Polycaprolactone in Bone Tissue Engineering: A Comprehensive Review of Innovations in Scaffold Fabrication and Surface Modifications
Abstract
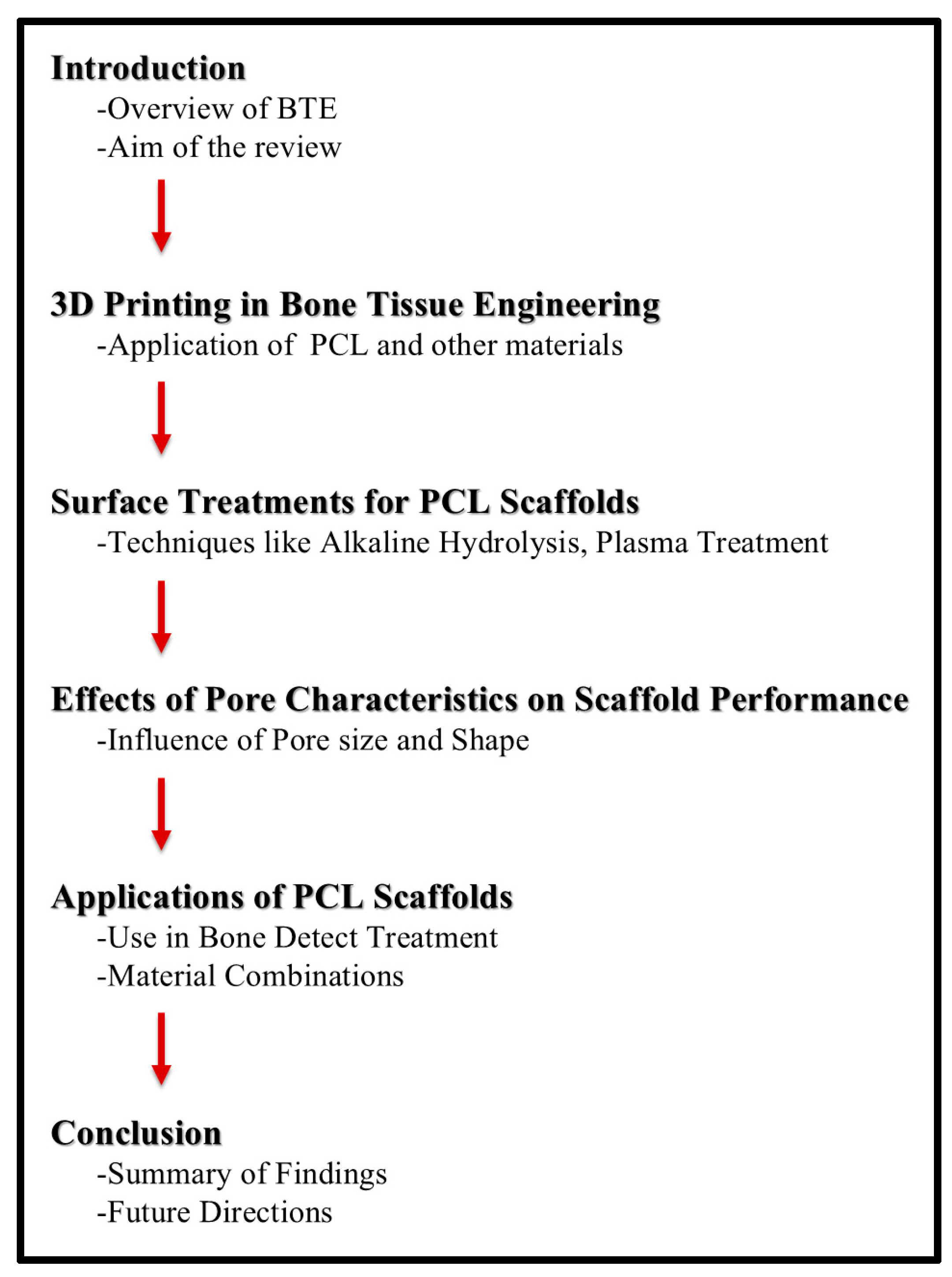
:1. Introduction
1.1. Overview of Bone Tissue Engineering (BTE)
1.2. Three-Dimensional (3D) Printing in Bone Tissue Engineering
2. Surface Treatments for PCL Scaffolds
2.1. Surface Coatings
2.2. Alkaline Hydrolysis
2.3. Plasma Treatment
2.4. Aminolysis
3. Effects of Pore Characteristics on Scaffold Performance
3.1. Effect of Pore Size
3.2. Effect of Pore Shapes
4. Applications of PCL Scaffolds
4.1. Diseases Commonly Treated with PCL Scaffolds
4.2. Materials Combined with PCL Scaffolds
4.2.1. Hydrogel
4.2.2. Nanomaterials
4.2.3. Graphene Oxide (GO)
4.2.4. HA
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Janmohammadi, M.; Nourbakhsh, M.S.; Bahraminasab, M.; Tayebi, L. Effect of pore characteristics and alkali treatment on the physicochemical and biological properties of a 3D-printed polycaprolactone bone scaffold. ACS Omega 2023, 8, 7378–7394. [Google Scholar] [CrossRef]
- Lei, C.; Song, J.H.; Li, S.; Zhu, Y.N.; Liu, M.Y.; Wan, M.C.; Mu, Z.; Tay, F.R.; Niu, L.N. Advances in materials-based therapeutic strategies against osteoporosis. Biomaterials 2023, 296, 122066. [Google Scholar] [CrossRef]
- Menotti, F.; Scutera, S.; Coppola, B.; Longo, F.; Mandras, N.; Cavallo, L.; Comini, S.; Sparti, R.; Fiume, E.; Cuffini, A.M.; et al. Tuning of silver content on the antibacterial and biological properties of poly(varepsilon-caprolactone)/biphasic calcium phosphate 3D-scaffolds for bone tissue engineering. Polymers 2023, 15, 3618. [Google Scholar] [CrossRef]
- Bružauskaitė, I.; Bironaitė, D.; Bagdonas, E.; Bernotienė, E. Scaffolds and cells for tissue regeneration: Different scaffold pore sizes-different cell effects. Cytotechnology 2016, 68, 355–369. [Google Scholar] [CrossRef]
- Cao, L.; Yu, Y.; Wang, J.; Werkmeister, J.A.; McLean, K.M.; Liu, C. 2-N, 6-O-sulfated chitosan-assisted BMP-2 immobilization of PCL scaffolds for enhanced osteoinduction. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 74, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Re, F.; Borsani, E.; Rezzani, R.; Sartore, L.; Russo, D. Bone regeneration using mesenchymal stromal cells and biocompatible scaffolds: A concise review of the current clinical trials. Gels 2023, 9, 389. [Google Scholar] [CrossRef]
- Jang, J.W.; Min, K.E.; Kim, C.; Wern, C.; Yi, S. Rheological properties and 3D printing behavior of PCL and DMSO2 composites for bio-scaffold. Materials 2024, 17, 2459. [Google Scholar] [CrossRef]
- Nyberg, E.; Rindone, A.; Dorafshar, A.; Grayson, W.L. Comparison of 3D-printed poly-ε-caprolactone scaffolds functionalized with tricalcium phosphate, hydroxyapatite, Bio-Oss, or decellularized bone matrix. Tissue Eng Part A 2017, 23, 503–514. [Google Scholar] [CrossRef]
