Sr and Mg Doped Bi-Phasic Calcium Phosphate Macroporous Bone Graft Substitutes Fabricated by Robocasting: A Structural and Cytocompatibility Assessment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Synthesis of Biphasic Calcium Phosphate Powders
2.2. Preparation of the Robocasting “Inks” and Printing of the 3D Macroporous Constructs
2.3. Physical–Chemical Characterization Techniques
2.4. In Vitro Cytocompatibility Assays
2.4.1. Sample Preparation
2.4.2. Human Osteoblasts Cell Culturing
2.4.3. MTS-Based Cell Proliferation Assay
2.4.4. Lactate Dehydrogenase (LDH)-Based Cell Proliferation Assay
2.4.5. Acridine Orange (AO)-Based Cell Proliferation Assay
2.4.6. LDH Cell Death Assay
2.4.7. Epifluorescence Microscopy
2.4.8. SEM Preparation and Examination
2.4.9. Statistical Analysis
3. Results and Discussion
3.1. Physical-Chemical Investigations
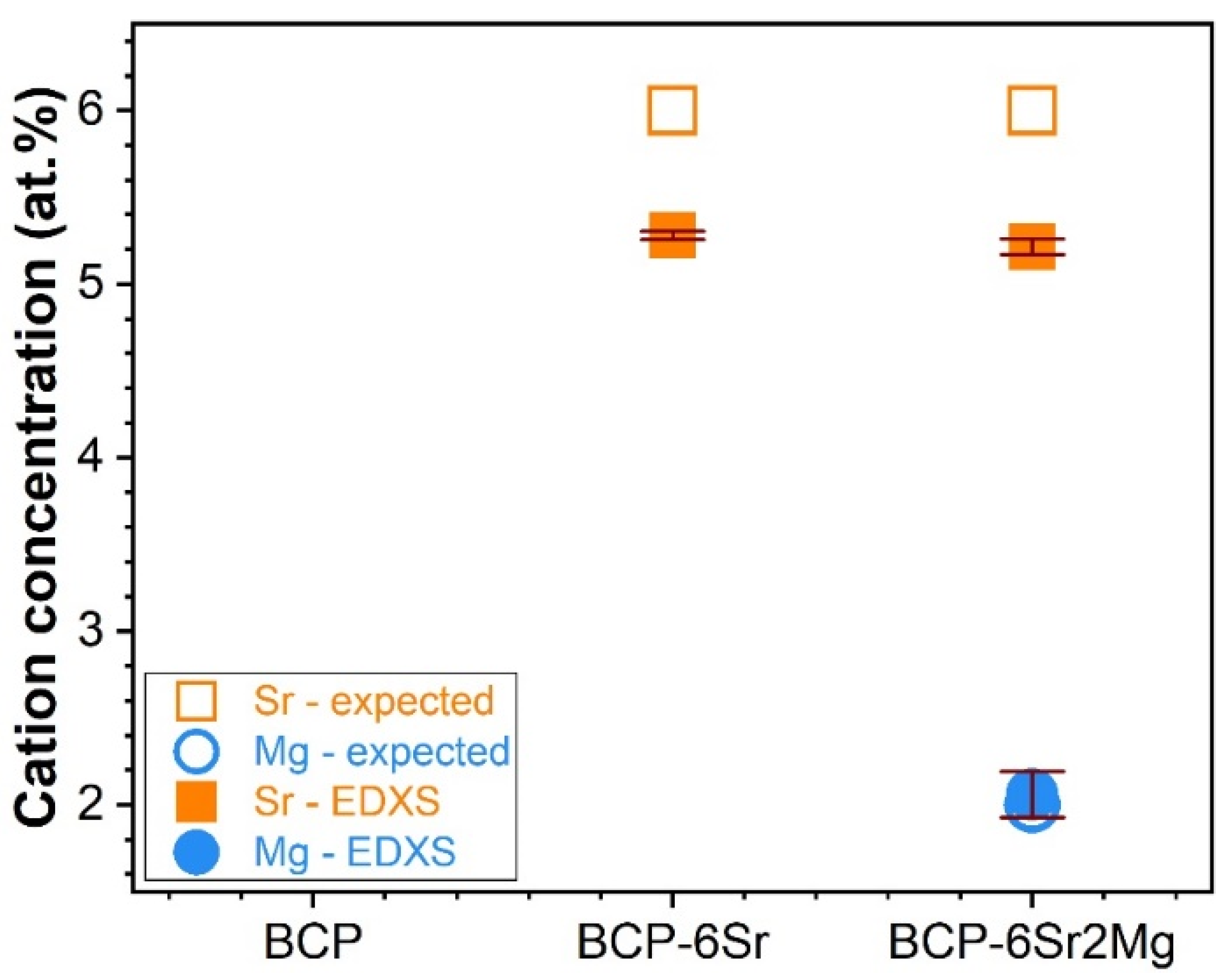
3.1.1. Morphology and Composition
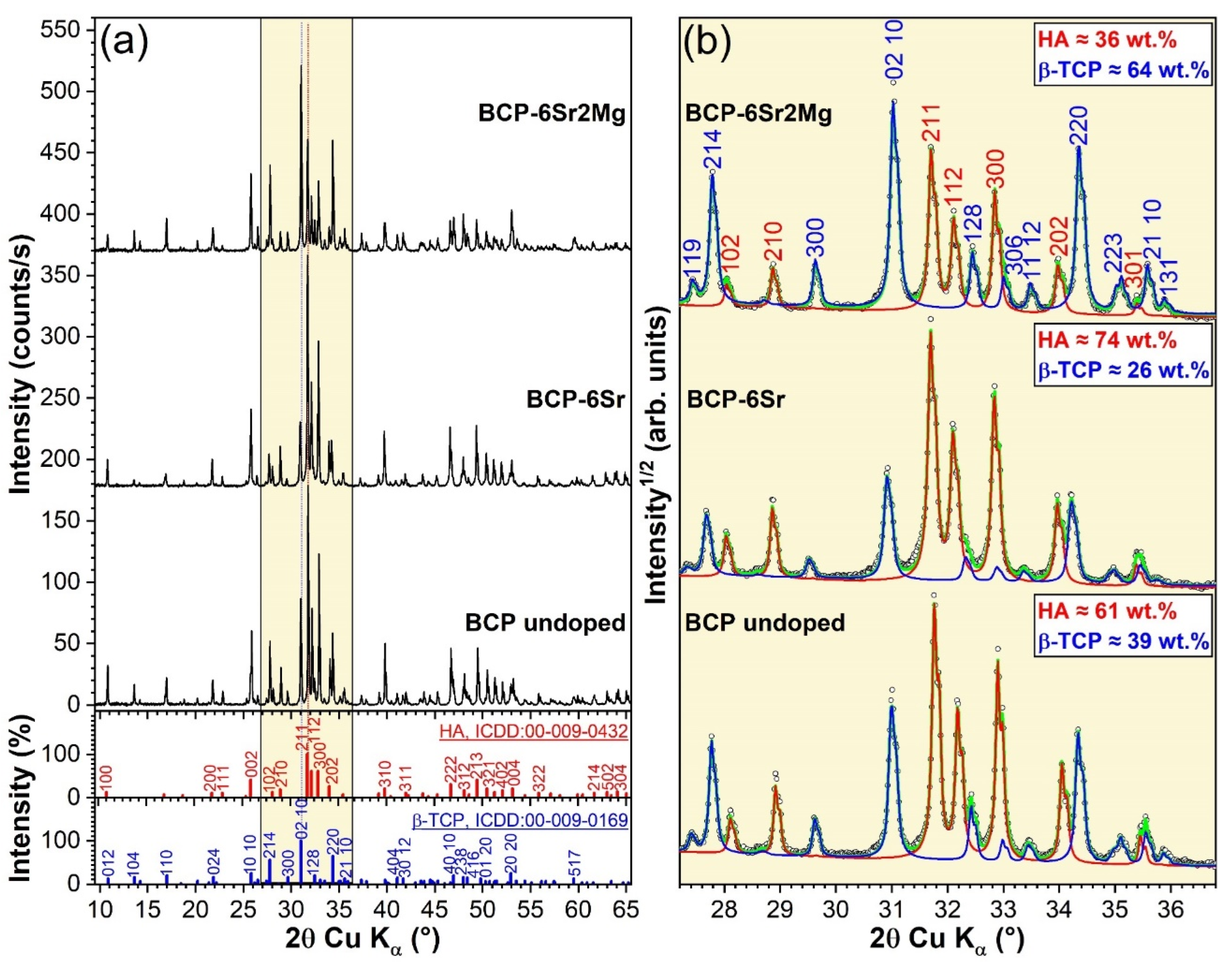
3.1.2. Structure
- HA presented an IR absorption spectrum featuring sharp peaks assigned to the doubly-degenerated (ν2) bending (~474 cm−1), triply-degenerated (ν4) bending (~570 and 602 cm−1), nondegenerated (ν1) symmetric stretching (~962 cm−1), and triply-degenerated (ν3) asymmetric stretching (~1033, 1045 and 1090 cm−1) of the orthophosphate groups; and the libration (νL) of the structural hydroxyl units (~632 cm−1) [76,77,78].
