Short-Term Hydrolytic Degradation of Mechanical Properties of Absorbable Surgical Sutures: A Comparative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Tensile Strength Tests
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- The study showed that absorbable surgical sutures experience a statistically significant reduction in tensile strength during the first three weeks after implantation.
- Not all rapidly absorbable sutures weaken significantly during this critical initial period, but those that do may weaken wound stability.
- These findings highlight the importance of suture selection based on specific clinical needs, as early loss of strength can affect the wound-healing process.
- The choice of polymer in suture materials should be carefully matched to the procedure, site of application and patient condition to minimise the risk of postoperative complications.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gierek, M.; Kuśnierz, K.; Lampe, P.; Ochała, G.; Kurek, J.; Hekner, B.; Merkel, K.; Majewski, J. Absorbable Sutures in General Surgery—Review, Available Materials, and Optimum Choices. Pol. Przegl Chir. 2018, 90, 34–37. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.C. Types and Properties of Surgical Sutures. In Biotextiles as Medical Implants; Elsevier: Amsterdam, The Netherlands, 2013; pp. 231–273. ISBN 978-1-84569-439-5. [Google Scholar]
- Zhukovskii, V.A. Surgical Suture Materials with Special Properties. Fibre Chem. 2015, 47, 197–201. [Google Scholar] [CrossRef]
- Abhari, R.E.; Martins, J.A.; Morris, H.L.; Mouthuy, P.-A.; Carr, A. Synthetic Sutures: Clinical Evaluation and Future Developments. J. Biomater. Appl. 2017, 32, 410–421. [Google Scholar] [CrossRef]
- Najibi, S.; Banglmeier, R.; Matta, J.; Tannast, M. Material Properties of Common Suture Materials in Orthopaedic Surgery. Iowa Orthop. J. 2010, 30, 84–88. [Google Scholar] [PubMed]
- Rokkanen, P.U. Absorbable Materials in Orthopaedic Surgery. Ann. Med. 1991, 23, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Kanimozhi, T.; Pachiyappan, K.M.; Kalaiselvi, E.; Mahalakshmi, V.; Gokarneshan, N. Mechanical Properties of Textile Sutures for Orthopaedic Surgery. GSC Adv. Res. Rev. 2021, 7, 272–274. [Google Scholar] [CrossRef]
- Naleway, S.E.; Lear, W.; Kruzic, J.J.; Maughan, C.B. Mechanical Properties of Suture Materials in General and Cutaneous Surgery: An Update on Mechanical Properties of Suture Materials. J. Biomed. Mater. Res. 2015, 103, 735–742. [Google Scholar] [CrossRef]
- Açan, E.; Hapa, O.; Barber, F.A. Mechanical Properties of Suture Materials. In Knots in Orthopedic Surgery; Akgun, U., Karahan, M., Randelli, P.S., Espregueira-Mendes, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2018; pp. 21–31. ISBN 978-3-662-56107-2. [Google Scholar]
- Odili, C.C.; Ilomuanya, M.O.; Sekunowo, O.I.; Gbenebor, O.P.; Adeosun, S.O. Knot Strength and Antimicrobial Evaluations of Partially Absorbable Suture. Prog. Biomater. 2023, 12, 51–59. [Google Scholar] [CrossRef]
