AFM Analysis of a Three-Point Flexure Tested, 3D Printing Definitive Restoration Material for Dentistry
Abstract
:1. Introduction
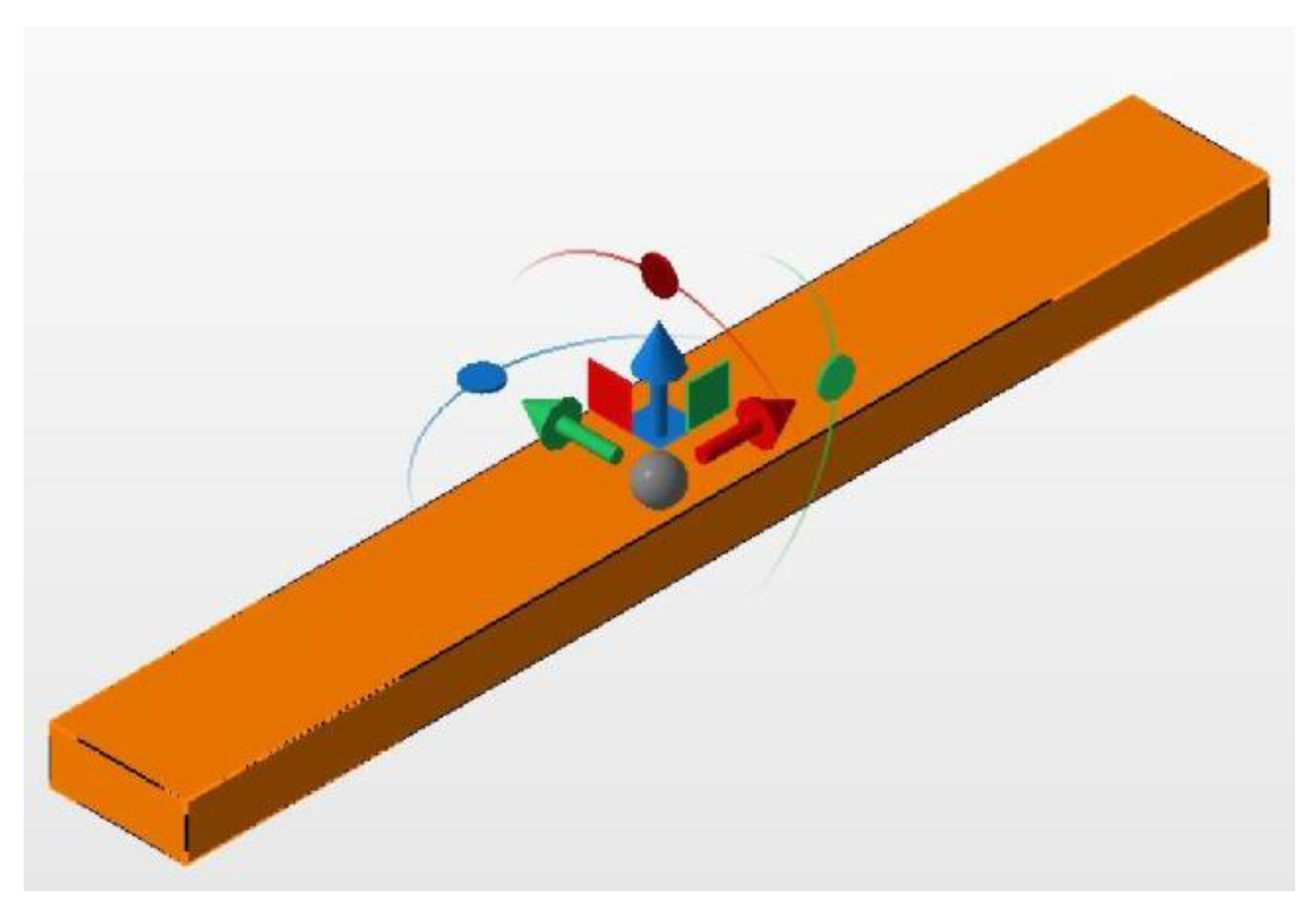
2. Materials and Methods
3. Results
3.1. Surface Roughness of Regions 1–4
3.2. Surface Roughness of Segments 1–9 Obtained from Region 1
3.3. Statistical Evaluation
4. Discussion
5. Conclusions
- Increased surface roughness after plastic deformation;
- Higher roughness than conventional materials, but still clinically acceptable before and after flexure testing;
- AFM surface analysis is suitable for investigating surface changes in 3D printed dental materials.