- β-TCP yielded a much more convoluted spectral envelope presenting broad maxima associated with the doubly-degenerated (ν2) bending (~435 cm−1), triply degenerated (ν4) asymmetric bending (at ~552 and 603 cm−1), factor group splitting of (ν1) symmetric stretching (at ~944 and 971 cm−1), and the triply degenerated (ν3) asymmetric stretching (at ~1015, 1036, 1081, and 1116 cm−1) of orthophosphate units [78,79,80].
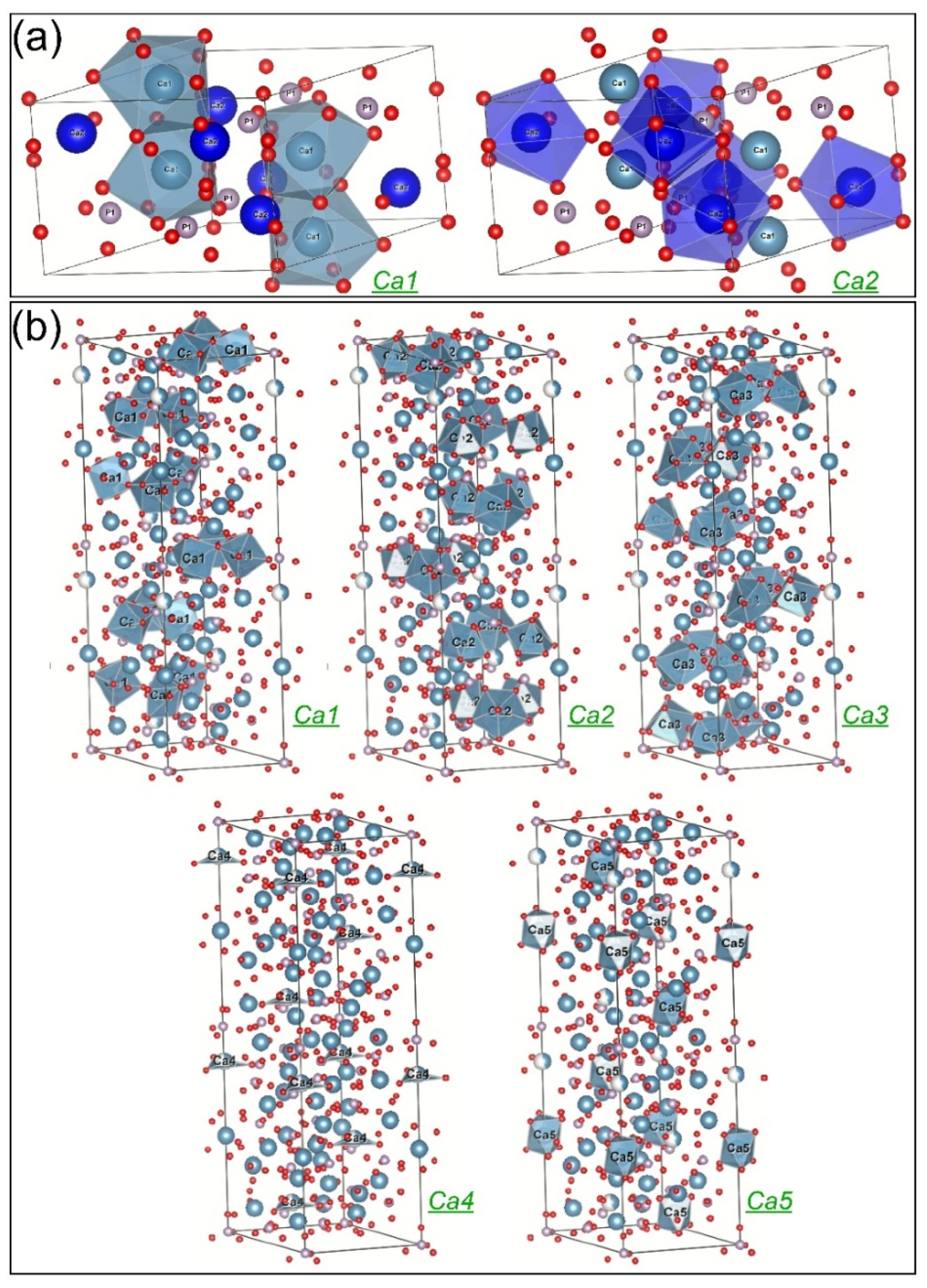
- In HA, Sr substituted Ca with a probability of about 10% on both positions. In comparison, Mg entered the Ca1 site replacing 10% of Ca from these positions and only 1% of Ca2. It is generally believed that larger-sized cations tend to have a higher coordination number with the surrounding anions, while smaller-sized cations prefer to occupy smaller coordination sites [88]. Indeed, Ressler et al. [87] showed experimentally that Sr can occupy preferentially Ca1 sites in HA, but our results have not confirmed this, since similar probabilities for Sr to occupy the nine-coordinated Ca1 and the seven-coordinated Ca2 sites in HA were found. However, if one considers only the first nearest neighbouring oxygen atoms, both positions of Ca in HA are basically six-coordinated [89], which may support our result on Sr site affinity in HA. The preference of the smaller Mg ion for Ca1 is in an even greater contradiction with the above-presented conventional expectations. However, Ren et al. [90] obtained by simulation that the substitution of Mg for Ca1 sites in HA is energetically favoured, while Matsunaga [88] predicted theoretically a preference of Mg for Ca2 position in HA. On the other hand, it is reasonable to accept that the substitution preferences of Mg are different when there is competition with Sr, as in our case.