- Ruiz-Aguilar, C. Porous phosphate-based bioactive glass/β-TCP scaffold for tooth remineralization. PLoS ONE 2023, 18, e0284885. [Google Scholar] [CrossRef]
- Sandanamsamy, L.; Harun, W.S.W.; Ishak, I.; Romlay, F.R.M.; Kadirgama, K.; Ramasamy, D.; Idris, S.R.A.; Tsumori, F. A comprehensive review on fused deposition modelling of polylactic acid. Prog. Addit. Manuf. 2022, 8, 775–799. [Google Scholar] [CrossRef]
- Ni, Z.; Shi, J.; Li, M.; Lei, W.; Yu, W. FDM 3D printing and soil-burial-degradation behaviors of residue of astragalus particles/thermoplastic starch/poly (lactic acid) biocomposites. Polymers 2023, 15, 2382. [Google Scholar] [CrossRef]
- Muta, S.; Ikeda, M.; Nikaido, T.; Sayed, M.; Sadr, A.; Suzuki, T.; Tagami, J. Chairside fabrication of provisional crowns on FDM 3D-printed PVA model. J. Prosthodont. Res. 2020, 64, 401–407. [Google Scholar] [CrossRef]
- Wismer, N.; Grad, S.; Fortunato, G.; Ferguson, S.J.; Alini, M.; Eglin, D. Biodegradable electrospun scaffolds for annulus fibrosus tissue engineering: Effect of scaffold structure and composition on annulus fibrosus cells in vitro. Tissue Eng. Part. A 2014, 20, 672–682. [Google Scholar] [CrossRef]
- Sowmya, B.; Hemavathi, A.B.; Panda, P.K. Poly (ε-caprolactone)-based electrospun nano-featured substrate for tissue engineering applications: A review. Prog. Biomater. 2021, 10, 91–117. [Google Scholar] [CrossRef]
- Siddiqui, N.; Asawa, S.; Birru, B.; Baadhe, R.; Rao, S. PCL-based composite scaffold matrices for tissue engineering applications. Mol. Biotechnol. 2018, 60, 506–532. [Google Scholar] [CrossRef]
- Yang, Y.; Wu, H.; Fu, Q.; Xie, X.; Song, Y.; Xu, M.; Li, J. 3D-printed polycaprolactone-chitosan based drug delivery implants for personalized administration. Mater. Des. 2022, 214, 110394. [Google Scholar] [CrossRef]
- Dwivedi, R.; Kumar, S.; Pandey, R.; Mahajan, A.; Nandana, D.; Katti, D.S.; Mehrotra, D. Polycaprolactone as biomaterial for bone scaffolds: Review of literature. J. Oral. Biol. Craniofac Res. 2020, 10, 381–388. [Google Scholar] [CrossRef]
- Ilyas, R.A.; Zuhri, M.Y.M.; Norrrahim, M.N.F.; Misenan, M.S.M.; Jenol, M.A.; Samsudin, S.A.; Nurazzi, N.M.; Asyraf, M.R.M.; Supian, A.B.M.; Bangar, S.P.; et al. Natural fiber-reinforced polycaprolactone green and hybrid biocomposites for various advanced applications. Polymers 2022, 14, 182. [Google Scholar] [CrossRef]
- Bohner, M.; Santoni, B.L.G.; Döbelin, N. β-tricalcium phosphate for bone substitution: Synthesis and properties. Acta Biomater. 2020, 113, 23–41. [Google Scholar] [CrossRef]
- Ghezzi, B.; Matera, B.; Meglioli, M.; Rossi, F.; Duraccio, D.; Faga, M.G.; Zappettini, A.; Macaluso, G.M.; Lumetti, S. Composite PCL scaffold with 70% β-TCP as suitable structure for bone replacement. Int. Dent. J. 2024; in press. [Google Scholar]