- Dennis, C.; Sethu, S.; Nayak, S.; Mohan, L.; Morsi, Y.; Manivasagam, G. Suture Materials—Current and Emerging Trends. J. Biomed. Mater. Res. 2016, 104, 1544–1559. [Google Scholar] [CrossRef]
- Polykandriotis, E.; Daenicke, J.; Bolat, A.; Grüner, J.; Schubert, D.W.; Horch, R.E. Individualized Wound Closure—Mechanical Properties of Suture Materials. JPM 2022, 12, 1041. [Google Scholar] [CrossRef]
- Li, Y.; Meng, Q.; Chen, S.; Ling, P.; Kuss, M.A.; Duan, B.; Wu, S. Advances, Challenges, and Prospects for Surgical Suture Materials. Acta Biomater. 2023, 168, 78–112. [Google Scholar] [CrossRef]
- Mukherjee, C.; Varghese, D.; Krishna, J.S.; Boominathan, T.; Rakeshkumar, R.; Dineshkumar, S.; Brahmananda Rao, C.V.S.; Sivaramakrishna, A. Recent Advances in Biodegradable Polymers—Properties, Applications and Future Prospects. Eur. Polym. J. 2023, 192, 112068. [Google Scholar] [CrossRef]
- Kuzu, T.E. Comparison Tensile Strength of Different Sutur Materials. Cumhur. Dent. J. 2022, 24, 355–360. [Google Scholar] [CrossRef]
- Deng, X.; Qasim, M.; Ali, A. Engineering and Polymeric Composition of Drug-eluting Suture: A Review. J. Biomed. Mater. Res. 2021, 109, 2065–2081. [Google Scholar] [CrossRef] [PubMed]
- Wade, R.G.; Wormald, J.C.; Figus, A. Absorbable versus Non-Absorbable Sutures for Skin Closure after Carpal Tunnel Decompression Surgery. Cochrane Database Syst. Rev. 2018, 2018, CD011757. [Google Scholar] [CrossRef]
- Karpiński, R.; Szabelski, J.; Maksymiuk, J. Effect of Ringer’s Solution on Tensile Strength of Non-Absorbable, Medium- and Long-Term Absorbable Sutures. Adv. Sci. Technol. Res. J. 2017, 11, 11–20. [Google Scholar] [CrossRef]
- Feeley, A.A.; Feeley, I.H.; Roopnarinesingh, R.; Bayer, T. Rates of Complications in Achilles Tendon Rupture Repair Using Absorbable and Nonabsorbable Suture Material; A Systematic Review. Foot 2022, 51, 101875. [Google Scholar] [CrossRef]
- Egbunah, U.P.; Adamson, O.; Fashina, A.; Adekunle, A.A.; James, O.; Adeyemo, W.L. Comparing the Treatment Outcomes of Absorbable Sutures, Nonabsorbable Sutures, and Tissue Adhesives in Cleft Lip Repair: A Systematic Review. Cleft Palate-Craniofacial J. 2022, 59, 110–120. [Google Scholar] [CrossRef]
- Sajid, M.S. Systematic Review of Absorbable vs Non-Absorbable Sutures Used for the Closure of Surgical Incisions. WJGS 2014, 6, 241. [Google Scholar] [CrossRef]
- Xu, B.; Xu, B.; Wang, L.; Chen, C.; Yilmaz, T.U.; Zheng, W.; He, B. Absorbable Versus Nonabsorbable Sutures for Skin Closure: A Meta-Analysis of Randomized Controlled Trials. Ann. Plast. Surg. 2016, 76, 598–606. [Google Scholar] [CrossRef]
- Abiri, A.; Paydar, O.; Tao, A.; LaRocca, M.; Liu, K.; Genovese, B.; Candler, R.; Grundfest, W.S.; Dutson, E.P. Tensile Strength and Failure Load of Sutures for Robotic Surgery. Surg. Endosc. 2017, 31, 3258–3270. [Google Scholar] [CrossRef] [PubMed]
- Pillai, C.K.S.; Sharma, C.P. Review Paper: Absorbable Polymeric Surgical Sutures: Chemistry, Production, Properties, Biodegradability, and Performance. J. Biomater. Appl. 2010, 25, 291–366. [Google Scholar] [CrossRef]
