Orthodontic Ceramic Bracket Removal Using Lasers: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Focused Question
2.2. Protocol
2.3. Eligibility Criteria
- •
- Laser debonding;
- •
- Use of ceramic brackets;
- •
- Use of all types of lasers;
- •
- In vitro and in vivo studies;
- •
- Studies published in English;
- •
- Full-text availability.
- •
- Use of metal brackets;
- •
- Use of forceps or ultrasound to debond brackets;
- •
- Review articles;
- •
- Duplicated publications.
2.4. Information Sources, Search Strategy, and Study Selection
2.5. Data Collection and Data Items
2.6. Assessing Risk of Bias in Individual Studies
2.7. Quality Assessment
3. Results
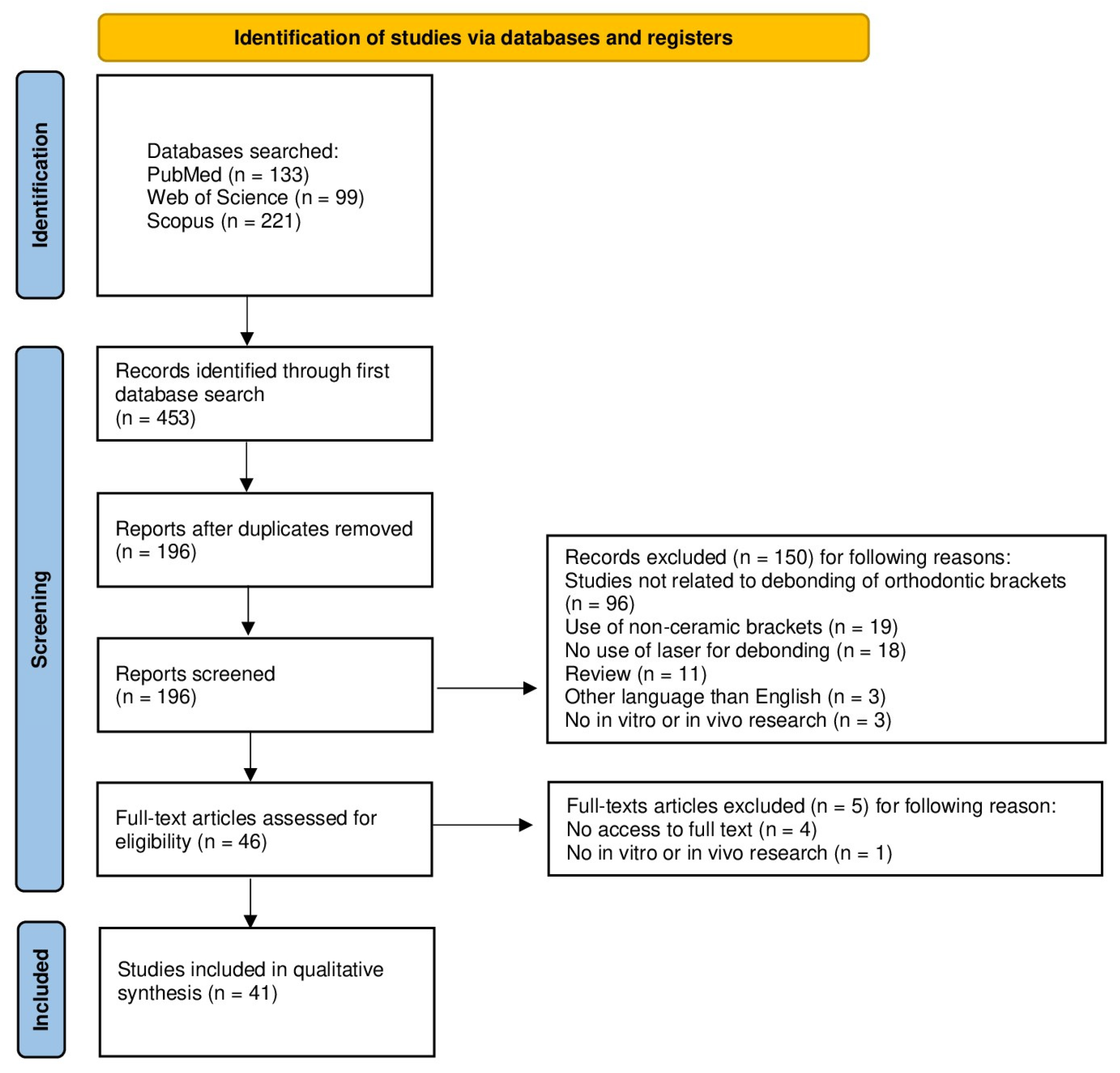
3.1. Study Selection
3.2. General Characteristics of the Included Studies
3.2.1. CO2 Laser Debonding
3.2.2. Er:YAG (Erbium–Yttrium, Aluminum, Garnet) Laser Debonding
3.2.3. Diode Laser Debonding
3.2.4. Er,Cr:YSGG (Erbium, Chromium–Yttrium, Scandium, Gallium, Garnet) Laser Debonding
3.2.5. Nd:YAG (Neodymium–Yttrium, Aluminum, Garnet) Laser Debonding
3.2.6. Tm:YAP (Thulium–Yttrium, Aluminum, Perovskite) Laser Debonding
3.3. Main Study Outcomes
3.4. Quality Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Russell, J.S. Current Products and Practice. J. Orthod. 2005, 32, 146–163. [Google Scholar] [CrossRef] [PubMed]
- Woś, P.; Kiryk, S.; Dyl, T.; Kiryk, J.; Horodniczy, T.; Szablińska, M.; Dubowik, M.A.; Dobrzyński, W.; Mikulewicz, M.; Matys, J.; et al. Laser Applications in Metal Orthodontic Bracket Debonding: A Systematic Review. Appl. Sci. 2025, 15, 927. [Google Scholar] [CrossRef]
- Khalil, A.S.; Tamish, N.M.; Elkalza, A.R. Assessment of Chemical, Ultrasonic, Diode Laser, and Er:YAG Laser Application on Debonding of Ceramic Brackets. BMC Oral Health 2022, 22, 79. [Google Scholar] [CrossRef] [PubMed]
- Dhannawat, P.K.; Gilani, R.; Shrivastav, S.S.; Kamble, R.H.; Murarka, S.P.; Rathi, S.S.; Vishnani, R. Debonding Techniques—A Review. J. Evol. Med. Dent. Sci. 2021, 10, 3430–3435. [Google Scholar] [CrossRef]
- Subramani, K.; Bollu, P. Debonding of Orthodontic Ceramic Brackets: A Comprehensive Review of the Literature—Part 1. IP Indian J. Orthod. Dentofac. Res. 2020, 6, 109–113. [Google Scholar] [CrossRef]
- Subramani, K.; Bollu, P. Debonding of Orthodontic Ceramic Brackets: A Comprehensive Review of the Literature—Part 2. IP Indian J. Orthod. Dentofac. Res. 2020, 6, 114–119. [Google Scholar] [CrossRef]
- Suliman, S.N.; Trojan, T.M.; Tantbirojn, D.; Versluis, A. Enamel Loss Following Ceramic Bracket Debonding: A Quantitative Analysis in Vitro. Angle Orthod. 2015, 85, 651–656. [Google Scholar] [CrossRef]
- Grocholewicz, K. Effect of Orthodontic Debonding and Adhesive Removal on the Enamel—Current Knowledge and Future Perspectives—A Systematic Review. Med. Sci. Monit. 2014, 20, 1991–2001. [Google Scholar] [CrossRef]
- Vidor, M.M.; Felix, R.P.; Marchioro, E.M.; Hahn, L. Enamel Surface Evaluation after Bracket Debonding and Different Resin Removal Methods. Dental Press J. Orthod. 2015, 20, 61–67. [Google Scholar] [CrossRef]
- Nakada, N.; Uchida, Y.; Inaba, M.; Kaetsu, R.; Shimizu, N.; Namura, Y.; Motoyoshi, M. Pain and Removal Force Associated with Bracket Debonding: A Clinical Study. J. Appl. Oral Sci. 2021, 29, e20200879. [Google Scholar] [CrossRef]
- Ajwa, N.; Alfayez, H.; Al-Oqab, H.; Melibary, R.; Alzamil, Y. The Effect of Erbium-Doped Yttrium Aluminum Garnet Laser in Debonding of Orthodontic Brackets: A Systematic Review of the Literature. Photobiomodul. Photomed. Laser Surg. 2021, 39, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Tocchio, R.M.; Williams, P.T.; Mayer, F.J.; Standing, K.G. Laser Debonding of Ceramic Orthodontic Brackets. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Leśniak, K.; Matys, J.; Żmuda-Stawowiak, D.; Mroczka, K.; Dominiak, M.; Brugnera Junior, A.; Gruber, R.; Romanos, G.E.; Sculean, A. Er:YAG Laser for Metal and Ceramic Bracket Debonding: An In Vitro Study on Intrapulpal Temperature, SEM, and EDS Analysis. Photomed. Laser Surg. 2018, 36, 595–600. [Google Scholar] [CrossRef]
- Mosaddad, S.A.; Abduo, J.; Zakizade, M.; Tebyaniyan, H.; Hussain, A. The Effect of Various Lasers on the Bond Strength Between Orthodontic Brackets and Dental Ceramics: A Systematic Review and Meta-Analysis. Photobiomodul. Photomed. Laser Surg. 2024, 42, 20–48. [Google Scholar] [CrossRef]
- Azzeh, E.; Feldon, P.J. Laser Debonding of Ceramic Brackets: A Comprehensive Review. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 79–83. [Google Scholar] [CrossRef]
- Mahmoud, E.; Pacurar, M.; Bechir, E.S.; Maris, M.; Olteanu, C.; Dascalu, I.T.; Moldovan, M. Comparison of Shear Bond Strength and Adhesive Remnant Index of Brackets Bonded with Two Types of Orthodontic Adhesives. Mater. Plast. 2017, 54, 141–144. [Google Scholar] [CrossRef]
- Gupta, M.; David, S.A.; Nishad, A.; Ramanna, P.K.; Bhagvandas, S.C. In Vitro Analysis of Shear Bond Strength and Adhesive Remnant Index of Stainless Steel Brackets with Different Adhesive Systems to Enamel. J. Contemp. Dent. Pract. 2018, 19, 1047–1051. [Google Scholar] [CrossRef]
- Kunizhev, B.I.; Torshkhoeva, Z.S.; Zhelikhazhev, R.N.; Starov, A.V. Destruction of Polymers under the Action of Laser Radiation. IOP Conf. Ser. Mater. Sci. Eng. 2021, 1083, 012040. [Google Scholar] [CrossRef]
- Kiryk, J.; Matys, J.; Nikodem, A.; Burzyńska, K.; Grzech-Leśniak, K.; Dominiak, M.; Dobrzyński, M. The Effect of Er:YAG Laser on a Shear Bond Strength Value of Orthodontic Brackets to Enamel—A Preliminary Study. Materials 2021, 14, 2093. [Google Scholar] [CrossRef]
- Guzman, U.A.; Jerrold, L.; Vig, P.S.; Abdelkarim, A. Comparison of Shear Bond Strength and Adhesive Remnant Index between Precoated and Conventionally Bonded Orthodontic Brackets. Prog. Orthod. 2013, 14, 39. [Google Scholar] [CrossRef]
- Mesaroș, A.; Mesaroș, M.; Buduru, S. Orthodontic Bracket Removal Using LASER-Technology—A Short Systematic Literature Review of the Past 30 Years. Materials 2022, 15, 548. [Google Scholar] [CrossRef] [PubMed]
- Zach, L.; Cohen, G. Pulp Response to Externally Applied Heat. Oral Surg. Oral Med. Oral Pathol. 1965, 19, 515–530. [Google Scholar] [CrossRef] [PubMed]
- Nalbantgil, D.; Tozlu, M.; Oztoprak, M.O. Pulpal Thermal Changes Following Er-YAG Laser Debonding of Ceramic Brackets. Sci. World J. 2014, 2014, 1–4. [Google Scholar] [CrossRef]
- Sauk, J.J.; Norris, K.; Foster, R.A.; Moehring, J.M.; Somerman, M.J. Expression of Heat Stress Proteins by Human Periodontal Ligament Cells. J. Oral Pathol. Med. 1988, 17, 496–498. [Google Scholar] [CrossRef]
