Crack Propagation and Fatigue Performance of Partial Posterior Indirect Restorations: An Extended Finite Element Method Study
Abstract
:1. Introduction
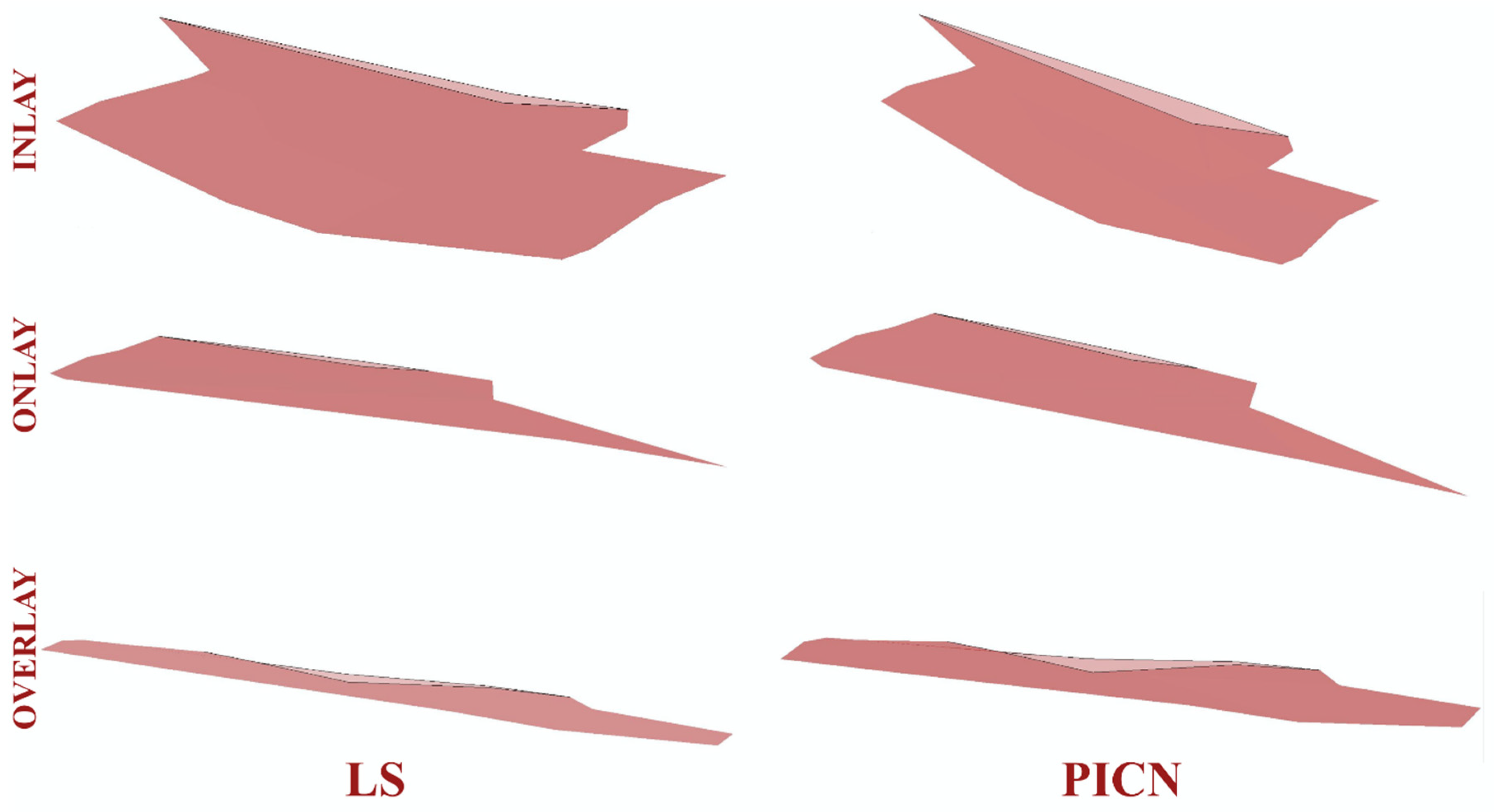
2. Materials and Methods
2.1. Finite Element Modeling
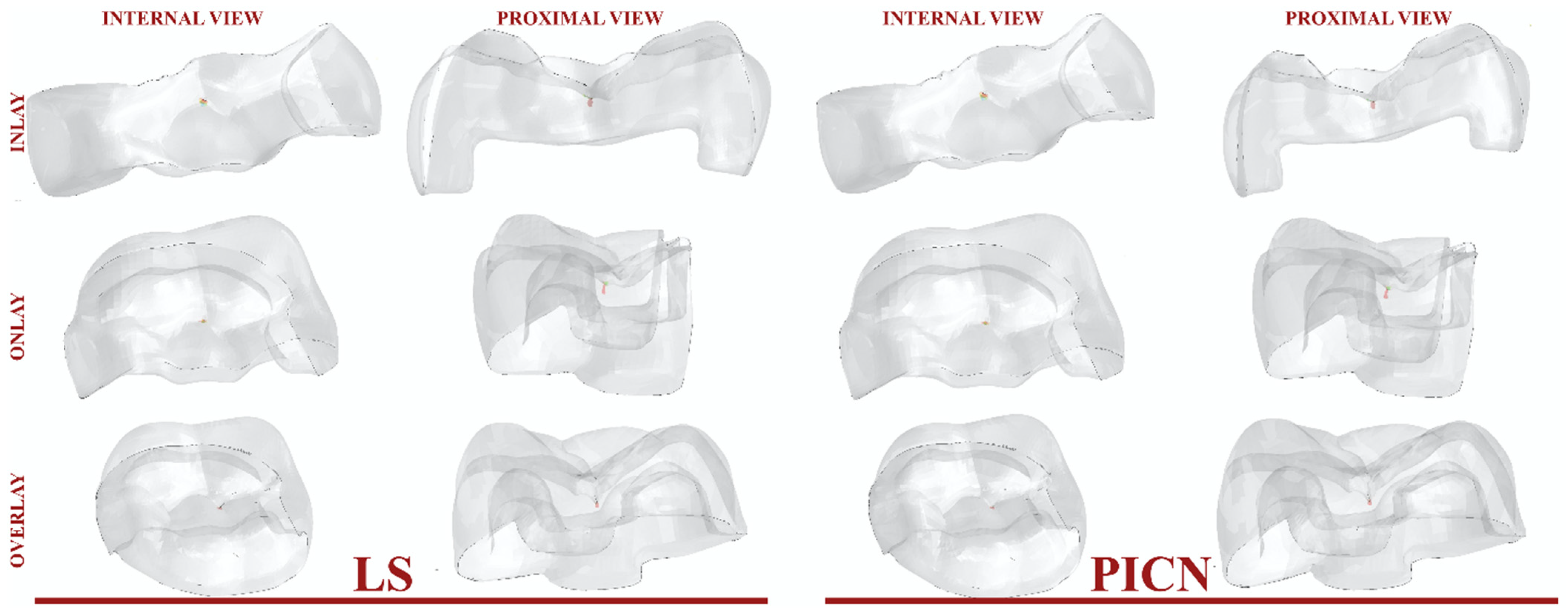
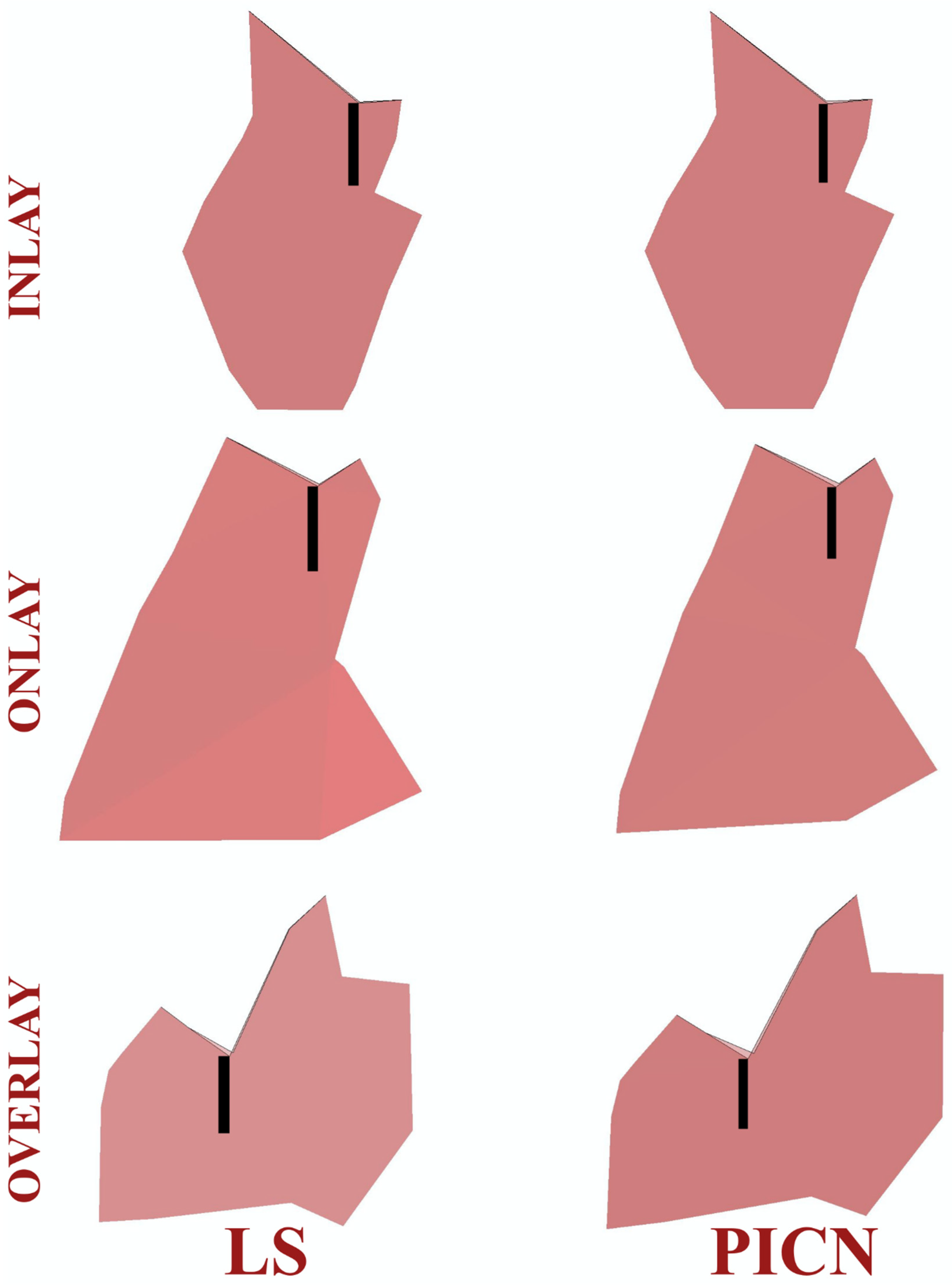
2.2. An Extended Finite Element (XFEM) Analysis
2.3. Calculation of Fatigue Performance
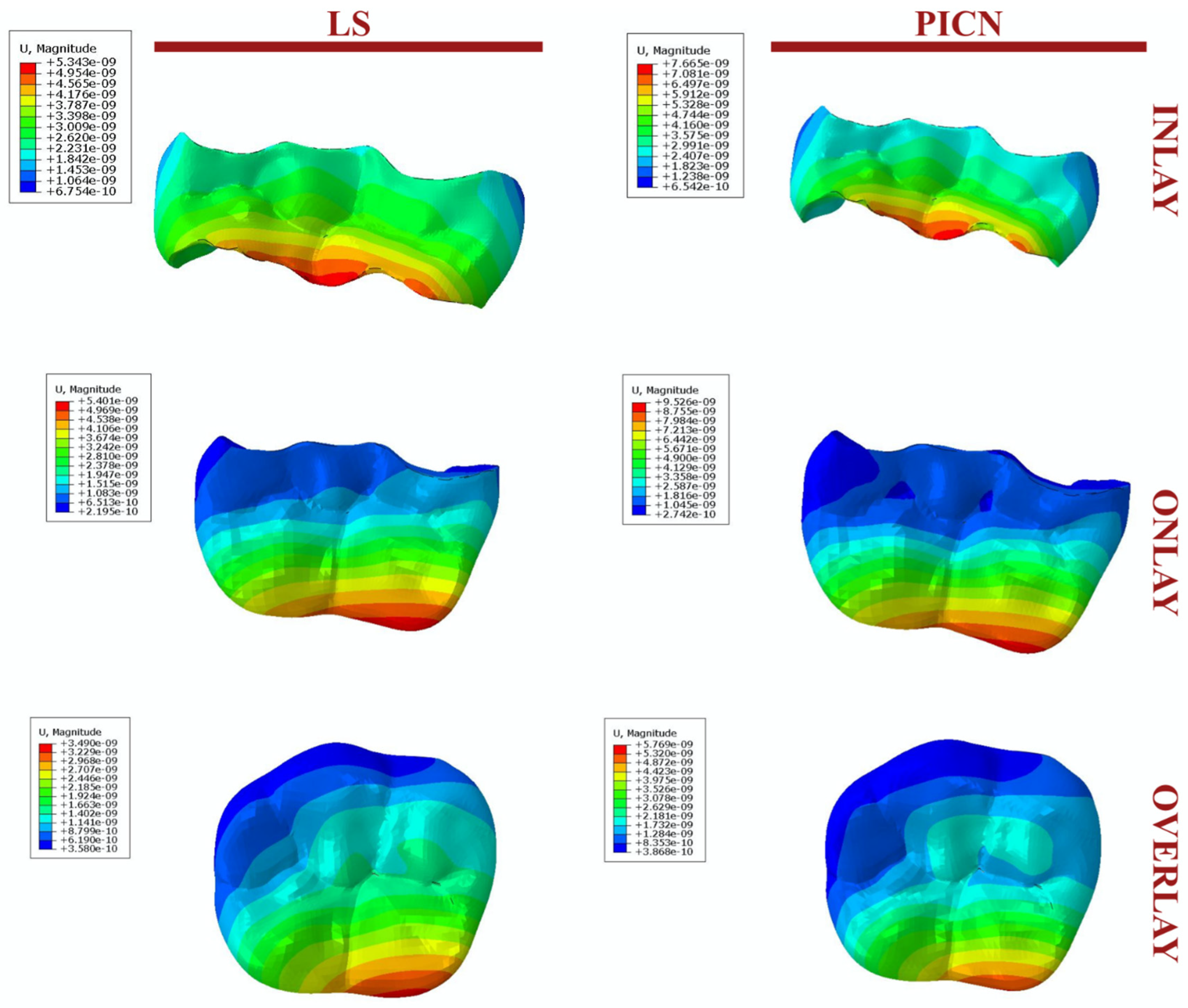
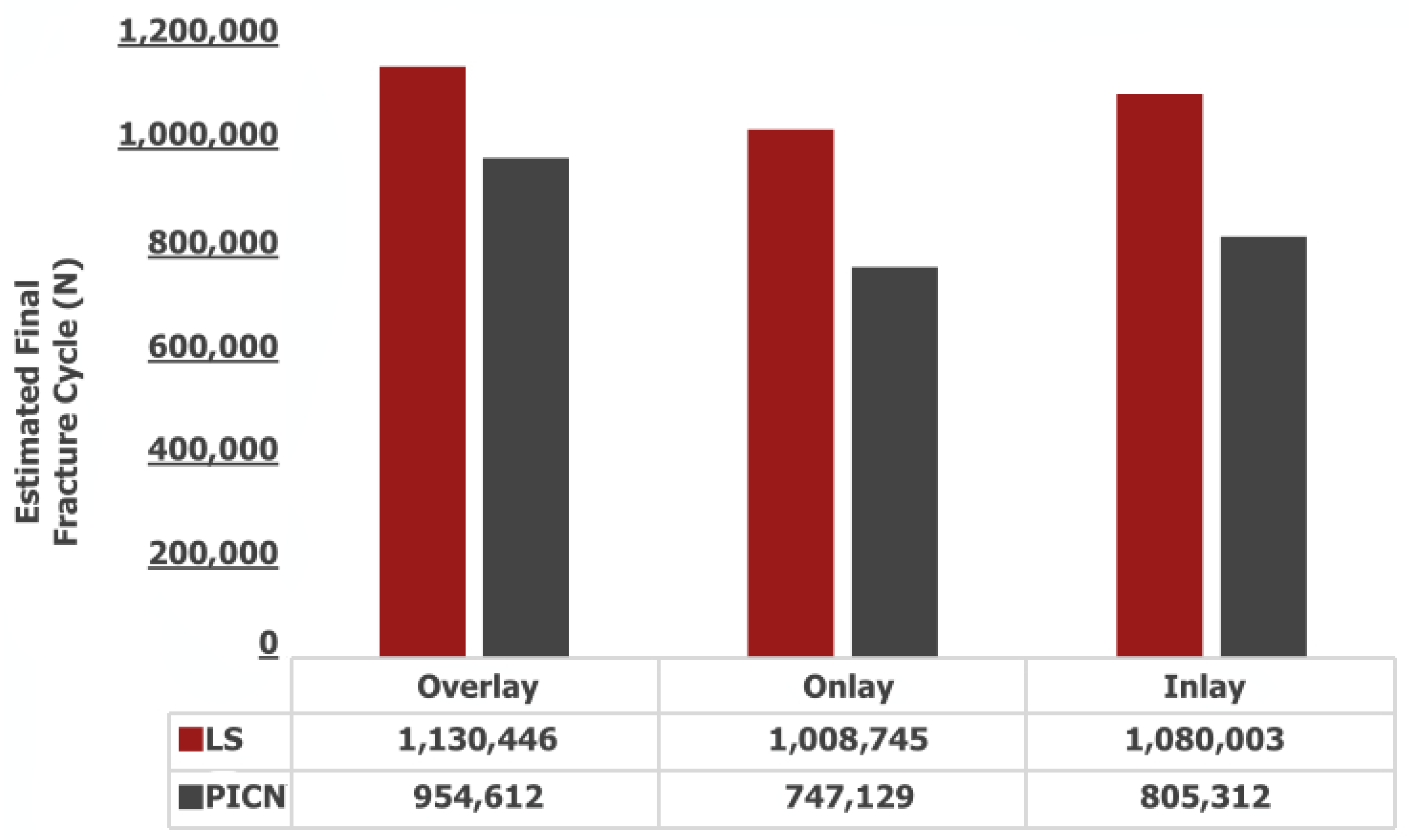
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Deliperi, S.; Bardwell, D.N. An Alternative Method to Reduce Polymerization Shrinkage in Direct Posterior Composite Restorations. J. Am. Dent. Assoc. 2002, 133, 1387–1398. [Google Scholar] [CrossRef] [PubMed]
- Soares, L.M.; Razaghy, M.; Magne, P. Optimization of Large MOD Restorations: Composite Resin Inlays vs. Short Fiber-Reinforced Direct Restorations. Dent. Mater. 2018, 34, 587–597. [Google Scholar] [CrossRef]
- Singhal, S.; Gurtu, A.; Singhal, A.; Bansal, R.; Mohan, S. Effect of Different Composite Restorations on the Cuspal Deflection of Premolars Restored with Different Insertion Techniques—An In Vitro Study. J. Clin. Diagn. Res. 2017, 11, 67–70. [Google Scholar] [CrossRef]
- Conserva, E.; Consolo, U.; Gimenez Sancho, A.; Foschi, F.; Paolone, G.; Giovarrusscio, M.; Sauro, S. Stress Distribution in Carbon-Post Applied with Different Composite Core Materials: A Three-Dimensional Finite Element Analysis. J. Adhes. Sci. Technol. 2017, 31, 2435–2444. [Google Scholar] [CrossRef]
- Batalha-Silva, S.; De Andrada, M.A.C.; Maia, H.P.; Magne, P. Fatigue Resistance and Crack Propensity of Large MOD Composite Resin Restorations: Direct versus CAD/CAM Inlays. Dent. Mater. 2013, 29, 324–331. [Google Scholar] [CrossRef]
