Quantum Dot-Based Nanosensors for In Vitro Detection of Mycobacterium tuberculosis
Abstract
1. Introduction
2. Current Tuberculosis Diagnostic Methods
2.1. Molecular Diagnostic Tests
2.2. Tuberculosis Tests Based on T-Cell Analysis
2.3. Culture Methods
2.4. Skin Tests
2.5. Tests Based on Mycobacterium Staining
2.6. Other Methods
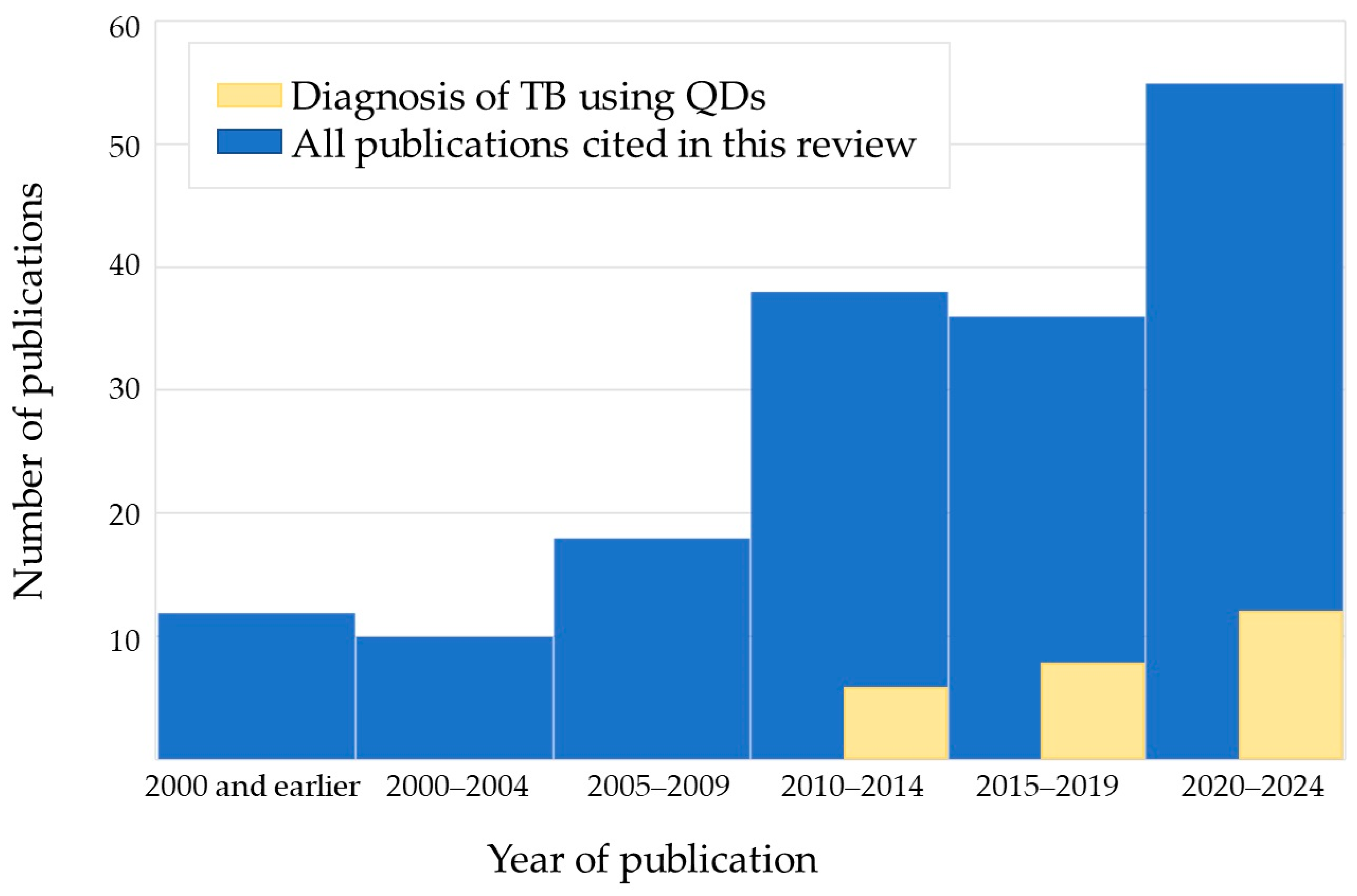
3. Quantum Dot-Based Nanosensors for M. tuberculosis Detection and Tuberculosis Diagnosis
4. Multiple Diagnostic Markers for M. tuberculosis Detection and Tuberculosis Diagnosis
5. Summary and Outlook
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Available online: https://www.who.int/data/gho/data/themes/topics/sdg-target-3_3-communicable-diseases (accessed on 10 January 2023).