- Eriksson, A.R.; Albrektsson, T. Temperature Threshold Levels for Heat-Induced Bone Tissue Injury: A Vital-Microscopic Study in the Rabbit. J. Prosthet. Dent. 1983, 50, 101–107. [Google Scholar] [CrossRef]
- Gibas-Stanek, M.; Pełka, P.; Pihut, M. What Is the Safest Method of Orthodontic Debonding- a Systematic Review of the Literature. Folia Med. Cracov. 2023, 30, 133–156. [Google Scholar] [CrossRef]
- Ozcan, M.; Finnema, K.; Ybema, A. Evaluation of Failure Characteristics and Bond Strength after Ceramic and Polycarbonate Bracket Debonding: Effect of Bracket Base Silanization. Eur. J. Orthod. 2008, 30, 176–182. [Google Scholar] [CrossRef]
- Huang, X.; Lin, J.; Demner-Fushman, D. Evaluation of PICO as a Knowledge Representation for Clinical Questions. AMIA Annu. Symp. Proc. 2006, 2006, 359–363. [Google Scholar]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Struzik, N.; Wiśniewska, K.; Piszko, P.J.; Piszko, A.; Kiryk, J.; Matys, J.; Dobrzyński, M. SEM Studies Assessing the Efficacy of Laser Treatment for Primary Teeth: A Systematic Review. Appl. Sci. 2024, 14, 1107. [Google Scholar] [CrossRef]
- Kiryk, J.; Kiryk, S.; Kensy, J.; Świenc, W.; Palka, B.; Zimoląg-Dydak, M.; Dobrzyński, W.; Matys, J.; Dobrzyński, M. Effectiveness of Laser-Assisted Teeth Bleaching: A Systematic Review. Appl. Sci. 2024, 14, 9219. [Google Scholar] [CrossRef]
- Piszko, P.J.; Piszko, A.; Kiryk, J.; Lubojański, A.; Dobrzyński, W.; Wiglusz, R.J.; Matys, J.; Dobrzyński, M. The Influence of Fluoride Gels on the Physicochemical Properties of Tooth Tissues and Dental Materials—A Systematic Review. Gels 2024, 10, 98. [Google Scholar] [CrossRef] [PubMed]
- Struzik, N.; Kensy, J.; Piszko, P.J.; Kiryk, J.; Wiśniewska, K.; Kiryk, S.; Korjat, Ł.; Horodniczy, T.; Sobierajska, P.; Matys, J.; et al. Contamination in Bone Substitute Materials: A Systematic Review. Appl. Sci. 2024, 14, 8266. [Google Scholar] [CrossRef]
- Piszko, P.J.; Piszko, A.; Kiryk, S.; Kiryk, J.; Horodniczy, T.; Struzik, N.; Wiśniewska, K.; Matys, J.; Dobrzyński, M. Bone Regeneration Capabilities of Scaffolds Containing Chitosan and Nanometric Hydroxyapatite—Systematic Review Based on In Vivo Examinations. Biomimetics 2024, 9, 503. [Google Scholar] [CrossRef]
- Rygas, J.; Matys, J.; Wawrzyńska, M.; Szymonowicz, M.; Dobrzyński, M. The Use of Graphene Oxide in Orthodontics—A Systematic Review. J. Funct. Biomater. 2023, 14, 500. [Google Scholar] [CrossRef]
- Kowalski, J.; Rygas, J.; Homa, K.; Dobrzyński, W.; Wiglusz, R.J.; Matys, J.; Dobrzyński, M. Antibacterial Activity of Endodontic Gutta-Percha—A Systematic Review. Appl. Sci. 2023, 14, 388. [Google Scholar] [CrossRef]
- Kensy, J.; Dobrzyński, M.; Wiench, R.; Grzech-Leśniak, K.; Matys, J. Fibroblasts Adhesion to Laser-Modified Titanium Surfaces—A Systematic Review. Materials 2021, 14, 7305. [Google Scholar] [CrossRef]
- Watson, P.F.; Petrie, A. Method Agreement Analysis: A Review of Correct Methodology. Theriogenology 2010, 73, 1167–1179. [Google Scholar] [CrossRef]
- Arima, S.; Namura, Y.; Tamura, T.; Shimizu, N. Easy Debonding of Ceramic Brackets Bonded with a Light-Cured Orthodontic Adhesive Containing Microcapsules with a CO2 Laser. Photomed. Laser Surg. 2018, 36, 162–168. [Google Scholar] [CrossRef]
- Macri, R.T.; de Lima, F.A.; Bachmann, L.; Galo, R.; Romano, F.L.; Borsatto, M.C.; Matsumoto, M.A.N. CO2 Laser as Auxiliary in the Debonding of Ceramic Brackets. Lasers Med. Sci. 2015, 30, 1835–1841. [Google Scholar] [CrossRef]
- Ahrari, F.; Heravi, F.; Fekrazad, R.; Farzanegan, F.; Nakhaei, S. Does Ultra-Pulse CO2 Laser Reduce the Risk of Enamel Damage during Debonding of Ceramic Brackets? Lasers Med. Sci. 2012, 27, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Matos, D.S.; Küchler, E.C.; Borsatto, M.C.; Matsumoto, M.A.N.; Marques, F.V.; Romano, F.L. CO2 Laser Irradiation for Debonding Ceramic Orthodontic Brackets. Braz. Dent. J. 2021, 32, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Saito, A.; Namura, Y.; Isokawa, K.; Shimizu, N. CO2 Laser Debonding of a Ceramic Bracket Bonded with Orthodontic Adhesive Containing Thermal Expansion Microcapsules. Lasers Med. Sci. 2015, 30, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Strobl, K.; Bahns, T.L.; Wiliham, L.; Bishara, S.E.; Stwalley, W.C. Laser-Aided Debonding of Orthodontic Ceramic Brackets. Am. J. Orthod. Dentofac. Orthop. 1992, 101, 152–158. [Google Scholar] [CrossRef]
- Ma, T.; Marangoni, R.D.; Flint, W. In Vitro Comparison of Debonding Force and Intrapulpal Temperature Changes during Ceramic Orthodontic Bracket Removal Using a Carbon Dioxide Laser. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 203–210. [Google Scholar] [CrossRef]
- Obata, A. Super Pulse CO2 Laser for Bracket Bonding and Debonding. Eur. J. Orthod. 1999, 21, 193–198. [Google Scholar] [CrossRef]
- Iijima, M.; Yasuda, Y.; Muguruma, T.; Mizoguchi, I. Effects of CO2 Laser Debonding of a Ceramic Bracket on the Mechanical Properties of Enamel. Angle Orthod. 2010, 80, 1029–1035. [Google Scholar] [CrossRef]
- Mimura, H.; Deguchi, T.; Obata, A.; Yamagishi, T.; Ito, M. Comparison of Different Bonding Materials for Laser Debonding. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 267–273. [Google Scholar] [CrossRef]
- Tehranchi, A.; Fekrazad, R.; Zafar, M.; Eslami, B.; Kalhori, K.A.M.; Gutknecht, N. Evaluation of the Effects of CO2 Laser on Debonding of Orthodontics Porcelain Brackets vs. the Conventional Method. Lasers Med. Sci. 2011, 26, 563–567. [Google Scholar] [CrossRef]
- Demirkan, I.; Sarp, A.S.K.; Gülsoy, M. Ceramic Bracket Debonding with Tm:Fiber Laser. J. Biomed. Opt. 2016, 21, 065007. [Google Scholar] [CrossRef]
- Dostalová, T.; Jelinková, H.; Šulc, J.; Němec, M.; Fibrich, M.; Jelínek, M.; Michalík, P.; Bučková, M. Bond Strengths Evaluation of Laser Ceramic Bracket Debonding. Laser Phys. 2012, 22, 1395–1400. [Google Scholar] [CrossRef]
- Dostalova, T.; Jelinkova, H.; Sulc, J.; Nemec, M.; Jelinek, M.; Fibrich, M.; Michalik, P.; Miyagi, M.; Seydlova, M. Ceramic Bracket Debonding by Tm:YAP Laser Irradiation. Photomed. Laser Surg. 2011, 29, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Dostálová, T.; Jelínková, H.; Šulc, J.; Koranda, P.; Nemec, M.; Racek, J.; Miyagi, M. Laser Radiation Bracket Debonding; Rechmann, P., Fried, D., Eds.; SPIE: Bellingham, WA, USA, 2008; p. 684304. [Google Scholar]
- Han, X.; Liu, X.; Bai, D.; Meng, Y.; Huang, L. Nd:YAG Laser-Aided Ceramic Brackets Debonding: Effects on Shear Bond Strength and Enamel Surface. Appl. Surf Sci. 2008, 255, 613–615. [Google Scholar] [CrossRef]
- Hayakawa, K. Nd: YAG Laser for Debonding Ceramic Orthodontic Brackets. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 638–647. [Google Scholar] [CrossRef]