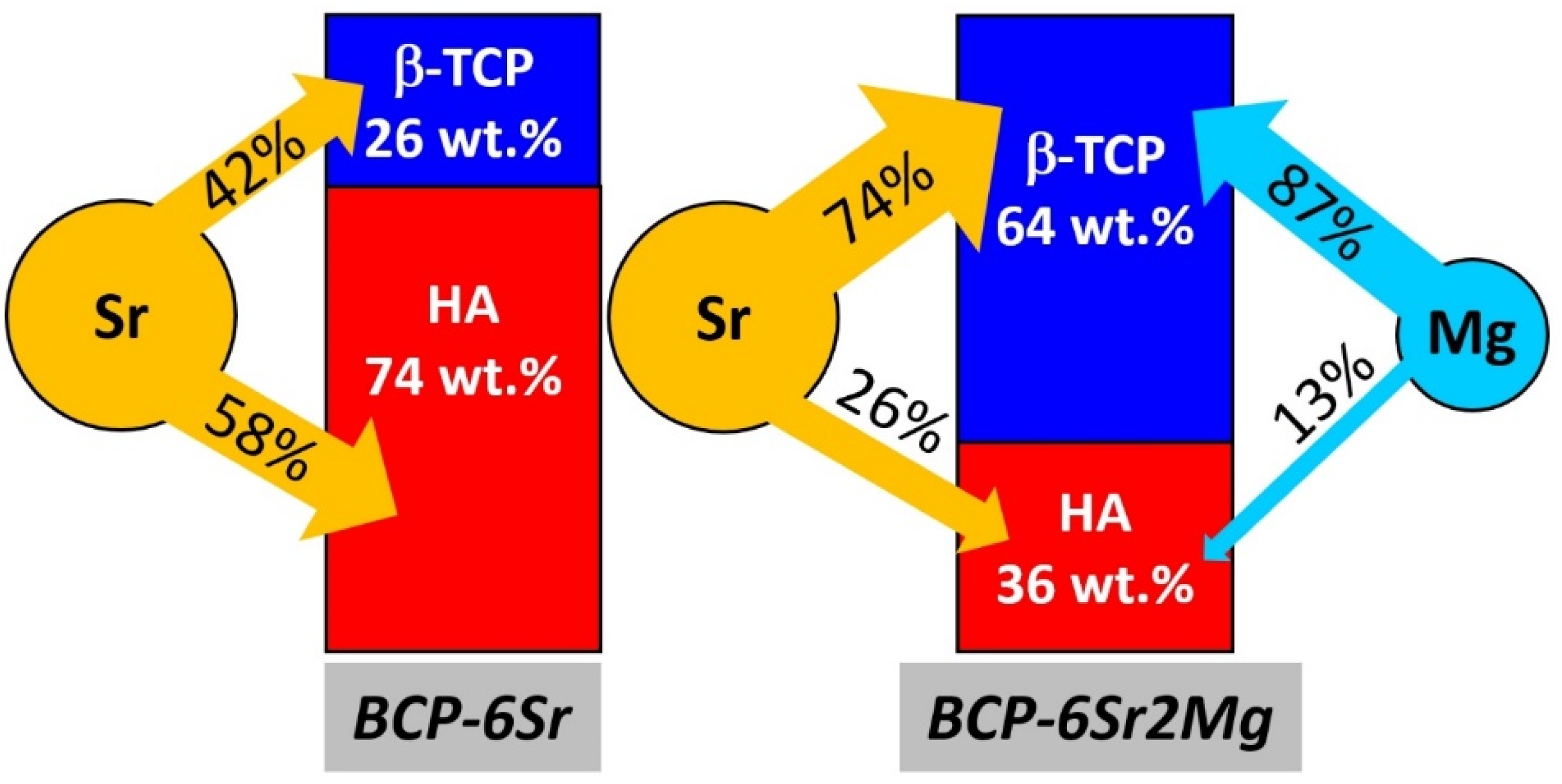
- In β-TCP, Sr behaved differently, when used as a single dopant than when associated with Mg. As a single dopant, Sr preferentially replaced Ca4 (~70%) and Ca3 (25%), and ~13% of Ca1, Ca2, or Ca5. The preference of Sr for Ca3 and Ca4 sites in β-TCP agrees with the theoretical predictions of Matsunaga et al. [91]. The affinity of Sr for the Ca4 sites has been also experimentally demonstrated in the case of β-TCP in several studies [56,92,93]. In the presence of Mg, Sr apparently substituted all Ca4 atoms, possibly occupying also part of the vacant positions of this crystallographic site. Mg showed a strong preference for the Ca3 (~35%) and Ca1 (~25%) sites, while Sr substituted about 15% of Ca on Ca2 sites, and ca. 5% from the Ca1, Ca3, and Ca5 sites. Therefore, the preference of Sr for Ca4 sites in β-TCP was enhanced in the presence of Mg, (i.e., BCP-6Sr2Mg samples), while the share of Ca3 and Ca1 sites decreased as an [56,92,93] effect of competition between Sr and Mg cations.
