Comparative Biomechanical Evaluation of Novel Screwless Retained Dental Implant Prosthesis: A 3D Finite Element Analysis
Abstract
:1. Introduction
2. Materials and Methods
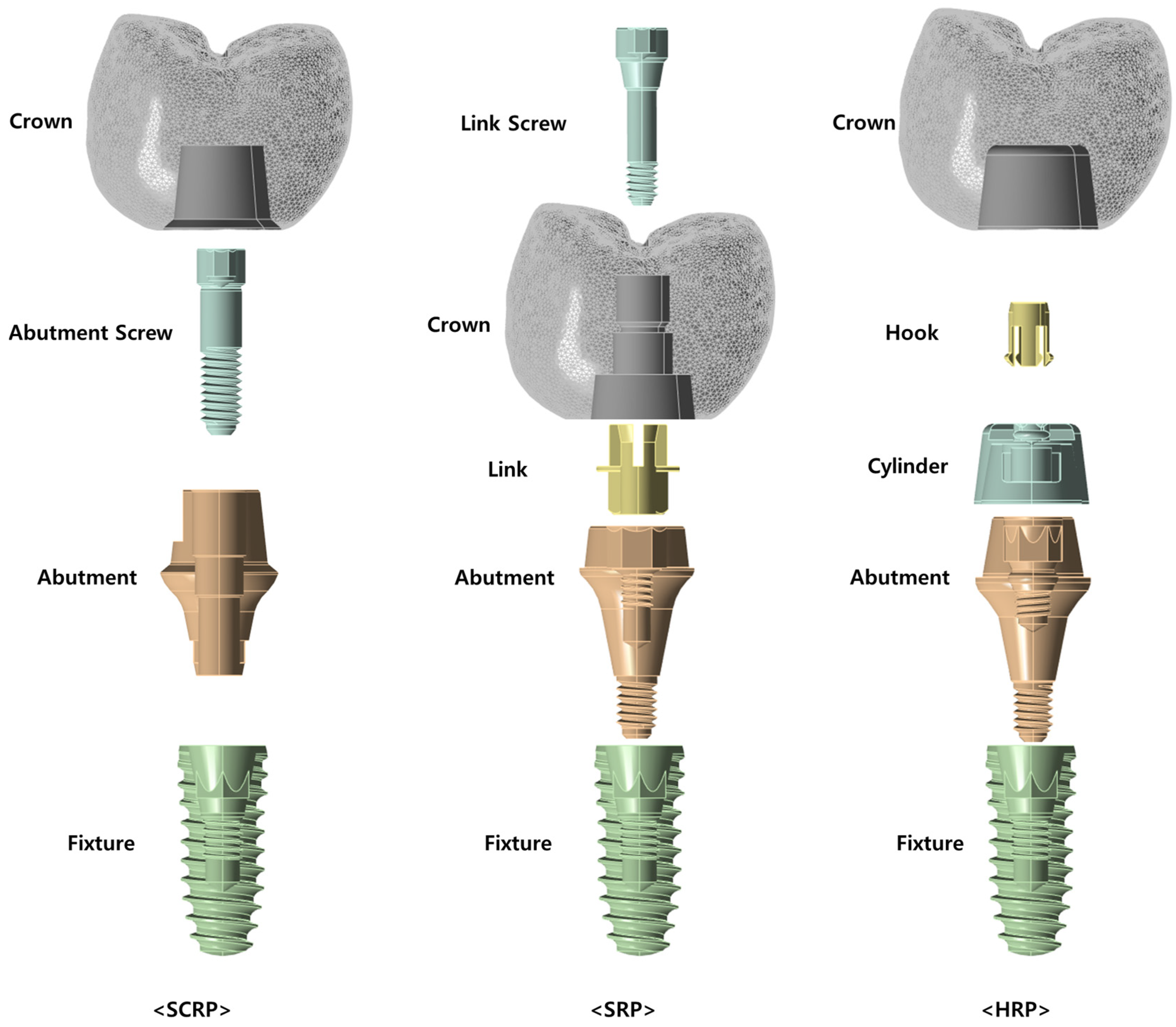
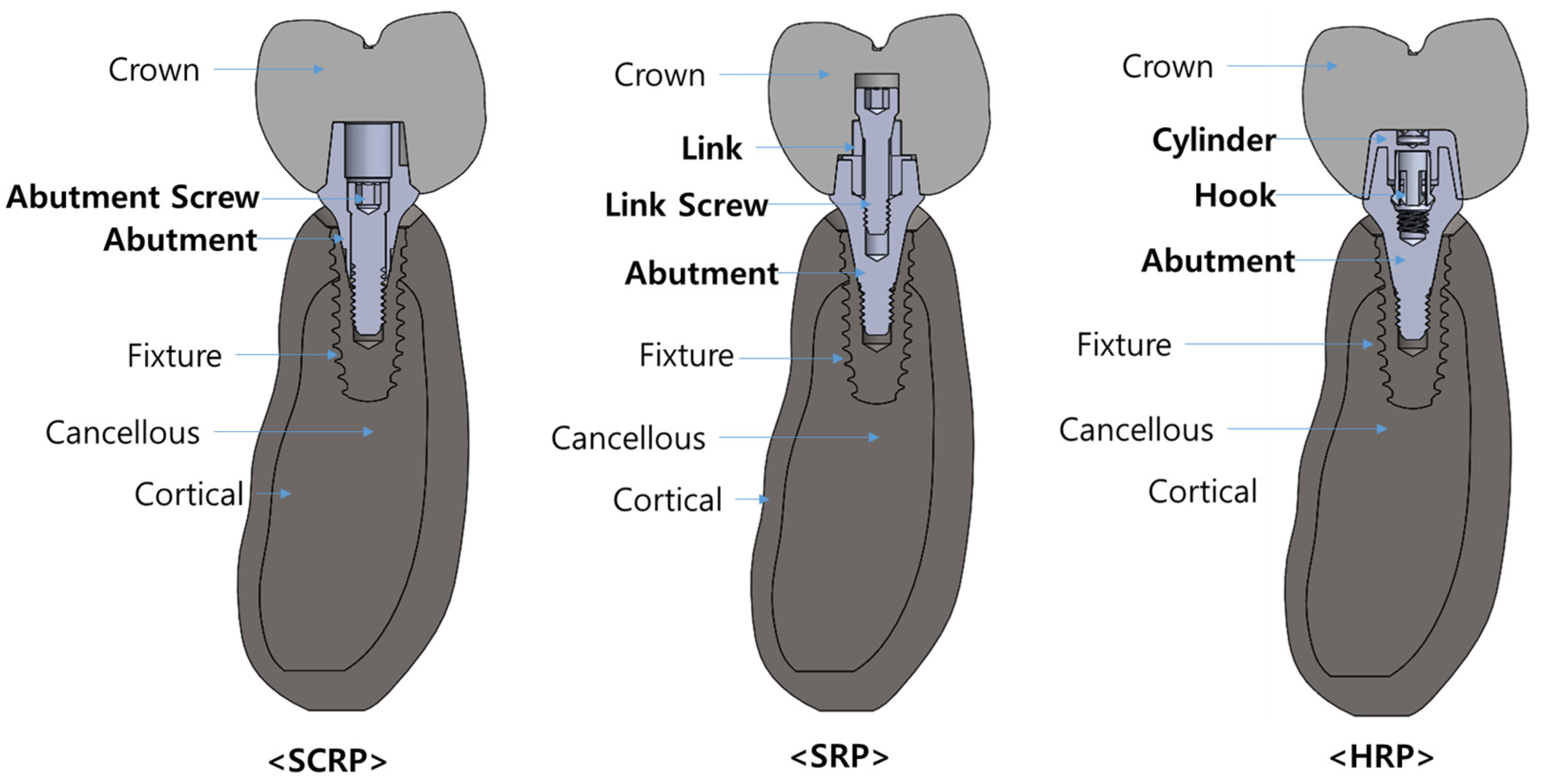
2.1. 3D Model Design
2.2. Material Properties
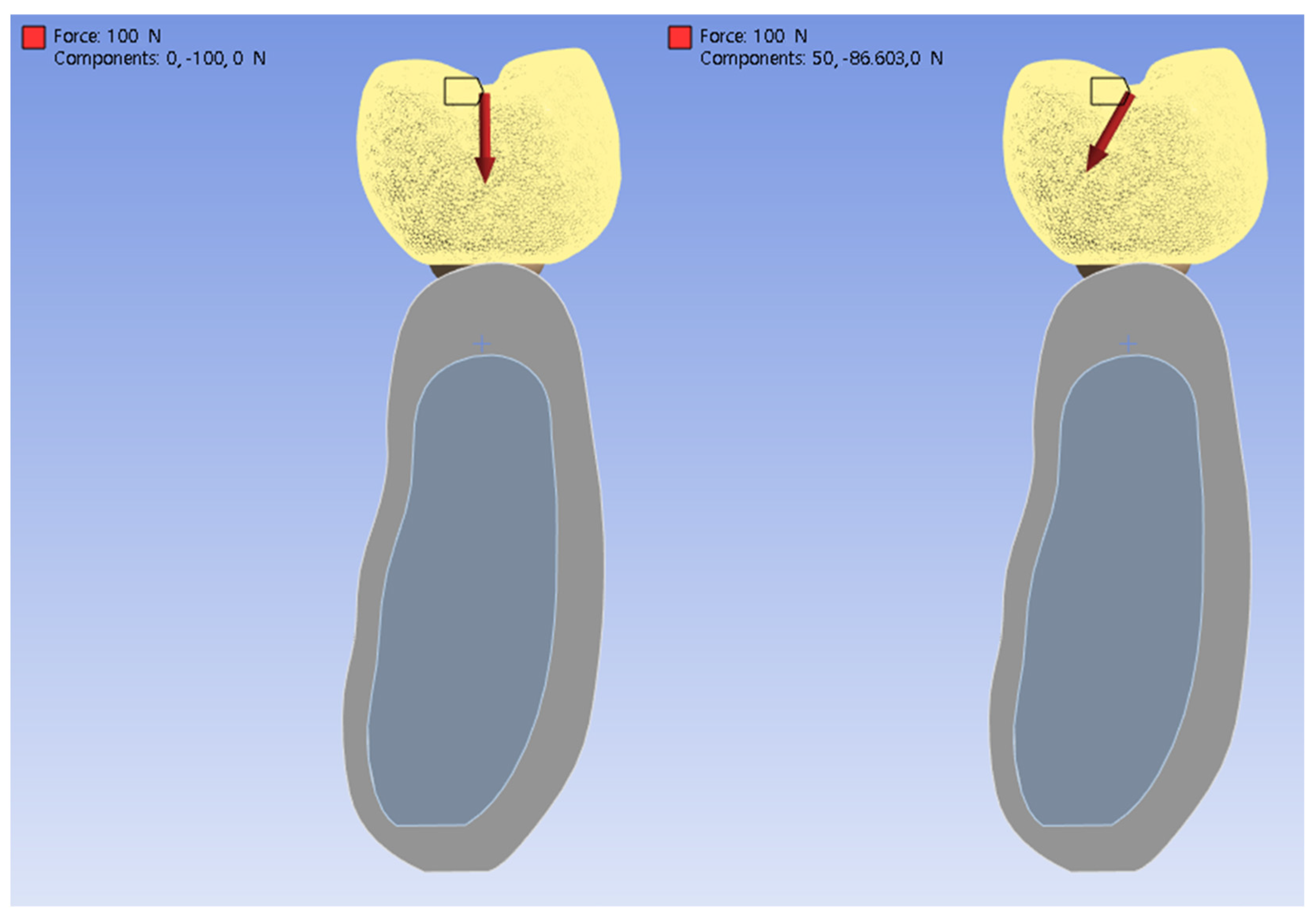
2.3. Loading Conditions
2.4. Finite Element Analysis
3. Results
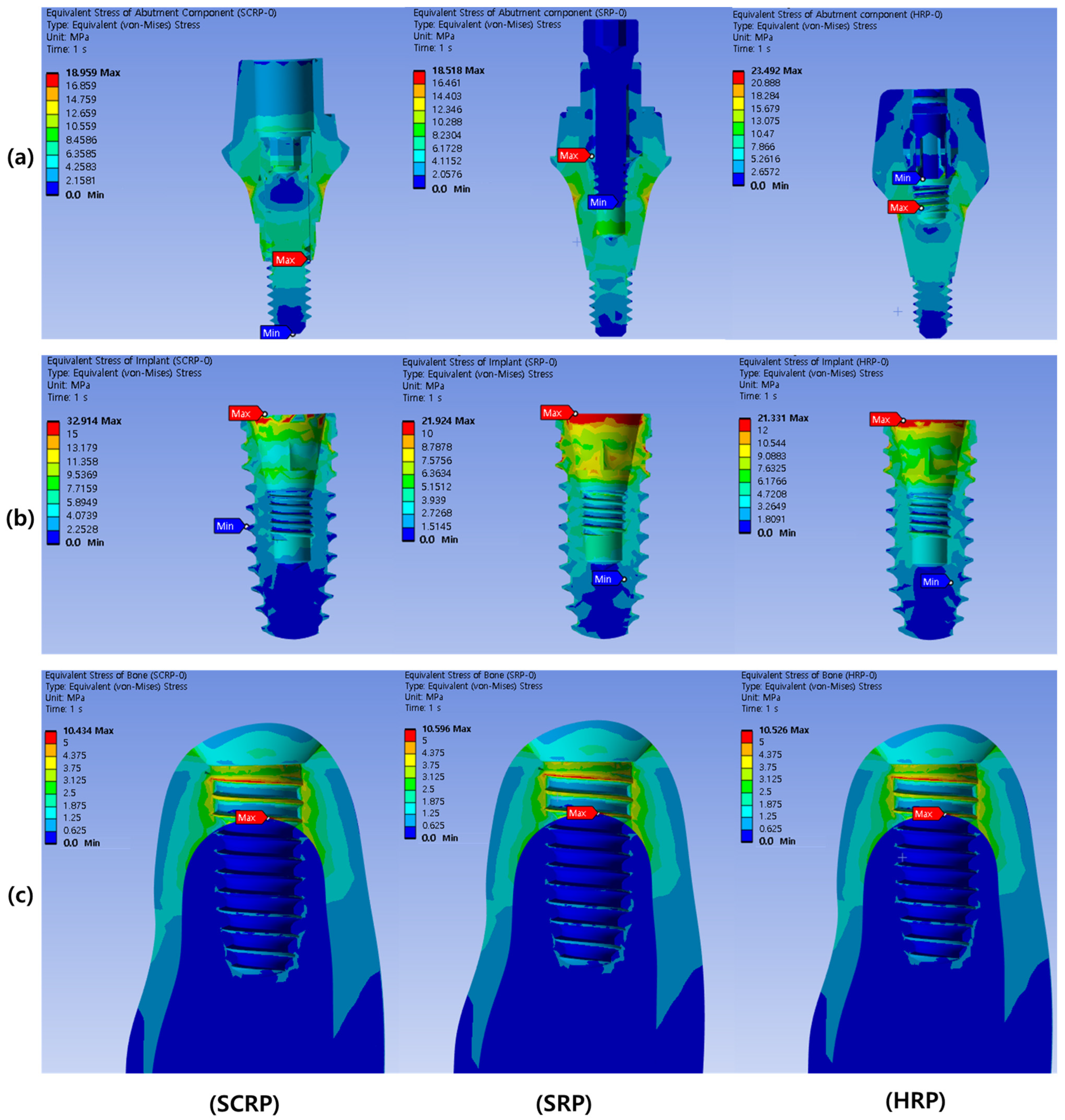
3.1. Bio-Mechanical Behaviors Under Vertical Loading Conditions
3.2. Bio-Mechanical Behaviors Under Oblique Loading Conditions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lindh, T.; Gunne, J.; Tillberg, A.; Molin, M. A meta-analysis of implants in partial edentulism. Clin. Oral Implants Res. 1998, 9, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Moraschini, V.; Poubel, L.d.C.; Ferreira, V.; dos Sp Barboza, E. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-J.; Lee, J.-H.; Kim, J.C.; Lee, J.-B.; Yeo, I.-S.L. Biological responses to the transitional area of dental implants: Material-and structure-dependent responses of peri-implant tissue to abutments. Materials 2019, 13, 72. [Google Scholar] [CrossRef]
- Li, J.; Jansen, J.A.; Walboomers, X.F.; van den Beucken, J.J. Mechanical aspects of dental implants and osseointegration: A narrative review. J. Mech. Behav. Biomed. Mater. 2020, 103, 103574. [Google Scholar] [CrossRef]
- Alemayehu, D.B.; Jeng, Y.R. Three-Dimensional Finite Element Investigation into Effects of Implant Thread Design and Loading Rate on Stress Distribution in Dental Implants and Anisotropic Bone. Materials 2021, 14, 6974. [Google Scholar] [CrossRef]