- Downarowicz, P.; Noszczyk, P.; Mikulewicz, M.; Nowak, R. Thermal Effect of Er:YAG and Er,Cr:YSGG Used for Debonding Ceramic and Metal Orthodontic Brackets: An Experimental Analysis. Adv. Clin. Exp. Med. 2020, 29, 557–563. [Google Scholar] [CrossRef]
- Yilanci, H.; Yildirim, Z.B.; Ramoglu, S.I. Intrapulpal Temperature Increase During Er:YAG Laser-Aided Debonding of Ceramic Brackets. Photomed. Laser Surg. 2017, 35, 217–222. [Google Scholar] [CrossRef]
- Mocuta, D.-E.; Miron, M.I.; Lungeanu, D.; Mateas, M.; Ogodescu, E.; Todea, C.D. Laser Er:YAG-Assisted Debonding May Be a Viable Alternative to the Conventional Method for Monocrystalline Ceramic Brackets. Int. J. Environ. Res. Public Health 2022, 19, 14564. [Google Scholar] [CrossRef]
- Dostalova, T.; Jelinkova, H.; Remes, M.; Šulc, J.; Němec, M. The Use of the Er:YAG Laser for Bracket Debonding and Its Effect on Enamel Damage. Photomed. Laser Surg. 2016, 34, 394–399. [Google Scholar] [CrossRef]
- Mirhashemi, A.H.; Hossaini, S.M.H.; Etemadi, A.; Kharazifard, M.J.; Bahador, A.; Soudi, A. Effect of Er:YAG and Er,Cr:YSGG Lasers on Ceramic Bracket Debonding from Composite Blocks. Front. Dent. 2019, 16, 88. [Google Scholar] [CrossRef]
- Mundethu, A.R.; Gutknecht, N.; Franzen, R. Rapid Debonding of Polycrystalline Ceramic Orthodontic Brackets with an Er:YAG Laser: An in Vitro Study. Lasers Med. Sci. 2014, 29, 1551–1556. [Google Scholar] [CrossRef] [PubMed]
- Tozlu, M.; Oztoprak, M.O.; Arun, T. Comparison of Shear Bond Strengths of Ceramic Brackets after Different Time Lags between Lasing and Debonding. Lasers Med. Sci. 2012, 27, 1151–1155. [Google Scholar] [CrossRef]
- Hoteit, M.; Nammour, S.; Zeinoun, T. Evaluation of Enamel Topography after Debonding Orthodontic Ceramic Brackets by Different Er,Cr:YSGG and Er:YAG Lasers Settings. Dent. J. 2020, 8, 6. [Google Scholar] [CrossRef] [PubMed]
- Hamadah, O.; Bachir, W.; Zamzam, M.K. Thermal Effect of Er:YAG Laser Pulse Durations on Teeth During Ceramic Bracket Debonding. Dent. Med. Probl. 2016, 53, 352–357. [Google Scholar] [CrossRef]
- Nalbantgil, D.; Tozlu, M.; Oztoprak, M.O. Comparison of Different Energy Levels of Er:YAG Laser Regarding Intrapulpal Temperature Change During Safe Ceramic Bracket Removal. Photomed. Laser Surg. 2018, 36, 209–213. [Google Scholar] [CrossRef]
- Nalbantgil, D.; Oztoprak, M.O.; Tozlu, M.; Arun, T. Effects of Different Application Durations of ER:YAG Laser on Intrapulpal Temperature Change during Debonding. Lasers Med. Sci. 2011, 26, 735–740. [Google Scholar] [CrossRef]
- Oztoprak, M.O.; Nalbantgil, D.; Erdem, A.S.; Tozlu, M.; Arun, T. Debonding of Ceramic Brackets by a New Scanning Laser Method. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 195–200. [Google Scholar] [CrossRef]
- Alakuş Sabuncuoğlu, F.; Erşahan, Ş.; Ertürk, E. Debonding of Ceramic Brackets by Er:YAG Laser. J. Istanb. Univ. Fac. Dent. 2016, 50, 24. [Google Scholar] [CrossRef]
- Rao, A.; Deenadayalan, P.; Deepak, C.; Dilipkumar, D.; Angrish, N.; Shetty, S.S. Effect of ER, CR: YSGG Laser Debonding on Enamel Surface Changes in Stainless Steel and Ceramic Brackets—An in Vitro Study. J. Orthod. Sci. 2023, 12, 7. [Google Scholar] [CrossRef]
- Abdulaziz, A.; El-Kholy, M.M.; Bushra, S.S.; Ali, S.M.; Shehab, K.A. Performance of Two Laser Motion Modes versus Conventional Orthodontic Ceramic Brackets Debonding Technique on Enamel Surface Topography. Lasers Med. Sci. 2024, 39, 156. [Google Scholar] [CrossRef]
- Stein, S.; Wenzler, J.; Hellak, A.; Schauseil, M.; Korbmacher-Steiner, H.; Braun, A. Intrapulpal Temperature Increases Caused by 445-Nm Diode Laser-Assisted Debonding of Self-Ligating Ceramic Brackets During Simulated Pulpal Fluid Circulation. Photomed. Laser Surg. 2018, 36, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Stein, S.; Kleye, A.; Schauseil, M.; Hellak, A.; Korbmacher-Steiner, H.; Braun, A. 445-Nm Diode Laser-Assisted Debonding of Self-Ligating Ceramic Brackets. Biomed. Eng. Biomed. Tech. 2017, 62, 513–520. [Google Scholar] [CrossRef]
- Stein, S.; Hellak, A.; Schauseil, M.; Korbmacher-Steiner, H.; Braun, A. Effects of 445-Nm Diode Laser-Assisted Debonding of Self-Ligating Ceramic Brackets on Shear Bond Strength. Photomed. Laser Surg. 2018, 36, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Yassaei, S.; Soleimanian, A.; Nik, Z.E. Effects of Diode Laser Debonding of Ceramic Brackets on Enamel Surface and Pulpal Temperature. J. Contemp. Dent. Pract. 2015, 16, 270–274. [Google Scholar] [CrossRef]
- Feldon, P.J.; Murray, P.E.; Burch, J.G.; Meister, M.; Freedman, M.A. Diode Laser Debonding of Ceramic Brackets. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 458–462. [Google Scholar] [CrossRef]
- Sarp, A.S.K.; Gülsoy, M. Ceramic Bracket Debonding with Ytterbium Fiber Laser. Lasers Med. Sci. 2011, 26, 577–584. [Google Scholar] [CrossRef]

| Authors | Laser Parameters | Protocol of Debonding | Brackets | SBS | Results ARI | Temperature Increase |
|---|---|---|---|---|---|---|
| Khalil [3] | Diode laser (Simpler, Doctor Smile, Italy) with continuous mode Power: 4 W Wavelength: 980 nm Tip diameter: 300 μm Time: 12 s Er:YAG laser (Pluser, Doctor Smile, Brendola, Italy) Power: 4 W Wavelength: 2940 nm Tip diameter: 1 mm | Shear testing of the brackets was performed with a universal testing machine, and then ARI assessment and scanning electron microscopy were used to evaluate the enamel microstructure. | Brackets: monocrystalline ceramic brackets (Perfect Clear, Hubit, Uiwang-si, Republic of Korea) Adhesive: GC Ortho Connect adhesive (GC Ortho Connect, GC Orthodontics, Breckerfeld, Germany). | Mean shear bond strength Group I (control): 14.99 MPa Group II (chemical-aided debonding): 14.25 MPa Group III (ultrasonic-aided debonding): 11.17 MPa Group IV (diode laser-aided debonding): 11.13 MPa Group V (Er:YAG laser-aided debonding): 9.39 MPa | Statistically significant higher ARI was found solely in group V when compared to group I, group II, group III, and group IV. No other significant differences were found between the groups with regard to ARI. | No data |
| Tocchio [12] | Nd:YAG laser XeCI excimer (Hypcrex- 400, Lumonics, Kanata, ON, Canada) Wavelengths: 248 nm, 308 nm, 1060 nm Power: 8 W Pulse energy: 21 mJ | The brackets were debonded by exposing their labial surfaces to XeCI excimer laser light with wavelengths of 248 nm, 308 nm, and 1060 nm, with light power densities ranging from around 3 to 33 W/cm 2 under an externally induced stress of either 0.8 MPa or 0 MPa. | Brackets: single crystal alumina (sapphire) brackets (Starfire, “A” Company, San Diego, CA, USA) and polycrystalline alumina brackets (Transcend, Unitek, Monrovia, CA, USA) Adhesive: no data | No data | No data | No data |
