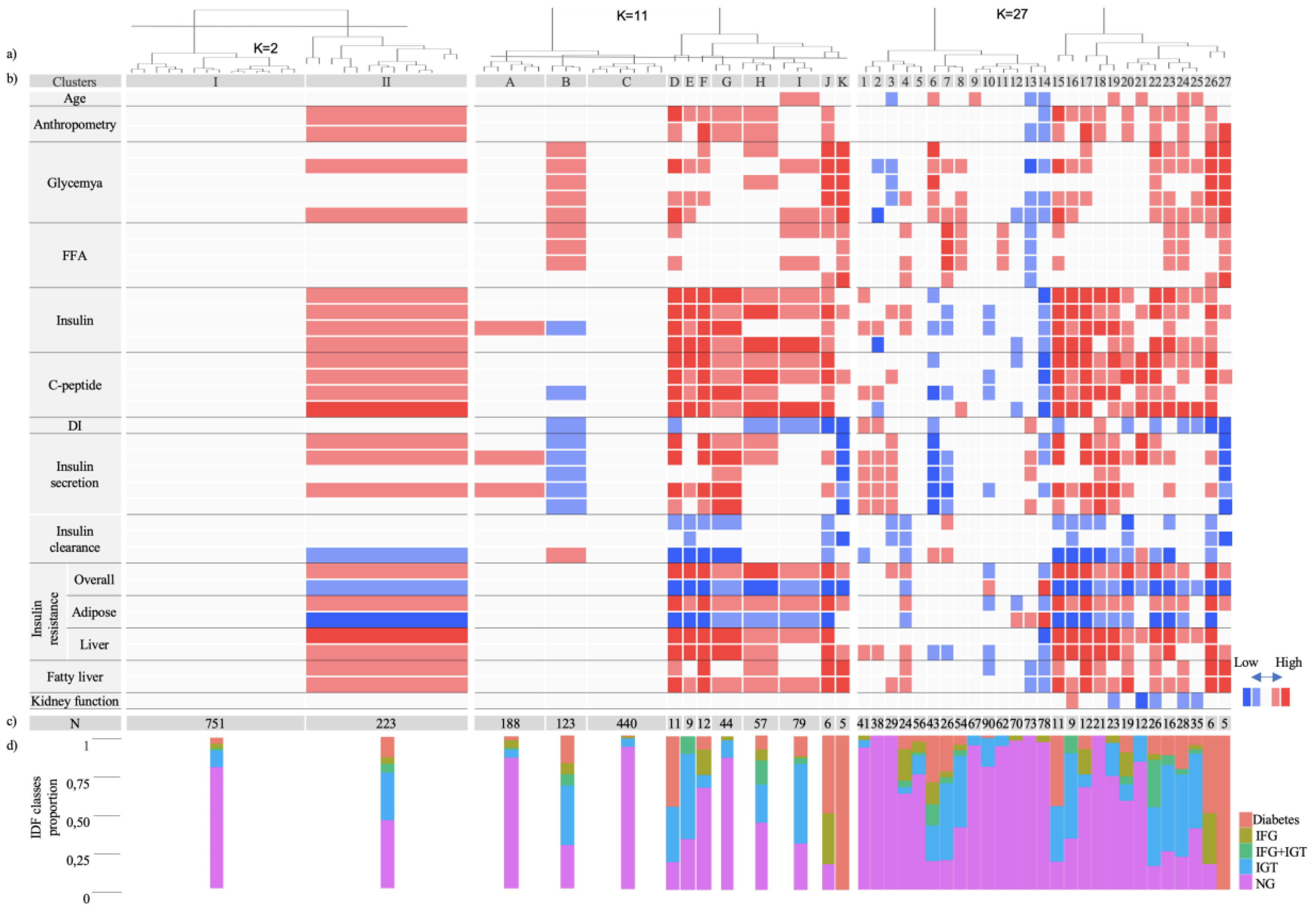
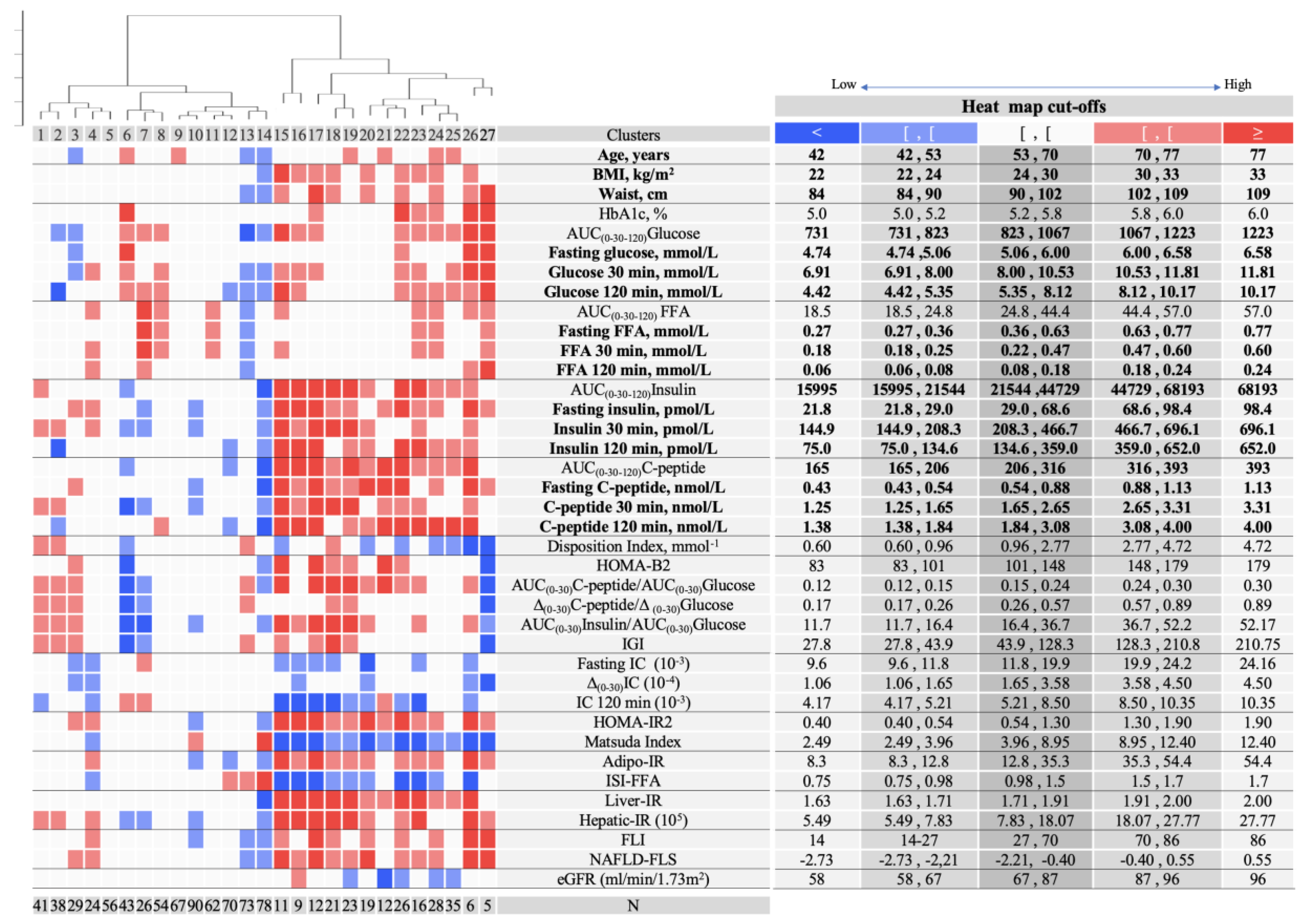
2.6. Cluster Analysis
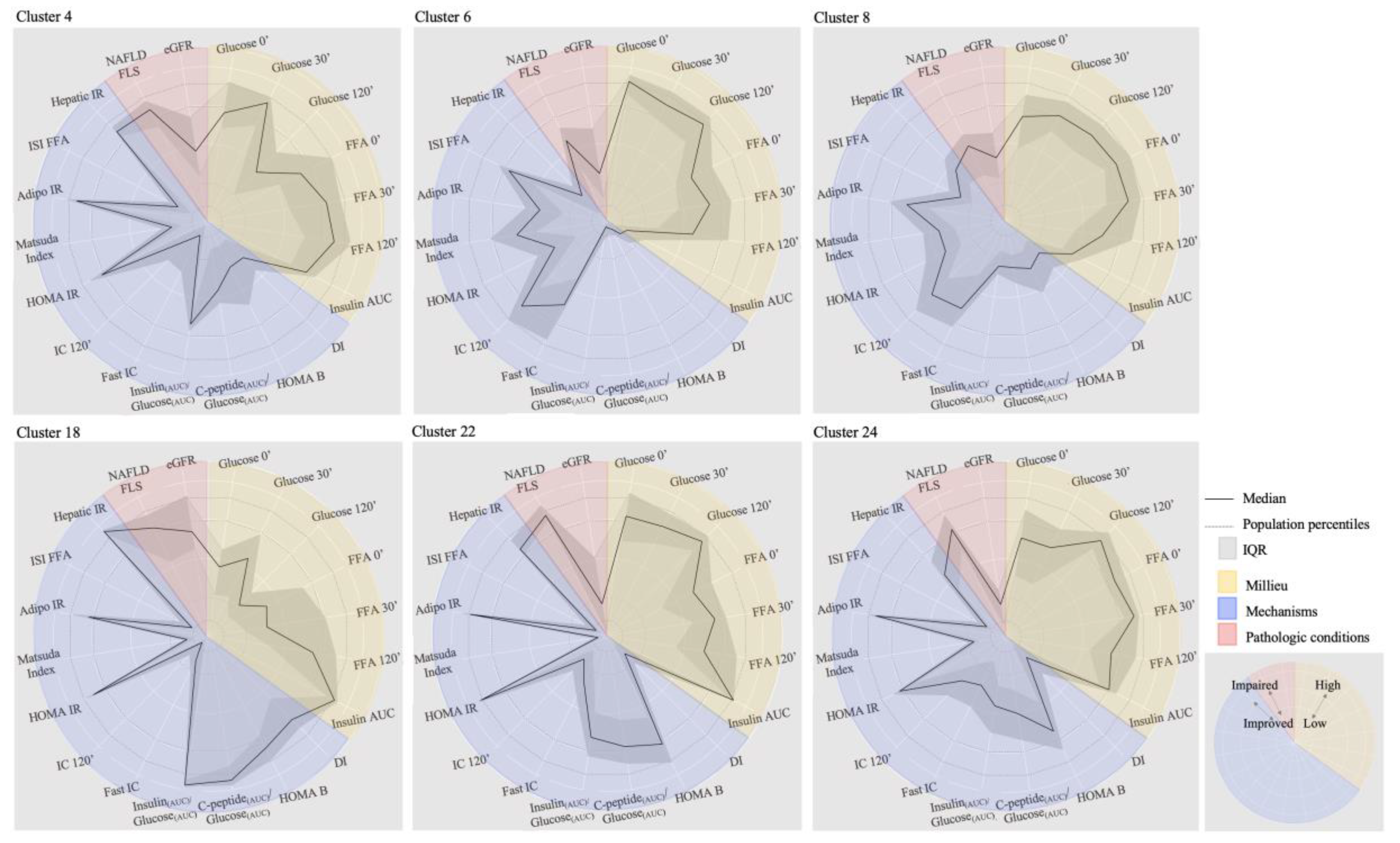
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tuomi, T.; Santoro, N.; Caprio, S.; Cai, M.; Weng, J.; Groop, L. The many faces of diabetes: A disease with increasing heterogeneity. Lancet 2014, 383, 1084–1094. [Google Scholar] [CrossRef]
- Zhang, P.; Zhang, X.; Brown, J.; Vistisen, D.; Sicree, R.; Shaw, J.; Nichols, G. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 2010, 87, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Bommer, C.; Sagalova, V.; Heesemann, E.; Manne-Goehler, J.; Atun, R.; Bärnighausen, T.; Davies, J.; Vollmer, S. Global economic burden of diabetes in adults: Projections from 2015 to 2030. Diabetes Care 2018, 41, 963–970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, Y.; Ley, S.H.; Hu, F.B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 2018, 14, 88–98. [Google Scholar] [CrossRef]
- Pina, A.; Macedo, M.P.; Henriques, R. Clustering clinical data in R. In Mass Spectrometry Data Analysis in Proteomics; Matthiesen, R., Ed.; Springer: New York, NY, USA, 2020; pp. 309–343. ISBN 978-1-4939-9744-2. [Google Scholar]
- Ahlqvist, E.; Storm, P.; Käräjämäki, A.; Martinell, M.; Dorkhan, M.; Carlsson, A.; Vikman, P.; Prasad, R.B.; Aly, D.M.; Almgren, P.; et al. Novel subgroups of adult-onset diabetes and their association with outcomes: A data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 2018, 6, 361–369. [Google Scholar] [CrossRef] [Green Version]
- Dennis, J.M.; Shields, B.M.; Henley, W.E.; Jones, A.G.; Hattersley, A.T. Disease progression and treatment response in data-driven subgroups of type 2 diabetes compared with models based on simple clinical features: An analysis using clinical trial data. Lancet Diabetes Endocrinol. 2019, 8587, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Zou, X.; Zhou, X.; Zhu, Z.; Ji, L. Novel subgroups of patients with adult-onset diabetes in Chinese and US populations. Lancet Diabetes Endocrinol. 