- Dejak, B.; Młotkowski, A. A Comparison of Stresses in Molar Teeth Restored with Inlays and Direct Restorations, Including Polymerization Shrinkage of Composite Resin and Tooth Loading during Mastication. Dent. Mater. 2015, 31, e77–e87. [Google Scholar] [CrossRef] [PubMed]
- Chotiwutthiphatthana, D.; Angwaravong, O.; Angwarawong, T. Effect of Different Indirect Composite Onlay and Core Materials on Fracture Resistance of Endodontically Treated Maxillary Premolars. J. Prosthodont. Res. 2023, 67, 376–383. [Google Scholar] [CrossRef]
- Rocca, G.T.; Saratti, C.M.; Cattani-Lorente, M.; Feilzer, A.J.; Scherrer, S.; Krejci, I. The Effect of a Fiber Reinforced Cavity Configuration on Load Bearing Capacity and Failure Mode of Endodontically Treated Molars Restored with CAD/CAM Resin Composite Overlay Restorations. J. Dent. 2015, 43, 1106–1115. [Google Scholar] [CrossRef] [PubMed]
- Al-Fouzan, A.; Tashkandi, E. Volumetric Measurements of Removed Tooth Structure Associated with Various Preparation Designs. Int. J. Prosthodont. 2013, 26, 545–548. [Google Scholar] [CrossRef]
- Edelhoff, D.; Sorensen, J.A. Tooth Structure Removal Associated with Various Preparation Designs for Anterior Teeth. J. Prosthet. Dent. 2002, 87, 503–509. [Google Scholar] [CrossRef]
- Zarone, F.; Di Mauro, M.I.; Ausiello, P.; Ruggiero, G.; Sorrentino, R. Current Status on Lithium Disilicate and Zirconia: A Narrative Review. BMC Oral Health 2019, 19, 134. [Google Scholar] [CrossRef]
- de Carvalho, A.B.G.; de Andrade, G.S.; Tribst, J.P.M.; Grassi, E.D.A.; Ausiello, P.; Saavedra, G.d.S.F.A.; Bressane, A.; de Melo, R.M.; Borges, A.L.S. Mechanical Behavior of Different Restorative Materials and Onlay Preparation Designs in Endodontically Treated Molars. Materials 2021, 14, 1923. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Paranhos, M.P.G.; Schlichting, L.H. Influence of Material Selection on the Risk of Inlay Fracture during Pre-Cementation Functional Occlusal Tapping. Dent. Mater. 2011, 27, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Comba, A.; Baldi, A.; Carossa, M.; Michelotto Tempesta, R.; Garino, E.; Llubani, X.; Rozzi, D.; Mikonis, J.; Paolone, G.; Scotti, N. Post-Fatigue Fracture Resistance of Lithium Disilicate and Polymer-Infiltrated Ceramic Network Indirect Restorations over Endodontically-Treated Molars with Different Preparation Designs: An In-Vitro Study. Polymers 2022, 14, 5084. [Google Scholar] [CrossRef] [PubMed]
- Cui, B.; Zhang, R.; Sun, F.; Ding, Q.; Lin, Y.; Zhang, L.; Nan, C. Mechanical and Biocompatible Properties of Polymer-Infiltrated-Ceramic-Network Materials for Dental Restoration. J. Adv. Ceram. 2020, 9, 123–128. [Google Scholar] [CrossRef]
- Øilo, M.; Hardang, A.D.; Ulsund, A.H.; Gjerdet, N.R. Fractographic Features of Glass-Ceramic and Zirconia-Based Dental Restorations Fractured during Clinical Function. Eur. J. Oral Sci. 2014, 122, 238–244. [Google Scholar] [CrossRef]
- Boonrawd, N.; Rungsiyakull, P.; Rungsiyakull, C.; Louwakul, P. Effects of Composite Resin Core Level and Periodontal Pocket Depth on Crack Propagation in Endodontically Treated Teeth: An Extended Finite Element Method Study. J. Prosthet. Dent. 2022, 128, 195.e1–195.e7. [Google Scholar] [CrossRef]
- Dal Piva, A.M.d.O.; Tribst, J.P.M.; Borges, A.L.S.; de Melo, R.M.; Bottino, M.A. Influence of Substrate Design for in Vitro Mechanical Testing. J. Clin. Exp. Dent. 2019, 11, e119–e125. [Google Scholar] [CrossRef]
- Kishen, A. Mechanisms and Risk Factors for Fracture Predilection in Endodontically Treated Teeth. Endod. Top. 2006, 13, 57–83. [Google Scholar] [CrossRef]