| Grzech-Leśniak [13] | Er:YAG laser (Morita, Irvine, CA, USA) Time: 6 s Distance: 1 mm (groups 1, 2), 2 mm (group 3) Wavelength: 2940 nm Power: 3.4 W Energy: 170 mJ Frequency: 20 Hz Pulse duration: 300 ls Tip diameter: 0.8 mm Level of air/fluid: 3 mL/s | Three different laser application methods for bracket debonding were used. | Brackets: metal (Victory Series; 3M Unitek, Monrovia, CA, USA) and ceramic brackets (Inspire-ICE; Ormco, Orange, CA, USA) Adhesive: Transbond XT (3M Unitek, Monrovia, CA, USA). The Er:YAG laser was used to irradiate the brackets. | No data | Mean ranks: Group 1: 25.80 Group 2: 22.03 Group 3: 21.20 | The mean temperature gradient Group 1: 1.29 ± 0.42 °C Group 2: 1.78 ± 0.60 °C Group 3: 0.83 ± 0.43 °C All groups: 1.30 ± 0.62 °C |
| Arima [39] | CO2 laser 10,600 nm Time: 3–6 s Distance: in contact with labial surface of the bracket Power: 5 or 7 W Beam diameter: 0.15 mm Continuous wave (CW) | Irradiation for 3, 4, 5, and 6 sec at an intensity of 5 W or 7 W with (C) and without (NC) air cooling. SBS measured 10 min after irradiation. | Zirconium brackets (COBY, Biodent, Tokyo, Japan) with base area 12.4 mm2 Adhesive: Transbond XT (3M Unitek, Monrovia, CA, USA) + bonding agent containing microcapsules (0–30 wt%) | Change compared to the control group: 30% of agent containing microcapsules = −6.8 MPa 25% = −0.17-fold 20% = −0.39-fold 10% = −0.89-fold 0% = −0.81-fold | 0% of microcapsule content: Score 0 × 4 Score 1 × 2 10% Score 0 × 1 Score 1 × 5 20% Score 0 × 3 Score 1 × 3 25% Score 0 × 5 Score 1 × 2 30% Score 0 × 4 Score 1 × 2 | Maximum temp. increase: 5 s, 7 W, C = 5.3 °C 6 s, 7 W, C = 5.9 °C 5 s, 7 W, NC = 6.6 °C 6 s, 7 W, NC = 7.4 °C |
| Macri [40] | CO2 laser 10,600 nm Time: 3 or 5 s Pulse duration: 0.001 or 0.003 s Distance: 4 mm Power: 5, 8, or 10 W | SBS was measured immediately after laser irradiation. | Polycrystalline bracket (Fascination, Dentaurum, Ispringen, Germany) Adhesive: Transbond XT (3M/Unitek, Monrovia, CA, USA) | 10 W, of 0.01 s pulse = 7.33 (1.89) MPa 8 W, of 0.01 s pulse = 9.04 (3.26) MPa 5 W, of 0.01 s pulse = 10.56 (3.47) MPa 5 W, of 0.03 s pulse = 11.72 (5.42) MPa | Mean: 10 W, of 0.01 s pulse = 2.53 8 W, of 0.01 s pulse = 1.66 5 W, of 0.01 s pulse = 2.26 5 W, of 0.03 s pulse = 2.46 | Mean increase: 10 W, of 0.01 s pulse; 8 W, of 0.01 s pulse; 5 W, of 0.01 s pulse; 5 W, of 0.03 s pulse; Less than 5.5 °C Irradiation with other combinations of parameters above 5.5 °C |
| Ahrari [41] | CO2 laser 10,600 nm Time: 5 s Distance: 5 mm Power: 188 W Pulse duration: 500 μs Beam diameter: 1 mm Surface area cm2 Frequency: 400 Hz | Brackets were debonded with pliers 3 s after irradiation. | Polycrystalline brackets Fascination (Dentaurum, Ispringen, Germany) or monocrystalline brackets Inspire Ice (Ormco, Orange, CA, USA) Adhesive: Transbond XT (3M Unitek, Monrovia, CA, USA) | No data | Polycrystalline brackets Score 0 × 1 Score 1 × 5 Score 2 × 9 Score 3 × 5 Monocrystalline brackets Score 0 × 2 Score 1 × 1 Score 2 × 3 Score 3 × 14 | Mean increase Polycrystalline brackets 3.9 ± 0.32 °C Monocrystalline brackets 4.4 ± 0.5 °C |
| Matos [42] | CO2 laser 10,600 nm Time: 3 s Distance: 4 mm Power: 10 W Pulse duration: 0.01 s | SBS testing was performed right after laser irradiation | Polycrystalline brackets Fascination (Dentaurum, Ispringen, Germany) or monocrystalline brackets Inspire Ice (Ormco, Orange, CA, USA) Adhesive: Transbond XT (3M Unitek, Monrovia, CA, USA) or Z250 (3M ESPE, Dental Products Division, St. Paul, MN, USA) | Polycrystalline brackets + Transbond XT = 0.92 (0.18) MPa Polycrystalline brackets + Z250 = 0.28 (0.7) MPa Monocrystalline brackets + Transbond XT = 3.45 (0.68) MPa Monocrystalline brackets + Z250 = 3.52 (1.04) MPa | Mean Polycrystalline brackets + Transbond XT = 1.6 (1.3) Polycrystalline brackets + Z250 = 2.66 (0.48) Monocrystalline brackets + Transbond XT = 1.2 (1.08) Monocrystalline brackets + Z250 = 1.86 (0.99) | No data |
| Saito [43] | CO2 laser (Opelaser Pro, Yoshida, Tokyo, Japan) Distance: in contact with the labial face of a bracket head Beam diameter: 0.5 mm Power: 3 W Time: few seconds | Bonding materials with different microcapsule contents (0, 30, and 40 weight percent) were used to bond ceramic brackets to bovine permanent mandibular incisors. The bond strengths were assessed following laser irradiation for 4, 5, and 6 s and compared to groups that were not laser-treated. A measurement of the pulp chamber’s temperature during laser irradiation was then performed. | Brackets: ceramic brackets Adhesive: experimentally produced 4-META/MMA-TBB resin orthodontic adhesives (Orthomite SuperBond, Sun Medical, Moriyama, Japan) containing 30 and 40 wt% thermal expansion microcapsules, which expanded 70-fold upon heating to 80 °C (Matsumoto Microsphere F-36D, Matsumoto Yushi- Seiyaku, Osaka, Japan) in the polymer powder. | Shear bond strengths around 18 MPa without laser irradiation did not change with laser irradiation for 4–6 s when the adhesive did not contain microcapsules. | No significant difference in ARI score after debonding was detected between with and without CO2 laser irradiation, but there were many scores of 0 and 1. | Temperature increases in the pulp chamber for each irradiation were less than 4.3 °C. |
| Strobl [44] | CO2 laser 10,600 nm Time: 2 s Power: 7–14 W Nd:YAG laser 1060 nm Time: 5 s | Brackets were debonded with bracket removal fork after irradiation. | Polycrystalline alumina (A12OD (Transcend, Unitek/3M, Monrovia, CA, USA)) and 30 monocrystalline (sapphire) alumina brackets (Starfire, A Company/Johnson & Johnson, San Diego, CA, USA). Adhesive: Concise (3M, Minneapolis, MN, USA). | No data | ARI for brackets debonded without laser Polycrystalline: Score 1 × 24 Score 2 × 3 Score 3 × 0 Score 4 × 2 Score 5 × 1 Monocrystalline: Score 1 × 16 Score 2 × 3 Score 3 × 1 Score 4 × 0 Score 5 × 0 | No data |
| Tsun Ma [45] | CO2 laser 10,600 nm Time: 1, 2, 3 s Distance: as close as possible to the labial surface of the ceramic bracket Power: 18 W Beam diameter: 1 mm Waveguide length: 1 m | Debonding force was applied during the laser irradiation (1, 2, 3 s) using modified pliers with laser waveguide. The ceramic bracket was removed from the tooth as soon as the adhesive softening temperature was reached. | Polycrystalline alumina orthodontic brackets (Transcend 6000, Unitek/3M), Adhesive: Transbond, Unitek/3M) | No data | No data | Human teeth: 1 s, +0.91 (°C) 2 s, +1.74 (°C) 3 s, +2.67 (°C) Bovine teeth: 1 s, +1.65 (°C) 2 s, +3.31 (°C) 3 s, +5.15 (°C) |