- Ma, Y.; Dai, H.; Huang, X.; Long, Y. 3D printing of bioglass-reinforced β-TCP porous bioceramic scaffolds. J. Mater. Sci. 2019, 54, 10437–10446. [Google Scholar] [CrossRef]
- Liao, H.T.; Lee, M.Y.; Tsai, W.W.; Wang, H.C.; Lu, W.C. Osteogenesis of adipose-derived stem cells on polycaprolactone-β-tricalcium phosphate scaffold fabricated via selective laser sintering and surface coating with collagen type I. J. Tissue Eng. Regen. Med. 2016, 10, E337–E353. [Google Scholar] [CrossRef]
- Ngo, S.T.; Lee, W.F.; Wu, Y.F.; Salamanca, E.; Aung, L.M.; Chao, Y.Q.; Tsao, T.C.; Hseuh, H.W.; Lee, Y.H.; Wang, C.C.; et al. Fabrication of solvent-free PCL/β-TCP composite fiber for 3D printing: Physiochemical and biological investigation. Polymers 2023, 15, 1391. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Park, S.A.; Kang, Y.G.; Shin, J.W.; Park, Y.S.; Gu, S.R.; Wu, Y.R.; Wei, J.; Shin, J.W. PCL/β-TCP composite scaffolds exhibit positive osteogenic differentiation with mechanical stimulation. Tissue Eng. Regen. Med. 2017, 14, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, C.; Song, T.; Cao, Z.; Wang, T. 3D printed polycaprolactone/β-tricalcium phosphate/carbon nanotube composite—Physical properties and biocompatibility. Heliyon 2024, 10, e26071. [Google Scholar] [CrossRef] [PubMed]
- Javkhlan, Z.; Hsu, S.H.; Chen, R.S.; Chen, M.H. 3D-printed polycaprolactone scaffolds coated with beta tricalcium phosphate for bone regeneration. J. Formos. Med. Assoc. 2024, 123, 71–77. [Google Scholar] [CrossRef]
- Wang, Q.; Ye, W.; Ma, Z.; Xie, W.; Zhong, L.; Wang, Y.; Rong, Q. 3D printed PCL/β-TCP cross-scale scaffold with high-precision fiber for providing cell growth and forming bones in the pores. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 127, 112197. [Google Scholar] [CrossRef]
- Lu, L.; Zhang, Q.; Wootton, D.; Chiou, R.; Li, D.; Lu, B.; Lelkes, P.; Zhou, J. Biocompatibility and biodegradation studies of PCL/β-TCP bone tissue scaffold fabricated by structural porogen method. J. Mater. Sci. Mater. Med. 2012, 23, 2217–2226. [Google Scholar] [CrossRef] [PubMed]
- Roh, H.S.; Jung, S.C.; Kook, M.S.; Kim, B.H. In vitro study of 3D PLGA/n-HAp/β-TCP composite scaffolds with etched oxygen plasma surface modification in bone tissue engineering. Appl. Surf. Sci. 2016, 388, 321–330. [Google Scholar] [CrossRef]
- Dabasinskaite, L.; Krugly, E.; Baniukaitiene, O.; Martuzevicius, D.; Ciuzas, D.; Jankauskaite, L.; Aukstikalne, L.; Usas, A. The effect of ozone treatment on the physicochemical properties and biocompatibility of electrospun poly(ε)caprolactone scaffolds. Pharmaceutics 2021, 13, 1288. [Google Scholar] [CrossRef]
