Poor Compliance of Diabetic Patients with AI-Enabled E-Health Self-Care Management in Saudi Arabia
Abstract
:1. Introduction
2. Literature Survey
3. Artificial Intelligence and Self Compliance in Diabetic Patients
4. Levels of Practice in Self-Management
5. Methodology
- (a)
- Inclusion: Patients aged 18 years or older (adults), Saudi citizens, male and female, with more than one year of treatment for diabetes.
- (b)
- Exclusion: Patients below 18 years of age, non-Saudi citizens, less than one year of diabetes treatment.
6. Results
6.1. Demographic Profile
6.2. Diabetes Status
6.3. Outpatient Treatment Status
7. Discussion
8. Conclusions
9. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Diabetes Federation (IDF). Diabetes Facts & Figures. 9 December 2021. Available online: https://www.idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html (accessed on 6 October 2022).
- Robert, A.A.; Aldawish, M. The Worrying Trend of Diabetes Mellitus in Saudi Arabia: An Urgent Call to Action. Curr. Diabetes Rev. 2020, 16, 204–210. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). eHealth at WHO. 2019. Available online: https://www.who.int/ehealth/en/ (accessed on 15 January 2022).
- Eysenbach, G. What is e-health? J. Med. Internet Res. 2001, 3, e20. [Google Scholar] [CrossRef] [PubMed]
- Thestrup, J.; Gergely, T.; Beck, P. Exploring New Care Models in Diabetes Management and Therapy with a Wireless Mobile eHealth Platform. In MobiHealth 2011: Wireless Mobile Communication and Healthcare; Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering Series; Nikita, K., Lin, J., Fotiadis, D., Arredondo, W.M., Eds.; Springer: Berlin/Heidelberg, Germany, 2012; Volume 83, pp. 203–210. [Google Scholar] [CrossRef]
- Kaufman, N.; Khurana, I.; Holmen, H.; Torbjørnsen, A.; Wahl, A.; Jenum, A.; Småstuen, M.C.; Årsand, E.; Ribu, L.; Harrison, S.; et al. Using digital health technology to prevent and treat diabetes. Diabetes Technol. Ther. 2016, 18, S56–S68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- From, K. The Emergence of Personalised E-Health Care. Open Access Government UK. 12 April 2018. Available online: https://www.openaccessgovernment.org/emergence-personalised-ehealth-care/44428/ (accessed on 20 February 2022).
- Cahn, A.; Akirov, A.; Raz, I. Digital health technology and diabetes management. J. Diabetes 2018, 10, 10–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Gemert-Pijnen, J.E.; Nijland, N.; van Limburg, M.; Ossebaard, H.C.; Kelders, S.M.; Eysenbach, G.; Seydel, E.R. A holistic framework to improve the uptake and impact of eHealth technologies. J. Med. Internet Res. 2011, 13, e111. [Google Scholar] [CrossRef] [PubMed]
- Adenuga, O.A.; Kekwaletswe, R.M.; Coleman, A. eHealth integration and interoperability issues: Towards a solution through enterprise architecture. Health Inf. Sci. Syst. 2015, 3, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Weber-Jahnke, J.; Peyton, L.; Topaloglou, T. eHealth system interoperability. Inf. Syst. Front. 2012, 14, 1–3. [Google Scholar] [CrossRef]