- Modrák, M.; Trebuňová, M.; Balogová, A.F.; Hudák, R.; Živčák, J. Biodegradable Materials for Tissue Engineering: Development, Classification and Current Applications. JFB 2023, 14, 159. [Google Scholar] [CrossRef] [PubMed]
- Hynes, C.G.; Morra, E.; Walsh, P.; Buchanan, F. Degradation of Biomaterials. In Tissue Engineering; Elsevier: Amsterdam, The Netherlands, 2023; pp. 213–259. ISBN 978-0-12-824459-3. [Google Scholar]
- Deshayes, S.; Kasko, A.M. Polymeric Biomaterials with Engineered Degradation. J. Polym. Sci. Part. A Polym. Chem. 2013, 51, 3531–3566. [Google Scholar] [CrossRef]
- Başçı, O.; Akgun, U.; Barber, F.A. Biological Properties of Suture Materials. In Knots in Orthopedic Surgery; Akgun, U., Karahan, M., Randelli, P.S., Espregueira-Mendes, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2018; pp. 11–20. ISBN 978-3-662-56107-2. [Google Scholar]
- Sheik-Ali, S.; Guets, W. Absorbable vs Non Absorbable Sutures for Wound Closure. Systematic Review of Systematic Reviews. Wound Med. 2018, 23, 35–37. [Google Scholar] [CrossRef]
- Hamza, A.A.; El-Bakary, M.A.; El-Rashidy, N.M.; Omar, E. The Influence of Degradation in Different pH Buffer Solutions on the Optical and Durability Properties of Monocryl Suture: (An in Vitro Study). Polym. Bull. 2024, 81, 3149–3168. [Google Scholar] [CrossRef]
- Hofmann, D.; Entrialgo-Castaño, M.; Kratz, K.; Lendlein, A. Knowledge-Based Approach towards Hydrolytic Degradation of Polymer-Based Biomaterials. Adv. Mater. 2009, 21, 3237–3245. [Google Scholar] [CrossRef]
- Lekic, N.; Dodds, S.D. Suture Materials, Needles, and Methods of Skin Closure: What Every Hand Surgeon Should Know. J. Hand Surg. 2022, 47, 160–171.e1. [Google Scholar] [CrossRef]
- Zhang, Z.; Jiang, L.; Hu, J. 5-Fluorouracil Injection for the Treatment of a Suture-Induced Foreign Body Reaction after Blepharoplasty. Aesth Plast. Surg. 2024. [Google Scholar] [CrossRef]
- Sharma, P.; Singh, D.; Pant, S.; Dave, V. Nanotechnology Based Advanced Medical Textiles and Biotextiles for Healthcare, 1st ed.; CRC Press: Boca Raton, FL, USA, 2024; ISBN 978-1-00-333161-2. [Google Scholar]
- Chellamani, K.P.; Veerasubramanian, D.; Balaji, R.V. Surgical Sutures: An Overview. J. Acad. Indus Res. 2013, 1, 778–782. [Google Scholar]
- Byrne, M.; Aly, A. The Surgical Suture. Aesthetic Surg. J. 2019, 39, S67–S72. [Google Scholar] [CrossRef] [PubMed]
- Thacker, J.G.; Rodeheaver, G.; Moore, J.W.; Kauzlarich, J.J.; Kurtz, L.; Edgerton, M.T.; Edlich, R.F. Mechanical Performance of Surgical Sutures. Am. J. Surg. 1975, 130, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Karpiński, R.; Gajewski, J.; Szabelski, J.; Barta, D. Application of Neural Networks in Prediction of Tensile Strength of Absorbable Sutures. Appl. Comput. Sci. 2017, 13, 76–86. [Google Scholar] [CrossRef]
- Srinivasulu, K.; Kumar, N.D. A Review on Properties of Surgical Sutures and Applications in Medical Field. Int. J. Res. Eng. Technol. 2014, 2, 85–96. [Google Scholar]
- Callahan, T.L.; Lear, W.; Kruzic, J.J.; Maughan, C.B. Mechanical Properties of Commercially Available Nylon Sutures in the United States. J. Biomed. Mater. Res. 2017, 105, 815–819. [Google Scholar] [CrossRef]