- Significance of printing direction and its impact on the properties of 3D printed objects produced from VarseoSmile Crown plus;
- Creation of an optimized and standardized procedure to reach plastic deformation in 3D printed dental materials;
- Reduced distance between measurement regions to see how much of the workpiece is affected;
- Impact of fillers in surface changes in the bending procedure;
- Clinical consequences of the measured increase in surface roughness and its clinical effects in combination with VarseoSmile Crown plus;
- Material changes in vivo.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Whitaker, M. The history of 3D printing in healthcare. Bull. R. Coll. Surg. Engl. 2014, 96, 228–229. [Google Scholar] [CrossRef]
- Savini, A.; Savini, G. A short history of 3D printing, a technological revolution just started. In Proceedings of the 2015 ICOHTEC/IEEE International History Of High-Technologies and Their Socio-Cultural Contexts Conference (HISTELCON), Tel-Aviv, Israel, 18–19 August 2015; pp. 1–8. [Google Scholar]
- Shahrubudin, N.; Lee, T.C.; Ramlan, R. An overview on 3D printing technology: Technological, materials, and applications. Procedia Manuf. 2019, 35, 1286–1296. [Google Scholar] [CrossRef]
- Xu, D.; Shi, J.; Qiu, R.; Lei, W.; Yu, W. Comparative Investigations on Properties of Three Kinds of FDM 3D-Printed Natural Plant Powder/Poly(lactic acid) Biocomposites. Polymers 2023, 15, 557. [Google Scholar] [CrossRef] [PubMed]
- Selema, A.; Ibrahim, M.N.; Sergeant, P. Metal additive manufacturing for electrical machines: Technology review and latest advancements. Energies 2022, 15, 1076. [Google Scholar] [CrossRef]
- Pilipović, A. Sheet lamination. In Polymers for 3D Printing; Elsevier: Amsterdam, The Netherlands, 2022; pp. 127–136. [Google Scholar]
- Aimar, A.; Palermo, A.; Innocenti, B. The role of 3D printing in medical applications: A state of the art. J. Healthc. Eng. 2019, 2019, 5340616. [Google Scholar] [CrossRef] [Green Version]
- Panja, N.; Maji, S.; Choudhuri, S.; Ali, K.A.; Hossain, C.M. 3D bioprinting of human hollow organs. AAPS PharmSciTech 2022, 23, 139. [Google Scholar] [CrossRef]
- Uboldi, M.; Perrotta, C.; Moscheni, C.; Zecchini, S.; Napoli, A.; Castiglioni, C.; Gazzaniga, A.; Melocchi, A.; Zema, L. Insights into the Safety and Versatility of 4D Printed Intravesical Drug Delivery Systems. Pharmaceutics 2023, 15, 757. [Google Scholar] [CrossRef]
- Tomohisa, O.; Kamio, T.; Maeda, Y.; Tsubosaki, K.; Kato, T.; Iwata, H. Application of Medical Imaging and 3D Printing Technology in Teaching the Handling of Novel Medicine in Periodontal Surgery. Cureus 2022, 14, e29271. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3D printing in digital prosthetic dentistry: An overview of recent developments in additive manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef]
- Li, Z.; Wang, Q.; Liu, G. A Review of 3D Printed Bone Implants. Micromachines 2022, 13, 528. [Google Scholar] [CrossRef]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Prasad, S.; Kader, N.A.; Sujatha, G.; Raj, T.; Patil, S. 3D printing in dentistry. Future Med. 2018, 2, 89–91. [Google Scholar] [CrossRef]
- Anadioti, E.; Musharbash, L.; Blatz, M.B.; Papavasiliou, G.; Kamposiora, P. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health 2020, 20, 343. [Google Scholar] [CrossRef]