- Kuziemsky, C.E.; Weber-Jahnke, J.H. An eBusiness-based framework for eHealth interoperability. J. Emerg. Technol. Web Intell. 2009, 1, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Rejeb, O.; Bastide, R.; Lamine, E.; Marmier, F.; Pingaud, H. A model driven engineering approach for business continuity management in e-Health systems. In Proceedings of the 6th IEEE International Conference on Digital Ecosystems and Technologies (DEST), Campione d’Italia, Italy, 18–20 June 2012; pp. 1–7. [Google Scholar] [CrossRef]
- Bourquard, K.; Le Gall, F.; Cousin, P. Standards for interoperability in digital health: Selection and implementation in an eHealth project. In Requirements Engineering for Digital Health; Fricker, S., Thümmler, C., Gavras, A., Eds.; Springer: Cham, Switzerland, 2015; pp. 95–115. [Google Scholar] [CrossRef]
- Kayser, L.; Kushniruk, A.; Osborne, R.H.; Norgaard, O.; Turner, P. Enhancing the effectiveness of consumer-focused health information technology systems through eHealth literacy: A framework for understanding users’ needs. JMIR Hum. Factors 2015, 2, e9. [Google Scholar] [CrossRef] [Green Version]
- Inverardi, P.; Mori, M. Requirements models at run-time to support consistent system evolutions. In Proceedings of the 2nd International Workshop on Requirements@ Run.Time, Trento, Italy, 30 August 2011; pp. 1–8. [Google Scholar] [CrossRef]
- Vasilyeva, E.; Pechenizkiy, M.; Puuronen, S. Towards the framework of adaptive user interfaces for eHealth. In Proceedings of the 18th IEEE Symposium on Computer-Based Medical Systems (CBMS’05), Dublin, Ireland, 23–24 June 2005; pp. 139–144. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, J.J.; La Torre, I.D.; Fernández, G.; López-Coronado, M. Analysis of the security and privacy requirements of cloud-based electronic health records systems. J. Med. Internet Res. 2013, 15, e186. [Google Scholar] [CrossRef]
- Alturki, R.; Alyamani, H.J.; Ikram, M.A.; Rahman, M.A.; Alshehri, M.D.; Khan FHaleem, M. Sensor-Cloud Architecture: A Taxonomy of Security Issues in Cloud-Assisted Sensor Networks. IEEE Access 2021, 9, 89344–89359. [Google Scholar] [CrossRef]
- Grundy, J.; Abdelrazek, M.; Curumsing, M.K. Vision: Improved development of mobile eHealth applications. In Proceedings of the IEEE/ACM 5th International Conference on Mobile Software Engineering and Systems (MOBILESoft), Gothenburg, Sweden, 27 May–3 June 2018; pp. 219–223. [Google Scholar]
- Heffernan, K.J.; Chang, S.; Maclean, S.T.; Callegari, E.T.; Garland, S.M.; Reavley, N.J.; Varigos, G.A.; Wark, J.D. Guidelines and recommendations for developing interactive eHealth apps for complex messaging in health promotion. JMIR Mhealth Uhealth 2016, 4, e14. [Google Scholar] [CrossRef]