| Akihito Obata [46] | 2 super pulse and 1 continuous wave normal pulse CO2 laser 10,600 nm Power: 2, 3, 4 W Super pulse: Pulse width: 1–500 milliseconds Pulse width: 200–800 microseconds Normal pulse: Pulse width: 5–500 milliseconds | Laser irradiation was started the moment the compression cell touched the bracket | Ceramic brackets (Transcendend series 6000 3M/UNITEK Monrovia, CA, USA) for laser debonding; 4-META MMA resin | No data | No data | 2 W: - super pulse +1.4 °C 3 W: - super pulse +2.1 °C - normal pulse +2.7 °C |
| Iijima, M. [47] | CO2 laser: - wavelength: 10.6 μm - continuous wave - spot diameter: 0.45 mm - power outputs tested: 3 W, 4 W, 5 W, and 6 W - application time: 5 s per spot - distance from bracket: approximately 1 mm - applied to the 4 bracket wings (5 s each) | Immediate mechanical debonding with a universal testing machine (EZ Test, Shimadzu, Kyoto, Japan) using knife-edged shearing blade parallel to buccal surface; crosshead speed: 0.5 mm/min. | Brackets: single-crystal brackets (Inspire ice, Ormco, Orange, CA, USA) Adhesive: 1. Conventional etch and rinse adhesive (Transbond XT, 3M Unitek, Monrovia, CA, USA) 2. Self-etching adhesive (Transbond Plus, 3M Unitek, Monrovia, CA, USA) | Mean: 1. Conventional: control = 15.5 MPa 3 W, 10 MPa 4 W, 10 MPa 5 W, 10 MPa 6 W, 8 MPa 2. Self-etching: control = 12 MPa 3 W, 9 MPa 4 W, 5 MPa 5 W, 4 MPa 6 W, 3 MPa | 1. Conventional: Control: Score 1 × 4 Score 2 × 1 6 W: Score 1 × 4 Score 2 × 1 2. Self-etching: Control: Score 0 × 1 Score 1 × 4 3 W: Score 1 × 5 4 W: Score 0 × 1 Score 1 × 4 5 W: Score 1 × 5 6 W: Score 1 × 5 | Low output (3 W and 4 W): increase of about 100 °C to 150 °C High output (5 W and 6 W): increase of 200 °C Temperature returned to room temperature within 30 s after irradiation for all power settings |
| Mimura, H. [48] | CO2 laser: - wavelength: 10.6 μm - power outputs: 3 W and 7 W - tip placement: just apart from bracket - continuous application | Mechanical removal using shear force with force applied perpendicular to bracket–enamel interface (initial force 3 kgf, 1 mm/min speed). | Brackets: polycrystalline alumina brackets (Transcend series 6000, Unitek/3M, Monrovia, CA, USA) Adhesive: 1. Bis-GMA composite resin (Concise, 3M, Monrovia, CA, USA) 77% quartz filler 2. 4-META MMA resin (Super-Bond), no filler | Mean: 1. Concise groups: control = 14.81 kgf 3 W = 5.85 kgf 7 W = 4.01 kgf 2. Super-Bond groups: control = 12.49 kgf 3 W = 3.63 kgf 7 W = 3.41 kgf | MARI 1. Concise group: Control: Score 1 × 0 Score 2 × 3 Score 3 × 5 Score 4 × 12 3 W laser: Score 1 × 2 Score 2 × 6 Score 3 × 7 Score 4 × 5 7 W laser: Score 1 × 0 Score 2 × 6 Score 3 × 9 Score 4 × 5 2. Super-Bond: Control: Score 1 × 0 Score 2 × 2 Score 3 × 6 Score 4 × 12 3 W laser: Score 1 × 0 Score 2 × 1 Score 3 × 6 Score 4 × 13 7 W laser: Score 1 × 0 Score 2 × 1 Score 3 × 3 Score 4 × 16 | No measurements during the deboning process. Thermal expansion: - Super-Bond: expanded until 80 °C (peak at 60 °C), then began contracting above 80 °C - Concise: showed linear expansion with temperature increase (4× greater than bracket expansion) |
| Tehranchi, A. [49] | CO2 laser: - power density: 50 W - exposure time: 5 s - pulse duration: 500 μs - interval between pulses: 2000 μs - frequency: 400 Hz - spot size: 1 mm - application: at center of brackets | Mechanical removal using the Instron machine blade immediately after the laser stopped with constant speed of 1 mm/min. | Brackets: polycrystalline alumina brackets (G & H Series, Schönheide, Germany) positioned 4 mm from incisal edge Adhesive: chemically cured orthodontic composite resin (No-mix, Unitek, Blue Bell, PA, USA) | Means: Control group: 23.7607 Laser group: 9.9145 | ARI (Kruskal–Wallis test) Control: - mean rank: 11.53 - debonding site closer to enamel–adhesive interface Laser: - mean rank: 30.63 - debonding site closer to bracket surface ARI (U test) Control: mean 8.93 Laser: mean 22.07 | No measurements during the procedure. |
| Demirkan [50] | Tm:fiber laser 1940 nm Time: 7 or 10 s Energy: 21, 25, or 30 J Power: 2.5 or 3 W Beam diameter: 400 μm | Brackets were irradiated with a scanning or non-scanning method. SBS was measured during irradiation. | Polycrystalline brackets (GH. Franklin, IN, USA) Adhesive: 3M, Unite Bonding Adhesive Set, Monrovia, CA, USA | Lack of precise date | No data | Scanning method: 2.5 W, 7 s = 5.02 (1.67) °C 3.0 W, 7 s = 3.56 (0.92) °C 2.5 W 10 s = 4.27 (0.89) °C 3 W 10 s = 6.21 (3.45) °C Non-scanning method: 2.5 W, 7 s = 3.86 (1.20) °C 3.0 W, 7 s = 4.82 (3.10) °C 2.5 W, 10 s = 5.57 (2.06) °C 3.0 W, 10 s = 3.92 (0.89) °C |
| Dostalova [51] | Tm:YAP laser 1998 nm Time: 60 s Power: 1 or 4 W Beam diameter: 3 mm | Brackets were debonded with pliers after irradiation. | Brackets: Fascination 2 (Dentaurum, Ispiringen, Germany) or Charity SL APC (3M Unitek Orthodontic Products, Monrovia, CA, USA) Adhesive: ConTec LC (Dentaurum, Ispringen, Germany). | No data | No data | Mean increase Fascination 1 W = 0.9 (0.5) °C 4 W = 2.8 (0.9) °C Charity 1 W = 0.7.(0.3) °C 4 W = 2.6 (1.1) °C |
| Tatjana Dostalova [52] | Tm:YAP Laser Irradiation 1998 nm Time: 60 s Power: 1 and 2 W Beam diameter: 3 mm Fluence: 849 or 1698 J/cm2 Irradiance: 14 or 28 W/cm2 Water flow: 2 mL/min. Spot size: 3 mm | After a period of 60 sec, the ceramic bracket was removed from the tooth surface mechanically, with 3M Unitek band-removing pliers (Unitek, Monrovia, CA, USA). | Fascination 2 (Dentaurum, Pforzheim, Germany) + Adhesive: ConTec LC adhesive (Dentaurum, Ispringen, Germany) BIS-GMA Charity SL APC (3M Unitek Orthodontic Products, Monrovia, CA, USA) + Adhesive: Transbond plus (3M Unitek Orthodontic Products, Monrovia, CA, USA) (Bis- GMA/TEGDMA (triethylene glycol dimethacrylate-based SEP adhesive system) self-etching primer | No data | No data | 1 W: - Fascination 2 +3 °C - Charity +3.8 °C |
| Dostálová, T. [53] | 1. GaAlAs diode laser: - wavelength: 808 nm - maximum output power: 20 W - fiber core diameter: 400 μm - numerical aperture: 0.22 - 1–10 W power settings - time of irradiation: 60 s 2. Tm:YAP laser: - wavelength: 1980 nm - maximum output power: 3.8 W - 1–2 W power settings - time of irradiation: 30, 60, or 90 s | After irradiation, brackets were removed mechanically. | Brackets: ceramic brackets Fascination 2 (Dentaurum, Ispringen, Germany) Adhesive: ConTec LC (Dentaurum, Ispringen, Germany) Primer: ConTec Primer Etching: ConTec Etch (applied for 15 s) | No data | No data | 1. GaAlAs: without cooling - 1 W, 60 s: 18 °C increase - 2 W, 60 s: 29 °C increase - 10 W, 60 s: 114 °C increase No successful debonding 2. Tm:YAP: Without cooling: - 1 W, 60 s: 31 °C increase With cooling: - 1 W, 60 s: 2 °C increase - 1 W, 90 s: 5 °C increase - 2 W, 60 s: 9 °C increase Temperature monitored using NiCr-Ni thermocouple and thermal imaging camera |