- Lam, C.X.; Hutmacher, D.W.; Schantz, J.T.; Woodruff, M.A.; Teoh, S.H. Evaluation of polycaprolactone scaffold degradation for 6 months in vitro and in vivo. J. Biomed. Mater. Res. A 2009, 90, 906–919. [Google Scholar] [CrossRef]
- Yaseri, R.; Fadaie, M.; Mirzaei, E.; Samadian, H.; Ebrahiminezhad, A. Surface modification of polycaprolactone nanofibers through hydrolysis and aminolysis: A comparative study on structural characteristics, mechanical properties, and cellular performance. Sci. Rep. 2023, 13, 9434. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Kim, J.E.; Han, J.; Jeong, S.; Lim, J.W.; Lee, M.C.; Son, H.; Kim, H.B.; Choung, Y.H.; Seonwoo, H.; et al. 3D-Printed Poly(ε-Caprolactone)/Hydroxyapatite Scaffolds Modified with Alkaline Hydrolysis Enhance Osteogenesis In Vitro. Polymers 2021, 13, 257. [Google Scholar] [CrossRef]
- Gupta, D.; Singh, A.K.; Kar, N.; Dravid, A.; Bellare, J. Modelling and optimization of NaOH-etched 3-D printed PCL for enhanced cellular attachment and growth with minimal loss of mechanical strength. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 98, 602–611. [Google Scholar] [CrossRef] [PubMed]
- Bagdoniene, L.; Bagdonas, E.; Ridikaite, E.; Baniukaitiene, O.; Peciulyte, L.; Pupiute, A.; Martuzevicius, D.; Krugly, E. Enhancing 3D poly[ɛ]caprolactone scaffold properties through alkaline hydrolysis for improved chondrocyte culture: Morphological, physicochemical, and biocompatibility evaluations. J. Drug Deliv. Sci. Technol. 2024, 97, 105806. [Google Scholar] [CrossRef]
- Bartnikowski, M.; Abdal-Hay, A.; Bartnikowski, N.J.; Kim, Y.K.; Ivanovski, S. A comprehensive study of acid and base treatment of 3D printed poly(ε-caprolactone) scaffolds to tailor surface characteristics. Appl. Surf. Sci. 2021, 555, 149602. [Google Scholar] [CrossRef]
- Shafei, S.; Foroughi, J.; Chen, Z.; Wong, C.S.; Naebe, M. Short oxygen plasma treatment leading to long-term hydrophilicity of conductive PCL-PPy nanofiber scaffolds. Polymers 2017, 9, 614. [Google Scholar] [CrossRef]
- Jeon, H.; Lee, H.; Kim, G. A surface-modified poly(ε-caprolactone) scaffold comprising variable nanosized surface-roughness using a plasma treatment. Tissue Eng. Part. C Methods 2014, 20, 951–963. [Google Scholar] [CrossRef]
- Valenti, C.; Pagano, S.; Bozza, S.; Ciurnella, E.; Lomurno, G.; Capobianco, B.; Coniglio, M.; Cianetti, S.; Marinucci, L. Use of the Er:YAG laser in conservative dentistry: Evaluation of the microbial population in carious lesions. Materials 2021, 14, 2387. [Google Scholar] [CrossRef]
- Jeznach, O.; Kolbuk, D.; Sajkiewicz, P. Aminolysis of various aliphatic polyesters in a form of nanofibers and films. Polymers 2019, 11, 1669. [Google Scholar] [CrossRef]
- Jamalpour, M.R.; Yadegari, A.; Vahdatinia, F.; Amirabad, L.M.; Jamshidi, S.; Shojaei, S.; Shokri, A.; Moeinifard, E.; Omidi, M.; Tayebi, L. 3D-printed bi-layered polymer/hydrogel construct for interfacial tissue regeneration in a canine model. Dent. Mater. 2022, 38, 1316–1329. [Google Scholar] [CrossRef]