3.2. Preliminary In Vitro Cytocompatibility Assessments
3.2.1. Cell Proliferation
MTS-Based Cell Proliferation Assay
LDH-Based Cell Proliferation Assay
AO-Based Cell Proliferation Assay
Integrative Analysis of the Cell Proliferation Assays
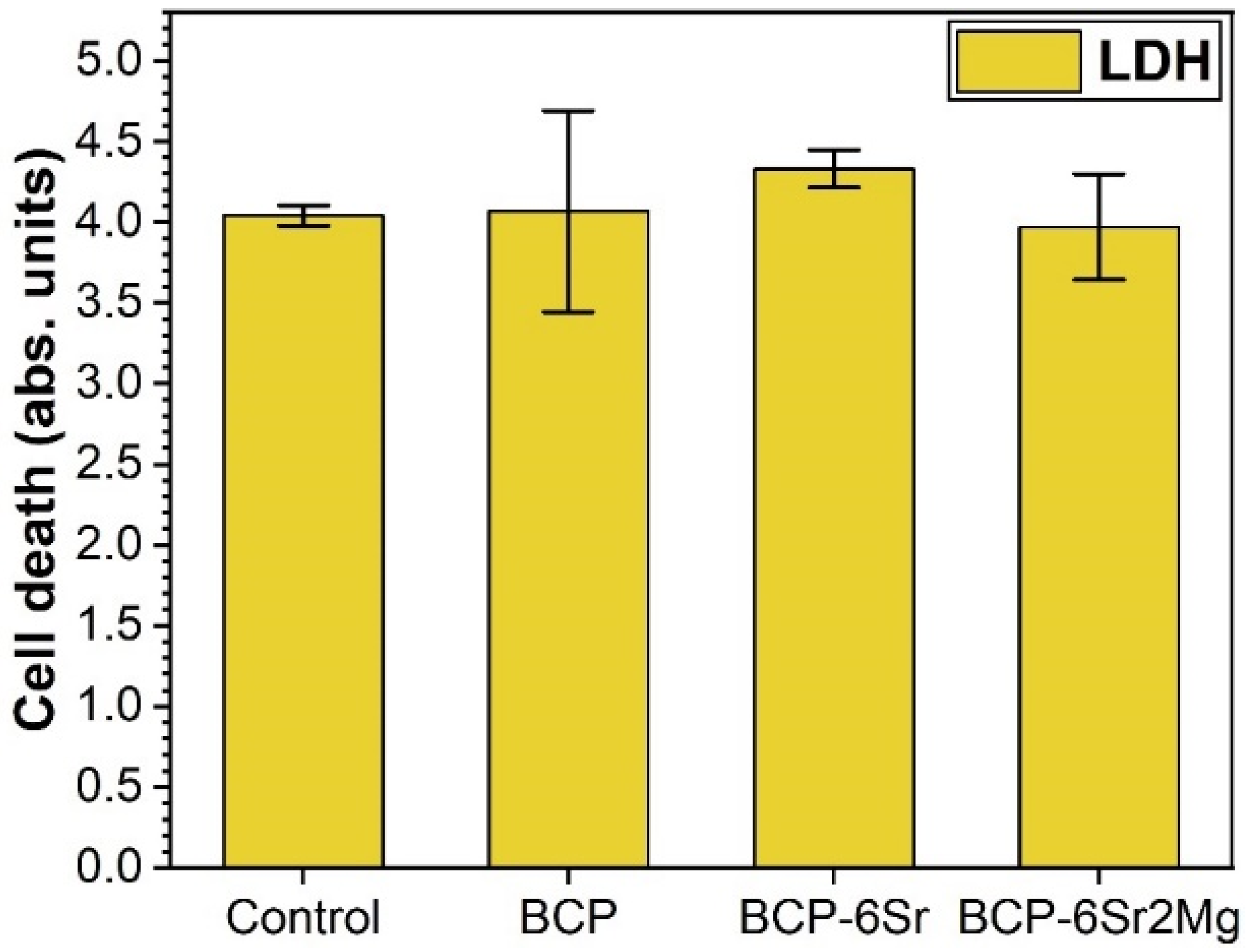
3.2.2. Cell Death
3.2.3. Cell Morphology
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Greenwald, A.S.; Boden, S.D.; Goldberg, V.M.; Khan, Y.; Laurencin, C.T.; Rosier, R.N. Bone-Graft Substitutes: Facts, Fictions, and Applications. J. Bone Jt. Surg.-Am. Vol. 2001, 83, 98–103. [Google Scholar] [CrossRef]
- Gillman, C.E.; Jayasuriya, A.C. FDA-Approved Bone Grafts and Bone Graft Substitute Devices in Bone Regeneration. Mater. Sci. Eng. C 2021, 130, 112466. [Google Scholar] [CrossRef]
- Beaman, F.D.; Bancroft, L.W.; Peterson, J.J.; Kransdorf, M.J. Bone Graft Materials and Synthetic Substitutes. Radiol. Clin. N. Am. 2006, 44, 451–461. [Google Scholar] [CrossRef]
- Titsinides, S.; Agrogiannis, G.; Karatzas, T. Bone Grafting Materials in Dentoalveolar Reconstruction: A Comprehensive Review. Jpn. Dent. Sci. Rev. 2019, 55, 26–32. [Google Scholar] [CrossRef]
- Sohn, H.-S.; Oh, J.-K. Review of Bone Graft and Bone Substitutes with an Emphasis on Fracture Surgeries. Biomater. Res. 2019, 23, 9. [Google Scholar] [CrossRef]
- Huang, Y.-C.; Chen, C.-Y.; Lin, K.-C.; Renn, J.-H.; Tarng, Y.-W.; Hsu, C.-J.; Chang, W.-N.; Yang, S.-W. Comparing Morbidities of Bone Graft Harvesting from the Anterior Iliac Crest and Proximal Tibia: A Retrospective Study. J. Orthop. Surg. Res. 2018, 13, 115. [Google Scholar] [CrossRef]
- Ou, C.J.; Sternfeld, W.C.; Stausmire, J.M. Iliac Crest Herniation Secondary to Autogenous Bone Grafting Found on Osteopathic Examination. J. Osteopath. Med. 2015, 115, 518–521. [Google Scholar] [CrossRef]
- Fowler, B.L.; Dall, B.E.; Rowe, D.E. Complications Associated with Harvesting Autogenous Iliac Bone Graft. Am. J. Orthop. 1995, 24, 895–903. [Google Scholar] [PubMed]
- Hinsenkamp, M.; Muylle, L.; Eastlund, T.; Fehily, D.; Noël, L.; Strong, D.M. Adverse Reactions and Events Related to Musculoskeletal Allografts: Reviewed by the World Health Organisation. Int. Orthop. 2012, 36, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, N.; Jupiter, D.C.; Clawson, L.D.; la Fontaine, J. Incorporation of Bovine-Based Structural Bone Grafts Used in Reconstructive Foot Surgery. J. Foot Ankle Surg. 2012, 51, 30–33. [Google Scholar] [CrossRef]
- Buser, Z.; Brodke, D.S.; Youssef, J.A.; Meisel, H.-J.; Myhre, S.L.; Hashimoto, R.; Park, J.-B.; Tim Yoon, S.; Wang, J.C. Synthetic Bone Graft versus Autograft or Allograft for Spinal Fusion: A Systematic Review. J. Neurosurg. Spine 2016, 25, 509–516. [Google Scholar] [CrossRef]
- Plantz, M.A.; Gerlach, E.B.; Hsu, W.K. Synthetic Bone Graft Materials in Spine Fusion: Current Evidence and Future Trends. Int. J. Spine Surg. 2021, 15, S104–S112. [Google Scholar] [CrossRef] [PubMed]
- Zwingenberger, S.; Nich, C.; Valladares, R.D.; Yao, Z.; Stiehler, M.; Goodman, S.B. Recommendations and Considerations for the Use of Biologics in Orthopedic Surgery. BioDrugs 2012, 26, 245–256. [Google Scholar] [CrossRef]
- Touri, M.; Moztarzadeh, F.; Osman, N.A.A.; Dehghan, M.M.; Mozafari, M. 3D–Printed Biphasic Calcium Phosphate Scaffolds Coated with an Oxygen Generating System for Enhancing Engineered Tissue Survival. Mater. Sci. Eng. C 2018, 84, 236–242. [Google Scholar] [CrossRef]
- Gaddam, A.; Brazete, D.S.; Neto, A.S.; Nan, B.; Fernandes, H.R.; Ferreira, J.M.F. Robocasting and Surface Functionalization with Highly Bioactive Glass of ZrO2 Scaffolds for Load Bearing Applications. J. Am. Ceram. Soc. 2022, 105, 1753–1764. [Google Scholar] [CrossRef]
- Entezari, A.; Roohani, I.; Li, G.; Dunstan, C.R.; Rognon, P.; Li, Q.; Jiang, X.; Zreiqat, H. Architectural Design of 3D Printed Scaffolds Controls the Volume and Functionality of Newly Formed Bone. Adv. Healthc. Mater. 2019, 8, 1801353. [Google Scholar] [CrossRef]
- Marques, C.F.; Perera, F.H.; Marote, A.; Ferreira, S.; Vieira, S.I.; Olhero, S.; Miranda, P.; Ferreira, J.M.F. Biphasic Calcium Phosphate Scaffolds Fabricated by Direct Write Assembly: Mechanical, Anti-Microbial and Osteoblastic Properties. J. Eur. Ceram. Soc. 2017, 37, 359–368. [Google Scholar] [CrossRef]
- Miranda, P.; Saiz, E.; Gryn, K.; Tomsia, A.P. Sintering and Robocasting of β-Tricalcium Phosphate Scaffolds for Orthopaedic Applications. Acta Biomater. 2006, 2, 457–466. [Google Scholar] [CrossRef]
- Raymond, Y.; Thorel, E.; Liversain, M.; Riveiro, A.; Pou, J.; Ginebra, M.-P. 3D Printing Non-Cylindrical Strands: Morphological and Structural Implications. Addit. Manuf. 2021, 46, 102129. [Google Scholar] [CrossRef]
- Eggli, P.S.; Muller, W.; Schenk, R.K. Porous Hydroxyapatite and Tricalcium Phosphate Cylinders with Two Different Pore Size Ranges Implanted in the Cancellous Bone of Rabbits. A Comparative Histomorphometric and Histologic Study of Bone Ingrowth and Implant Substitution. Clin. Orthop. Relat. Res. 1988, 232, 127–138. [Google Scholar] [CrossRef]