- Zhou, Y.L.; Yang, Q.Q.; Zhang, L.; Tang, J.B. Nanoparticle-Coated Sutures Providing Sustained Growth Factor Delivery to Improve the Healing Strength of Injured Tendons. Acta Biomater. 2021, 124, 301–314. [Google Scholar] [CrossRef]
- Săvulescu, A.-F.; Cîrlan, C.; Blăjuț, F.-C.; Iordache, M.; Iordache-Petrescu, M.-I.; Ionescu, A.-B.; Lutencu, C.; Popa, L. Classic Suturing Materials Overview. Ind. Textila 2022, 73, 574–579. [Google Scholar] [CrossRef]
- Tobias, K.M.; Kidd, C.E.; Mulon, P.; Zhu, X. Tensile Properties of Synthetic, Absorbable Monofilament Suture Materials before and after Incubation in Phosphate-buffered Saline. Vet. Surg. 2020, 49, 550–560. [Google Scholar] [CrossRef]
- Müller, D.A.; Snedeker, J.G.; Meyer, D.C. Two-Month Longitudinal Study of Mechanical Properties of Absorbable Sutures Used in Orthopedic Surgery. J. Orthop. Surg. Res. 2016, 11, 111. [Google Scholar] [CrossRef]
- Karpiński, R.; Szabelski, J.; Maksymiuk, J. Seasoning Polymethyl Methacrylate (PMMA) Bone Cements with Incorrect Mix Ratio. Materials 2019, 12, 3073. [Google Scholar] [CrossRef]
- Szabelski, J.; Karpiński, R.; Krakowski, P.; Jojczuk, M.; Jonak, J.; Nogalski, A. Analysis of the Effect of Component Ratio Imbalances on Selected Mechanical Properties of Seasoned, Medium Viscosity Bone Cements. Materials 2022, 15, 5577. [Google Scholar] [CrossRef] [PubMed]
- Juarros-Basterretxea, J.; Aonso-Diego, G.; Postigo, Á.; Montes-Álvarez, P.; Menéndez-Aller, Á.; García-Cueto, E. Post-Hoc Tests in One-Way ANOVA: The Case for Normal Distribution. Methodology 2024, 20, 84–99. [Google Scholar] [CrossRef]
- Nanda, A.; Mohapatra, D.B.B.; Mahapatra, A.P.K.; Mahapatra, A.P.K.; Mahapatra, A.P.K. Multiple Comparison Test by Tukey’s Honestly Significant Difference (HSD): Do the Confident Level Control Type I Error. Int. J. Stat. Appl. Math. 2021, 6, 59–65. [Google Scholar] [CrossRef]
- Midway, S.; Robertson, M.; Flinn, S.; Kaller, M. Comparing Multiple Comparisons: Practical Guidance for Choosing the Best Multiple Comparisons Test. PeerJ 2020, 8, e10387. [Google Scholar] [CrossRef]
- Srinivas, T.R.; Ho, B.; Kang, J.; Kaplan, B. Post Hoc Analyses: After the Facts. Transplantation 2015, 99, 17–20. [Google Scholar] [CrossRef]
- Kim, H.-Y. Statistical Notes for Clinical Researchers: Post-Hoc Multiple Comparisons. Restor. Dent. Endod. 2015, 40, 172. [Google Scholar] [CrossRef]
- He, W.; Benson, R. Polymeric Biomaterials. In Applied Plastics Engineering Handbook; Elsevier: Amsterdam, The Netherlands, 2017; pp. 145–164. ISBN 978-0-323-39040-8. [Google Scholar]
- Kim, J.-C.; Lee, Y.-K.; Lim, B.-S.; Rhee, S.-H.; Yang, H.-C. Comparison of Tensile and Knot Security Properties of Surgical Sutures. J. Mater. Sci. Mater. Med. 2007, 18, 2363–2369. [Google Scholar] [CrossRef]
- Zhu, Q.; Liu, L.; Ma, P. Effect of Structural Parameters, Knotting Methods, and Wet State on the Tensile Properties of Sutures for Orthopedic Surgery. J. Ind. Text. 2024, 54, 15280837241257928. [Google Scholar] [CrossRef]