2019, 7, 9–11. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Diabetes Mellitus: Report of a WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1965; Volume 310. [Google Scholar]
- DeFronzo, R.A. From the triumvirate to the ominous octet: A new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009, 58, 773–795. [Google Scholar] [CrossRef] [Green Version]
- McCarthy, M.I. Painting a new picture of personalised medicine for diabetes. Diabetologia 2017, 60, 793–799. [Google Scholar] [CrossRef] [Green Version]
- Tabák, A.G.; Herder, C.; Kivimäki, M. Prediabetes: A high-risk state for developing diabetes Progression from prediabetes to diabetes Reversion to normoglycaemia Risk prediction. Lancet 2014, 379, 2279–2290. [Google Scholar] [CrossRef] [Green Version]
- Gardete-Correia, L.; Boavida, J.M.; Raposo, J.F.; Mesquita, A.C.; Fona, C.; Carvalho, R.; Massano-Cardoso, S. Original Article: Epidemiology First diabetes prevalence study in Portugal: PREVADIAB study. Diabet. Med. 2010, 27, 879–881. [Google Scholar] [CrossRef]
- WHO; IDF. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia; WHO Press: Geneva, Switzerland, 2006. [Google Scholar]
- International Diabetes Federation. IDF Clinical Practice Recommendations for managing Type 2 Diabetes in Primary Care; International Diabetes Federation: Brussels, Belgium, 2017; ISBN 9782930229850. [Google Scholar]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic syndrome—A new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Levy, J.; Matthews, D.; Hermans, M. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care 1998, 21, 2191–2192. [Google Scholar] [CrossRef] [PubMed]