- le Huec, J.C.; Clément, D.; Brouillaud, B.; Barthe, N.; Dupuy, B.; Foliguet, B.; Basse-Cathalinat, B. Evolution of the Local Calcium Content around Irradiated β-Tricalcium Phosphate Ceramic Implants: In Vivo Study in the Rabbit. Biomaterials 1998, 19, 733–738. [Google Scholar] [CrossRef]
- Ballouze, R.; Marahat, M.H.; Mohamad, S.; Saidin, N.A.; Kasim, S.R.; Ooi, J.P. Biocompatible magnesium-doped Biphasic Calcium Phosphate for Bone Regeneration. J. Biomed. Mater. Res. Part B Appl. Biomater. 2021, 109, 1426–1435. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimi, M.; Botelho, M.G.; Dorozhkin, S.V. Biphasic Calcium Phosphates Bioceramics (HA/TCP): Concept, Physicochemical Properties and the Impact of Standardization of Study Protocols in Biomaterials Research. Mater. Sci. Eng. C 2017, 71, 1293–1312. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Huang, X.; Wang, C.; Dang, X.; Wang, K. Repair of Bone Defects Using a New Biomimetic Construction Fabricated by Adipose-Derived Stem Cells, Collagen I, and Porous Beta-Tricalcium Phosphate Scaffolds. Exp. Biol. Med. 2013, 238, 1331–1343. [Google Scholar] [CrossRef]
- Manjubala, I.; Sastry, T.P.; Kumar, R.V.S. Bone In-Growth Induced by Biphasic Calcium Phosphate Ceramic in Femoral Defect of Dogs. J. Biomater. Appl. 2005, 19, 341–360. [Google Scholar] [CrossRef] [PubMed]
- Puttini, I.; Poli, P.; Maiorana, C.; Vasconcelos, I.; Schmidt, L.; Colombo, L.; Hadad, H.; Santos, G.; Carvalho, P.; Souza, F. Evaluation of Osteoconduction of Biphasic Calcium Phosphate Ceramic in the Calvaria of Rats: Microscopic and Histometric Analysis. J. Funct. Biomater. 2019, 10, 7. [Google Scholar] [CrossRef] [PubMed]
- D’Arros, C.; Rouillon, T.; Veziers, J.; Malard, O.; Borget, P.; Daculsi, G. Bioactivity of Biphasic Calcium Phosphate Granules, the Control of a Needle-like Apatite Layer Formation for Further Medical Device Developments. Front. Bioeng. Biotechnol. 2020, 7, 426. [Google Scholar] [CrossRef]
- Wang, W.; Yeung, K.W.K. Bone Grafts and Biomaterials Substitutes for Bone Defect Repair: A Review. Bioact. Mater. 2017, 2, 224–247. [Google Scholar] [CrossRef]
- Cao, H.; Kuboyama, N. A Biodegradable Porous Composite Scaffold of PGA/β-TCP for Bone Tissue Engineering. Bone 2010, 46, 386–395. [Google Scholar] [CrossRef]
- Cacciotti, I. Cationic and Anionic Substitutions in Hydroxyapatite. In Handbook of Bioceramics and Biocomposites; Antoniac, I.V., Ed.; Springer International Publishing: Cham, Switzerland, 2015; pp. 1–68. ISBN 978-3-319-09230-0. [Google Scholar]
- Tite, T.; Popa, A.C.; Balescu, L.M.; Bogdan, I.M.; Pasuk, I.; Ferreira, J.M.F.; Stan, G.E. Cationic Substitutions in Hydroxyapatite: Current Status of the Derived Biofunctional Effects and Their in Vitro Interrogation Methods. Materials 2018, 11, 2081. [Google Scholar] [CrossRef]
- Singh, R.K.; Awasthi, S.; Dhayalan, A.; Ferreira, J.M.F.; Kannan, S. Deposition, Structure, Physical and Invitro Characteristics of Ag-Doped β-Ca3(PO4)2/Chitosan Hybrid Composite Coatings on Titanium Metal. Mater. Sci. Eng. C 2016, 62, 692–701. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, J.H.; Shepherd, D.V.; Best, S.M. Substituted Hydroxyapatites for Bone Repair. J. Mater. Sci. Mater. Med. 2012, 23, 2335–2347. [Google Scholar] [CrossRef] [PubMed]
- Bose, S.; Fielding, G.; Tarafder, S.; Bandyopadhyay, A. Understanding of Dopant-Induced Osteogenesis and Angiogenesis in Calcium Phosphate Ceramics. Trends Biotechnol. 2013, 31, 594–605. [Google Scholar] [CrossRef] [PubMed]
- Perez, R.A.; Seo, S.J.; Won, J.E.; Lee, E.J.; Jang, J.H.; Knowles, J.C.; Kim, H.W. Therapeutically Relevant Aspects in Bone Repair and Regeneration. Mater. Today 2015, 18, 573–589. [Google Scholar] [CrossRef]
- Wu, C.; Chang, J. Multifunctional Mesoporous Bioactive Glasses for Effective Delivery of Therapeutic Ions and Drug/Growth Factors. J. Control. Release 2014, 193, 282–295. [Google Scholar] [CrossRef]
- Ren, X.; Zhao, M.; Lash, B.; Martino, M.M.; Julier, Z. Growth Factor Engineering Strategies for Regenerative Medicine Applications. Front. Bioeng. Biotechnol. 2020, 7, 469. [Google Scholar] [CrossRef]
- Mitchell, A.C.; Briquez, P.S.; Hubbell, J.A.; Cochran, J.R. Engineering Growth Factors for Regenerative Medicine Applications. Acta Biomater. 2016, 30, 1–12. [Google Scholar] [CrossRef]
- Andrés, N.C.; Sieben, J.M.; Baldini, M.; Rodríguez, C.H.; Famiglietti, Á.; Messina, P.V. Electroactive Mg2+-Hydroxyapatite Nanostructured Networks against Drug-Resistant Bone Infection Strains. ACS Appl. Mater. Interfaces 2018, 10, 19534–19544. [Google Scholar] [CrossRef]