- Herring, S.W. Mechanical Influences on Suture Development and Patency. Craniofacial Sutures 2008, 12, 41–56. [Google Scholar]
- Andryszczyk, M.; Topoliński, T. Systematic Review and Meta-Analysis of Surgical Suture Strength According to the Type, Structure and Geometry of Suture Materials. Acta Bioeng. Biomech. 2021, 23, 1–10. [Google Scholar]
- Tomihata, K.; Suzuki, M.; Ikada, Y. The pH Dependence of Monofilament Sutures on Hydrolytic Degradation. J. Biomed. Mater. Res. 2001, 58, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Ping Ooi, C.; Cameron, R.E. The Hydrolytic Degradation of Polydioxanone (PDSII) Sutures. Part I: Morphological Aspects. J. Biomed. Mater. Res. 2002, 63, 280–290. [Google Scholar] [CrossRef] [PubMed]
- Gupta, B.; Jain, R.; Anjum, N.; Singh, H. Preparation of Antimicrobial Sutures by Preirradiation Grafting of Acrylonitrile onto Polypropylene Monofilament. III. Hydrolysis of the Grafted Suture. J. Appl. Polym. Sci. 2004, 94, 2509–2516. [Google Scholar] [CrossRef]
- Deeken, C.R.; Eliason, B.J.; Pichert, M.D.; Grant, S.A.; Frisella, M.M.; Matthews, B.D. Differentiation of Biologic Scaffold Materials Through Physicomechanical, Thermal, and Enzymatic Degradation Techniques. Ann. Surg. 2012, 255, 595–604. [Google Scholar] [CrossRef]
- Sun, L.; Wanasekara, N.; Chalivendra, V.; Calvert, P. Nano-Mechanical Studies on Polyglactin Sutures Subjected to in Vitro Hydrolytic and Enzymatic Degradation. J. Nanosci. Nanotechnol. 2015, 15, 93–99. [Google Scholar] [CrossRef]
- Chu, C.C.; Williams, D.F. The Effect of Gamma Irradiation on the Enzymatic Degradation of Polyglycolic Acid Absorbable Sutures. J. Biomed. Mater. Res. 1983, 17, 1029–1040. [Google Scholar] [CrossRef]
- Daood, U.; Ilyas, M.S.; Ashraf, M.; Akbar, M.; Asif, A.; Khan, A.S.; Sidhu, P.; Sheikh, Z.; Davamani, F.; Matinlinna, J.; et al. A Novel Coated Suture Displays Antimicrobial Activity without Compromising Structural Properties. J. Oral. Maxillofac. Surg. 2024, 82, S027823912400329X. [Google Scholar] [CrossRef]
- Chopra, A.; Cecil, A.; Eshwaramoorthy, R.; John, R.S. An in Vitro Study for the Evaluation of Morphological and Biochemical Characteristics of Absorbable Sutures Coated with Genistein and Nicotine. Eur. J. Clin. Exp. Med. 2023, 21, 742–749. [Google Scholar] [CrossRef]
- Nguyen, T.T.; Langenfeld, J.G.; Reinhart, B.C.; Lyden, E.I.; Campos, A.S.; Wadman, M.C.; Jamison, M.R.; Morin, S.A.; Barksdale, A.N. An Evaluation of the Usability and Durability of 3D Printed versus Standard Suture Materials. Wound Repair. Regen. 2024, 32, 229–233. [Google Scholar] [CrossRef]
- Wickramasinghe, S.; Peng, C.; Ladani, R.; Tran, P. Analysing Fracture Properties of Bio-Inspired 3D Printed Suture Structures. Thin-Walled Struct. 2022, 176, 109317. [Google Scholar] [CrossRef]
- Nicolás, P.; Lassalle, V.L.; Ferreira, M.L. Evaluation of Biocatalytic Pathways in the Synthesis of Polyesters: Towards a Greener Production of Surgical Sutures. Polym. Adv. Techs 2023, 34, 64–78. [Google Scholar] [CrossRef]