- Chun, H.J.; Cheong, S.Y.; Han, J.H.; Heo, S.J.; Chung, J.P.; Rhyu, I.C.; Choi, Y.C.; Baik, H.K.; Ku, Y.; Kim, M.H. Evaluation of design parameters of osseointegrated dental implants using finite element analysis. J. Oral Rehabil. 2002, 29, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-H.; Kim, J.C.; Kim, H.-Y.; Yeo, I.-S.L. Influence of Connections and Surfaces of Dental Implants on Marginal Bone Loss: A Retrospective Study Over 7 to 19 Years. Int. J. Oral Maxillofac. Implant. 2020, 35, 1195–1202. [Google Scholar] [CrossRef] [PubMed]
- Herekar, M.G.; Patil, V.N.; Mulani, S.S.; Sethi, M.; Padhye, O. The influence of thread geometry on biomechanical load transfer to bone: A finite element analysis comparing two implant thread designs. Dent. Res. J. 2014, 11, 489. [Google Scholar]
- Lee, J.-H.; Jang, H.Y.; Lee, S.Y. Finite element analysis of dental implants with zirconia crown restorations: Conventional cement-retained vs. cementless screw-retained. Materials 2021, 14, 2666. [Google Scholar] [CrossRef]
- Michalakis, K.X.; Hirayama, H.; Garefis, P.D. Cement-retained versus screw-retained implant restorations: A critical review. Int. J. Oral Maxillofac. Implant. 2003, 18, 719–728. [Google Scholar]
- Chee, W.; Jivraj, S. Screw versus cemented implant supported restorations. Br. Dent. J. 2006, 201, 501–507. [Google Scholar] [CrossRef]