| Xianglong Han [54] | Nd:YAG laser 1060 nm Time: 3 s Distance: 1 mm Power: 3 W Beam diameter: 0.6 mm Pulse width: 0.2 ms | Brackets were removed with shear debonding force. Laser was also used in 3 groups. | - metallic (MBT, 3M Unitek, Monrovia, CA, USA) and -polycrystalline ceramic brackets (Clarity, 3M Unitek,Monrovia, CA, USA) - orthodontic adhesive following the manufacturers’ recommendations. | Group: 1. Metallic brackets 9.78 MPa 2. Ceramic brackets 11.63 MPa 3. Ceramic brackets + laser irradiation 5.13 MPa | Group 1 Score 1 × 1 Score 2 × 2 Score 3 × 2 Score 4 × 3 Score 5 × 2 Score 6 × 0 Group 2 Score 1 × 1 Score 2 × 0 Score 3 × 1 Score 4 × 2 Score 5 × 4 Score 6 × 2 Group 3 Score 1 × 3 Score 2 × 4 Score 3 × 2 Score 4 × 0 Score 5 × 0 Score 6 × 1 | No data |
| Hayakawa, K. [55] | Nd:YAG laser: - wavelength: 1060 nm - maximum output: 1.2 ms - pulse duration: 3.0 J with 5 pulses per second - single pulse per location (1 pps) - energy levels tested: 1.0 J, 2.0 J, 3.0 J - fiber waveguide diameter: 0.4 mm - output energy from fiber tip was 8.9% lower than nominal output power - tip distance from bracket: 0.1 mm without direct contact - applied to 2 spots: mesiodistal center of gingival surface and coronal surface under each bracket wing | 1. Immediate removal (2.0 J and 3.0 J groups): no mechanical force needed; laser application caused spontaneous debonding. 2. Non-immediate removal: universal testing machine was used for brackets that did not debond spontaneously. | Brackets: 1. Single crystal ceramic brackets (Inspire, Shofu, Kyoto, Japan) 2. Polycrystalline ceramic brackets (Clarity, 3M Unitek, Monrovia, CA, USA) Adhesive: 1. 4-META/MMA based adhesive without fillers (Super-Bond, Sun Medical, Moriyama, Japan) 2. Bis-GMA-based photoactivated adhesive with fillers (Transbond, 3M Unitek, Monrovia, CA, USA) | Mean: Control = 25–30 MPa 1.0 J = 20–25 MPa 2.0 J = 10–15 MPa 3.0 J = 5–10 MPa | No data | Maximum temperature rise: 5.1 °C. Mean temperature increases by group: Single crystal + MMA: 2.0 J (1.71 °C), 3.0 J (2.46 °C) Single crystal + Bis-GMA: 2.0 J (1.74 °C), 3.0 J (1.67 °C) Polycrystalline + MMA: 2.0 J (1.09 °C), 3.0 J (1.44 °C) Polycrystalline + Bis-GMA: 2.0 J (1.07 °C), 3.0 J (2.08 °C) Temperature peak occurred at 0.5 s after irradiation and returned to baseline after 3 s. |
| Downarowicz [56] | Er,Cr:YSGG laser 2780 nm Time: 5–25 s Distance: 1–2 mm Power: 2.78–2.85 W Energy: 185–190 mJ Beam diameter: 0.6 mm Frequency: 25 Hz Pulse duration: 300 μs Er:YAG laser 2940 nm Time: 5–15 s Distance: 1–2 mm Power: 4 W Energy: 200 mJ, Beam diameter: 0.8 mm Frequency: 20 Hz Pulse duration: 300 μs | The brackets were irradiated by a laser until spontaneous debonding occurred. | Brackets: Inspire-ICE (Ormco, Glendora, CA, USA) Adhesive: Transbond XT (3M Unitek, Maplewood, MN, USA) | No data | No data | Er,Cr:YSGG Outside: 23.3 °C Inner: 21.4 °C Er:YAG Outside: 24.7 °C Inner: 24.2 °C |
| Yilanci [57] | Er:YAG laser 2940 nm Time: 4–6 s Power: 1.2 W Energy: 600 mJ Beam diameter: 1.3 mm Surface area: 0.004225 cm2 Frequency: 2 Hz Power density: 90.4 W/cm2 Fluence: 45.2 J/cm2 | Brackets were removed with help of laser light after thermocycling (group B) or without thermocycling (group A). | Monocrystalline brackets (Radiance, American Orthodontics, Sheboygan, WI, USA) Adhesive: Transbond XT (3 M; Unitek, Monrovia, CA, USA) | No data | No data | Mean change Group A Incisors = +2.12 °C Premolars = +2.26 °C Group B Incisors = +2.61 °C Premolars = +1.74 °C |
| Mocuta [58] | Er:YAG laser 2940 nm Distance: 1 mm Energy: 600 mJ Pulse duration: 800 μs Beam diameter: 1.3 mm Frequency: 2 Hz | Brackets were debonded using Er:YAG laser-assisted action. | Monocrystalline brackets Adhesive: no data | No data | No data | No data |
| Dostalova [59] | Er:YAG 2 940 nm Time: 140 s Peak power: 1 kW Energy: 280 mJ Beam diameter: 1 mm Frequency: 6 Hz Power density: 144 kW/cm2 Fluence: 36 J/cm2 | The locks were irradiated for 140 s, then debonded using special pliers. | Brackets: Clarity Advanced (3M Unitek, Monrovia, CA, USA) Adhesive: Transbond XT (3M Unitek, Monrovia, CA, USA) or Variolink II Professional Set (Ivoclar Vivadent AG, Schaan, Liechtenstein) | No data | No data | Increase from 2.2 °C to 3.0 °C |
| Mirhashemi [60] | Er,Cr:YSGG laser Time: 10 s Distance: 2 mm Power: 3 W Beam diameter: 800 μm Fluence: 22/28 J/cm2 Er: YAG laser Time: 10 s Pulse duration: 100 μs Distance: 2 mm Power: 3 W Beam diameter: 1 mm Frequency: 20 Hz Fluence: 22/28 J/cm2 | SBS was measured immediately after laser irradiation to three sides of the bracket bases. | Brackets: GAC International Inc. (Islandia, NY, USA) Adhesive: Transbond XT (3M Unitek, Monrovia, CA, USA). | Mean Er,Cr:YSGG laser = 18.03 MPa Er:YAG laser = 17.01 MPa | Er,Cr:YSGG laser Score 0 × 1 Score 1 × 9 Score 3 × 2 Er:YAG laser Score 1 × 8 Score 2 × 2 Score 3 × 2 | No data |
| Mundethu [61] | Er:YAG 2940 nm Time: one pulse Distance: in contact Energy: 600 mJ Pulse duration: 800 μs Beam diameter: 1.3 mm Frequency: 2 Hz | Debonding was performed using a laser tip in contact with the center of the bracket. | Polycrystalline brackets (Damon Clear; Ormco Corp, Orange, CA, USA) Adhesive: Blugloo (Ormco Corp, Orange, CA, USA) | No data | Score 3 for all specimens | No data |
| Tozlu [62] | Er:YAG laser 2940 nm Time: 6 s Distance: 2 mm Power: 5 W Beam diameter: 1 mm | Debonding with SBS measurement was performed 1 s, 18 s, 30 s, or 60 s after laser exposure. | Polycrystalline brackets (Transcend series 6000, 3M Unitek, Monrovia, CA, USA) Adhesive: Transbond XT (3 M Unitek, Monrovia, CA, USA) | 1 s = 2.74 ± 1.99 MPa 18 s = 10.36 ± 2.12 MPa 30 s = 16.38 ± 2.25 MPa 60 s = 18.11 ± 2.40 MPa | 1 s Score 1 × 1 Score 2 × 6 Score 3 × 13 18 s Score 1 × 3 Score 2 × 7 Score 3 × 10 30 s Score 1 × 3 Score 2 × 9 Score 3 × 8 60 s Score 1 × 4 Score 2 × 10 Score 3 × 6 | No data |
| Hoteit [63] | Er,Cr:YSGG laser (Waterlase MD, Biolase technology, Inc., Irvine, CA, USA) Wavelength: 2780 nm MX7 sapphire tip Beam diameter: 0.7 mm at the impact point Time: 6 s 70% air and 30% water Er:YAG laser (Fidelis; Fotona, Medical laser, Ljubljana, Slovenia) Wavelength: 2940 nm using 0.9 mm as a beam diameter at the impact point. | Six groups were debonded using Er,Cr:YSGG. Eight groups were debonded with an Er:YAG laser. | Brackets: adhesive pre-coated bracket (APC) Flash-free, 3M clarity advance ceramic brackets, Monrovia, CA, USA Adhesive: Transbond XT bonding (3M Unitek, Monrovia, CA, USA) 15 experimental groups based on various Er:YAG settings | The mean shear bond strength (SBS) levels: Er,Cr:YSGG 5 W/20 Hz: 5.30 ± 5.26 MPa Control group: 21.07 ± 1.80 MPa | No data | No data |
