Enhancing Bioactivity and Mechanical Properties of Nano-Hydroxyapatite Derived from Oyster Shells through Hydrothermal Synthesis
Abstract
:1. Introduction
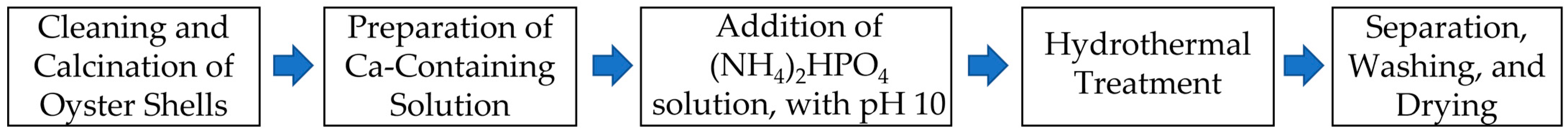
2. Materials and Methods
3. Results and Discussion
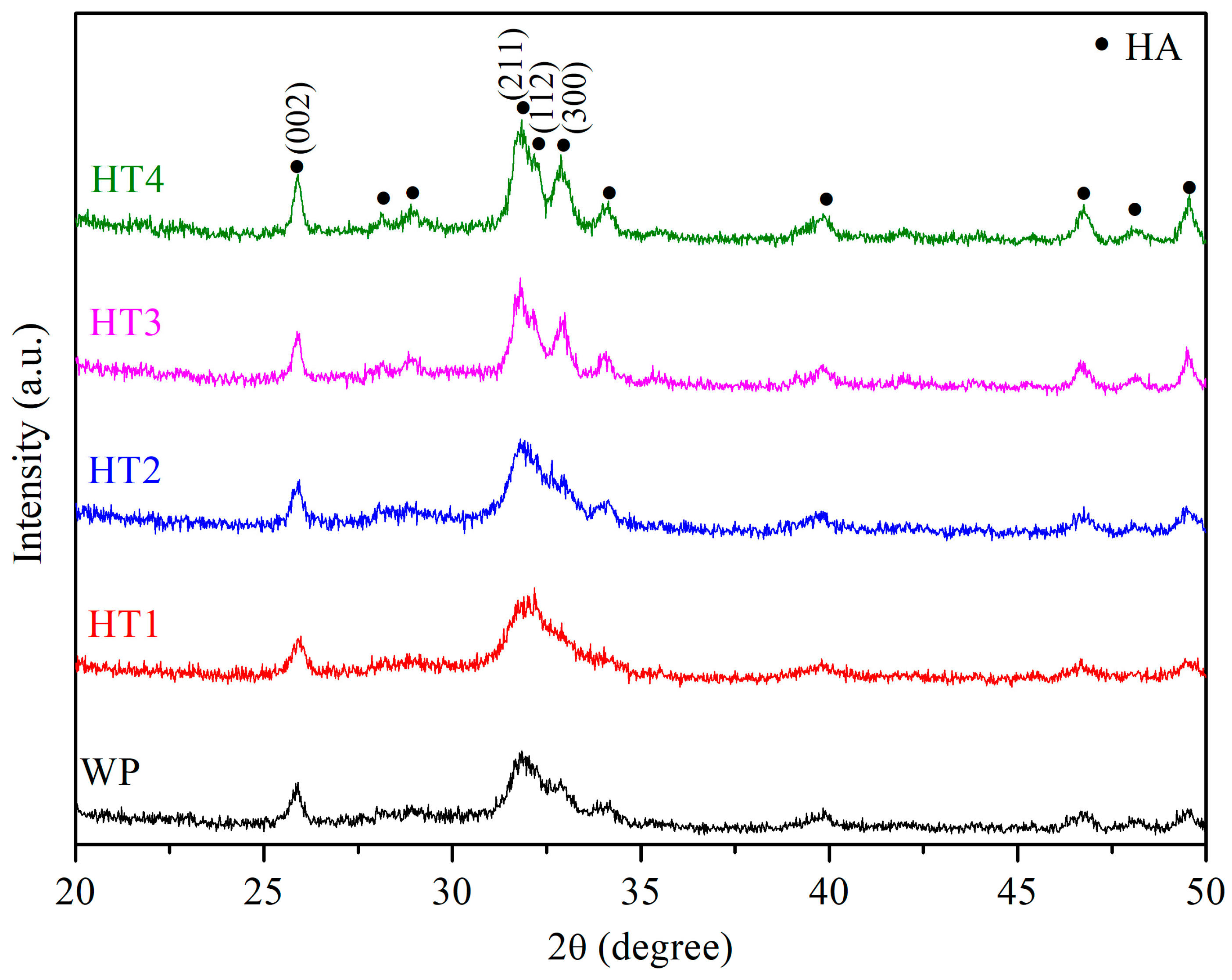
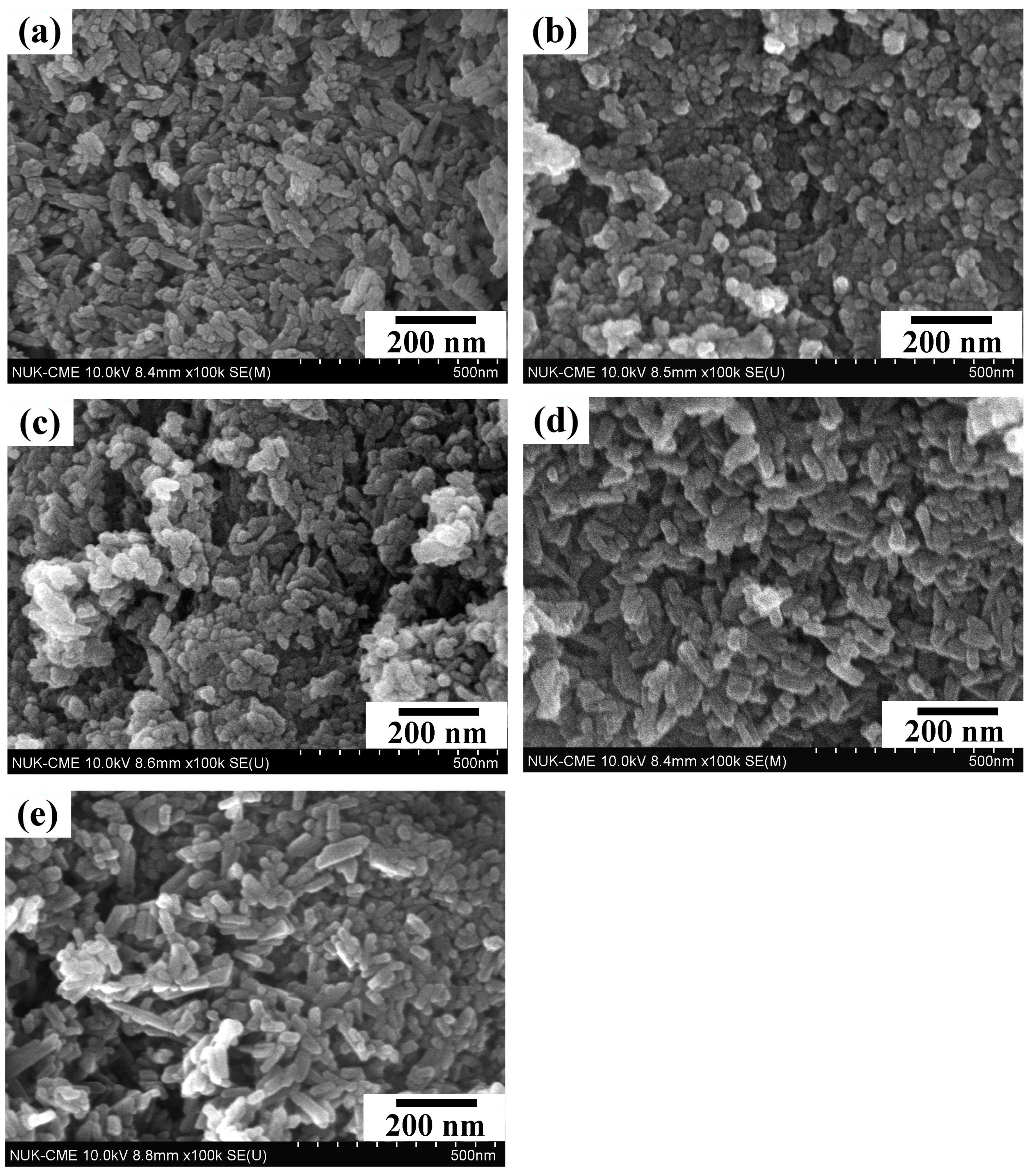
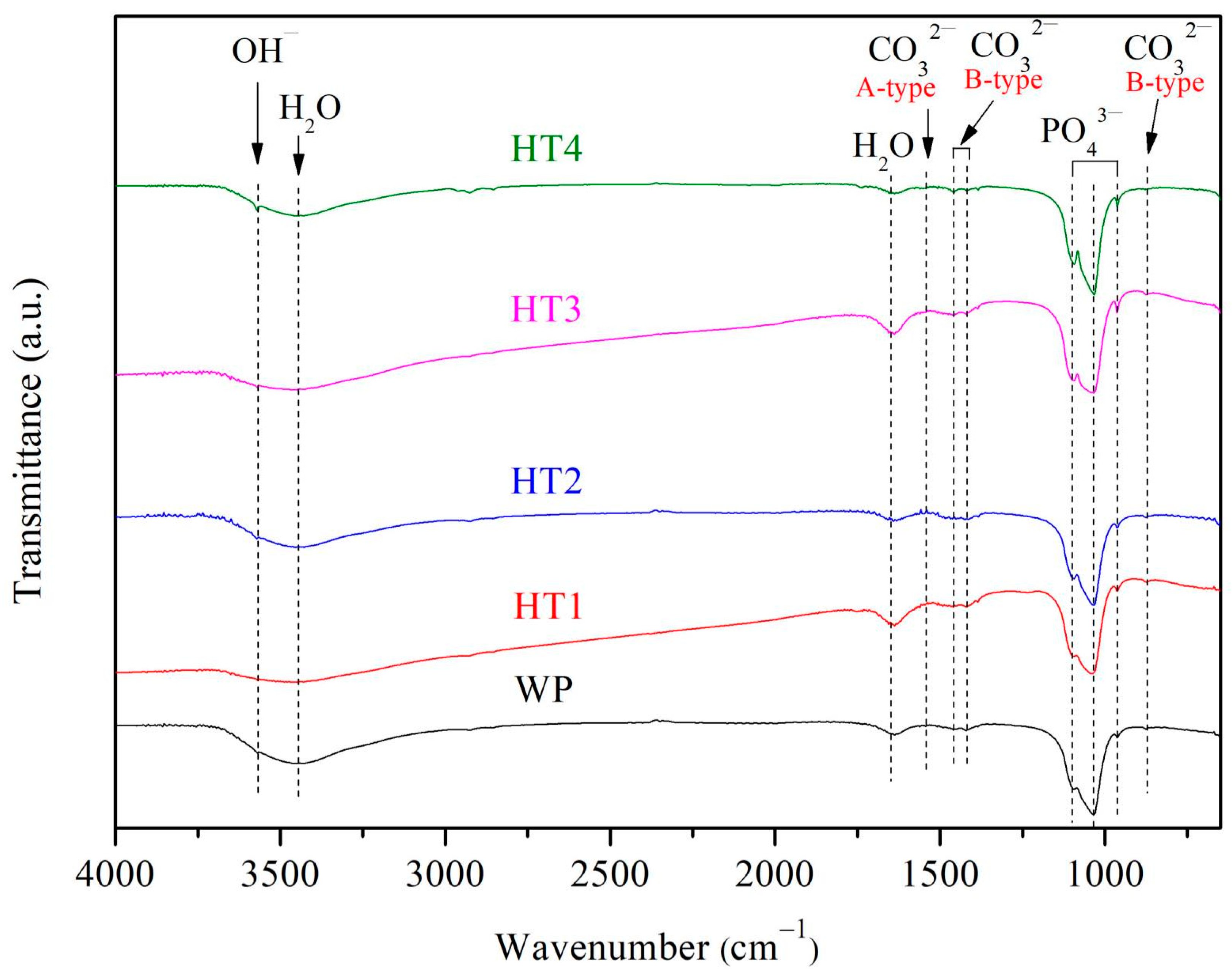
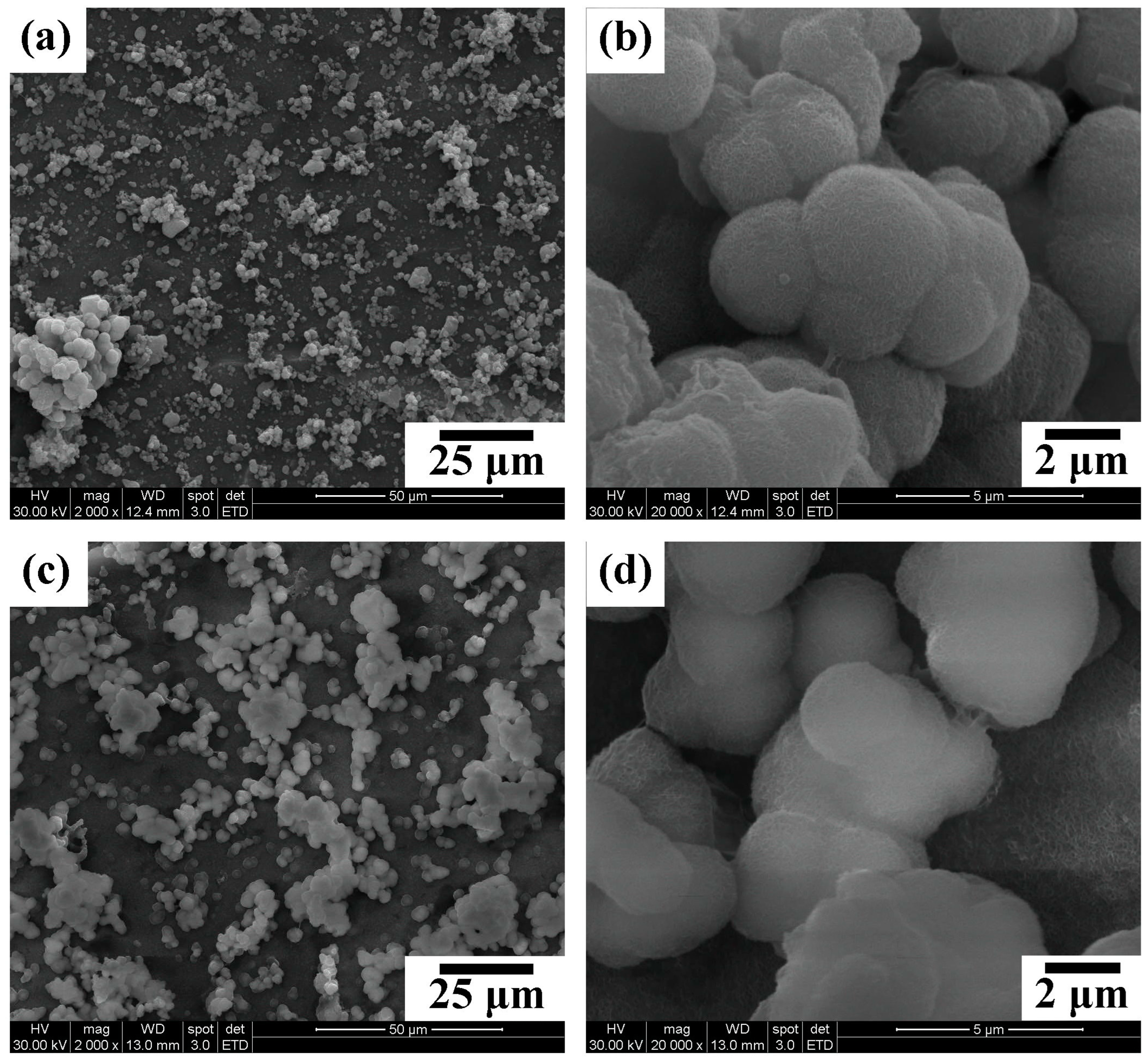
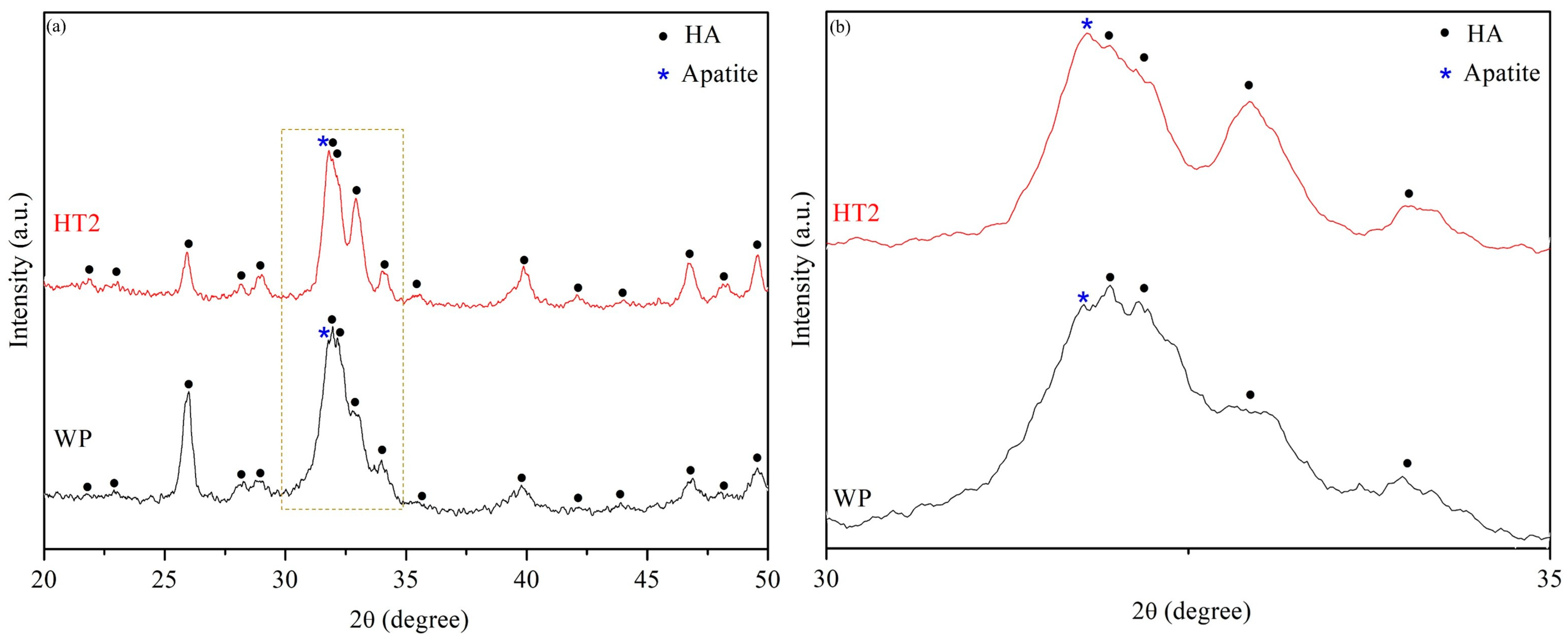
3.1. Characteristics of nHA Prepared under Various Hydrothermal Reaction Times