- Turkyilmaz, I.; Wilkins, G.N. 3D printing in dentistry–exploring the new horizons. J. Dent. Sci. 2021, 16, 1037. [Google Scholar] [CrossRef]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef]
- Nesic, D.; Schaefer, B.M.; Sun, Y.; Saulacic, N.; Sailer, I. 3D printing approach in dentistry: The future for personalized oral soft tissue regeneration. J. Clin. Med. 2020, 9, 2238. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.-S.; Jiang, H.B. A review of 3D printing in dentistry: Technologies, affecting factors, and applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef]
- Arnetzl, G.; Arnetzl, G. CAD/CAM-Systeme. Stomatologie 2013, 110, 10–18. [Google Scholar] [CrossRef]
- Baroudi, K.; Ibraheem, S.N. Assessment of chair-side computer-aided design and computer-aided manufacturing restorations: A review of the literature. J. Int. Oral Health JIOH 2015, 7, 96. [Google Scholar]
- Bego. Scientific Studies on VarseoSmile Crown Plus. Available online: https://www.bego.com/3d-printing/materials/varseosmile-crown-plus/scientific-studies/ (accessed on 5 July 2022).
- Bego. VarseoSmile Temp. Available online: https://www.bego.com/3d-printing/materials/varseosmile-temp/ (accessed on 5 July 2022).
- Koletsi, D.; Iliadi, A.; Eliades, T.; Eliades, G. In vitro simulation and in vivo assessment of tooth wear: A meta-analysis of in vitro and clinical research. Materials 2019, 12, 3575. [Google Scholar] [CrossRef] [Green Version]
- Batak, B.; Çakmak, G.; Johnston, W.M.; Yilmaz, B. Surface roughness of high-performance polymers used for fixed implant-supported prostheses. J. Prosthet. Dent. 2021, 126, 254.e1–254.e6. [Google Scholar] [CrossRef] [PubMed]
- Shembish, F.A.; Tong, H.; Kaizer, M.; Janal, M.N.; Thompson, V.P.; Opdam, N.J.; Zhang, Y. Fatigue resistance of CAD/CAM resin composite molar crowns. Dent. Mater. 2016, 32, 499–509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gwyddion. Gwyddion. Available online: http://gwyddion.net/ (accessed on 5 July 2022).
- Nečas, D.; Klapetek, P. Gwyddion: An open-source software for SPM data analysis. Open Phys. 2012, 10, 181–188. [Google Scholar] [CrossRef]
- Nold, J.; Wesemann, C.; Rieg, L.; Binder, L.; Witkowski, S.; Spies, B.C.; Kohal, R.J. Does printing orientation matter? In-vitro fracture strength of temporary fixed dental prostheses after a 1-year simulation in the artificial mouth. Materials 2021, 14, 259. [Google Scholar] [CrossRef]
- Mahalaxmi, S. Materials Used in Dentistry; Wolters Kluwer India Private Ltd.: Chandigarh, India, 2013. [Google Scholar]
- de Jager, N.; Münker, T.J.; Guilardi, L.F.; Jansen, V.J.; Sportel, Y.G.; Kleverlaan, C.J. The relation between impact strength and flexural strength of dental materials. J. Mech. Behav. Biomed. Mater. 2021, 122, 104658. [Google Scholar] [CrossRef]
- Mulliken, A.D.; Boyce, M.C. Mechanics of the rate-dependent elastic–plastic deformation of glassy polymers from low to high strain rates. Int. J. Solids Struct. 2006, 43, 1331–1356. [Google Scholar] [CrossRef] [Green Version]
- Cahn, R.W.; Mughrabi, H.; Haasen, P.; Kramer, E.J. Materials Science and Technology: Plastic Deformation and Fracture of Materials; VCH: Hoboken, NJ, USA, 1993. [Google Scholar]
- BEGO. VarseoSmile Crown Plus: Gebrauchsanweisung. Available online: https://www.bego.com/fileadmin/user_downloads/Mediathek/3D-Druck/Materialien/DE_Gebrauchsanweisungen/VarseoSmileCrown-plus/de_20740_0002_ga_de.pdf (accessed on 15 March 2021).