- Al Hayek, A.A.; Robert, A.A.; Al Dawish, M.A.; Zamzami, M.M.; Sam, A.E.; Alzaid, A.A. Impact of an education program on patient anxiety, depression, glycemic control, and adherence to self-care and medication in type 2 diabetes. J. Fam. Community Med. 2013, 20, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.R.; Al-Abdul Lateef, Z.N.; Al Aithan, M.A.; Bu-Khamseen, M.A.; Al Ibrahim, I.; Khan, S.A. Factors contributing to non-compliance among diabetics attending primary health centers in the Al Hasa district of Saudi Arabia. J. Fam. Community Med. 2012, 19, 26–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alanzi, T.M.; Istepanian, R.S.; Philip, N.; Sungoor, A. A study on perception of managing diabetes mellitus through social networking in the Kingdom of Saudi Arabia. In Proceedings of the XIII Mediterranean Conference on Medical and Biological Engineering and Computing, Seville, Spain, 25–28 September 2013; Romero, L.R., Ed.; Springer: Cham, Switzerland, 2014. [Google Scholar]
- Alotaibi, M.M. A study on the needs for educating and managing fasting diabetes through mobile health in the Kingdom of Saudi Arabia. Int. J. Comput. Syst. 2015, 2, 95–98. [Google Scholar]
- Alotaibi, M.M.; Istepanian, R.; Philip, N. A mobile diabetes management and educational system for type-2 diabetics in Saudi Arabia (SAED). Mhealth 2016, 2, 33. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, E.; Yunus, F.; Househ, M. The impact of mobile phone screen size on user comprehension of health information. Stud. Health Technol. Inform. 2013, 190, 154–156. [Google Scholar] [PubMed]
- Hoque, M.R. An Empirical Study of Mhealth Adoption in a Developing Country: The Moderating Effect of Gender Concern. BMC Med. Inform. Decis. Mak. 2016, 16, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alturki, R.; Gay, V. The Development of an Arabic Weight-Loss App Akser Waznk: Qualitative Results. JMIR Form. Res. 2019, 3, e11785. [Google Scholar] [CrossRef] [Green Version]
- Alturki, R.; Gay, V. Usability Attributes for Mobile Applications: A Systematic Review. In Recent Trends and Advances in Wireless and IoT-enabled Networks; Springer: Cham, Switzerland, 2019; pp. 53–62. [Google Scholar]
- Alturki, R.; Gay, V. A Systematic Review on What Features Should be supported by Fitness Apps and Wearables to Help Users Overcome Obesity. Int. J. Res. Eng. Technol. 2016, 5, 197–206. [Google Scholar]
- Kariuki, E.G.; Okanda, P. Adoption of M-Health and Usability Challenges in M-Health Applications in Kenya: Case of Uzazi Poa M-Health Prototype Application. In Proceedings of the 2017 IEEE AFRICON, Cape Town, South Africa, 18–20 September 2017; pp. 530–535. [Google Scholar]
- Zhang, X.; Han, X.; Dang, Y.; Meng, F.; Guo, X.; Lin, J. User acceptance of mobile health services from users’ perspectives: The role of self-efficacy and response-efficacy in technology acceptance. Inform. Health Soc. Care 2017, 42, 194–206. [Google Scholar] [CrossRef] [PubMed]
- Crico, C.; Renzi, C.; Graf, N.; Buyx, A.; Kondylakis, H.; Koumakis, L.; Pravettoni, G. mHealth and Telemedicine Apps: In Search of a Common Regulation. ecancerMedicalscience 2018, 12, 853. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atallah, N.; Khalifa, M.; El Metwally, A.; Househ, M. The Prevalence and Usage of Mobile Health Applications among Mental Health Patients in Saudi Arabia. Comput. Methods Programs Biomed. 2018, 156, 163–168. [Google Scholar] [CrossRef]