- Petrie, C.S.; Williams, J.L. Comparative evaluation of implant designs: Influence of diameter, length, and taper on strains in the alveolar crest: A three-dimensional finite-element analysis. Clin. Oral Implants Res. 2005, 16, 486–494. [Google Scholar] [CrossRef]
- Pierrisnard, L.; Hure, G.; Barquins, M.; Chappard, D. Two dental implants designed for immediate loading: A finite element analysis. Int. J. Oral Maxillofac. Implant. 2002, 17, 353–362. [Google Scholar]
- Dogus, S.M.; Kurtz, K.S.; Watanabe, I.; Griggs, J.A. Effect of engaging abutment position in implant-borne, screw-retained three-unit fixed cantilevered prostheses. J. Prosthodont. Implant. Esthet. Reconstr. Dent. 2011, 20, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Guichet, D.L.; Caputo, A.A.; Choi, H.; Sorensen, J.A. Passivity of fit and marginal opening in screw-or cement-retained implant fixed partial denture designs. Int. J. Oral Maxillofac. Implant. 2000, 15, 239–246. [Google Scholar]
- Cho, H.-J.; Jeon, J.-Y.; Ahn, S.-J.; Lee, S.-W.; Chung, J.-R.; Park, C.-J.; Hwang, K.-G. The preliminary study for three-dimensional alveolar bone morphologic characteristics for alveolar bone restoration. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 33. [Google Scholar] [CrossRef] [PubMed]
- Schindler, H.J.; Stengel, E.; Spiess, W.E. Feedback control during mastication of solid food textures—A clinical-experimental study. J. Prosthet. Dent. 1998, 80, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Yamanishi, Y.; Yamaguchi, S.; Imazato, S.; Nakano, T.; Yatani, H. Influences of implant neck design and implant-abutment joint type on peri-implant bone stress and abutment micromovement: Three-dimensional finite element analysis. Dent. Mater. 2012, 28, 1126–1133. [Google Scholar] [CrossRef]