- Herzberg-Schäfer, S.A.; Staiger, H.; Heni, M.; Ketterer, C.; Guthoff, M.; Kantartzis, K.; Machicao, F.; Stefan, N.; Häring, H.U.; Fritsche, A. Evaluation of fasting state-/oral glucose tolerance test-derived measures of insulin release for the detection of genetically impaired β-cell function. PLoS ONE 2010, 5, e14194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsuda, M.; DeFronzo, R.A. Insulin sensitivity indices obtained from oral glucose tolerance testing: Comparison with the euglycemic insulin clamp. Diabetes Care 1999, 22, 1462–1470. [Google Scholar] [CrossRef]
- Vangipurapu, J.; Stančáková, A.; Kuulasmaa, T.; Paananen, J.; Kuusisto, J.; Ferrannini, E.; Laakso, M. A novel surrogate index for hepatic insulin resistance. Diabetologia 2011, 54, 540–543. [Google Scholar] [CrossRef] [Green Version]
- Abdul-Ghani, M.A.; Matsuda, M.; Balas, B.; DeFronzo, R.A. Muscle and liver insulin resistance indexes derived from the oral glucose tolerance test. Diabetes Care 2007, 30, 89–94. [Google Scholar] [CrossRef] [Green Version]
- Gastaldelli, A.; Harrison, S.A.; Belfort-Aguilar, R.; Hardies, L.J.; Balas, B.; Schenker, S.; Cusi, K. Importance of changes in adipose tissue insulin resistance to histological response during thiazolidinedione treatment of patients with nonalcoholic steatohepatitis. Hepatology 2009, 50, 1087–1093. [Google Scholar] [CrossRef]
- Belfiore, F.; Iannello, S.; Volpicelli, G. Insulin sensitivity indices calculated from basal and OGTT-induced insulin, glucose, and FFA levels. Mol. Genet. Metab. 1998, 63, 134–141. [Google Scholar] [CrossRef]
- Kahl, S.; Straßburger, K.; Nowotny, B.; Livingstone, R.; Klüppelholz, B.; Keßel, K.; Hwang, J.H.; Giani, G.; Hoffmann, B.; Pacini, G.; et al. Comparison of liver fat indices for the diagnosis of hepatic steatosis and insulin resistance. PLoS ONE 2014, 9, e94059. [Google Scholar] [CrossRef] [Green Version]
- Balkau, B.; Lange, C.; Vol, S.; Fumeron, F.; Bonnet, F. Nine-year incident diabetes is predicted by fatty liver indices: The French D.E.S.I.R. study. BMC Gastroenterol. 2010, 10, 56. [Google Scholar] [CrossRef] [PubMed]