- Abid, A. M-Health Technologies to Be Key Enablers of Saudi Digital Transformation Process: Expert. Retrieved 12 April 2019. Available online: http://www.arabnews.com/node/1465921/saudi-arabia (accessed on 20 March 2022).
- Shrivastava, S.R.; Shrivastava, P.S.; Ramasamy, J. Role of self-care in management of diabetes mellitus. J. Diabetes Metab. Disord. 2013, 12, 14. [Google Scholar] [CrossRef] [Green Version]
- Alanazi, F.; Gay, V.; Alanazi, M.; Alturki, R. Modelling Health Process and System Requirements Engineering for Better eHealth Services in Saudi Arabia. Int. J. Adv. Comput. Sci. Appl. 2021, 12, 9–11. [Google Scholar] [CrossRef]
- Saad, A.M.; Younes, Z.M.; Ahmed, H.; Brown, J.A.; Al Owesie, R.M.; Hassoun, A.A. Self-efficacy, self-care and glycaemic control in Saudi Arabian patients with type 2 diabetes mellitus: A cross-sectional survey. Diabetes Res. Clin. Pract. 2018, 137, 28–36. [Google Scholar] [CrossRef]
- Al-Hanawi, M.K.; Alsharqi, O.; Almazrou, S.; Vaidya, K. Healthcare Finance in the Kingdom of Saudi Arabia: A Qualitative Study of Householders’ Attitudes. Appl. Health Econ. Health Policy 2018, 16, 55–64. [Google Scholar] [CrossRef]
- Patrick, K.; Griswold, W.G.; Raab, F.; Intille, S.S. Health and the Mobile Phone. Am. J. Prev. Med. 2008, 35, 177–181. [Google Scholar] [CrossRef]
- Brzan, P.P.; Rotman, E.; Pajnkihar, M.; Klanjsek, P. Mobile Applications for Control and Self Management of Diabetes: A Systematic Review. J. Med. Syst. 2016, 40, 210. [Google Scholar] [CrossRef]
- Schwartz, J.M.; Moy, A.J.; Rossetti, S.C.; Elhadad, N.; Cato, K.D. Clinician involvement in research on machine learning-based predictive clinical decision support for the hospital setting: A scoping review. J. Am. Med. Inform. Assoc. 2021, 28, 653–663. [Google Scholar] [CrossRef]
- Cleveringa, F.G.W.; Gorter, K.J.; van den Donk, M.; van Gijsel, J.; Rutten, G.E.H.M. Computerized Decision Support Systems in Primary Care for Type 2 Diabetes Patients Only Improve Patients’ Outcomes when Combined with Feedback on Performance and Case Management: A Systematic Review. Diabetes Technol. Ther. 2013, 15, 180–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, K.H.; Beam, A.L.; Kohane, I.S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2018, 2, 719–731. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. BMJ J. 2017, 2, 230–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- North West Primary Care. 5 Ways Smart Watches Can Improve Your Health. 2020. Available online: https://www.nwpc.com (accessed on 29 July 2022).
- Alqahtani, A.H.; Alzahrani, A.S.; Alzahrani, S.H.; Alqahtani, S.M.; AlOtaibi, A.F.; Khan, A.A. Levels of Practice and Determinants of Diabetes Self-Care in Primary Health Care in Jeddah City, Saudi Arabia. Cureus 2020, 12, e8816. [Google Scholar] [CrossRef] [PubMed]