- Rethinam, S.; Thotapalli Parvathaleswara, S.; Nandhagobal, G.; Alagumuthu, T.; Robert, B. Preparation of Absorbable Surgical Suture: Novel Approach in Biomedical Application. J. Drug Deliv. Sci. Technol. 2018, 47, 454–460. [Google Scholar] [CrossRef]
- Zhukovskii, V.A. Problems and Prospects for Development and Production of Surgical Suture Materials. Fibre Chem. 2008, 40, 208–216. [Google Scholar] [CrossRef]
- Cannizzo, S.A.; Roe, S.C.; Harms, C.A.; Stoskopf, M.K. Effect of Water Temperature on the Hydrolysis of Two Absorbable Sutures Used in Fish Surgery. FACETS 2017, 1, 44–54. [Google Scholar] [CrossRef]
- Ramanna, P.K.; Mishra, D.; Lahiri, B.; Awasthi, N.; Das, A.; Ravi, R.V. Impact of Fluoridated Mouthwashes on Strength and Durability of Three Different Synthetic Absorbable Suturing Materials: An In Vitro Study. J. Contemp. Dent. Pract. 2022, 23, 431–436. [Google Scholar] [CrossRef]
- Abullais, S.; Al-Qahtani, N.; Naqash, T.; Khan, A.; Arora, S.; Bhavikatti, S. Evaluation of Mechanical Properties of Three Commonly Used Suture Materials for Clinical Oral Applications: An in Vitro Study. VSP 2022, 79, 155–161. [Google Scholar] [CrossRef]
- Liu, Z.; Zhao, L.; Wang, Y.; Dai, K.; Lu, A.; Zhao, P. Application of Dural Suturing in the Endoscopic Endonasal Approach to the Sellar Region. Front. Surg. 2022, 9, 944663. [Google Scholar] [CrossRef]
- Karpiński, R.; Szabelski, J.; Krakowski, P.; Jojczuk, M.; Jonak, J.; Nogalski, A. Evaluation of the Effect of Selected Physiological Fluid Contaminants on the Mechanical Properties of Selected Medium-Viscosity PMMA Bone Cements. Materials 2022, 15, 2197. [Google Scholar] [CrossRef]
- Karpiński, R.; Szabelski, J.; Maksymiuk, J. Effect of Physiological Fluids Contamination on Selected Mechanical Properties of Acrylate Bone Cement. Materials 2019, 12, 3963. [Google Scholar] [CrossRef]
- Okamura, T.; Ikeda, T.; Honda, T.; Ichikawa, T.; Nakao, K. Innovative Double Suturing Technique for Gastric Endoscopic Hand Suturing after Endoscopic Submucosal Dissection: A Case Report and Technique Description. Endoscopy 2024, 56, E285–E287. [Google Scholar] [CrossRef]
- Das, A.; Lahiri, B.; Singh, P.K.; Kumari, D.; Mishra, D.; Bhushan, P. Assessment of the Impact of Commonly Used Beverages on Durability of Suture Materials: An In Vitro Study. J. Pharm. Bioallied Sci. 2023, 15, S447–S450. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Wang, Y.; Ji, Y. Novel Method to Assess the Dynamic Tensile Properties of Sports Medicine Suture. J. Mech. Med. Biol. 2023, 24, 2350064. [Google Scholar] [CrossRef]
- Walton, R.A.; Liuzza, L.; Takawira, C.; Leonardi, C.; Lopez, M.J. Biocomposite Anchors Have Greater Yield Load and Energy Compared with All-Suture Anchors in an In Vitro Ovine Infraspinatus Tendon Repair Model. Arthrosc. Sports Med. Rehabil. 2024, 6, 100938. [Google Scholar] [CrossRef] [PubMed]
| Suture Group by Absorption Time | Estimated Retention Time of 50% of Initial Strength | Total Absorption Time |
|---|---|---|
| Short | 5–7 days | 42–56 days |
| Medium | 14–21 days | 60–90 days |