- Bedogni, G.; Bellentani, S.; Miglioli, L.; Masutti, F.; Passalacqua, M.; Castiglione, A.; Tiribelli, C. The fatty liver index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006, 6, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Iii, A.F.C.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T. Article annals of internal medicine a new equation to estimate glomerular filtration rate. S. Afr. J. Sci. 2012, 604–612. [Google Scholar]
- Vesanto, J.; Alhoniemi, E. Clustering of the self-organizing map. IEEE Trans. Neural Netw. 2000, 11, 586–600. [Google Scholar] [CrossRef] [PubMed]
- Toppila, I. Identifying Novel Phenotype Profiles of Diabetic Complications and Their Genetic Components Using Machine Learning Approaches. Master’s Thesis, Aalto University, Aalto, Finland, 2016. [Google Scholar]
- Wehrens, R.; Kruisselbrink, J. Flexible self-organizing maps in kohonen 3.0. J. Stat. Softw. 2018, 87, 2768. [Google Scholar] [CrossRef] [Green Version]
- R Core Team R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018; Available online: https://www.R-project.org/ (accessed on 8 August 2020).
- Kassambara, A.; Mundt, F. Factoextra: Extract and Visualize the Results of Multivariate Data Analyses. R Package Version 1.0.5. 2017. Available online: https://CRAN.R-project.org/package=factoextra (accessed on 8 August 2020).
- Hennig, C. Cluster-wise assessment of cluster stability. Comput. Stat. Data Anal. 2007, 52, 258–271. [Google Scholar] [CrossRef] [Green Version]
- Ormazabal, V.; Nair, S.; Elfeky, O.; Aguayo, C.; Salomon, C.; Zuñiga, F.A. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc. Diabetol. 2018, 17, 1–14. [Google Scholar] [CrossRef]
- Bonora, E.; Formentini, G.; Calcaterra, F.; Lombardi, S.; Marini, F.; Zenari, L.; Saggiani, F.; Poli, M.; Perbellini, S.; Raffaelli, A.; et al. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects: Prospective data from the Verona Diabetes Complications Study. Diabetes Care 2002, 25, 1135–1141. [Google Scholar] [CrossRef] [Green Version]