- Zhang, Z.; Guazzato, M.; Sornsuwan, T.; Scherrer, S.S.; Rungsiyakull, C.; Li, W.; Swain, M.V.; Li, Q. Thermally Induced Fracture for Core-Veneered Dental Ceramic Structures. Acta Biomater. 2013, 9, 8394–8402. [Google Scholar] [CrossRef]
- Schroeder, G.; Rösch, P.; Kunzelmann, K.H. Influence of the Preparation Design on the Survival Probability of Occlusal Veneers. Dent. Mater. 2022, 38, 646–654. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Kim, B.S.; Kim, H.; Cho, S.Y. Occlusal Stress Distribution and Remaining Crack Propagation of a Cracked Tooth Treated with Different Materials and Designs: 3D Finite Element Analysis. Dent. Mater. 2021, 37, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Gonzaga, C.C.; Yoshimura, H.N.; Cesar, P.F.; Miranda, W.G. Subcritical Crack Growth in Porcelains, Glass-Ceramics, and Glass-Infiltrated Alumina Composite for Dental Restorations. J. Mater. Sci. Mater. Med. 2009, 20, 1017–1024. [Google Scholar] [CrossRef] [PubMed]
- Guess, P.C.; Schultheis, S.; Wolkewitz, M.; Zhang, Y.; Strub, J.R. Influence of Preparation Design and Ceramic Thicknesses on Fracture Resistance and Failure Modes of Premolar Partial Coverage Restorations. J. Prosthet. Dent. 2013, 110, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Homaei, E.; Farhangdoost, K.; Tsoi, J.K.H.; Matinlinna, J.P.; Pow, E.H.N. Static and Fatigue Mechanical Behavior of Three Dental CAD/CAM Ceramics. J. Mech. Behav. Biomed. Mater. 2016, 59, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Aboushelib, M.N.; Elsafi, M.H. Survival of Resin Infiltrated Ceramics under Influence of Fatigue. Dent. Mater. 2016, 32, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Swain, M.V.; Coldea, A.; Bilkhair, A.; Guess, P.C. Interpenetrating Network Ceramic-Resin Composite Dental Restorative Materials. Dent. Mater. 2016, 32, 34–42. [Google Scholar] [CrossRef]