- World Health Organization. “Tuberculosis in Women”, World Health Organization, Fact Sheet October 2016. Available online: https://www.aidsdatahub.org/sites/default/files/resource/tb-and-women.pdf (accessed on 10 January 2023).
- Chakaya, J.; Khan, M.; Ntoumi, F.; Aklillu, E.; Fatima, R.; Mwaba, P.; Kapata, N.; Mfinanga, S.; Hasnain, S.E.; Katoto, P.D.M.C.; et al. Global Tuberculosis Report 2020–Reflections on the Global TB Burden, Treatment and Prevention Efforts. Int. J. Infect. Dis. 2021, 113, S7–S12. [Google Scholar] [CrossRef] [PubMed]
- Maddineni, M.; Panda, M. Pulmonary Tuberculosis in a Young Pregnant Female: Challenges in Diagnosis and Management. Infect. Dis. Obstet. Gynecol. 2008, 2008, 628985. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, Q.; Yang, X.; Wen, J.; Tang, D.; Qi, M.; He, J. Host Factors Associated with False Negative Results in an Interferon-γ Release Assay in Adults with Active Tuberculosis. Heliyon 2023, 9, e22900. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guidelines on the Management of Latent Tuberculosis Infection; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Yang, X.; Fan, S.; Ma, Y.; Chen, H.; Xu, J.-F.; Pi, J.; Wang, W.; Chen, G. Current Progress of Functional Nanobiosensors for Potential Tuberculosis Diagnosis: The Novel Way for TB Control? Front. Bioeng. Biotechnol. 2022, 10, 1036678. [Google Scholar] [CrossRef]
- Mukherjee, S.; Perveen, S.; Negi, A.; Sharma, R. Evolution of Tuberculosis Diagnostics: From Molecular Strategies to Nanodiagnostics. Tuberculosis 2023, 140, 102340. [Google Scholar] [CrossRef]
- Gupta, A.K.; Singh, A.; Singh, S. Diagnosis of Tuberculosis: Nanodiagnostics Approaches. In NanoBioMedicine; Saxena, S.K., Khurana, S.M.P., Eds.; Springer: Singapore, 2020; pp. 261–283. ISBN 978-981-329-897-2. [Google Scholar]
- Jin, T.; Fei, B.; Zhang, Y.; He, X. The Diagnostic Value of Polymerase Chain Reaction for Mycobacterium tuberculosis to Distinguish Intestinal Tuberculosis from Crohn’s Disease: A Meta-Analysis. Saudi J. Gastroenterol. 2017, 23, 3. [Google Scholar] [CrossRef]
- Steingart, K.R.; Schiller, I.; Horne, D.J.; Pai, M.; Boehme, C.C.; Dendukuri, N. Xpert MTB/RIF Assay for Pulmonary Tuberculosis and Rifampicin Resistance in Adults. Cochrane Database Syst. Rev. 2014, 2014, CD009593. [Google Scholar] [CrossRef]
- Ssengooba, W.; Katamba, A.; Sserubiri, J.; Semugenze, D.; Nyombi, A.; Byaruhanga, R.; Turyahabwe, S.; Joloba, M.L. Performance Evaluation of Truenat MTB and Truenat MTB-RIF DX Assays in Comparison to Gene XPERT MTB/RIF Ultra for the Diagnosis of Pulmonary Tuberculosis in Uganda. BMC Infect. Dis. 2024, 24, 190. [Google Scholar] [CrossRef]
- Bjerrum, S.; Schiller, I.; Dendukuri, N.; Kohli, M.; Nathavitharana, R.R.; Zwerling, A.A.; Denkinger, C.M.; Steingart, K.R.; Shah, M. Lateral Flow Urine Lipoarabinomannan Assay for Detecting Active Tuberculosis in People Living with HIV. Cochrane Database Syst. Rev. 2019, 10, CD011420. [Google Scholar] [CrossRef]
- Manga, S.; Perales, R.; Reaño, M.; D’Ambrosio, L.; Migliori, G.B.; Amicosante, M. Performance of a Lateral Flow Immunochromatography Test for the Rapid Diagnosis of Active Tuberculosis in a Large Multicentre Study in Areas with Different Clinical Settings and Tuberculosis Exposure Levels. J. Thorac. Dis. 2016, 8, 3307–3313. [Google Scholar] [CrossRef][Green Version]