- Kumar, R.; Nandhini, L.; Sadishkumar, K.; Sahoo, J.; Vivekanadan, M. Evidence for current diagnostic criteria of diabetes mellitus. World J. Diabetes 2016, 7, 396–405. [Google Scholar] [CrossRef]
- Romeo, S.; Kozlitina, J.; Xing, C.; Pertsemlidis, A.; Cox4, D.; Pennacchio, L.A.; Boerwinkle, E.; Cohen, J.C.; Hobbs, H.H. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 2008, 40, 1461–1465. [Google Scholar] [CrossRef] [Green Version]
| Population | All | Male | Female | p-Value | |||
|---|---|---|---|---|---|---|---|
| Total n (%) | 974 | 387 (40) | 587 (60) | ||||
| Normoglycemia n (%) Prediabetes n (%) Diabetes (%) | 707 (72) 211 (22) 56 (6) | 279 (72) 85 (22) 23 (6) | 428 (73) 126(21) 33 (6) | 0.08 | |||
| Parameters | Med | (p25, p75) | Med | (p25, p75) | Med | (p25, p75) | p-value |
| Age, Years | 62 | (53,70) | 62 | (53, 70) | 62 | (53, 69) | 0.93 |
| BMI, kg/m2 | 27 | (24, 30) | 26 | (25, 29) | 27 | (24, 31) | 0.020 |
| Waist, cm | 96 | (89, 102) | 98 | (92, 104) | 94 | (87, 101) | <0.0001 |
| HbA1c, %(mmol/mol) | 5.5 (37) | (5.2, 5.8) (33, 40) | 5.4 (36) | (5.2, 5.7) (33, 39) | 5.5 (37) | (5.3, 5.8) (34, 40) | <0.0001 |
| AUC(0–30–120)Glucose | 928 | (822, 1068) | 927 | (834, 1065) | 929 | (812, 1069) | 0.78 |
| Fasting Glucose, mmol/L | 5.46 | (5.03, 5.96) | 5.57 | (5.14, 6.11) | 5.40 | (4.98, 5.89) | <0.0001 |
| Glucose 30 min, mmol/L | 9.16 | (7.97, 10.54) | 9.32 | (8.11, 10.62) | 9.05 | (7.89, 10.44) | 0.023 |
| Glucose 120 min, mmol/L | 6.58 | (5.43, 8.26) | 6.26 | (5.09, 7.88) | 6.74 | (5.60, 8.37) | 0.0012 |
| AUC(0–30–120) FFA | 33 | (25, 44) | 34 | (26, 45) | 35 | (24, 44) | 0.034 |
| Fasting FFA, mmol/L | 0.48 | (0.35, 0.63) | 0.49 | (0.36, 0.63) | 0.47 | (0.35, 0.63) | 0.34 |
| FFA 30 min, mmol/L | 0.33 | (0.24, 0.47) | 0.33 | (0.24, 0.47) | 0.33 | (0.25, 0.47) | 0.55 |
| FFA 120 min, mmol/L | 0.12 | (0.07, 0.17) | 0.13 | (0.09, 0.16) | 0.11 | (0.07, 0.16) | <0.0001 |