- Homaei, E.; Farhangdoost, K.; Pow, E.H.N.; Matinlinna, J.P.; Akbari, M.; Tsoi, J.K.H. Fatigue Resistance of Monolithic CAD/CAM Ceramic Crowns on Human Premolars. Ceram. Int. 2016, 42, 15709–15717. [Google Scholar] [CrossRef]
- Giner, E.; Sukumar, N.; Tarancón, J.E.; Fuenmayor, F.J. An Abaqus Implementation of the Extended Finite Element Method. Eng. Fract. Mech. 2009, 76, 347–368. [Google Scholar] [CrossRef]
- Zhang, Z.; Thompson, M.; Field, C.; Li, W.; Li, Q.; Swain, M.V. Fracture Behavior of Inlay and Onlay Fixed Partial Dentures—An in-Vitro Experimental and XFEM Modeling Study. J. Mech. Behav. Biomed. Mater. 2016, 59, 279–290. [Google Scholar] [CrossRef]
- Wu, F.; Yao, W.X. A Fatigue Damage Model of Composite Materials. Int. J. Fatigue 2010, 32, 134–138. [Google Scholar] [CrossRef]
- Broutman, L.; Sahu, S. A New Theory to Predict Cumulative Fatigue Damage in Fiberglass Reinforced Plastics. Compos. Mater. Test. Des. Second Conf. 2009, 497, 170–188. [Google Scholar]
- Gulec, L.; Ulusoy, N. Effect of Endocrown Restorations with Different CAD/CAM Materials: 3D Finite Element and Weibull Analyses. Biomed Res. Int. 2017, 2017, 5638683. [Google Scholar] [CrossRef] [PubMed]
- Hofsteenge, J.W.; van den Heijkant, I.A.; Cune, M.S.; Bazos, P.K.; van der Made, S.; Kerdijk, W.; Gresnigt, M. Influence of Preparation Design and Restorative Material on Fatigue and Fracture Strength of Restored Maxillary Premolars. Oper. Dent. 2021, 46, E68–E79. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, S.; Vieira, G.F.; Agra, C.M.; Sesma, N.; Gil, C. Fracture Strength of Teeth Restored with Ceramic Inlays and Overlays. Braz. Dent. J. 2009, 20, 143–148. [Google Scholar] [CrossRef]