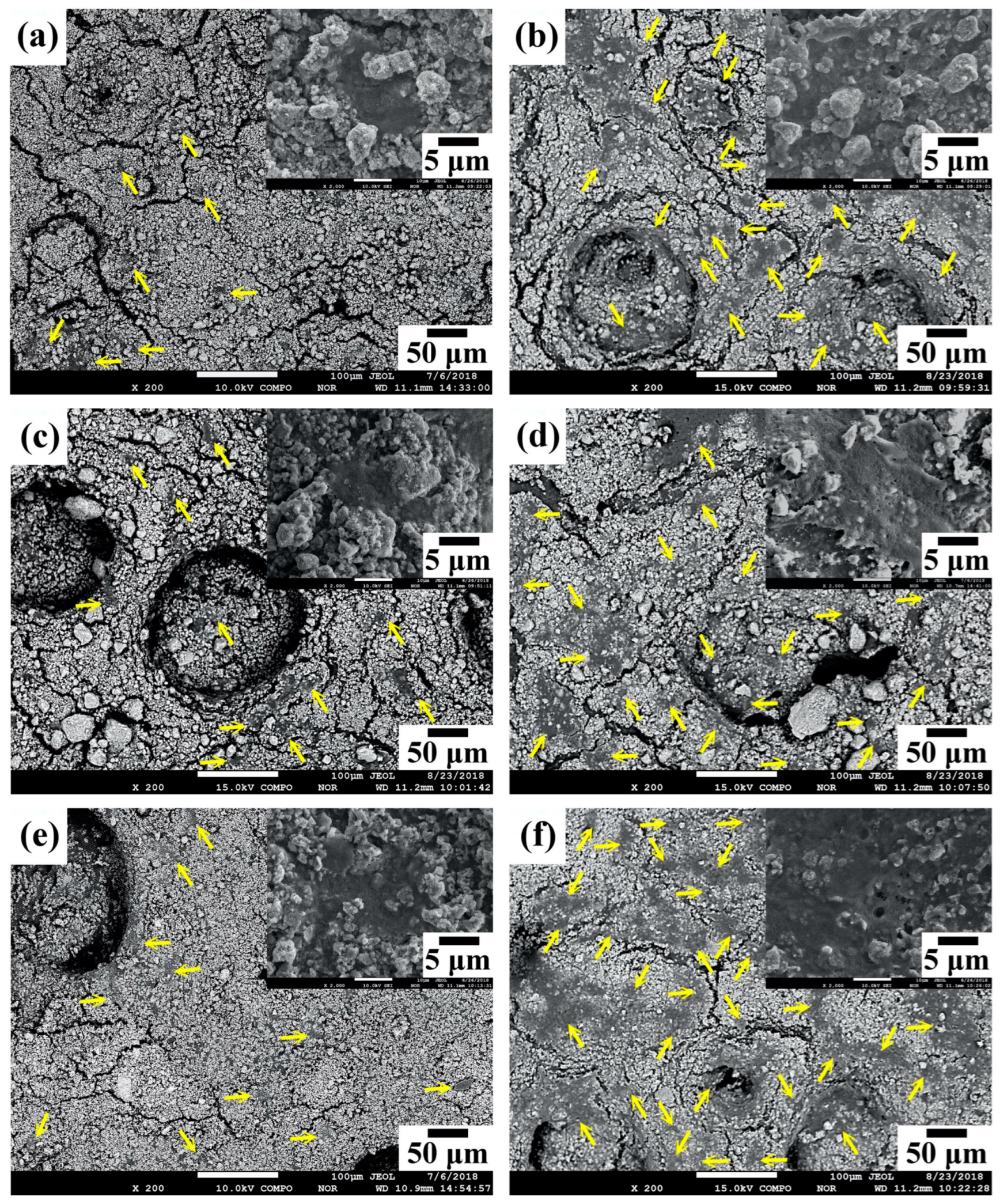
3.2. Bioactivity Evaluation
3.3. Cell Culture
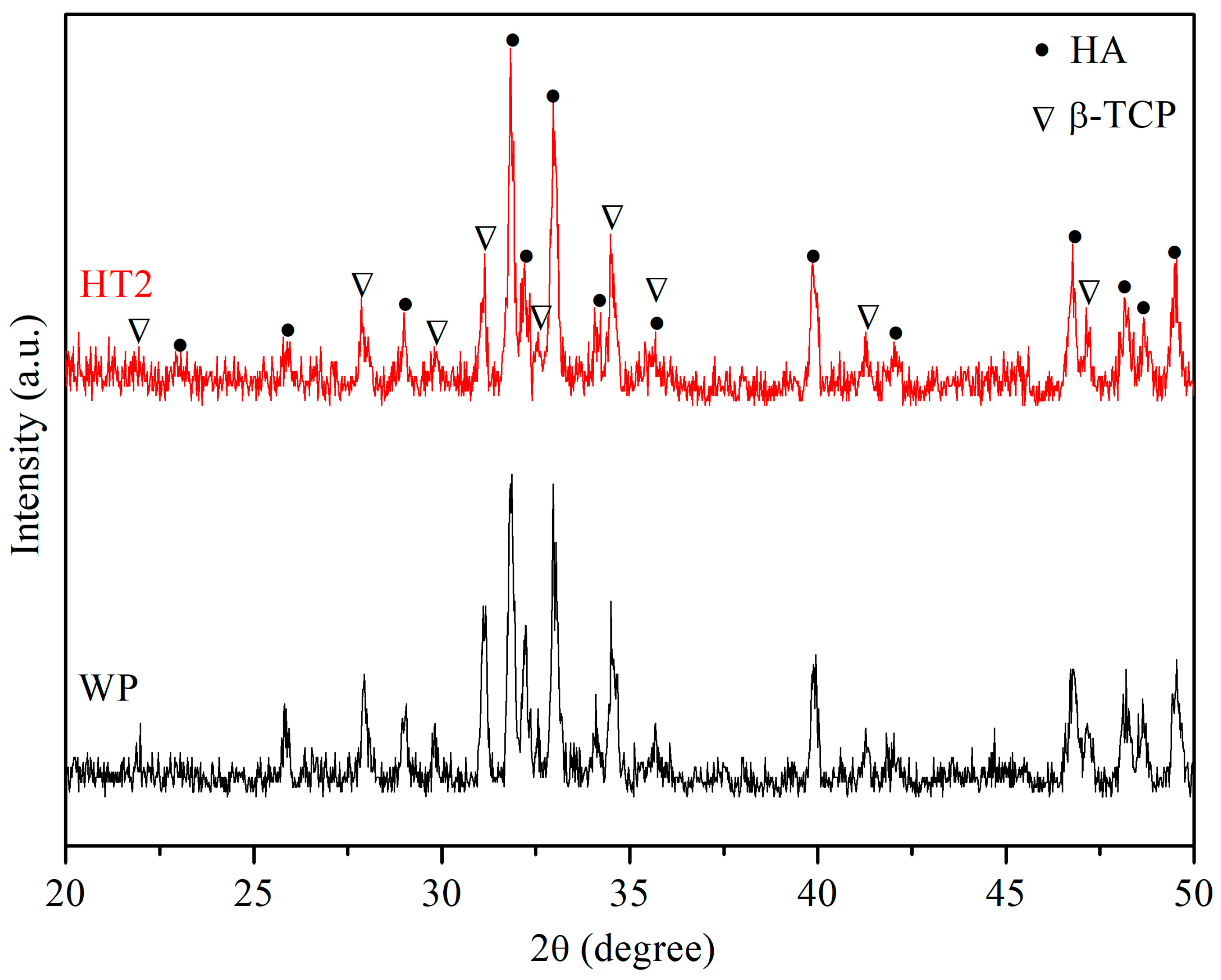
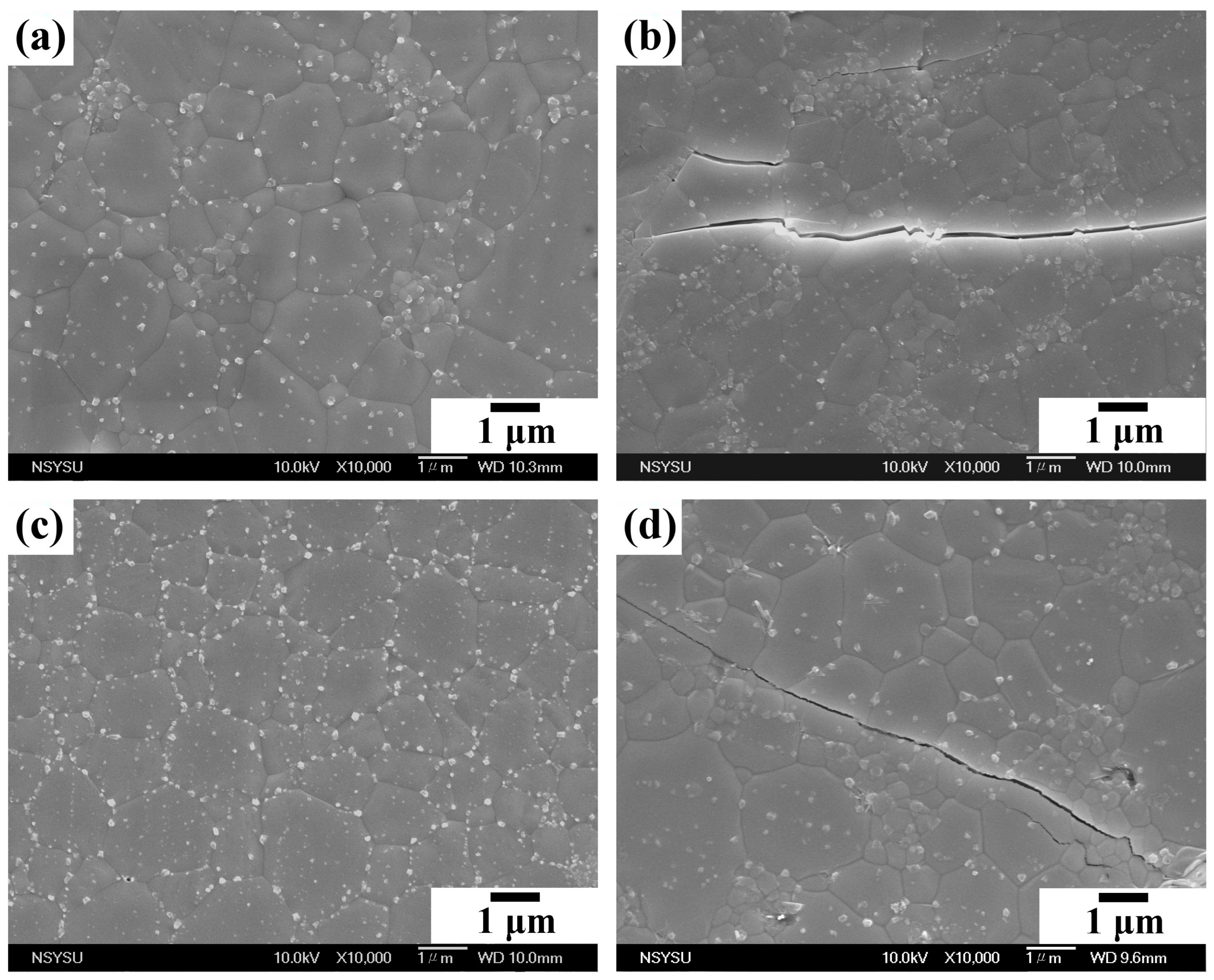
3.4. Sintering Properties
4. Conclusions
- Synthesis and crystallinity: Nano-grade HA was successfully synthesized using both wet precipitation and hydrothermal methods. The crystallinity of the nHA synthesized by the hydrothermal method was greater than that of the precipitation method. As the hydrothermal reaction time increased, the crystallinity