| Hamadah [64] | Er:YAG laser (Lightwalker® ST-E, 8 W, Fotona Inc., Ljubljana, Slovenia) Wavelength: 2940 nm Distance: 0.7 cm Laser spot size: 0.9 mm Pulse duration: 50, 100, and 300 μs Frequency: 30 Hz Water/air: 2 mL/s and 2 mL/s | Brackets were exposed to the Er:YAG laser for 6 s using the laser-scanning method. | Brackets: ceramic brackets (20/40™ Ceramic Brackets, American Orthodontics, Sheboygan, WI, USA) Adhesive: orthodontic composite (3M Unitek®, Transbond® XT, Monrovia, CA, USA) | No data | Group 1: 2, 3 Group 2: 3 Group 3: 3 | No data |
| Nalbantgil [65] | Er:YAG laser (VersaWave, Hoya ConBio, Fremont, CA, USA) Wavelength: 2940 nm Pulse repetition rate: 20 Hz Pulse duration: 300 ms Water spray: 40–50 mL/min Tip Diameter: 1 mm Laser irradiation for the three study groups: 1. 2 W(100 mJ at 20 Hz) 2. 4 W (200 mJ at 20 Hz) 3. 6 W (300 mJ at 20 Hz) | To assess the debonding site, adhesive remnant index (ARI) scores were noted. A thermocouple was used to prepare 60 human premolar teeth at the same energy levels and in the same manner in order to measure intrapulpal thermal increase. | Brackets: polycrystalline alumina brackets (Transcend series 6000; 3M Unitek, Monrovia, CA, USA) Adhesive: Transbond XT (3M Unitek, Monrovia, CA, USA) orthodontic adhesive system | No data | There was no statistical difference among experimental groups, excluding the control group. | The temperature increases were Group 2 W: 0.67 ± 12 °C Group 4 W:1.25 ± 0.16 °C Group 6 W: 2.36 ± 0.23 °C |
| Didem Nalbantgil [66] | ER:YAG laser 2940 nm Time: 3, 6, 9 s Distance: 2 mm Power: 4.2 W Beam diameter: 1 mm Frequency: 30 Hz Energy: 140 mJ | Debonding with shear test was carried out 45 s after the laser pulse; laser irradiation lasted 3, 6, 9 s. Control group without irradiation. | Polycrystalline alumina incisor brackets (Transcend series 6000, 3M Unitek, Monrovia, CA, USA) Adhesive: Transbond XT (3M Unitek, Monrovia, CA, USA) and light-cured with halogen light curing unit (Optilux, Kerr, Orange, CA, USA) | Control group: 22.76 MPa 3 s irradiation: 12.38 MPa 6 s irradiation: 10.75 MPa 9 s irradiation: 8.81 MPa | Control group: Score 0 × 1 Score 1 × 5 Score 2 × 10 Score 3 × 4 3 s group: Score 0 × 0 Score 1 × 3 Score 2 × 8 Score 3 × 9 6 s group: Score 0 × 0 Score 1 × 5 Score 2 × 6 Score 3 × 9 9 s group: Score 0 × 0 Score 1 × 0 Score 2 × 5 Score 3 × 15 | 3 s group: +1.27 °C 6 s group: +2.79 °C 9 s group: + 4.59 °C |
| Oztoprak, M. O. [67] | Er:YAG laser: wavelength: 2940 nm - power: 4.2 W - duration: 9 s per bracket - application method: scanning motion horizontally parallel to bracket slot - tip distance from bracket: 2 mm | Mechanical removal 45 s after laser exposure using shear force. Force applied occluso-gingivally using a universal testing machine. | Brackets: polycrystalline ceramic brackets (Transcend series 6000, 3M Unitek, Monrovia, CA, USA) Adhesive: Transbond XT (3M Unitek, Monrovia, CA, USA)), light-cured for 40 s | Mean: Control group = 20.75 MPa Laser group = 9.52 MPa | Control group: Score 0 × 3 Score 1 × 11 Score 2 × 12 Score 3 × 4 Laser group: Score 1 × 1 Score 2 × 10 Score 3 × 19 | No measurements during the procedure. |
| Alakuş-Sabuncuoǧlu, F. [68] | Er:YAG laser - wavelength: 2940 nm - mode: maxi short pulse (MSP) - pulse width: 100 μs - pulse frequency: 10 Hz - power: 3 W - energy per pulse: 120 mJ - duration: 6 s - application method: scanning in reverse S pattern - tip distance: 1 mm from bracket - used with air and water cooling | Mechanical removal using universal testing machine (Shimadzu Autograph AG-IS) with speed: 0.5 mm/min. | Brackets: polycrystalline ceramic brackets (Transcend series 6000, 3M Unitek, Monrovia, CA, USA) Adhesive: Transbond XT (3M Unitek, Monrovia, CA, USA)), light-cured for 10 s from 4 sides (total 40 s) | Mean: Control group: 13.42 ± 1.23 MPa Laser group: 8.47 ± 0.71 MPa | Control group: Score 0 × 2 Score 1 × 4 Score 2 × 4 Score 3 × 0 Laser group: Score 0 × 0 Score 1 × 1 Score 2 × 4 Score 3 × 5 | No measurements during the procedure. |
| Rao [69] | Er,Cr:YSGG laser 2780 nm Distance: 1 mm Power: 4.5 or 6 W | Following laser irradiation, the brackets were removed as per the manufacturer’s instructions. | Brackets: no data Adhesive: Transbond XT (3 M Unitek, Monrovia, CA, USA) | No data | Mean: 4.5 W = 1.33 (0.62) 6 W = 1.07 (0.59) | No data |
| Abdulaziz [70] | Er,Cr:YSGG laser (Waterlase iPlus; Biolase Technology Inc., Irvine, CA, USA) Wavelength: 2780 nm Frequency: 20 Hz Power: 4 W Tip diameter: 0.6 mm Pulse duration: 60 μs Level of air/fluid cooling: 70% air and 30% Time: 6 s | Scanning electron microscopy was used for the evaluation of the enamel’s microstructure, surface roughness following polishing, intrapulpal temperature increase, and adhesive remnant index (ARI). | Brackets: monocrystalline ceramic brackets (Perfect Clear, Hubit, Uiwang-si, Republic of Korea) Adhesive: Adhesive bond following Orthosolo (ORMCO, Orange, CA, USA). Debonding: Er,Cr:YSGG laser applications. | No data | Compared to the circular group, the conventional group had a substantially greater percentage of adhesive remnant index values of 2 and 3. Compared to the scanning group, the traditional group had a noticeably greater percentage of adhesive remnant index values of 2 and 3. | There was a significantly higher average intrapulpal temperature increase in the circular group (1.9 ± 0.5 °C) compared to the scanning group (0.9 ± 0.2 °C) |
| Stein [71] | 445 nm diode laser Time: 15 s Distance: in contact Beam diameter: 320 μm CW Power density: 2 W/cm2 Fluence: 30 J/cm2 | Debonding was performed using the laser tip in contact mode at a 90° angle to the bracket surface. | Polycrystalline brackets In-Ovation C (GAC, Grafelfing, Germany). Adhesive: Transbond XT (3M/Unitek, Monrovia, CA, USA). | No data | No data | Mean: Inner = 38.15 (0.51) °C Outside = 39.58 (2.38) °C |
| Stein [72] | 445 nm diode laser Time: 15 s Power: 2 W Beam diameter: 320 μm CW | Immediately after laser application, the bracket was removed with bracket-removal pliers. | Polycrystalline brackets In-Ovation C (GAC, Grafelfing, Germany). Adhesive: Transbond XT (3M/Unitek, Monrovia, CA, USA). | No data | Eye/10-fold magnification: Score 0 × 9 Score 2 × 2 Score 3 × 4 20-fold magnification: Score 0 × 8 Score 1 × 1 Score 2 × 4 Score 3 × 2 | No data |