- Wafaie, R.A.; Ibrahim Ali, A.; Mahmoud, S.H. Fracture Resistance of Prepared Premolars Restored with Bonded New Lab Composite and All-Ceramic Inlay/Onlay Restorations: Laboratory Study. J. Esthet. Restor. Dent. 2018, 30, 229–239. [Google Scholar] [CrossRef]
- de Azevedo Cubas, G.B.; Habekost, L.; Camacho, G.B.; Pereira-Cenci, T. Fracture Resistance of Premolars Restored with Inlay and Onlay Ceramic Restorations and Luted with Two Different Agents. J. Prosthodont. Res. 2011, 55, 53–59. [Google Scholar] [CrossRef]
- De Habekost, L.V.; Camacho, G.B.; Pinto, M.B.; Demarco, F.F. Fracture Resistance of Premolars Restored with Partial Ceramic Restorations and Submitted to Two Different Loading Stresses. Oper. Dent. 2006, 31, 204–211. [Google Scholar] [CrossRef]
- Huda, I.; Pandey, A.; Kumar, N.; Sinha, S.; Kavita, K.; Raj, R. Resistance against Fracture in Teeth Managed by Root Canal Treatment on Restoring with Onlays, Inlays, and Endocrowns: A Comparative Analysis. J. Contemp. Dent. Pract. 2021, 22, 799–804. [Google Scholar]
- Kassis, C.; Khoury, P.; Mehanna, C.Z.; Baba, N.Z.; Bou Chebel, F.; Daou, M.; Hardan, L. Effect of Inlays, Onlays and Endocrown Cavity Design Preparation on Fracture Resistance and Fracture Mode of Endodontically Treated Teeth: An In Vitro Study. J. Prosthodont. 2021, 30, 625–631. [Google Scholar] [CrossRef]
- Naik, V.; Jain, A.; Rao, R.; Naik, B. Comparative Evaluation of Clinical Performance of Ceramic and Resin Inlays, Onlays, and Overlays: A Systematic Review and Meta Analysis. J. Conserv. Dent. 2022, 25, 347. [Google Scholar] [CrossRef]
- Channarong, W.; Lohawiboonkij, N.; Jaleyasuthumkul, P.; Ketpan, K.; Duangrattanaprathip, N.; Wayakanon, K. Fracture Resistance of Bonded Ceramic Overlay Restorations Prepared in Various Designs. Sci. Rep. 2022, 12, 16599. [Google Scholar] [CrossRef] [PubMed]