of nHA also increased. Additionally, the hydrothermal time influenced the particle morphology; the nHA particles exhibited a rod-like shape when the reaction time exceeded 6 h, with the particle aspect ratio increasing over time.
- Yield and purity: HT2 presented the highest yield of 59.27% in this study. The XRD results showed that only a single HA phase was present, with no secondary phases or residual raw materials detected.
- Composition and trace elements: The synthesized nHA exhibited AB-type carbonation, with some OH− and PO43− groups substituted by CO32−. It also contained beneficial trace elements such as Na, Mg, K, and Sr, derived from the oyster shells, which promote human bone tissue growth.
- Bioactivity and cell proliferation: After 28 days of immersion in SBF, the formation of bone-like apatite on the surfaces of the WP and HT2 samples was observed, indicating superior bioactivity. Both the WP and HT2 samples supported good cell proliferation and attachment. On day 1, the osteoblasts on the surface of HT2 exhibited a flattened and spread morphology. By day 7, the HT2 sample displayed the largest cell coverage area.
- Mechanical properties: The WP and HT2 samples were compacted and sintered at 1200 °C for 4 h. The microhardness values were 5.26 GPa for WP and 5.65 GPa for HT2, while the fracture toughness values were 0.97 MPa·m0.5 for WP and 1.23 MPa·m0.5 for HT2. These values are higher than the microhardness (2.61–3.13 GPa) and fracture toughness (0.94 MPa·m0.5) of human tooth enamel, with HT2 showing superior performance.