- Lai, Y.; Li, Y.; Cao, H.; Long, J.; Wang, X.; Li, L.; Li, C.; Jia, Q.; Teng, B.; Tang, T.; et al. Osteogenic Magnesium Incorporated into PLGA/TCP Porous Scaffold by 3D Printing for Repairing Challenging Bone Defect. Biomaterials 2019, 197, 207–219. [Google Scholar] [CrossRef]
- Zhu, T.; Cui, Y.; Zhang, M.; Zhao, D.; Liu, G.; Ding, J. Engineered Three-Dimensional Scaffolds for Enhanced Bone Regeneration in Osteonecrosis. Bioact. Mater. 2020, 5, 584–601. [Google Scholar] [CrossRef]
- Özbek, Y.Y.; Baştan, F.E.; Üstel, F. Synthesis and Characterization of Strontium-Doped Hydroxyapatite for Biomedical Applications. J. Therm. Anal. Calorim. 2016, 125, 745–750. [Google Scholar] [CrossRef]
- Landi, E.; Tampieri, A.; Celotti, G.; Sprio, S.; Sandri, M.; Logroscino, G. Sr-Substituted Hydroxyapatites for Osteoporotic Bone Replacement. Acta Biomater. 2007, 3, 961–969. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, Q.; Zhu, S.; Luo, E.; Li, J.; Feng, G.; Liao, Y.; Hu, J. The Effect of Strontium-Substituted Hydroxyapatite Coating on Implant Fixation in Ovariectomized Rats. Biomaterials 2010, 31, 9006–9014. [Google Scholar] [CrossRef]
- Guida, A.; Towler, M.R.; Wall, J.G.; Hill, R.G.; Eramo, S. Preliminary Work on the Antibacterial Effect of Strontium in Glass Ionomer Cements. J. Mater. Sci. Lett. 2003, 22, 1401–1403. [Google Scholar] [CrossRef]
- Baheiraei, N.; Eyni, H.; Bakhshi, B.; Najafloo, R.; Rabiee, N. Effects of Strontium Ions with Potential Antibacterial Activity on in Vivo Bone Regeneration. Sci. Rep. 2021, 11, 8745. [Google Scholar] [CrossRef] [PubMed]
- Popa, A.C.; Fernandes, H.R.; Necsulescu, M.; Luculescu, C.; Cioangher, M.; Dumitru, V.; Stuart, B.W.; Grant, D.M.; Ferreira, J.M.F.; Stan, G.E. Antibacterial Efficiency of Alkali-Free Bio-Glasses Incorporating ZnO and/or SrO as Therapeutic Agents. Ceram. Int. 2019, 45, 4368–4380. [Google Scholar] [CrossRef]
- Furko, M.; Havasi, V.; Kónya, Z.; Grünewald, A.; Detsch, R.; Boccaccini, A.R.; Balázsi, C. Development and Characterization of Multi-Element Doped Hydroxyapatite Bioceramic Coatings on Metallic Implants for Orthopedic Applications. Bol. Soc. Esp. Ceram. Vidr. 2018, 57, 55–65. [Google Scholar] [CrossRef]
- Bigi, A.; Boanini, E.; Capuccini, C.; Gazzano, M. Strontium-Substituted Hydroxyapatite Nanocrystals. Inorg. Chim. Acta 2007, 360, 1009–1016. [Google Scholar] [CrossRef]
- Xue, W.; Hosick, H.L.; Bandyopadhyay, A.; Bose, S.; Ding, C.; Luk, K.D.K.; Cheung, K.M.C.; Lu, W.W. Preparation and Cell–Materials Interactions of Plasma Sprayed Strontium-Containing Hydroxyapatite Coating. Surf. Coat. Technol. 2007, 201, 4685–4693. [Google Scholar] [CrossRef]
- Vukomanovic, M.; Gazvoda, L.; Anicic, N.; Rubert, M.; Suvorov, D.; Müller, R.; Hofmann, S. Multi-Doped Apatite: Strontium, Magnesium, Gallium and Zinc Ions Synergistically Affect Osteogenic Stimulation in Human Mesenchymal Cells Important for Bone Tissue Engineering. Biomater. Adv. 2022, 140, 213051. [Google Scholar] [CrossRef]
- Ressler, A.; Antunović, M.; Teruel-Biosca, L.; Ferrer, G.G.; Babić, S.; Urlić, I.; Ivanković, M.; Ivanković, H. Osteogenic Differentiation of Human Mesenchymal Stem Cells on Substituted Calcium Phosphate/Chitosan Composite Scaffold. Carbohydr. Polym. 2022, 277, 118883. [Google Scholar] [CrossRef] [PubMed]
- Neto, A.S.; Ferreira, J.M.F. Doped Calcium Phosphate Scaffolds Obtained by Robocasting from Hydrothermally Synthesized Powders. AdvNanoBioMD 2018, 2, 301–315. [Google Scholar]
- Kannan, S.; Pina, S.; Ferreira, J.M.F. Formation of Strontium-Stabilized β-Tricalcium Phosphate from Calcium-Deficient Apatite. J. Am. Ceram. Soc. 2006, 89, 3277–3280. [Google Scholar] [CrossRef]
- Kannan, S.; Goetz-Neunhoeffer, F.; Neubauer, J.; Ferreira, J.M.F. Ionic Substitutions in Biphasic Hydroxyapatite and β-Tricalcium Phosphate Mixtures: Structural Analysis by Rietveld Refinement. J. Am. Ceram. Soc. 2008, 91, 1–12. [Google Scholar] [CrossRef]
- Kannan, S.; Goetz-Neunhoeffer, F.; Neubauer, J.; Pina, S.; Torres, P.M.C.; Ferreira, J.M.F. Synthesis and Structural Characterization of Strontium- and Magnesium-Co-Substituted β-Tricalcium Phosphate. Acta Biomater. 2010, 6, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Torres, P.M.C.; Abrantes, J.C.C.; Kaushal, A.; Pina, S.; Döbelin, N.; Bohner, M.; Ferreira, J.M.F. Influence of Mg-Doping, Calcium Pyrophosphate Impurities and Cooling Rate on the Allotropic A↔β-Tricalcium Phosphate Phase Transformations. J. Eur. Ceram. Soc. 2016, 36, 817–827. [Google Scholar] [CrossRef]
- Bigi, A.; Foresti, E.; Gregorini, R.; Ripamonti, A.; Roveri, N.; Shah, J.S. The Role of Magnesium on the Structure of Biological Apatites. Calcif. Tissue Int. 1992, 50, 439–444. [Google Scholar] [CrossRef]
- Combes, C.; Cazalbou, S.; Rey, C. Apatite Biominerals. Minerals 2016, 6, 34. [Google Scholar] [CrossRef]
- Wallach, S. Effects of Magnesium on Skeletal Metabolism. Magnes. Trace Elem. 1990, 9, 1–14. [Google Scholar]