- Lubliner, J. Plasticity Theory; Courier Corporation: Chelmsford, MA, USA, 2008. [Google Scholar]
- Instruments, O. AFM: Exploring Tapping Mode and AM-FM. Available online: https://afm.oxinst.com/outreach/tapping-mode-for-afm-am-fm (accessed on 14 November 2022).
- AG, N. How Does AFM Work? Available online: https://www.nanosurf.com/en/support/afm-operating-principle (accessed on 14 November 2022).
- Burgo, T.L.; Pereira, G.K.R.; Iglesias, B.A.; Moreira, K.S.; Valandro, L.F. AFM advanced modes for dental and biomedical applications. J. Mech. Behav. Biomed. Mater. 2022, 136, 105475. [Google Scholar] [CrossRef]
- Olmos-Olmos, G.; Teutle-Coyotecatl, B.; Román-Mendez, C.D.; Carrasco-Gutiérrez, R.; González-Torres, M.; Contreras-Bulnes, R.; Rodríguez-Vilchis, L.E.; de los Angeles Moyaho-Bernal, M. The influence of light-curing time on fluoride release, surface topography, and bacterial adhesion in resin-modified glass ionomer cements: AFM and SEM in vitro study. Microsc. Res. Tech. 2021, 84, 1628–1637. [Google Scholar] [CrossRef]
- Toledano, M.; Osorio, E.; Aguilera, F.S.; Muñoz-Soto, E.; Toledano-Osorio, M.; López-López, M.T.; Medina-Castillo, A.L.; Carrasco-Carmona, Á.; Osorio, R. Polymeric nanoparticles for endodontic therapy. J. Mech. Behav. Biomed. Mater. 2020, 103, 103606. [Google Scholar] [CrossRef]
- Lee, Y.-L.; Li, K.; Yiu, C.; Boyd, D.; Ekambaram, M. Evaluation of developmentally hypomineralised enamel after surface pretreatment with Papacarie Duo gel and different etching modes: An in vitro SEM and AFM study. Eur. Arch. Paediatr. Dent. 2021, 23, 117–131. [Google Scholar] [CrossRef]
- Connelly, J.T.; Gavara, N.; Sliogeryte, K.; Blowes, L.M. Research techniques made simple: Analysis of skin cell and tissue mechanics using atomic force microscopy. J. Investig. Dermatol. 2021, 141, 1867–1871.e1. [Google Scholar] [CrossRef]
- Sorozini, M.; dos Reis Perez, C.; Rocha, G.M. Enamel sample preparation for AFM: Influence on roughness and morphology. Microsc. Res. Tech. 2018, 81, 1071–1076. [Google Scholar] [CrossRef]
- Giessibl, F.J. Advances in atomic force microscopy. Rev. Mod. Phys. 2003, 75, 949. [Google Scholar] [CrossRef] [Green Version]
- Alharbi, N.; Teerakanok, S.; Satterthwaite, J.D.; Giordano, R.; Silikas, N. Quantitative nano-mechanical mapping AFM-based method for elastic modulus and surface roughness measurements of model polymer infiltrated ceramics. Dent. Mater. 2022, 38, 935–945. [Google Scholar] [CrossRef]
- Amdjadi, P.; Ghasemi, A.; Najafi, F.; Nojehdehian, H. Pivotal role of filler/matrix interface in dental composites. Biomed. Res. 2017, 28, 1054–1065. [Google Scholar]
- Rastelli, A.N.; Jacomassi, D.P.; Faloni, A.P.S.; Queiroz, T.P.; Rojas, S.S.; Bernardi, M.I.B.; Bagnato, V.S.; Hernandes, A.C. The filler content of the dental composite resins and their influence on different properties. Microsc. Res. Tech. 2012, 75, 758–765. [Google Scholar] [CrossRef]