- Rasoulianboroujeni, M.; Yadegari, A.; Tajik, S.; Tayebi, L. Development of a modular reinforced bone tissue engineering scaffold with enhanced mechanical properties. Mater. Lett. 2022, 318, 132170. [Google Scholar] [CrossRef] [PubMed]
- Omidi, M.; Almeida, L.E.; Tayebi, L. Optimization of the modular reinforced bone scaffold for customized alveolar bone defects. Mater. Lett. 2023, 331, 133413. [Google Scholar] [CrossRef] [PubMed]
- Augustin, J.; Feichtner, F.; Waselau, A.C.; Julmi, S.; Klose, C.; Wriggers, P.; Maier, H.J.; Meyer-Lindenberg, A. Effect of pore size on tissue ingrowth and osteoconductivity in biodegradable Mg alloy scaffolds. J. Appl. Biomater. Funct. Mater. 2022, 20, 22808000221078168. [Google Scholar] [CrossRef]
- Aydin, M.S.; Sahin, M.; Dogan, Z.; Kiziltas, G. Microstructural characterization of PCL-HA bone scaffolds based on nonsolvent-induced phase separation. ACS Omega 2023, 8, 47595–47605. [Google Scholar] [CrossRef] [PubMed]
- Andrade Mier, M.S.; Bakirci, E.; Stahlhut, P.; Blum, R.; Dalton, P.D.; Villmann, C. Primary glial cell and glioblastoma morphology in cocultures depends on scaffold design and hydrogel composition. Adv Biol 2023, 7, e2300029. [Google Scholar] [CrossRef]
- Qian, E.; Kang, Y. Branched channels in porous β-tricalcium phosphate scaffold promote vascularization. ACS Appl. Mater. Interfaces 2024, 16, 19081–19093. [Google Scholar] [CrossRef]
- Ghalia, M.A.; Alhanish, A. Mechanical and biodegradability of porous PCL/PEG copolymer-reinforced cellulose nanofibers for soft tissue engineering applications. Med. Eng. Phys. 2023, 120, 104055. [Google Scholar] [CrossRef]
- Tokeshi, S.; Fukawa, T.; Itadera, E.; Akazawa, T.; Fujiyoshi, T.; Takaso, M.; Nakagawa, K.; Yamauchi, T.; Osada, N.; Ohtori, S. Efficacy and safety of beta-tricalcium phosphate/polylactic-co-glycolic acid for implantation of bone defects. Cureus 2023, 15, e43597. [Google Scholar] [CrossRef]
- Chocholata, P.; Kulda, V.; Babuska, V. Fabrication of scaffolds for bone-tissue regeneration. Materials 2019, 12, 568. [Google Scholar] [CrossRef]
- Annabi, N.; Tamayol, A.; Uquillas, J.A.; Akbari, M.; Bertassoni, L.E.; Cha, C.; Camci-Unal, G.; Dokmeci, M.R.; Peppas, N.A.; Khademhosseini, A. 25th anniversary article: Rational design and applications of hydrogels in regenerative medicine. Adv. Mater. 2014, 26, 85–123. [Google Scholar] [CrossRef]
- Zhang, H.; Mao, X.; Du, Z.; Jiang, W.; Han, X.; Zhao, D.; Han, D.; Li, Q. Three dimensional printed macroporous polylactic acid/hydroxyapatite composite scaffolds for promoting bone formation in a critical-size rat calvarial defect model. Sci. Technol. Adv. Mater. 2016, 17, 136–148. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.S.; Lee, J.S.; Gao, G.; Cho, D.W. Direct 3D cell-printing of human skin with functional transwell system. Biofabrication 2017, 9, 025034. [Google Scholar] [CrossRef] [PubMed]