- Caverzasio, J. Strontium Ranelate Promotes Osteoblastic Cell Replication through at Least Two Different Mechanisms. Bone 2008, 42, 1131–1136. [Google Scholar] [CrossRef]
- Klontzas, M.E.; Kenanidis, E.I.; MacFarlane, R.J.; Michail, T.; Potoupnis, M.E.; Heliotis, M.; Mantalaris, A.; Tsiridis, E. Investigational Drugs for Fracture Healing: Preclinical & Clinical Data. Expert Opin. Investig. Drugs 2016, 25, 585–596. [Google Scholar] [CrossRef] [PubMed]
- Prakasam, M.; Chirazi, A.; Pyka, G.; Prokhodtseva, A.; Lichau, D.; Largeteau, A. Fabrication and Multiscale Structural Properties of Interconnected Porous Biomaterial for Tissue Engineering by Freeze Isostatic Pressure (FIP). J. Funct. Biomater. 2018, 9, 51. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, N.; Hamlet, S.; Love, R.M.; Nguyen, N.-T. Porous Scaffolds for Bone Regeneration. J. Sci. Adv. Mater. Dev. 2020, 5, 1–9. [Google Scholar] [CrossRef]
- Walthers, C.M.; Nazemi, A.K.; Patel, S.L.; Wu, B.M.; Dunn, J.C.Y. The Effect of Scaffold Macroporosity on Angiogenesis and Cell Survival in Tissue-Engineered Smooth Muscle. Biomaterials 2014, 35, 5129–5137. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.R.; Crute, B.E.; Patrone, L.M.; Gabriels, J.; Lane, M.E.; Buskirk, R.G. Microporosity of the Substratum Regulates Differentiation of MDCK Cells in Vitro. In Vitro Cell. Dev. Biol. 1989, 25, 914–922. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Fan, Y.; Dunne, N.; Li, X. Effect of Microporosity on Scaffolds for Bone Tissue Engineering. Regen. Biomater. 2018, 5, 115–124. [Google Scholar] [CrossRef]
- Mocanu, A.C.; Miculescu, M.; Machedon-Pisu, T.; Maidaniuc, A.; Ciocoiu, R.C.; Ioniță, M.; Pasuk, I.; Stan, G.E.; Miculescu, F. Internal and External Surface Features of Newly Developed Porous Ceramics with Random Interconnected 3D Channels by a Fibrous Sacrificial Porogen Method. Appl. Surf. Sci. 2019, 489, 226–238. [Google Scholar] [CrossRef]
- Li, J.; Chong, Y.T.; Teng, C.P.; Liu, J.; Wang, F. Microporosity Mediated Proliferation of Preosteoblast Cells on 3D Printed Bone Scaffolds. Nano Sel. 2021, 2, 1997–2006. [Google Scholar] [CrossRef]
- Pecqueux, F.; Tancret, F.; Payraudeau, N.; Bouler, J.M. Influence of Microporosity and Macroporosity on the Mechanical Properties of Biphasic Calcium Phosphate Bioceramics: Modelling and Experiment. J. Eur. Ceram. Soc. 2010, 30, 819–829. [Google Scholar] [CrossRef]
- de Groot, K. Effect of Porosity and Physicochemical Properties on the Stability, Resorption, and Strength of Calcium Phosphate Ceramics. Ann. N. Y. Acad. Sci. 1988, 523, 227–233. [Google Scholar] [CrossRef]
- Bignon, A.; Chouteau, J.; Chevalier, J.; Fantozzi, G.; Carret, J.P.; Chavassieux, P.; Boivin, G.; Melin, M.; Hartmann, D. Effect of Micro- and Macroporosity of Bone Substitutes on Their Mechanical Properties and Cellular Response. J. Mater. Sci. Mater. Med. 2003, 14, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xu, H.H.K.; Takagi, S.; Chow, L.C. In-Situ Hardening Hydroxyapatite-Based Scaffold for Bone Repair. J. Mater. Sci. Mater. Med. 2006, 17, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Hing, K.A.; Annaz, B.; Saeed, S.; Revell, P.A.; Buckland, T. Microporosity Enhances Bioactivity of Synthetic Bone Graft Substitutes. J. Mater. Sci. Mater. Med. 2005, 16, 467–475. [Google Scholar] [CrossRef]
- Rosa, A.L.; Beloti, M.M.; van Noort, R. Osteoblastic Differentiation of Cultured Rat Bone Marrow Cells on Hydroxyapatite with Different Surface Topography. Dent. Mater. 2003, 19, 768–772. [Google Scholar] [CrossRef]
- Chirică, I.M.; Enciu, A.-M.; Tite, T.; Dudău, M.; Albulescu, L.; Iconaru, S.L.; Predoi, D.; Pasuk, I.; Enculescu, M.; Radu, C.; et al. The Physico-Chemical Properties and Exploratory Real-Time Cell Analysis of Hydroxyapatite Nanopowders Substituted with Ce, Mg, Sr, and Zn (0.5–5 at.%). Materials 2021, 14, 3808. [Google Scholar] [CrossRef] [PubMed]
- Markovic, M.; Fowler, B.O.; Tung, M.S. Preparation and Comprehensive Characterization of a Calcium Hydroxyapatite Reference Material. J. Res. Natl. Inst. Stand. Technol. 2004, 109, 553. [Google Scholar] [CrossRef] [PubMed]
- Jillavenkatesa, A.; Condrate, R.A. The Infrared and Raman Spectra of β-and α-Tricalcium Phosphate (Ca3 (Po4)2). Spectrosc. Lett. 1998, 31, 1619–1634. [Google Scholar] [CrossRef]
- Topsakal, A.; Ekren, N.; Kilic, O.; Oktar, F.N.; Mahirogullari, M.; Ozkan, O.; Sasmazel, H.T.; Turk, M.; Bogdan, I.M.; Stan, G.E.; et al. Synthesis and Characterization of Antibacterial Drug Loaded β-Tricalcium Phosphate Powders for Bone Engineering Applications. J. Mater. Sci. Mater. Med. 2020, 31, 16. [Google Scholar] [CrossRef]
- Mocanu, A.C.; Miculescu, F.; Stan, G.E.; Ciocoiu, R.C.; Corobea, M.C.; Miculescu, M.; Ciocan, L.T. Preliminary Studies on Graphene-Reinforced 3D Products Obtained by the One-Stage Sacrificial Template Method for Bone Reconstruction Applications. J. Funct. Biomater. 2021, 12, 13. [Google Scholar] [CrossRef]