- Chen, H.; Nakagawa, A.; Takamori, M.; Abe, S.; Ueno, D.; Horita, N.; Kato, S.; Seki, N. Diagnostic Accuracy of the Interferon-Gamma Release Assay in Acquired Immunodeficiency Syndrome Patients with Suspected Tuberculosis Infection: A Meta-Analysis. Infection 2022, 50, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Tortoli, E.; Mandler, F.; Tronci, M.; Penati, V.; Sbaraglia, G.; Costa, D.; Montini, G.; Predominato, M.; Riva, R.; Passerini Tosi, C.; et al. Multicenter Evaluation of Mycobacteria Growth Indicator Tube (MGIT) Compared with the BACTEC Radiometric Method, BBL Biphasic Growth Medium and Löwenstein—Jensen Medium. Clin. Microbiol. Infect. 1997, 3, 468–473. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cruciani, M.; Scarparo, C.; Malena, M.; Bosco, O.; Serpelloni, G.; Mengoli, C. Meta-Analysis of BACTEC MGIT 960 and BACTEC 460 TB, with or without Solid Media, for Detection of Mycobacteria. J. Clin. Microbiol. 2004, 42, 2321–2325. [Google Scholar] [CrossRef] [PubMed]
- Martinez, M.R.; Sardiñas, M.; Garcia, G.; Mederos, L.M.; Díaz, R. Evaluation of BacT/ALERT 3D System for Mycobacteria Isolates. J. Travel Res. 2014, 02, 59–64. [Google Scholar] [CrossRef]
- Rose, D.N.; Schechter, C.B.; Adler, J.J. Interpretation of the Tuberculin Skin Test. J. Gen. Intern. Med. 1995, 10, 635–642. [Google Scholar] [CrossRef]
- Abdelaziz, M.M.; Bakr, W.M.K.; Hussien, S.M.; Amine, A.E.K. Diagnosis of Pulmonary Tuberculosis Using Ziehl–Neelsen Stain or Cold Staining Techniques? J. Egypt. Public Health Assoc. 2016, 91, 39–43. [Google Scholar] [CrossRef]
- Cattamanchi, A.; Davis, J.L.; Worodria, W.; den Boon, S.; Yoo, S.; Matovu, J.; Kiidha, J.; Nankya, F.; Kyeyune, R.; Byanyima, P.; et al. Sensitivity and Specificity of Fluorescence Microscopy for Diagnosing Pulmonary Tuberculosis in a High HIV Prevalence Setting. Int. J. Tuberc. Lung Dis. 2009, 13, 1130–1136. [Google Scholar]
- Pinto, L.M.; Pai, M.; Dheda, K.; Schwartzman, K.; Menzies, D.; Steingart, K.R. Scoring Systems Using Chest Radiographic Features for the Diagnosis of Pulmonary Tuberculosis in Adults: A Systematic Review. Eur. Respir. J. 2013, 42, 480–494. [Google Scholar] [CrossRef]
- Wang, Y.; Xu, Q.; Xu, B.; Lin, Y.; Yang, X.; Tong, J.; Huang, C. Clinical Performance of Nucleotide MALDI-TOF-MS in the Rapid Diagnosis of Pulmonary Tuberculosis and Drug Resistance. Tuberculosis 2023, 143, 102411. [Google Scholar] [CrossRef]
- Metcalfe, J.; Bacchetti, P.; Esmail, A.; Reckers, A.; Aguilar, D.; Wen, A.; Huo, S.; Muyindike, W.R.; Hahn, J.A.; Dheda, K.; et al. Diagnostic Accuracy of a Liquid Chromatography-Tandem Mass Spectrometry Assay in Small Hair Samples for Rifampin-Resistant Tuberculosis Drug Concentrations in a Routine Care Setting. BMC Infect. Dis. 2021, 21, 99. [Google Scholar] [CrossRef]
- Nsubuga, G.; Kennedy, S.; Rani, Y.; Hafiz, Z.; Kim, S.; Ruhwald, M.; Alland, D.; Ellner, J.; Joloba, M.; Dorman, S.E.; et al. Diagnostic Accuracy of the NOVA Tuberculosis Total Antibody Rapid Test for Detection of Pulmonary Tuberculosis and Infection with Mycobacterium tuberculosis. J. Clin. Tuberc. Other Mycobact. Dis. 2023, 31, 100362. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Tewari, R.; Dhatwalia, S.K.; Yadav, R.; Behera, D.; Sethi, S. A Loop-Mediated Isothermal Amplification Assay for the Diagnosis of Pulmonary Tuberculosis. Lett. Appl. Microbiol. 2019, 68, 219–225. [Google Scholar] [CrossRef] [PubMed]