- Zimmerli, B.; Strub, M.; Jeger, F.; Stadler, O.; Lussi, A. Composite materials: Composition, properties and clinical applications. A literature review. Schweiz. Mon. Zahnmed. Rev. Mens. Suisse D’odonto-Stomatol. Riv. Mens. Svizz. Odontol. Stomatol. 2010, 120, 972–986. [Google Scholar]
- Keshavamurthy, R.; Tambrallimath, V.; Rajhi, A.A.; Ahmed, R.M.S.; Patil, A.Y.; Yunus Khan, T.M.; Makannavar, R. Influence of Solid Lubricant Addition on Friction and Wear Response of 3D Printed Polymer Composites. Polymers 2021, 13, 2905. [Google Scholar] [CrossRef]
- Arun, Y.P.; Akash, N.; Bhavik, V.; Rahul, K.; Banapurmath, N.; Roseline, M.; Lekha, K.; Shridhar, N.M. Next Generation Material for Denture Teeth and Denture Base Material: Limpet Teeth (LT) as an Alternative Reinforcement in Polymethylmethacrylate (PMMA). J. Nano Electron. Phys. 2021, 13, 02033. [Google Scholar]
- Auschill, T.M.; Arweiler, N.B.; Brecx, M.; Reich, E.; Sculean, A.; Netuschil, L. The effect of dental restorative materials on dental biofilm. Eur. J. Oral Sci. 2002, 110, 48–53. [Google Scholar] [CrossRef]
- Bollen, C.M.; Papaioanno, W.; Van Eldere, J.; Schepers, E.; Quirynen, M.; Van Steenberghe, D. The influence of abutment surface roughness on plaque accumulation and peri-implant mucositis. Clin. Oral Implant. Res. 1996, 7, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Bürgers, R.; Cariaga, T.; Müller, R.; Rosentritt, M.; Reischl, U.; Handel, G.; Hahnel, S. Effects of aging on surface properties and adhesion of Streptococcus mutans on various fissure sealants. Clin. Oral Investig. 2009, 13, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Bürgers, R.; Gerlach, T.; Hahnel, S.; Schwarz, F.; Handel, G.; Gosau, M. In vivo and in vitro biofilm formation on two different titanium implant surfaces. Clin. Oral Implant. Res. 2010, 21, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Carlen, A.; Nikdel, K.; Wennerberg, A.; Holmberg, K.; Olsson, J. Surface characteristics and in vitro biofilm formation on glass ionomer and composite resin. Biomaterials 2001, 22, 481–487. [Google Scholar] [CrossRef]
- Hahnel, S.; Rosentritt, M.; Bürgers, R.; Handel, G. Adhesion of Streptococcus mutans NCTC 10449 to artificial teeth: An in vitro study. J. Prosthet. Dent. 2008, 100, 309–315. [Google Scholar] [CrossRef]
- Hahnel, S.; Wieser, A.; Lang, R.; Rosentritt, M. Biofilm formation on the surface of modern implant abutment materials. Clin. Oral Implant. Res. 2015, 26, 1297–1301. [Google Scholar] [CrossRef]
- Ionescu, A.; Wutscher, E.; Brambilla, E.; Schneider-Feyrer, S.; Giessibl, F.J.; Hahnel, S. Influence of surface properties of resin-based composites on in vitro Streptococcus mutans biofilm development. Eur. J. Oral Sci. 2012, 120, 458–465. [Google Scholar] [CrossRef]
- Kawai, K.; Urano, M.; Ebisu, S. Effect of surface roughness of porcelain on adhesion of bacteria and their synthesizing glucans. J. Prosthet. Dent. 2000, 83, 664–667. [Google Scholar] [CrossRef]