| AUC(0–30–120)Insulin | 31,225 | (22, 136; 45, 501) | 29,401 | (19, 554; 42, 928) | 32,019 | (4653, 23,534) | 0.002 |
| Fasting insulin, pmol/L | 43.1 | (29.1, 68.8) | 42.4 | (28.3, 68.4) | 43.8 | (29.8, 68.8) | 0.35 |
| Insulin 30 min, pmol/L | 318 | (210, 468) | 300 | (194, 464) | 331 | (223, 469) | 0.029 |
| Insulin 120 min, pmol/L | 238 | (138, 379) | 210 | (112, 317) | 252 | (158, 401) | <0.0001 |
| AUC(0–30–120)C-peptide | 256 | (208, 318) | 251 | (202, 311) | 261 | (202, 322) | 0.043 |
| Fasting C-peptide, nmol/L | 0.68 | (0.54, 0.88) | 0.68 | (0.54, 0.89) | 0.67 | (0.54, 0.86) | 0.57 |
| C-peptide 30 min, nmol/L | 2.09 | (1.66, 2.65) | 2.09 | (1.64, 2.63) | 2.11 | (1.66, 2.66) | 0.57 |
| C-peptide 120 min, nmol/L | 2.59 | (1.91, 3.47) | 2.48 | (1.77, 3.38) | 2.70 | (2.03, 3.53) | 0.003 |
| Disposition Index, mmol−1 | 1.67 | (0.98, 2.83) | 1.61 | (0.90, 2.67) | 1.72 | (1.01, 2.88) | 0.14 |
| HOMA-B2 | 123 | (102, 148) | 118 | (46, 98) | 118 | (105, 150) | 0.003 |
| AUC(0–30) C-peptide/ AUC(0–30) Glucose | 0.19 | (0.15, 0.24) | 0.19 | (0.14, 0.24) | 0.20 | (0.15, 0.25) | 0.07 |
| ∆(0–30)C-peptide/ ∆(0–30)Glucose | 0.38 | (0.26, 0.57) | 0.37 | (0.25, 0.55) | 0.38 | (0.26, 0.58) | 0.29 |
| AUC(0–30) Insulin/AUC(0–30) Glucose | 25.6 | (16.7, 37.1) | 23.5 | (14.5, 35.7) | 27.1 | (18.3, 37.8) | 0.004 |
| IGI | 77.0 | (45.9, 129.4) | 73.3 | (40.3, 121.1) | 79.9 | (47.6, 135.5) | 0.018 |
| Fasting IC (10−3) | 15.2 | (11.8, 19.7) | 15.8 | (12.1, 20.4) | 14.9 | (11.6, 19.3) | 0.0199 |
| ∆(0–30)IC (10−4) | 2.43 | (1.65, 3.56) | 2.54 | (1.69, 3.65) | 2.39 | (1.62, 3.51) | 0.32 |
| IC 120 min (10−3) | 6.69 | (5.20, 8, 35) | 7.05 | (5.25, 8.89) | 6.54 | (5.16, 8.12) | 0.005 |
| HOMA-IR2 | 0.81 | (0.55, 1.30) | 0.80 | (0.53, 1.30) | 0.82 | (0.56, 1.28) | 0.48 |
| Matsuda Index | 6.14 | (3.85, 8.77) | 6.27 | (4.06, 9.14) | 6.11 | (3.78, 8.62) | 0.22 |