| Long | 28–35 days | 180–210 days |
| Extra-long | 90 days | approx. 390 days |
| Suture Name | Total Absorption Time | Material | Sample Applications |
|---|---|---|---|
| SafilQuick+ | ~42 days | Polyglycolic acid | Gynaecology, urology, dentistry, paediatric surgery, ophthalmology ligation |
| Monosyn Quick | 56 days | Glyconate (72% glycolide, 14% caprolactone, 14% trimethylene carbonate) | Plastic surgery, odontology and otolaryngology, gynaecology, urology |
| Novosyn | 56–70 days | Copolymer of 90% glycolide and 10% L-lactide Poly (glycolide and L-lactide 90/10) | Gastrointestinal surgery, gynaecology, trauma and orthopaedic surgery, ophthalmology, urology, skin suturing |
| Monosyn | 60–90 days | Glyconate (72% glycolide, 14% caprolactone, 14% trimethylene carbonate) | Gastrointestinal surgery, gynaecology, urology, skin suturing, ligature |
| MonoPlus | 180–210 days | Poly-p-dioxanone | Abdominal anastomoses, orthopaedics, paediatric cardiac surgery, vascular surgery, neurosurgery, transplantology |
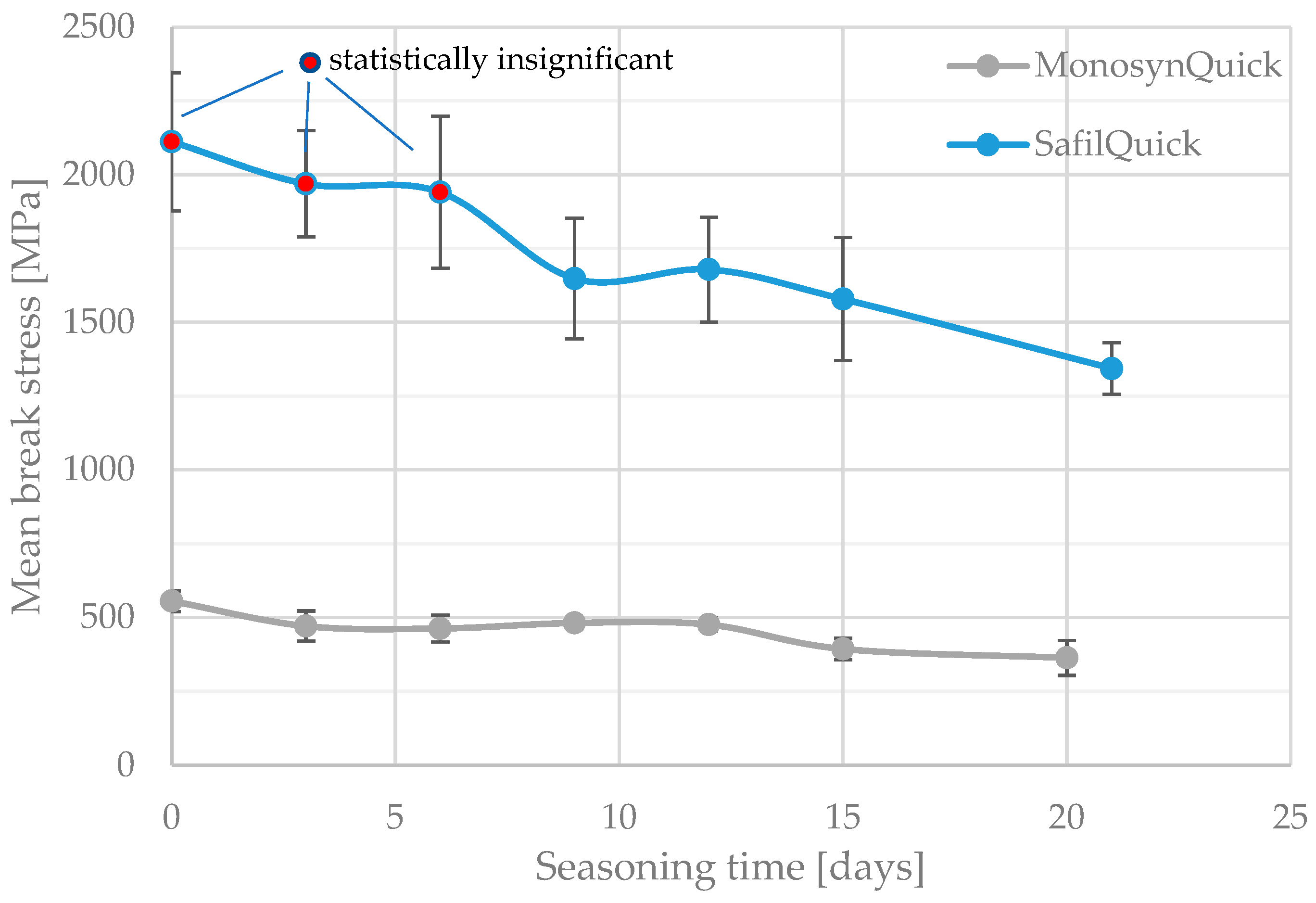
| Seasoning Time [Days] | No. of Specimens | Mean Break Stress [Mpa] | Break Stress SD [Mpa] | Groups of Homogeneous Results | Mean Strain at Break [mm] | Strain at Break SD [mm] | Groups of Homogeneous Results | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | 2 | 3 | ||||||
| 0 | 8 | 2111.74 | 233.95 | X | 24.06 | 2.51 | X | X | |||
| 3 | 8 | 1969.07 | 180.38 | X | 28.13 | 1.65 | X | ||||
| 6 | 8 | 1940.78 | 257.26 | X | X | 23.71 | 3.52 | X | |||
| 9 | 8 | 1647.90 | 204.73 | X | 22.00 | 3.44 | X | X | |||
| 12 | 8 | 1678.79 | 177.89 | X | X | 21.81 | 2.21 | X | X | ||
| 15 | 8 | 1579.04 | 208.33 | X | 21.01 | 2.10 | X | X | |||
| 21 | 8 | 1343.68 | 87.54 | X | 17.74 | 1.07 | X | ||||
| Seasoning Time [Days] | No. of Specimens | Mean Break Stress [Mpa] | Break Stress SD [Mpa] | Groups of Homogeneous Results | Mean Strain at Break [mm] | Strain at Break SD [mm] | Groups of Homogeneous Results | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 1 | ||||||
| 0 | 8 | 555.94 | 35.51 | X | 36.33 | 10.89 | X | |||
| 3 | 8 | 471.60 | 51.02 | X | X | X | 36.20 | 7.21 | X | |
| 6 | 8 | 463.24 | 45.84 | X | X | 36.25 | 2.92 | X | ||
| 9 | 8 | 482.01 | 10.20 | X | X | 37.63 | 1.90 | X | ||
| 12 | 6 | 476.52 | 21.30 | X | X | X | 38.82 | 1.38 | X | |
| 15 | 6 | 393.53 | 36.08 | X | X | 31.46 | 5.49 | X | ||
| 20 | 7 | 363.49 | 59.02 | X | 29.62 | 6.37 | X | |||
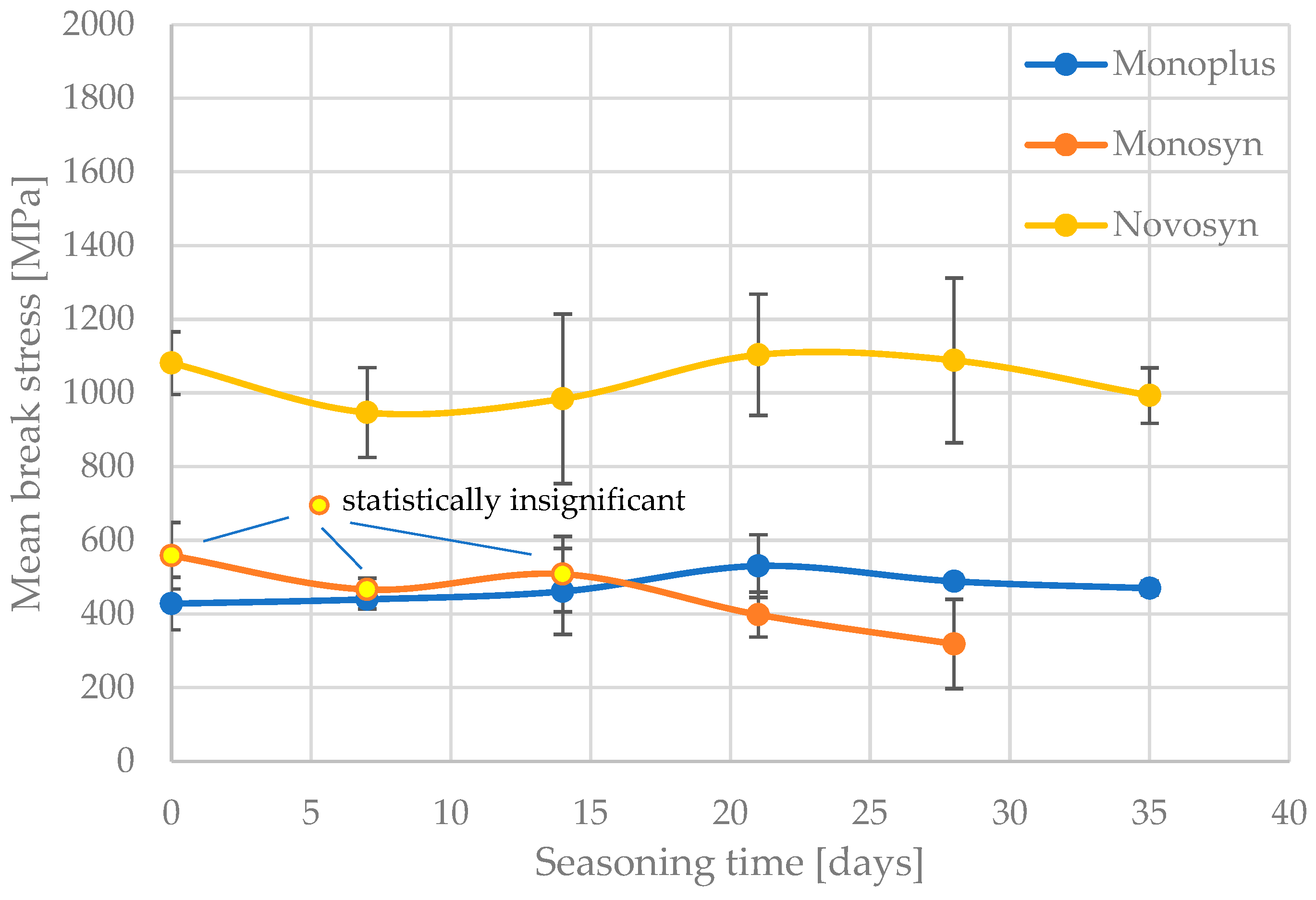
| Seasoning Time [Days] | No. of Specimens | Mean Break Stress [Mpa] | Break Stress SD [Mpa] | Groups of Homogeneous Results | Mean Strain at Break [mm] | Strain at Break SD [mm] | Groups of Homogeneous Results | |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 2 | ||||||
| 0 | 8 | 1081.18 | 85.03 | X | 37.79 | 4.85 | X | |
| 7 | 8 | 946.87 | 121.86 | X | 24.88 | 9.25 | X | X |
| 14 | 8 | 984.25 | 230.17 | X | 21.15 | 13.09 | X | |
| 21 | 8 | 1103.74 | 164.40 | X | 28.77 | 9.36 | X | X |
| 28 | 8 | 1088.61 | 223.77 | X | 21.32 | 7.95 | X | |