- Al Johani, K.A.; Kendall, G.E.; Snider, P.D. Self-management practices among type 2 diabetes patients attending primary health-care centres in Medina, Saudi Arabia. East. Mediterr. Health J. 2015, 21, 621–628. [Google Scholar] [CrossRef]
- Sabbah, K.O.A.; Al-Shehri, A.A. Practice and perception of self-management among diabetics in Taif, KSA: Impact of demographic factors. Int. J. Med. Sci. Public Health 2014, 3, 277–285. [Google Scholar] [CrossRef] [Green Version]
- World Population Review. Jeddah Population. 2019. Available online: http://worldpopulationreview.com/world-cities/jeddah-population/ (accessed on 12 December 2021).
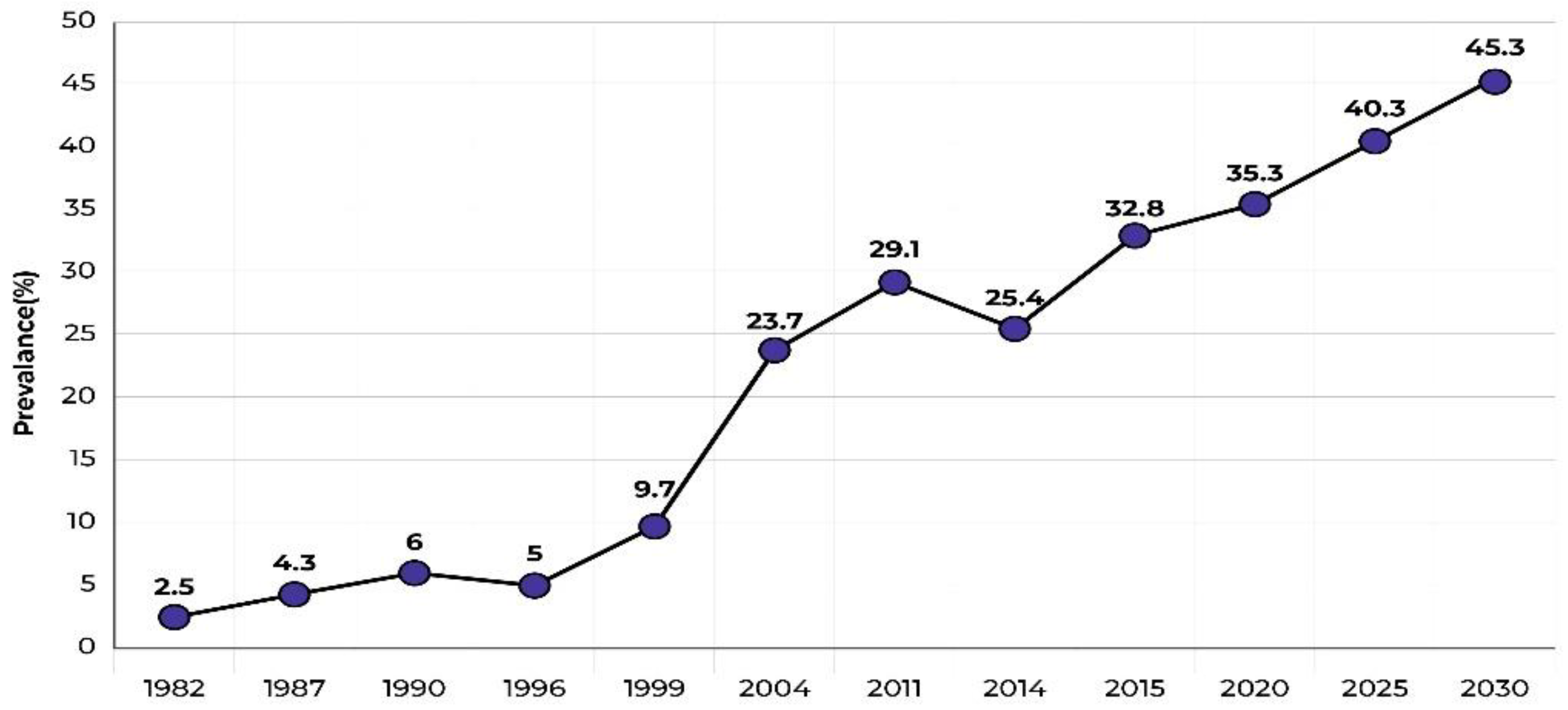
- ArabNews. Diabetes: Saudi Arabia’s Growing Health Problem. 12 April 2019. Available online: http://www.arabnews.com/node/1481756/saudi-arabia (accessed on 17 November 2021).
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet ESurveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics; Pearson: London, UK, 2007. [Google Scholar]
- Darkins, A.; Ryan, P.; Kobb, R.; Foster, L.; Edmonson, E.; Wakefield, B.; Lancaster, A.E. Coordination/Home Telehealth: The systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed. e-Health 2008, 14, 1118–1126. [Google Scholar] [CrossRef] [Green Version]
- Hess, R.; Bryce, C.L.; Paone, S.; Fischer, G.; McTigue, K.M.; Olshansky, E.; Zickmund, S.; Fitzgerald, K.; Siminerio, L. Exploring challenges and potentials of personal health records in diabetes self-management: Implementation and initial assessment. Telemed. e-Health 2007, 13, 509–518. [Google Scholar] [CrossRef] [Green Version]
- Blaya, J.A.; Fraser, H.S.; Holt, B. E-health technologies show promise in developing countries. Health Aff. 2010, 29, 244–251. [Google Scholar] [CrossRef] [Green Version]
- Winterlich, A.; Stevenson, I.; Waldren, A.; Dawson, T. Diabetes Digital Coach: Developing an infrastructure for e-health self-management tools. In Proceedings of the 9th International Conference on Developments in eSystems Engineering (DeSE), Liverpool, UK, 31 August–2 September 2016; pp. 68–73. [Google Scholar] [CrossRef]
- King, D.K.; Doty, A.; Martin, C.; Boggs, J.M.; Faber, A.J.; Geno, C.R.; Glasgow, R.E. What patients want: Relevant health information technology for diabetes self-management. Health Technol. 2012, 2, 147–157. [Google Scholar] [CrossRef]
- Su, C.-J.; Wu, C.-Y. JADE implemented mobile multi-agent based, distributed information platform for pervasive health care monitoring. Appl. Soft Comput. 2011, 11, 315–325. [Google Scholar] [CrossRef]
- Ricciardi, L.; Mostashari, F.; Murphy, J.; Daniel, J.G.; Siminerio, E.P. A National Action Plan To Support Consumer Engagement Via E-Health. Health Aff. 2013, 32, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, F.; Gay, V. e-Health for Diabetes Self-Management in Saudi Arabia: Barriers and Solutions. In Proceedings of the 36th International Business Information Management Association Conference (IBIMA), Granada, Spain, 4–5 November 2020; ISBN 978-0-9998551-5-7. [Google Scholar]