- WHO. The Use of Loop-Mediated Isothermal Amplification (TB-LAMP) for the Diagnosis of Pulmonary Tuberculosis: Policy Guidance; WHO Guidelines Approved by the Guidelines Review Committee; World Health Organization: Geneva, Switzerland, 2016; ISBN 978-92-4-151118-6. [Google Scholar]
- Horne, D.J.; Kohli, M.; Zifodya, J.S.; Schiller, I.; Dendukuri, N.; Tollefson, D.; Schumacher, S.G.; Ochodo, E.A.; Pai, M.; Steingart, K.R. Xpert MTB/RIF and Xpert MTB/RIF Ultra for Pulmonary Tuberculosis and Rifampicin Resistance in Adults. Cochrane Database Syst. Rev. 2019, 6, CD009593. [Google Scholar] [CrossRef] [PubMed]
- Aainouss, A.; Momen, G.; Belghiti, A.; Bennani, K.; Lamaammal, A.; Chetioui, F.; Messaoudi, M.; Blaghen, M.; Mouslim, J.; Khyatti, M.; et al. Performance of GeneXpert MTB/RIF in the Diagnosis of Extrapulmonary Tuberculosis in Morocco. Russ. J. Infect. Immun. 2021, 12, 78–84. [Google Scholar] [CrossRef]
- Ngangue, Y.R.; Mbuli, C.; Neh, A.; Nshom, E.; Koudjou, A.; Palmer, D.; Ndi, N.N.; Qin, Z.Z.; Creswell, J.; Mbassa, V.; et al. Diagnostic Accuracy of the Truenat MTB Plus Assay and Comparison with the Xpert MTB/RIF Assay to Detect Tuberculosis among Hospital Outpatients in Cameroon. J. Clin. Microbiol. 2022, 60, e00155-22. [Google Scholar] [CrossRef]
- Sevastyanova, E.V.; Smirnova, T.G.; Larionova, E.E.; Chernousova, L.N. Detection of mycobacteria by culture inoculation. Liquid media and automated systems. Bull. TsNIIT 2020, 4, 88–95. [Google Scholar] [CrossRef]
- Lee, H.S.; Park, K.U.; Park, J.O.; Chang, H.E.; Song, J.; Choe, G. Rapid, Sensitive, and Specific Detection of Mycobacterium tuberculosis Complex by Real-Time PCR on Paraffin-Embedded Human Tissues. J. Mol. Diagn. 2011, 13, 390–394. [Google Scholar] [CrossRef]
- Itani, L.Y.; Cherry, M.A.; Araj, G.F. Efficacy of BACTEC TB in the Rapid Confirmatory Diagnosis of Mycobacterial Infections. A Lebanese Tertiary Care Center Experience. J. Med. Liban. 2005, 53, 208–212. [Google Scholar]
- Campelo, T.A.; Cardoso De Sousa, P.R.; Nogueira, L.D.L.; Frota, C.C.; Zuquim Antas, P.R. Revisiting the Methods for Detecting Mycobacterium tuberculosis: What Has the New Millennium Brought Thus Far? Access Microbiol. 2021, 3, 000245. [Google Scholar] [CrossRef]
- Szewczyk, R.; Kowalski, K.; Janiszewska-Drobinska, B.; Druszczyńska, M. Rapid Method for Mycobacterium tuberculosis Identification Using Electrospray Ionization Tandem Mass Spectrometry Analysis of Mycolic Acids. Diagn. Microbiol. Infect. Dis. 2013, 76, 298–305. [Google Scholar] [CrossRef]
- El Khéchine, A.; Couderc, C.; Flaudrops, C.; Raoult, D.; Drancourt, M. Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry Identification of Mycobacteria in Routine Clinical Practice. PLoS ONE 2011, 6, e24720. [Google Scholar] [CrossRef] [PubMed]
- Bacanelli, G.; Araujo, F.R.; Verbisck, N.V. Improved MALDI-TOF MS Identification of Mycobacterium tuberculosis by Use of an Enhanced Cell Disruption Protocol. Microorganisms 2023, 11, 1692. [Google Scholar] [CrossRef]