| 35 | 8 | 993.05 | 75.38 | X | 31.32 | 4.53 | X | X |
| 42 | 8 | 1010.79 | 85.03 | X | 32.83 | 4.85 | X | X |
| Seasoning Time [Days] | No. of Specimens | Mean Break Stress [Mpa] | Break Stress SD [Mpa] | Groups of Homogeneous Results | Mean Strain at Break [mm] | Strain at Break SD [mm] | Groups of Homogeneous Results | ||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | ||||||
| 0 | 7 | 558.21 | 90.27 | X | 40.28 | 16.27 | X | ||
| 7 | 7 | 466.66 | 30.72 | X | X | 36.05 | 11.92 | X | |
| 14 | 7 | 508.28 | 102.63 | X | X | 40.62 | 12.51 | X | |
| 21 | 7 | 398.41 | 60.73 | X | X | 34.69 | 9.37 | X | |
| 28 | 7 | 318.52 | 121.06 | X | 31.29 | 9.40 | X | ||
| Seasoning Time [Days] | No. of Specimens | Mean Break Stress [Mpa] | Break Stress SD [Mpa] | Groups of Homogeneous Results | Mean Strain at Break [mm] | Strain at Break SD [mm] | Groups of Homogeneous Results | |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 2 | ||||||
| 0 | 7 | 428.34 | 71.57 | X | 24.91 | 14.22 | X | |
| 7 | 7 | 439.76 | 25.79 | X | 26.58 | 6.98 | X | X |
| 14 | 7 | 461.58 | 116.72 | X | 33.61 | 11.68 | X | X |
| 21 | 7 | 530.19 | 85.27 | X | 34.09 | 4.96 | X | X |
| 28 | 7 | 488.60 | 16.44 | X | 38.11 | 10.61 | X | X |
| 35 | 7 | 470.07 | 19.27 | X | 45.95 | 4.27 | X | |
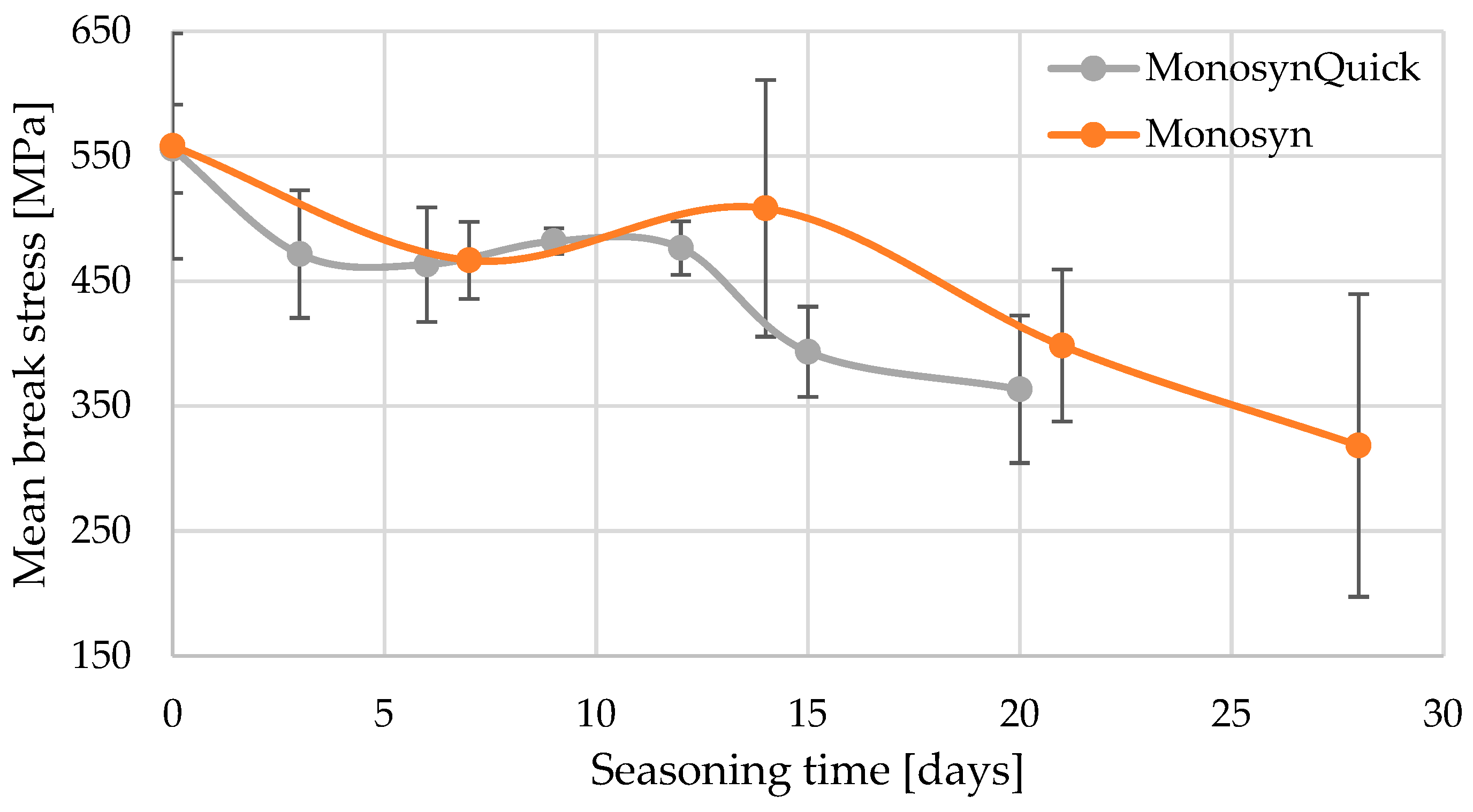
| Seasoning Time [Days] | Monosyn Variant | Mean Break Stress [MPa] | Break Stress SD [MPa] | Groups of Homogeneous Results | ||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||||
| 0 | - | 558.21 | 90.27 | X | ||||
| 0 | Quick | 555.94 | 35.51 | X | X | |||
| 3 | Quick | 471.60 | 51.02 | X | X | X | X | X |
| 6 | Quick | 463.24 | 45.84 | X | X | X | X | X |
| 7 | - | 466.66 | 30.72 | X | X | X | X | |
| 9 | Quick | 482.01 | 10.20 | X | X | X | X | |
| 12 | Quick | 476.52 | 21.30 | X | X | X | X | X |
| 14 | - | 508,28 | 102.63 | X | X | |||
| 15 | Quick | 393.53 | 36.08 | X | X | X | ||
| 20 | Quick | 363.49 | 59.02 | X | X | |||
| 21 | - | 398.41 | 60.73 | X | X | X | ||
| 28 | - | 318.52 | 121.06 | X | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szabelski, J.; Karpiński, R. Short-Term Hydrolytic Degradation of Mechanical Properties of Absorbable Surgical Sutures: A Comparative Study. J. Funct. Biomater. 2024, 15, 273. https://doi.org/10.3390/jfb15090273
Szabelski J, Karpiński R. Short-Term Hydrolytic Degradation of Mechanical Properties of Absorbable Surgical Sutures: A Comparative Study. Journal of Functional Biomaterials. 2024; 15(9):273. https://doi.org/10.3390/jfb15090273
Chicago/Turabian StyleSzabelski, Jakub, and Robert Karpiński. 2024. "Short-Term Hydrolytic Degradation of Mechanical Properties of Absorbable Surgical Sutures: A Comparative Study" Journal of Functional Biomaterials 15, no. 9: 273. https://doi.org/10.3390/jfb15090273
APA StyleSzabelski, J., & Karpiński, R. (2024). Short-Term Hydrolytic Degradation of Mechanical Properties of Absorbable Surgical Sutures: A Comparative Study. Journal of Functional Biomaterials, 15(9), 273. https://doi.org/10.3390/jfb15090273