- Aikens, J.E.; Rosland, A.M.; Piette, J.D. Improvements in illness self-management and psychological distress associated with telemonitoring support for adults with diabetes. Prim. Care Diabetes 2015, 9, 127–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ciemins, E.; Coon, P.; Peck, R.; Holloway, B.; Min, S.J. Using telehealth to provide diabetes care to patients in rural Montana: Findings from the promoting realistic individual self-management program. Telemed. e-Health 2011, 17, 596–602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aldahmash, A.M.; Ahmed, Z.; Qadri, F.R.; Thapa, S.; AlMuammar, A.M. Implementing a connected health intervention for remote patient monitoring in Saudi Arabia and Pakistan: Explaining ‘the what’and ‘the how’. Glob. Health 2019, 15, 20. [Google Scholar] [CrossRef]
- Sweileh, W.; Aker, O.; Hamooz, S. Rate of Compliance among Patients with Diabetes Mellitus and Hypertension. An-Najah Univ. J. Res. 2005, 19, 1–12. [Google Scholar]




| Description | Prescribed | Followed | Percentage | |
|---|---|---|---|---|
| A | Medical treatment | 199 | 183 | 92.0 |
| B | Diet control (quantity and type of daily consumed food) | 137 | 62 | 45.3 |
| C | Daily exercise | 172 | 47 | 27.3 |
| D | Self-care programme | 182 | 72 | 42 |
| E | Registered in the hospital e-health system | 182 | 88 | 48.4 |
| F | Hospital with e-health self-care management system | 182 | 72 | 39.6 |
| G | Regular blood glucose monitoring | 121 | 149 | 123.1 |
| H | Blood glucose reporting hospital through e-health | 121 | 49 | 40.5 |
| I | Insulin injection | 134 | 156 | 116.4 |
| J | Injection reporting hospital through e-health | 134 | 44 | 32.8 |
| K | Daily diet regulation | 89 | 60 | 67.4 |
| L | Daily work-out | 69 | 53 | 76.8 |
| M | Abnormal conditions reported | 210 | 76 | 36.2 |
| Variable | Correlation Co-Efficient |
|---|---|
| Experience with e-health system versus attitude about e-health system | 0.555 ** |
| Experience with e-health system versus higher education (postgraduate) | 0.160 * |
| Attitude about e-health system and participants with low incomes (<8000 riyals) | 0.166 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alanazi, F.; Gay, V.; Alturki, R. Poor Compliance of Diabetic Patients with AI-Enabled E-Health Self-Care Management in Saudi Arabia. Information 2022, 13, 509. https://doi.org/10.3390/info13110509
Alanazi F, Gay V, Alturki R. Poor Compliance of Diabetic Patients with AI-Enabled E-Health Self-Care Management in Saudi Arabia. Information. 2022; 13(11):509. https://doi.org/10.3390/info13110509
Chicago/Turabian StyleAlanazi, Fuhid, Valerie Gay, and Ryan Alturki. 2022. "Poor Compliance of Diabetic Patients with AI-Enabled E-Health Self-Care Management in Saudi Arabia" Information 13, no. 11: 509. https://doi.org/10.3390/info13110509
APA StyleAlanazi, F., Gay, V., & Alturki, R. (2022). Poor Compliance of Diabetic Patients with AI-Enabled E-Health Self-Care Management in Saudi Arabia. Information, 13(11), 509. https://doi.org/10.3390/info13110509