- Apel, E.; Deubener, J.; Bernard, A.; Höland, M.; Müller, R.; Kappert, H.; Rheinberger, V.; Höland, W. Phenomena and Mechanisms of Crack Propagation in Glass-Ceramics. J. Mech. Behav. Biomed. Mater. 2008, 1, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Velho, H.C.; Dapieve, K.S.; Rocha Pereira, G.K.; Fraga, S.; Valandro, L.F.; Venturini, A.B. Accelerated Loading Frequency Does Not Influence the Fatigue Behavior of Polymer Infiltrated Ceramic Network or Lithium Disilicate Glass-Ceramic Restorations. J. Mech. Behav. Biomed. Mater. 2020, 110, 103905. [Google Scholar] [CrossRef]
- Wegner, L.D.; Gibson, L.J. The Fracture Toughness Behaviour of Interpenetrating Phase Composites. Int. J. Mech. Sci. 2001, 43, 1771–1791. [Google Scholar] [CrossRef]
- Choi, S.; Yoon, H.I.; Park, E.J. Load-Bearing Capacity of Various CAD/CAM Monolithic Molar Crowns under Recommended Occlusal Thickness and Reduced Occlusal Thickness Conditions. J. Adv. Prosthodont. 2017, 9, 423–431. [Google Scholar] [CrossRef]
- de Carvalho, M.A.; Lazari-Carvalho, P.C.; Del Bel Cury, A.A.; Magne, P. Fatigue and Failure Analysis of Restored Endodontically Treated Maxillary Incisors without a Dowel or Ferrule. J. Prosthet. Dent. 2022; online ahead of print. [Google Scholar]
- Dartora, G.; Rocha Pereira, G.K.; Varella de Carvalho, R.; Zucuni, C.P.; Valandro, L.F.; Cesar, P.F.; Caldas, R.A.; Bacchi, A. Comparison of Endocrowns Made of Lithium Disilicate Glass-Ceramic or Polymer-Infiltrated Ceramic Networks and Direct Composite Resin Restorations: Fatigue Performance and Stress Distribution. J. Mech. Behav. Biomed. Mater. 2019, 100, 103401. [Google Scholar] [CrossRef]