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dominguez-Prado, D.M.; Ferradas-Garcia, L.; Perez-Alfonso, E.; Balvis-Balvis, P.; Lopez-Lopez, J.A.; Castro-Menendez, M. Epidemiology of Bone Fractures in the Hand in Adult Population Using the ICD-10 Classification. Acta Chir. Orthop. Traumatol. Cechoslov. 2022, 89, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Homa, K.; Zakrzewski, W.; Dobrzyński, W.; Piszko, P.J.; Piszko, A.; Matys, J.; Wiglusz, R.J.; Dobrzyński, M. Surface Functionalization of Titanium-Based Implants with a Nanohydroxyapatite Layer and Its Impact on Osteoblasts: A Systematic Review. J. Funct. Biomater. 2024, 15, 45. [Google Scholar] [CrossRef]
- Fendi, F.; Abdullah, B.; Suryani, S.; Usman, A.N.; Tahir, D. Development and application of hydroxyapatite-based scaffolds for bone tissue regeneration: A systematic literature review. Bone 2024, 183, 117075. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Shen, Y.; Jiang, L.; Zhang, Y. Surface Modification of Nano-Hydroxyapatite/Polymer Composite for Bone Tissue Repair Applications: A Review. Polymers 2024, 16, 1263. [Google Scholar] [CrossRef] [PubMed]
- Damiri, F.; Fatimi, A.; Musuc, A.M.; Santos, A.C.P.; Paszkiewicz, S.; Idumah, C.I.; Singh, S.; Varma, R.S.; Berrada, M. Nano-hydroxyapatite (nHAp) scaffolds for bone regeneration: Preparation, characterization and biological applications. J. Drug Deliv. Technol. 2024, 95, 105601. [Google Scholar] [CrossRef]
- Marchenko, E.S.; Dubovikov, K.M.; Baigonakova, G.A.; Shishelova, A.A.; Topolnitskiy, E.B.; Chernyshova, A.L. The influence of hydroxyapatite coatings with different structure and crystallinity on osteogenesis stimulation. Ceram. Int. 2024, 50, 27317–27330. [Google Scholar] [CrossRef]
- Surmeneva, M.A.; Ivanova, A.A.; Tian, Q.; Pittman, R.; Jiang, W.; Lin, J.; Liu, H.H.; Surmenev, R.A. Bone marrow derived mesenchymal stem cell response to the RF magnetron sputter deposited hydroxyapatite coating on AZ91 magnesium alloy. Mater. Chem. Phys. 2019, 221, 89–98. [Google Scholar] [CrossRef]
- Gelati, L.; Rabufetti, M.; Benaglia, M.; Campisi, S.; Gervasini, A.; Speranza, G.; Morelli, C.F. Hydroxyapatite: An eco-friendly material for enzyme immobilization. ChemPlusChem 2024, e202400204. [Google Scholar] [CrossRef] [PubMed]
- Weerasuriya, D.R.K.; Wijesinghe, W.P.S.L.; Rajapakse, R.M.G. Encapsulation of anticancer drug copper bis (8-hydroxyquinoline) in hydroxyapatite for pH-sensitive targeted delivery and slow release. Mater. Sci. Eng. C 2017, 71, 206–213. [Google Scholar] [CrossRef]
- Balasooriya, I.L.; Chen, J.; Korale Gedara, S.M.; Han, Y.; Wickramaratne, M.N. Applications of Nano Hydroxyapatite as Adsorbents: A Review. Nanomaterials 2022, 12, 2324. [Google Scholar] [CrossRef]
- Sun, D.; Liao, T.; Lin, H.; Sang, Y.; Liu, Y.; Ma, Q.; Yu, Z.; Zhang, B.; Jiang, W. Sustainable double-synergistic silver-hydroxyapatite composite catalyst derived from fish bones for efficient disinfection of Vibrio parahaemolyticus. Food Chem. 2024, 456, 139915. [Google Scholar] [CrossRef] [PubMed]
- Ramesh, S.; Loo, Z.Z.; Tan, C.Y.; Kelvin Chew, W.J.; Ching, Y.C.; Tarlochan, F.; Chandran, H.; Krishnasamy, S.; Bang, L.T.; Sarhan, A.A.D. Characterization of biogenic hydroxyapatite derived from animal bones for biomedical applications. Ceram. Int. 2018, 44, 10525–10530. [Google Scholar] [CrossRef]
- Adhikara, A.G.; Maharani, A.P.; Puspitasari, A.; Nuswantoro, N.F.; Juliadmi, D.; Maras, M.A.J.; Nugroho, D.B.; Saksono, B.; Gunawarman. Bovine hydroxyapatite for bone tissue engineering: Preparation, characterization, challenges, and future perspectives. Eur. Polym. J. 2024, 214, 113171. [Google Scholar] [CrossRef]
- Wu, S.C.; Hsu, H.C.; Liu, M.Y.; Ho, W.F. Characterization of nanosized hydroxyapatite prepared by an aqueous precipitation method using eggshells and mulberry leaf extract. J. Korean Ceram. Soc. 2021, 58, 116–122. [Google Scholar] [CrossRef]
- Wu, S.C.; Kao, Y.L.; Lu, Y.C.; Hsu, H.C.; Ho, W.F. Preparation and characterization of microrod hydroxyapatite bundles obtained from oyster shells through microwave irradiation. J. Aust. Ceram. Soc. 2021, 57, 1541–1551. [Google Scholar] [CrossRef]
- Wu, S.-C.; Hsu, H.-C.; Wang, H.-F.; Liou, S.-P.; Ho, W.-F. Synthesis and Characterization of Nano-Hydroxyapatite Obtained from Eggshell via the Hydrothermal Process and the Precipitation Method. Molecules 2023, 28, 4926. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Ye, X.; Wang, H.; Zhu, M.; Wang, B.; Yan, H. The influence of pH and temperature on the morphology of hydroxyapatite synthesized by hydrothermal method. Ceram. Int. 2003, 29, 629–633. [Google Scholar] [CrossRef]
- Jin, X.; Chen, X.; Cheng, Y.; Wang, L.; Hu, B.; Tan, J. Effects of hydrothermal temperature and time on hydrothermal synthesis of colloidal hydroxyapatite nanorods in the presence of sodium citrate. J. Colloid Interface Sci. 2015, 450, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Alif, M.F.; Aprillia, W.; Arief, S. A hydrothermal synthesis of natural hydroxyapatite obtained from Corbicula moltkiana freshwater clams shell biowaste. Mater. Lett. 2018, 230, 40–43. [Google Scholar] [CrossRef]
- Ferro, A.C.; Guedes, M. Mechanochemical synthesis of hydroxyapatite using cuttlefish bone and chicken eggshell as calcium precursors. Mater. Sci. Eng. C 2019, 97, 124–140. [Google Scholar] [CrossRef]
- Hsieh, K.-H.; Hsu, H.-C.; Kao, Y.-L.; Wu, S.-C.; Yang, T.-Y.; Ho, W.-F. Nanohydroxyapatite/Peptide Composite Coatings on Pure Titanium Surfaces with Nanonetwork Structures Using Oyster Shells. Nanomaterials 2024, 14, 577. [Google Scholar] [CrossRef] [PubMed]
- Raudonyte-Svirbutaviciene, E.; Klydziute, G.; Lukaviciute, L.; Antuzevics, A.; Balciunaite, A.; Norkus, E.; Beganskiene, A.; Zarkov, A.; Kareiva, A. Hydrothermal synthesis of Mn2+- and Cu2+-doped calcium hydroxyapatite: Morphological features and importance of EPR insights. Ceram. Int. 2024, 50, 4005–4013. [Google Scholar] [CrossRef]
- Nouri-Felekori, M.; Khakbiz, M.; Nezafati, N. Synthesis and characterization of Mg, Zn and Sr-incorporated hydroxyapatite whiskers by hydrothermal method. Mater. Lett. 2019, 243, 120–124. [Google Scholar] [CrossRef]