- González-Rodríguez, L.; Pérez-Davila, S.; Lama, R.; López-Álvarez, M.; Serra, J.; Novoa, B.; Figueras, A.; González, P. 3D printing of PLA:CaP:GO scaffolds for bone tissue applications. RSC Adv. 2023, 13, 15947–15959. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Dong, S. Graphene nanosheet: Synthesis, molecular engineering, thin film, hybrids, and energy and analytical applications. Chem. Soc. Rev. 2011, 40, 2644–2672. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Cote, L.J.; Kim, F.; Yuan, W.; Shull, K.R.; Huang, J. Graphene oxide sheets at interfaces. J. Am. Chem. Soc. 2010, 132, 8180–8186. [Google Scholar] [CrossRef]
- Murugan, S.; Parcha, S.R. Fabrication techniques involved in developing the composite scaffolds PCL/HA nanoparticles for bone tissue engineering applications. J. Mater. Sci. Mater. Med. 2021, 32, 93. [Google Scholar] [CrossRef]
- Shi, X.; Sitharaman, B.; Pham, Q.P.; Liang, F.; Wu, K.; Edward Billups, W.; Wilson, L.J.; Mikos, A.G. Fabrication of porous ultra-short single-walled carbon nanotube nanocomposite scaffolds for bone tissue engineering. Biomaterials 2007, 28, 4078–4090. [Google Scholar] [CrossRef]
- Gentile, P.; Chiono, V.; Carmagnola, I.; Hatton, P.V. An overview of poly(lactic-co-glycolic) acid (PLGA)-based biomaterials for bone tissue engineering. Int. J. Mol. Sci. 2014, 15, 3640–3659. [Google Scholar] [CrossRef]
| Materials | Advantage | Disadvantage |
|---|---|---|
| Hydrogel [2,6,50,51] |
|
|
| Nanomaterials [2,52,53] |
|
|
| Graphene oxide [54,55,56] |
| |
| Hydroxyapatite [1,57,58,59] |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liang, H.-Y.; Lee, W.-K.; Hsu, J.-T.; Shih, J.-Y.; Ma, T.-L.; Vo, T.T.T.; Lee, C.-W.; Cheng, M.-T.; Lee, I.-T. Polycaprolactone in Bone Tissue Engineering: A Comprehensive Review of Innovations in Scaffold Fabrication and Surface Modifications. J. Funct. Biomater. 2024, 15, 243. https://doi.org/10.3390/jfb15090243
Liang H-Y, Lee W-K, Hsu J-T, Shih J-Y, Ma T-L, Vo TTT, Lee C-W, Cheng M-T, Lee I-T. Polycaprolactone in Bone Tissue Engineering: A Comprehensive Review of Innovations in Scaffold Fabrication and Surface Modifications. Journal of Functional Biomaterials. 2024; 15(9):243. https://doi.org/10.3390/jfb15090243
Chicago/Turabian StyleLiang, Hsin-Yu, Wei-Keung Lee, Jui-Tsen Hsu, Jie-Yu Shih, Tien-Li Ma, Thi Thuy Tien Vo, Chiang-Wen Lee, Ming-Te Cheng, and I-Ta Lee. 2024. "Polycaprolactone in Bone Tissue Engineering: A Comprehensive Review of Innovations in Scaffold Fabrication and Surface Modifications" Journal of Functional Biomaterials 15, no. 9: 243. https://doi.org/10.3390/jfb15090243