- Ramírez-Sebastià, A.; Bortolotto, T.; Cattani-Lorente, M.; Giner, L.; Roig, M.; Krejci, I. Adhesive Restoration of Anterior Endodontically Treated Teeth: Influence of Post Length on Fracture Strength. Clin. Oral Investig. 2014, 18, 545–554. [Google Scholar] [CrossRef]
- Abraha, H.M.; Iriarte-Diaz, J.; Ross, C.F.; Taylor, A.B.; Panagiotopoulou, O. The Mechanical Effect of the Periodontal Ligament on Bone Strain Regimes in a Validated Finite Element Model of a Macaque Mandible. Front. Bioeng. Biotechnol. 2019, 7, 269. [Google Scholar]


| Materials | Young’s Modulus (MPa) | Poisson’s Ratio | Compressive Strength (Mpa) | Tensile Stress σTS (Mpa) | Fracture Toughness KIC (Mpa × ) | Strain Energy Release Rate G (J/m2) | References |
|---|---|---|---|---|---|---|---|
| Dentin | 18,600 | 0.31 | 282 | - | - | - | [1] |
| Enamel | 84,000 | 0.33 | 321 | - | - | - | [1] |
| LS | 98,000 | 0.23 | - | 210 | 2.27 | 52.6 | [2] |
| PICN | 35,000 | 0.23 | - | 148 | 1.2 | 41.1 | [2] |
| RelyX ARC | 5100 | 0.27 | - | - | - | - | [3] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demirel, M.G.; Mohammadi, R.; Keçeci, M. Crack Propagation and Fatigue Performance of Partial Posterior Indirect Restorations: An Extended Finite Element Method Study. J. Funct. Biomater. 2023, 14, 484. https://doi.org/10.3390/jfb14090484
Demirel MG, Mohammadi R, Keçeci M. Crack Propagation and Fatigue Performance of Partial Posterior Indirect Restorations: An Extended Finite Element Method Study. Journal of Functional Biomaterials. 2023; 14(9):484. https://doi.org/10.3390/jfb14090484
Chicago/Turabian StyleDemirel, Mehmet Gökberkkaan, Reza Mohammadi, and Murat Keçeci. 2023. "Crack Propagation and Fatigue Performance of Partial Posterior Indirect Restorations: An Extended Finite Element Method Study" Journal of Functional Biomaterials 14, no. 9: 484. https://doi.org/10.3390/jfb14090484