- Ho, W.F.; Lee, M.H.; Thomas, J.L.; Li, J.A.; Wu, S.C.; Hsu, H.C.; Lin, H.Y. Porous biphasic calcium phosphate granules from oyster shell promote the differentiation of induced pluripotent stem cells. Int. J. Mol. Sci. 2021, 22, 9444. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.C.; Hsu, H.C.; Hsu, S.K.; Tseng, C.P.; Ho, W.F. Preparation and characterization of hydroxyapatite synthesized from oyster shell powders. Adv. Powder Technol. 2017, 28, 1154–1158. [Google Scholar] [CrossRef]
- Du, M.; Chen, J.; Liu, K.; Xing, H.; Song, C. Recent advances in biomedical engineering of nano-hydroxyapatite including dentistry, cancer treatment and bone repair. Compos. B Eng. 2021, 215, 108790. [Google Scholar] [CrossRef]
- Mo, X.; Zhang, D.; Liu, K.; Zhao, X.; Li, X.; Wang, W. Nano-Hydroxyapatite Composite Scaffolds Loaded with Bioactive Factors and Drugs for Bone Tissue Engineering. Int. J. Mol. Sci. 2023, 24, 1291. [Google Scholar] [CrossRef] [PubMed]
- Bordea, I.R.; Candrea, S.; Alexescu, G.T.; Bran, S.; Baciut, M.; Baciut, G.; Lucaciu, O.; Dinu, C.M.; Todea, D.A. Nano-hydroxyapatite use in dentistry: A systematic review. Drug Metab. Rev. 2020, 52, 319–332. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Nanosized and nanocrystalline calcium orthophosphates. Acta Biomater. 2010, 6, 715–734. [Google Scholar] [CrossRef]
- Kalita, S.J.; Bhardwaj, A.; Bhatt, H.A. Nanocrystalline calcium phosphate ceramics in biomedical engineering. Mater. Sci. Eng. C 2007, 27, 441–449. [Google Scholar] [CrossRef]
- Mardziah, C.M.; Ramesh, S.; Wahid, M.A.; Chandran, H.; Sidhu, A.; Krishnasamy, S.; Purbolaksono, J.J.C.I. Effect of zinc ions on the structural characteristics of hydroxyapatite bioceramics. Ceram. Int. 2020, 46, 13945–13952. [Google Scholar] [CrossRef]
- Landi, E.; Tampieri, A.; Celotti, G.; Sprio, S. Densification behaviour and mechanisms of synthetic hydroxyapatites. J. Eur. Ceram. Soc. 2000, 20, 2377–2387. [Google Scholar] [CrossRef]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef] [PubMed]
- ASTM E112-96; Standard Test Methods for Determining Average Grain Size. ASTM International: Philadelphia, PA, USA, 1996.
- ASTM C1327-15; Standard Test Method for Vickers Indentation Hardness of Advanced Ceramics. ASTM International: West Conshohocken, PA, USA, 2019.
- Niihara, K.; Morena, R.; Hasselman, D. Evaluation of KIC of brittle solids by the indentation method with low crack-to-indent ratios. J. Mater. Sci. Lett. 1982, 1, 13–16. [Google Scholar] [CrossRef]
- Ibraheema, S.A.; Audub, E.A.; Jaafara, M.; Adudua, J.A.; Barminasa, J.T.; Ochigbob, V.; Igunnuc, A.; Malomo, S.O. Novel pectin from Parkia biglobosa pulp mediated green route synthesis of hydroxyapatite nanoparticles. Surf. Interfaces 2019, 17, 100360. [Google Scholar] [CrossRef]
- Wolff, J.; Hofmann, D.; Amelung, W.; Lewandowski, H.; Kaiser, K.; Bol, R. Rapid wet chemical synthesis for 33P-labelled hydroxyapatite–An approach for environmental research. Appl. Geochem. 2018, 97, 181–186. [Google Scholar] [CrossRef]
- Wang, X.; Li, Y.; Wei, J.; de Groot, K. Development of Biomimetic Nano-Hydroxyapatite/Poly(Hexamethylene Adipamide) Composites. Biomaterials 2002, 23, 4787–4791. [Google Scholar] [CrossRef] [PubMed]
- Webster, T.J.; Ergun, C.; Doremus, R.H.; Siegel, R.W.; Bizios, R. Enhanced osteoclast-like cell functions on nanophase ceramics. Biomaterials 2001, 22, 1327–1333. [Google Scholar] [CrossRef] [PubMed]
- Mohan, N.; Palangadan, R.; Varma, H. Hydroxyapatite scaffolds constituting highly oriented crystals derived from synthetic precursors by hydrothermal reactions. Ceram. Int. 2016, 42, 17259–17268. [Google Scholar] [CrossRef]
- Inoue, K.; Sassa, K.; Yokogawa, Y.; Sakka, Y.; Okido, M.; Asai, S. Control of crystal orientation of hydroxyapatite by imposition of a high magnetic field. Mater. Trans. 2003, 44, 1133–1137. [Google Scholar] [CrossRef]
- LeGeros, R.Z. Calcium phosphate-based osteoinductive materials. Chem. Rev. 2008, 108, 4742–4753. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Liao, X.; Zheng, L.; He, H.; Wang, H.; Fan, H.; Zhang, X. Preparation and cellular response of porous A-type carbonated hydroxyapatite nanoceramics. Mater. Sci. Eng. C 2012, 32, 929–936. [Google Scholar] [CrossRef]
- Xiao, W.; Bal, B.S.; Rahaman, M.N. Preparation of resorbable carbonate-substituted hollow hydroxyapatite microspheres and their evaluation in osseous defects in vivo. Mater. Sci. Eng. C 2016, 60, 324–332. [Google Scholar] [CrossRef] [PubMed]
- Cui, W.; Song, Q.; Su, H.; Yang, Z.; Yang, R.; Li, N.; Zhang, X. Synergistic effects of Mg-substitution and particle size of chicken eggshells on hydrothermal synthesis of biphasic calcium phosphate nanocrystals. J. Mater. Sci. Technol. 2020, 36, 27–36. [Google Scholar] [CrossRef]
- Li, H.; Zhao, X.; Cao, S.; Li, K.; Chen, M.; Xu, Z.; Lu, J.; Zhang, L. Na-doped hydroxyapatite coating on carbon/carbon composites: Preparation, in vitro bioactivity and biocompatibility. Appl. Surf. Sci. 2012, 263, 163–173. [Google Scholar] [CrossRef]
- Bushinsky, D.A.; Riordon, D.R.; Chan, J.S.; Krieger, N.S. Decreased potassium stimulates bone resorption. Am. J. Physiol. Cell Physiol. 1997, 272, F774–F780. [Google Scholar] [CrossRef] [PubMed]
- Hayhoe, R.P.; Lentjes, M.A.; Luben, R.N.; Khaw, K.T.; Welch, A.A. Dietary magnesium and potassium intakes and circulating magnesium are associated with heel bone ultrasound attenuation and osteoporotic fracture risk in the EPIC Norfolk cohort study. Am. J. Clin. Nutr. 2015, 102, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Marie, P.J. Strontium ranelate: A novel mode of action optimizing bone formation and resorption. Osteoporos. Int. 2005, 16, S7–S10. [Google Scholar] [CrossRef] [PubMed]
- Meunier, P.J.; Roux, C.; Seeman, E.; Ortolani, S.; Badurski, J.E.; Spector, T.D.; Cannata, J.; Balogh, A.; Lemmel, E.M.; Pors-Nielsen, S.; et al. The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N. Engl. J. Med. 2004, 350, 459–468. [Google Scholar] [CrossRef] [PubMed]
- ASTM F1185-03; Standard Specification for Composition of Hydroxylapatite for Surgical Implants. ASTM International: West Conshohocken, PA, USA, 2009.