- Teranaka, A.; Tomiyama, K.; Ohashi, K.; Miyake, K.; Shimizu, T.; Hamada, N.; Mukai, Y.; Hirayama, S.; Nihei, T. Relevance of surface characteristics in the adhesiveness of polymicrobial biofilms to crown restoration materials. J. Oral Sci. 2017, 60, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; He, S.; Wu, X.; Liang, S.; Mu, Z.; Wei, J.; Deng, F.; Deng, Y.; Wei, S. Polyetheretherketone/nano-fluorohydroxyapatite composite with antimicrobial activity and osseointegration properties. Biomaterials 2014, 35, 6758–6775. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, H.; Deng, Y.; Luo, Z.; Liu, X.; Wei, S. Study of oral microbial adhesion and biofilm formation on the surface of nano-fluorohydroxyapatite/polyetheretherketone composite. Zhonghua Kou Qiang Yi Xue Za Zhi Zhonghua Kouqiang Yixue Zazhi Chin. J. Stomatol. 2015, 50, 378–382. [Google Scholar]
- Heimer, S.; Schmidlin, P.R.; Roos, M.; Stawarczyk, B. Surface properties of polyetheretherketone after different laboratory and chairside polishing protocols. J. Prosthet. Dent. 2017, 117, 419–425. [Google Scholar] [CrossRef] [Green Version]
- Braem, M.; Finger, W.; Van Doren, V.; Lambrechts, P.; Vanherle, G. Mechanical properties and filler fraction of dental composites. Dent. Mater. 1989, 5, 346–349. [Google Scholar] [CrossRef]
- Germain, H.S.; Swartz, M.; Phillips, R.; Moore, B.; Roberts, T. Properties of microfilled composite resins as influenced by filler content. J. Dent. Res. 1985, 64, 155–160. [Google Scholar] [CrossRef]
- Hondrum, S.O.; Fernandez, R., Jr. Contouring, finishing, and polishing Class 5 restorative materials. Oper. Dent. 1997, 22, 30–36. [Google Scholar]
- Oh, W.-S.; DeLong, R.; Anusavice, K.J. Factors affecting enamel and ceramic wear: A literature review. J. Prosthet. Dent. 2002, 87, 451–459. [Google Scholar] [CrossRef]











Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sandmair, M.N.; Kleber, C.; Ströbele, D.A.; von See, C. AFM Analysis of a Three-Point Flexure Tested, 3D Printing Definitive Restoration Material for Dentistry. J. Funct. Biomater. 2023, 14, 152. https://doi.org/10.3390/jfb14030152
Sandmair MN, Kleber C, Ströbele DA, von See C. AFM Analysis of a Three-Point Flexure Tested, 3D Printing Definitive Restoration Material for Dentistry. Journal of Functional Biomaterials. 2023; 14(3):152. https://doi.org/10.3390/jfb14030152
Chicago/Turabian StyleSandmair, Maximilian N., Christoph Kleber, Dragan A. Ströbele, and Constantin von See. 2023. "AFM Analysis of a Three-Point Flexure Tested, 3D Printing Definitive Restoration Material for Dentistry" Journal of Functional Biomaterials 14, no. 3: 152. https://doi.org/10.3390/jfb14030152
APA StyleSandmair, M. N., Kleber, C., Ströbele, D. A., & von See, C. (2023). AFM Analysis of a Three-Point Flexure Tested, 3D Printing Definitive Restoration Material for Dentistry. Journal of Functional Biomaterials, 14(3), 152. https://doi.org/10.3390/jfb14030152