- Fowler, B.O. Infrared Studies of Apatites. I. Vibrational Assignments for Calcium, Strontium, and Barium Hydroxyapatites Utilizing Isotopic Substitution. Inorg. Chem. 1974, 13, 194–207. [Google Scholar] [CrossRef]
- Lutterotti, L. Total Pattern Fitting for the Combined Size–Strain–Stress–Texture Determination in Thin Film Diffraction. Nucl. Instrum. Methods Phys. Res. Sect. B Beam Interact. Mater. At. 2010, 268, 334–340. [Google Scholar] [CrossRef]
- Fadeev, I.V.; Shvorneva, L.I.; Barinov, S.M.; Orlovskii, V.P. Synthesis and Structure of Magnesium-Substituted Hydroxyapatite. Inorg. Mater. 2003, 39, 947–950. [Google Scholar] [CrossRef]
- Cacciotti, I.; Bianco, A.; Lombardi, M.; Montanaro, L. Mg-Substituted Hydroxyapatite Nanopowders: Synthesis, Thermal Stability and Sintering Behaviour. J. Eur. Ceram. Soc. 2009, 29, 2969–2978. [Google Scholar] [CrossRef]
- Famery, R.; Richard, N.; Boch, P. Preparation of α- and β-Tricalcium Phosphate Ceramics, with and without Magnesium Addition. Ceram. Int. 1994, 20, 327–336. [Google Scholar] [CrossRef]
- Hughes, J.M.; Cameron, M.; Crowley, K.D. Structural Variations in Natural F, OH, and Cl Apatites. Am. Miner. 1989, 74, 870–876. [Google Scholar]
- Yashima, M.; Sakai, A.; Kamiyama, T.; Hoshikawa, A. Crystal Structure Analysis of β-Tricalcium Phosphate Ca3(PO4)2 by Neutron Powder Diffraction. J. Solid State Chem. 2003, 175, 272–277. [Google Scholar] [CrossRef]
- Matsunaga, K. First-Principles Study of Substitutional Magnesium and Zinc in Hydroxyapatite and Octacalcium Phosphate. J. Chem. Phys. 2008, 128, 245101. [Google Scholar] [CrossRef]
- Matsunaga, K.; Inamori, H.; Murata, H. Theoretical Trend of Ion Exchange Ability with Divalent Cations in Hydroxyapatite. Phys. Rev. B 2008, 78, 94101. [Google Scholar] [CrossRef]
- Ren, F.; Leng, Y.; Xin, R.; Ge, X. Synthesis, Characterization and Ab Initio Simulation of Magnesium-Substituted Hydroxyapatite. Acta Biomater. 2010, 6, 2787–2796. [Google Scholar] [CrossRef]
- Matsunaga, K.; Kubota, T.; Toyoura, K.; Nakamura, A. First-Principles Calculations of Divalent Substitution of Ca2+ in Tricalcium Phosphates. Acta Biomater. 2015, 23, 329–337. [Google Scholar] [CrossRef]
- Renaudin, G.; Jallot, E.; Nedelec, J.M. Effect of Strontium Substitution on the Composition and Microstructure of Sol–Gel Derived Calcium Phosphates. J. Sol-Gel Sci. Technol. 2009, 51, 287–294. [Google Scholar] [CrossRef]
- Boanini, E.; Gazzano, M.; Nervi, C.; Chierotti, M.R.; Rubini, K.; Gobetto, R.; Bigi, A. Strontium and Zinc Substitution in β-Tricalcium Phosphate: An X-Ray Diffraction, Solid State NMR and ATR-FTIR Study. J. Funct. Biomater. 2019, 10, 20. [Google Scholar] [CrossRef] [PubMed]





| Sample Code | Sr (at.%) | Mg (at.%) |
|---|---|---|
| BCP | 0 | 0 |
| BCP–6Sr | 6 | 0 |
| BCP–6Sr2Mg | 6 | 2 |
| Sample Code | Initial Solid Loading (vol.%) | Mass Concentration (in wt.%) of Additives * | Final Solid Loading (vol. %) | ||
|---|---|---|---|---|---|
| Dispersant (35 wt.% aq. Sol.) | Binder (33 wt.% aq. Sol.) | Coagulant (10 wt.% aq. Sol.) | |||
| BCP | ~53.9 | 0.57 | 2.00 | 0.04 | ~50.8 |
| BCP—6Sr | ~54.8 | 0.40 | 2.00 | 0.07 | ~51.4 |
| BCP—6Sr2Mg | ~57.8 | 0.38 | 2.00 | 0.05 | ~54.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Besleaga, C.; Nan, B.; Popa, A.-C.; Balescu, L.M.; Nedelcu, L.; Neto, A.S.; Pasuk, I.; Leonat, L.; Popescu-Pelin, G.; Ferreira, J.M.F.; et al. Sr and Mg Doped Bi-Phasic Calcium Phosphate Macroporous Bone Graft Substitutes Fabricated by Robocasting: A Structural and Cytocompatibility Assessment. J. Funct. Biomater. 2022, 13, 123. https://doi.org/10.3390/jfb13030123
Besleaga C, Nan B, Popa A-C, Balescu LM, Nedelcu L, Neto AS, Pasuk I, Leonat L, Popescu-Pelin G, Ferreira JMF, et al. Sr and Mg Doped Bi-Phasic Calcium Phosphate Macroporous Bone Graft Substitutes Fabricated by Robocasting: A Structural and Cytocompatibility Assessment. Journal of Functional Biomaterials. 2022; 13(3):123. https://doi.org/10.3390/jfb13030123
Chicago/Turabian StyleBesleaga, Cristina, Bo Nan, Adrian-Claudiu Popa, Liliana Marinela Balescu, Liviu Nedelcu, Ana Sofia Neto, Iuliana Pasuk, Lucia Leonat, Gianina Popescu-Pelin, José M. F. Ferreira, and et al. 2022. "Sr and Mg Doped Bi-Phasic Calcium Phosphate Macroporous Bone Graft Substitutes Fabricated by Robocasting: A Structural and Cytocompatibility Assessment" Journal of Functional Biomaterials 13, no. 3: 123. https://doi.org/10.3390/jfb13030123
APA StyleBesleaga, C., Nan, B., Popa, A.-C., Balescu, L. M., Nedelcu, L., Neto, A. S., Pasuk, I., Leonat, L., Popescu-Pelin, G., Ferreira, J. M. F., & Stan, G. E. (2022). Sr and Mg Doped Bi-Phasic Calcium Phosphate Macroporous Bone Graft Substitutes Fabricated by Robocasting: A Structural and Cytocompatibility Assessment. Journal of Functional Biomaterials, 13(3), 123. https://doi.org/10.3390/jfb13030123