- Zhao, X.; Zhang, W.; Wang, Y.; Liu, Q.; Yang, J.; Zhang, L.; He, F. Fabrication of Al2O3 by anodic oxidation and hydrothermal synthesis of strong-bonding hydroxyapatite coatings on its surface. Appl. Surf. Sci. 2019, 470, 959–969. [Google Scholar] [CrossRef]
- Sachiko, H.S.; Jun, S.; Makoto, S.; Hideaki, E. Determination of fracture toughness of human permanent and primary enamel using an indentation microfracture method. J. Mater. Sci. Mater. Med. 2012, 23, 2047–2054. [Google Scholar] [CrossRef]
- Ge, J.; Cui, F.Z.; Wang, X.M.; Feng, H.L. Property variations in the prism and the organic sheath within enamel by nanoindentation. Biomaterials 2005, 26, 3333–3339. [Google Scholar] [CrossRef] [PubMed]
- Ayatollahi, M.R.; Karimzadeh, A. Nano-indentation measurement of fracture toughness of dental enamel. Int. J. Fract. 2013, 183, 113–118. [Google Scholar] [CrossRef]
- Magazzù, A.; Marcuello, C. Investigation of Soft Matter Nanomechanics by Atomic Force Microscopy and Optical Tweezers: A Comprehensive Review. Nanomaterials 2023, 13, 963. [Google Scholar] [CrossRef]
- Li, F.; Jiang, X.; Shao, Z.; Zhu, D.; Luo, Z. Microstructure and Mechanical Properties of Nano-Carbon Reinforced Titanium Matrix/Hydroxyapatite Biocomposites Prepared by Spark Plasma Sintering. Nanomaterials 2018, 8, 729. [Google Scholar] [CrossRef]

| Sample Code | Hydrothermal | Wet Precipitation |
|---|---|---|
| HT1 | 150 °C, 10 min | – |
| HT2 | 150 °C, 1 h | – |
| HT3 | 150 °C, 6 h | – |
| HT4 | 150 °C, 12 h | – |
| WP | – | 25 °C, 1 h |
| Conditions | Yield (%) | Crystallinity (%) | Crystallite Size (nm) | Particle Length (nm) | Particle Width (nm) | Aspect Ratio |
|---|---|---|---|---|---|---|
| WP | 64.94 ± 2.40 | 30.06 ± 1.36 | 19.32 ± 2.36 | 38.28 ± 6.22 | 18.85 ± 3.59 | 2.12 ± 0.59 |
| HT1 | 53.48 ± 20.98 | 26.04 ± 0.34 | 22.45 ± 2.09 | 40.31 ± 6.90 | 24.80 ± 3.61 | 1.66 ± 0.37 |
| HT2 | 59.27 ± 2.95 | 36.36 ± 1.88 | 24.56 ± 2.09 | 50.61 ± 11.76 | 26.54 ± 6.15 | 1.95 ± 0.47 |
| HT3 | 46.63 ± 9.00 | 53.04 ± 2.32 | 29.49 ± 2.27 | 82.27 ± 30.16 | 28.41 ± 6.18 | 2.99 ± 1.21 |
| HT4 | 47.27 ± 13.13 | 54.12 ± 0.91 | 30.85 ± 1.50 | 108.75 ± 23.66 | 28.57 ± 6.28 | 3.98 ± 1.22 |
| Microhardness (GPa) | Fracture Toughness (MPa·m0.5) | Relative Density (%) | Grain Size (μm) | Crystalline Phase Composition (HA/β-TCP) | |
|---|---|---|---|---|---|
| WP | 5.26 ± 0.20 | 0.97 ± 0.08 | 93.98 ± 1.37 | 0.81 ± 0.03 | 64/36 |
| HT2 | 5.65 ± 0.66 | 1.23 ± 0.05 | 93.63 ± 0.69 | 0.85 ± 0.02 | 80/20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, S.-C.; Hsu, H.-C.; Wu, W.-H.; Ho, W.-F. Enhancing Bioactivity and Mechanical Properties of Nano-Hydroxyapatite Derived from Oyster Shells through Hydrothermal Synthesis. Nanomaterials 2024, 14, 1281. https://doi.org/10.3390/nano14151281
Wu S-C, Hsu H-C, Wu W-H, Ho W-F. Enhancing Bioactivity and Mechanical Properties of Nano-Hydroxyapatite Derived from Oyster Shells through Hydrothermal Synthesis. Nanomaterials. 2024; 14(15):1281. https://doi.org/10.3390/nano14151281
Chicago/Turabian StyleWu, Shih-Ching, Hsueh-Chuan Hsu, Wen-Hui Wu, and Wen-Fu Ho. 2024. "Enhancing Bioactivity and Mechanical Properties of Nano-Hydroxyapatite Derived from Oyster Shells through Hydrothermal Synthesis" Nanomaterials 14, no. 15: 1281. https://doi.org/10.3390/nano14151281