- Yokoyama, S.; Wakabayashi, N.; Shiota, M.; Ohyama, T. The influence of implant location and length on stress distribution for three-unit implant-supported posterior cantilever fixed partial dentures. J. Prosthet. Dent. 2004, 91, 234–240. [Google Scholar] [CrossRef]
- Tabata, L.F.; Rocha, E.P.; Barao, V.A.; Assuncao, W.G. Platform switching: Biomechanical evaluation using three-dimensional finite element analysis. Int. J. Oral Maxillofac. Implant. 2011, 26, 482–491. [Google Scholar]
- Natali, A.N.; Pavan, P.G.; Ruggero, A.L. Analysis of bone-implant interaction phenomena by using a numerical approach. Clin. Oral Implants Res. 2006, 17, 67–74. [Google Scholar] [CrossRef]
- Aalaei, S.; Naraki, Z.R.; Nematollahi, F.; Beyabanaki, E.; Rad, A.S. Stress distribution pattern of screw-retained restorations with segmented vs. non-segmented abutments: A finite element analysis. J. Dent. Res. Dent. Clin. Dent. Prospect. 2017, 11, 149. [Google Scholar] [CrossRef] [PubMed]
- Rangert, B.; Gunne, J.; Glantz, P.O.; Svensson, A. Vertical load distribution on a three-unit prosthesis supported by a natural tooth and a single Brånemark implant. An in vivo study. Clin. Oral Implants Res. 1995, 6, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Gomes, E.A.; Assunção, W.G.; Tabata, L.F.; Barão, V.A.R.; Delben, J.A.; de Sousa, E.A.C. Effect of passive fit absence in the prosthesis/implant/retaining screw system: A two-dimensional finite element analysis. J. Craniofac. Surg. 2009, 20, 2000–2005. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Shindoi, N.; Hosokawa, R.; Tsuga, K.; Akagawa, Y. A biomechanical effect of wide implant placement and offset placement of three implants in the posterior partially edentulous region. J. Oral Rehabil. 2000, 27, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Siadat, H.; Hashemzadeh, S.; Geramy, A.; Bassir, S.H.; Alikhasi, M. Effect of offset implant placement on the stress distribution around a dental implant: A three-dimensional finite element analysis. J. Oral Implantol. 2015, 41, 646–651. [Google Scholar] [CrossRef] [PubMed]
- Pellizzer, E.P.; Falcón-Antenucci, R.M.; de Carvalho, P.S.P.; Sánchez, D.M.I.K.; Rinaldi, G.A.T.; de Aguirre, C.C.; Goiato, M.C. Influence of implant angulation with different crowns on stress distribution. J. Craniofac. Surg. 2011, 22, 434–437. [Google Scholar] [CrossRef] [PubMed]

| Component | Modulus of Elasticity (GPa) | Poisson’s Ratio (ν) | Density (kg/m3) |
|---|---|---|---|
| Cancellous Bone | 1.3 | 0.30 | 500 |
| Cortical Bone | 13 | 0.30 | 1180 |
| Titanium (Ti-Gr4) (Fixture) | 103 | 0.33 | 4620 |
| Titanium (Ti-6Al-4V) (Abutment, Screw, Link, Link Screw, Cylinder, Hook) | 103 | 0.33 | 4620 |
| Zirconia | 200 | 0.31 | 6090 |
| Components | SCRP | SRP | HRP |
|---|---|---|---|
| Abutment Component (Stress) | 18.96 MPa | 18.52 MPa | 23.49 MPa |