| Stein [73] | 445 nm diode laser Time: 15 s Distance: in contact Beam diameter: 320 μm CW Power density: 2 W/cm2 Fluence: 30 J/cm2 | SBS was measured immediately after laser irradiation to three sides of the bracket bases. | Polycrystalline brackets In-Ovation C (GAC, Grafelfing, Germany) Adhesive: Transbond XT (3 M Unitek, Monrovia, CA, USA) | Mean = 10.08 MPa | Score 1 × 7 Score 2 × 7 Score 3 × 1 | No data |
| Yassaei [74] | Diode laser (Fox, ARC, Nürnberg, Germany) Wavelength: 980 nm Power: 2.5 W Time: 10 s Distance: 5 mm | The adhesive remnant index (ARI), lengths, and frequency of enamel cracks were examined between the groups following debonding. It was also measured how much the intrapulpal temperature increased. | Brackets: polycrystalline ceramic brackets (Allure, Whitinsville, MA, USA Adhesive: bonding primer (Resilience, Ortho Technology, Tampa, FL, USA) | No data | Conventional debonding Group 1: 1 (6.7%) Group 2: 3 (20%) Group 3: 8 (53.3%) Group 4: 3 (20%) Laser debonding Group 1: 1 (6.7%) Group 2: 7 (46.7%) Group 3: 5 (33.3%) Group 4: 2 (13.3%) | Changes in temp: 1.46 °C |
| Feldon [75] | Diode laser 2 or 5 W/cm2 | At two laser energy levels—2 and 5 W per square centimeter—the shear bond strength and heat effects on the pulp chamber were evaluated. Significant variations in shear bond strength values were identified. | Brackets: Inspire ICE (Ormco, Orange, CA, USA), a monocrystalline bracket; and Clarity (3M Unitek, Monrovia, CA, USA), a polycrystalline bracket Adhesive: single-paste visible light-cured orthodontic adhesive system, Transbond XT (3M Unitek, Monrovia, CA, USA) Both monocrystalline and polycrystalline ceramic brackets were attached to the maxillary central incisors of cows | Mean shear bond strength Group 1: 9.79 MPa Group 2: 9.68 MPa Group 3: 7.24 MPa Group 4: 15.99 MPa Group 5: 9.27 MPa Group 6: 8.88 MPa | There were no significant ARI score differences between any of the groups tested. Uniformly, they all had a mean ARI score of or close to 3. | The mean increases in pulp chamber temperature or groups 3, 4, and 5 were statistically significantly less than the 5.5 °C increase threshold and not significantly different from the 1.8 °C standard. Group 6 had a mean pulp chamber increase significantly greater than the 1.8 °C standard and not significantly different from the 5.5 °C standard. |
| Ayşe Sena Kabaş Sarp [76] | Ytterbium fiber laser 1070 nm Distance: 15 cm Power: 20 W Beam diameter: 1.6 mm Laser mode: CW and modulated mode | The laser was turned on synchronously with shear load application and turned off when the bracket was debonded. | Polycrystalline ceramic brackets (G&H, Franklin, IN, USA) Adhesive: chemically curing Bis-GMA resin (3M, Unite Bonding Adhesive Set, St. Paul, MN, USA) | No Data | No Data | CW mode: 1. Control group 2. +1.77 °C 3. +3.2 °C 4. +3.7 °C 5. +8.6 °C Modulated mode: 200/600 + 2.7 °C 300/900 + 3.1 °C 400/1200 + 2.9 °C |
| Author | Sample Size Calculation | Group Size of at Least 10 Subjects | Control Group | Detailed Description of Laser Parameters | Detailed Description of the Debonding Method | Randomization | Total | Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Khalil [3] | 1 | 1 | 1 | 1 | 1 | 1 | 6 | Low |
| Tocchio [12] | 0 | 1 | 0 | 1 | 1 | 1 | 4 | Moderate |
| Grzech-Leśniak [13] | 0 | 1 | 1 | 1 | 1 | 0 | 4 | Moderate |
| Arima [39] | 0 | 1 | 1 | 1 | 1 | 1 | 5 | Low |
| Macri [40] | 0 | 1 | 1 | 1 | 1 | 1 | 5 | Low |
| Ahrari [41] | 0 | 1 | 1 | 1 | 1 | 1 | 5 | Low |
| Matos [42] | 0 | 1 | 1 | 0 | 1 | 1 | 4 | Moderate |
| Saito [43] | 0 | 1 | 0 | 1 | 1 | 1 | 4 | Moderate |
| Strobl [44] | 0 | 1 | 0 | 0 | 1 | 0 | 2 | High |
| Ma [45] | 0 | 1 | 1 | 1 | 1 | 0 | 4 | Moderate |
| Obata [46] | 0 | 1 | 1 | 0 | 0 | 0 | 2 | High |
| Iijima [47] | 0 | 1 | 1 | 1 | 1 | 1 | 5 | Low |
| Mimura [48] | 0 | 1 | 1 | 0 | 1 | 0 | 3 | Moderate |
| Tehranchi [49] | 0 | 1 | 1 | 1 | 1 | 0 | 4 | Moderate |
| Demirkan [50] | 0 | 0 | 1 | 1 | 1 | 0 | 3 | Moderate |
| Dostalová [51] | 0 | 1 | 1 | 0 | 1 | 0 | 3 | Moderate |
| Dostalova [52] | 0 | 1 | 1 | 1 | 1 | 0 | 4 | Moderate |
| Dostálová [53] | 0 | 1 | 0 | 1 | 1 | 0 | 3 | Moderate |
| Han [54] | 0 | 1 | 0 | 1 | 0 | 0 | 2 | High |
| Hayakawa [55] | 0 | 1 | 1 | 1 | 1 | 1 | 5 | Low |
| Downarowicz [56] | 0 | 1 | 0 | 1 | 1 | 0 | 3 | Moderate |
| Yilanci [57] | 0 | 1 | 0 | 1 | 0 | 0 | 2 | High |
| Mocuta [58] | 1 | 1 | 0 | 1 | 0 | 1 | 4 | Moderate |
| Dostalova [59] | 0 | 1 | 1 | 1 | 1 | 0 | 4 | Moderate |
| Mirhashemi [60] | 0 | 1 | 1 | 1 | 1 | 0 | 4 | Moderate |
| Mundethu [61] | 0 | 1 | 0 | 1 | 0 | 0 | 2 | High |
| Tozlu [62] | 0 | 1 | 1 | 1 | 1 | 1 | 5 | Low |
| Hoteit [63] | 0 | 1 | 1 | 1 | 0 | 1 | 4 | Moderate |
| Hamadah [64] | 0 | 1 | 0 | 1 | 0 | 1 | 3 | Moderate |
| Nalbantgil [65] | 0 | 1 | 1 | 1 | 0 | 1 | 4 | Moderate |
| Nalbantgil [66] | 0 | 1 | 1 | 1 | 1 | 1 | 5 | Low |
| Oztoprak [67] | 0 | 1 | 1 | 1 | 1 | 1 | 5 | Low |
| Alakuş-sabuncuoğlu [68] | 0 | 1 | 1 | 1 | 0 | 1 | 4 | Moderate |
| Rao [69] | 0 | 1 | 1 | 0 | 1 | 1 | 4 | Moderate |
| Abdulaziz [70] | 1 | 1 | 1 | 1 | 1 | 0 | 5 | Low |
| Stein [71] | 1 | 1 | 0 | 1 | 1 | 0 | 4 | Moderate |
| Stein [72] | 1 | 1 | 0 | 1 | 1 | 1 | 5 | Low |
| Stein [73] | 0 | 1 | 1 | 1 | 1 | 1 | 5 | Low |
| Yassaei [74] | 0 | 1 | 0 | 1 | 1 | 1 | 4 | Moderate |
| Feldon [75] | 0 | 1 | 1 | 0 | 1 | 0 | 3 | Moderate |
| Sarp [76] | 0 | 0 | 1 | 1 | 1 | 0 | 3 | Moderate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michalak, M.; Kiryk, S.; Kotela, A.; Wiśniewska, K.; Kiryk, J.; Zborowski, J.Z.; Matys, J.; Dobrzyński, M. Orthodontic Ceramic Bracket Removal Using Lasers: A Systematic Review. J. Funct. Biomater. 2025, 16, 123. https://doi.org/10.3390/jfb16040123
Michalak M, Kiryk S, Kotela A, Wiśniewska K, Kiryk J, Zborowski JZ, Matys J, Dobrzyński M. Orthodontic Ceramic Bracket Removal Using Lasers: A Systematic Review. Journal of Functional Biomaterials. 2025; 16(4):123. https://doi.org/10.3390/jfb16040123
Chicago/Turabian StyleMichalak, Mateusz, Sylwia Kiryk, Agnieszka Kotela, Kamila Wiśniewska, Jan Kiryk, Jacek Zbigniew Zborowski, Jacek Matys, and Maciej Dobrzyński. 2025. "Orthodontic Ceramic Bracket Removal Using Lasers: A Systematic Review" Journal of Functional Biomaterials 16, no. 4: 123. https://doi.org/10.3390/jfb16040123
APA StyleMichalak, M., Kiryk, S., Kotela, A., Wiśniewska, K., Kiryk, J., Zborowski, J. Z., Matys, J., & Dobrzyński, M. (2025). Orthodontic Ceramic Bracket Removal Using Lasers: A Systematic Review. Journal of Functional Biomaterials, 16(4), 123. https://doi.org/10.3390/jfb16040123