| Adipo-IR | 20.9 | (12.9, 35.1) | 20.5 | (12.6, 35.6) | 21.3 | (13.0, 35.0) | 0.76 |
| ISI-FFA | 1.14 | (0.90, 1.36) | 1.15 | (0.88, 1.37) | 1.12 | (0.90, 1.35) | 0.45 |
| Liver-IR | 1.81 | (1.73, 1.91) | 1.79 | (1.69,1.90) | 1.83 | (1.74, 1.93) | <0.0001 |
| Hepatic-IR (105) | 11.9 | (7.8, 18.0) | 11.6 | (7.5, 18.3) | 12.1 | (8.1, 17.9) | 0.35 |
| FLI | 47 | (25, 69) | 55 | (33, 75) | 40 | (20, 64) | <0.0001 |
| NAFLD-FLS | –1.30 | (−2.22, −0.42) | −1.29 | (−2.18, −0.27) | −1.32 | (−2.24, −0.52) | 0.38 |
| eGFR-CKD (mL/min/1.73 m2) | 77 | (66, 87) | 80 | (69, 89) | 75 | (65, 85) | <0.0001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pina, A.F.; Patarrão, R.S.; Ribeiro, R.T.; Penha-Gonçalves, C.; Raposo, J.F.; Gardete-Correia, L.; Duarte, R.; M. Boavida, J.; L. Medina, J.; Henriques, R.; et al. Metabolic Footprint, towards Understanding Type 2 Diabetes beyond Glycemia. J. Clin. Med. 2020, 9, 2588. https://doi.org/10.3390/jcm9082588
Pina AF, Patarrão RS, Ribeiro RT, Penha-Gonçalves C, Raposo JF, Gardete-Correia L, Duarte R, M. Boavida J, L. Medina J, Henriques R, et al. Metabolic Footprint, towards Understanding Type 2 Diabetes beyond Glycemia. Journal of Clinical Medicine. 2020; 9(8):2588. https://doi.org/10.3390/jcm9082588
Chicago/Turabian StylePina, Ana F., Rita S. Patarrão, Rogério T. Ribeiro, Carlos Penha-Gonçalves, João F. Raposo, Luís Gardete-Correia, Rui Duarte, José M. Boavida, José L. Medina, Roberto Henriques, and et al. 2020. "Metabolic Footprint, towards Understanding Type 2 Diabetes beyond Glycemia" Journal of Clinical Medicine 9, no. 8: 2588. https://doi.org/10.3390/jcm9082588
APA StylePina, A. F., Patarrão, R. S., Ribeiro, R. T., Penha-Gonçalves, C., Raposo, J. F., Gardete-Correia, L., Duarte, R., M. Boavida, J., L. Medina, J., Henriques, R., & Macedo, M. P. (2020). Metabolic Footprint, towards Understanding Type 2 Diabetes beyond Glycemia. Journal of Clinical Medicine, 9(8), 2588. https://doi.org/10.3390/jcm9082588