| Implant (stress) | 32.91 MPa | 21.92 MPa | 21.33 MPa |
| Bone (stress) | 10.43 MPa | 10.60 MPa | 10.54 MPa |
| Bone (strain) | 0.00108 mm/mm | 0.00110 mm/mm | 0.00109 mm/mm |
| Components | SCRP | SRP | HRP |
|---|---|---|---|
| Abutment Component (Stress) | 218.42 MPa | 185.07 MPa | 187.60 MPa |
| Implant (stress) | 262.24 MPa | 187.64 MPa | 187.50 MPa |
| Bone (stress) | 32.32 MPa | 32.22 MPa | 30.72 MPa |
| Bone (strain) | 0.00238 | 0.00237 | 0.00235 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.-S.; Kim, J.; Lim, J.; Ryu, J.-J. Comparative Biomechanical Evaluation of Novel Screwless Retained Dental Implant Prosthesis: A 3D Finite Element Analysis. J. Funct. Biomater. 2025, 16, 39. https://doi.org/10.3390/jfb16020039
Lee K-S, Kim J, Lim J, Ryu J-J. Comparative Biomechanical Evaluation of Novel Screwless Retained Dental Implant Prosthesis: A 3D Finite Element Analysis. Journal of Functional Biomaterials. 2025; 16(2):39. https://doi.org/10.3390/jfb16020039
Chicago/Turabian StyleLee, Ki-Sun, Jaeyeol Kim, JaeHyung Lim, and Jae-Jun Ryu. 2025. "Comparative Biomechanical Evaluation of Novel Screwless Retained Dental Implant Prosthesis: A 3D Finite Element Analysis" Journal of Functional Biomaterials 16, no. 2: 39. https://doi.org/10.3390/jfb16020039
APA StyleLee, K.-S., Kim, J., Lim, J., & Ryu, J.-J. (2025). Comparative Biomechanical Evaluation of Novel Screwless Retained Dental Implant Prosthesis: A 3D Finite Element Analysis. Journal of Functional Biomaterials, 16(2), 39. https://doi.org/10.3390/jfb16020039