- Thomas, S.N.; French, D.; Jannetto, P.J.; Rappold, B.A.; Clarke, W.A. Liquid Chromatography–Tandem Mass Spectrometry for Clinical Diagnostics. Nat. Rev. Methods Primers 2022, 2, 96. [Google Scholar] [CrossRef] [PubMed]
- Malo, A.; Kellermann, T.; Ignatius, E.H.; Dooley, K.E.; Dawson, R.; Joubert, A.; Norman, J.; Castel, S.; Wiesner, L. A Validated Liquid Chromatography Tandem Mass Spectrometry Assay for the Analysis of Pretomanid in Plasma Samples from Pulmonary Tuberculosis Patients. J. Pharm. Biomed. Anal. 2021, 195, 113885. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Li, S.; Zhao, W.; Deng, J.; Yan, Z.; Zhang, T.; Wen, S.A.; Guo, H.; Li, L.; Yuan, J.; et al. A Peptidomic Approach to Identify Novel Antigen Biomarkers for the Diagnosis of Tuberculosis. Infect. Drug Resist. 2022, 15, 4617–4626. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Song, B.; Jiang, H.; Yu, K.; Zhong, D. A Liquid Chromatography/Tandem Mass Spectrometry Method for the Simultaneous Quantification of Isoniazid and Ethambutol in Human Plasma. Rapid Commun. Mass Spectrom. 2005, 19, 2591–2596. [Google Scholar] [CrossRef]
- He, X.; Ma, N. An Overview of Recent Advances in Quantum Dots for Biomedical Applications. Colloids Surf. B Biointerfaces 2014, 124, 118–131. [Google Scholar] [CrossRef]
- Medintz, I.L.; Uyeda, H.T.; Goldman, E.R.; Mattoussi, H. Quantum Dot Bioconjugates for Imaging, Labelling and Sensing. Nat. Mater. 2005, 4, 435–446. [Google Scholar] [CrossRef]
- Brkić, S. Applicability of Quantum Dots in Biomedical Science. In Ionizing Radiation Effects and Applications; Djezzar, B., Ed.; InTech: London, UK, 2018; ISBN 978-953-51-3953-9. [Google Scholar]
- Samokhvalov, P.S.; Karaulov, A.V.; Nabiev, I.R. Controlling the photoluminescence lifetime of quantum dots by engineering the structure of their shells. Opt. Spectrosc. 2023, 131, 1262. [Google Scholar] [CrossRef]
- Bilan, R.; Nabiev, I.; Sukhanova, A. Quantum Dot-Based Nanotools for Bioimaging, Diagnostics, and Drug Delivery. ChemBioChem 2016, 17, 2103–2114. [Google Scholar] [CrossRef]
- Sukhanova, A.; Ramos-Gomes, F.; Chames, P.; Sokolov, P.; Baty, D.; Alves, F.; Nabiev, I. Multiphoton Deep-Tissue Imaging of Micrometastases and Disseminated Cancer Cells Using Conjugates of Quantum Dots and Single-Domain Antibodies. In Multiplexed Imaging; Zamir, E., Ed.; Methods in Molecular Biology; Springer: New York, NY, USA, 2021; Volume 2350, pp. 105–123. ISBN 978-1-07-161592-8. [Google Scholar]
- Sokolov, P.; Samokhvalov, P.; Sukhanova, A.; Nabiev, I. Biosensors Based on Inorganic Composite Fluorescent Hydrogels. Nanomaterials 2023, 13, 1748. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Zhou, G. Phase Transfer of Hydrophobic QDs for Water-Soluble and Biocompatible Nature through Silanization. Mater. Res. Bull. 2011, 46, 2367–2372. [Google Scholar] [CrossRef]
- Xue, J.; Li, H.; Liu, J.; Wang, Y.; Liu, Y.; Sun, D.; Wang, W.; Huang, L.; Tang, J. Facile Synthesis of Silver Sulfide Quantum Dots by One Pot Reverse Microemulsion under Ambient Temperature. Mater. Lett. 2019, 242, 143–146. [Google Scholar] [CrossRef]
- Chen, J.; Kong, Y.; Wang, W.; Fang, H.; Wo, Y.; Zhou, D.; Wu, Z.; Li, Y.; Chen, S. Direct Water-Phase Synthesis of Lead Sulfide Quantum Dots Encapsulated by β-Lactoglobulin for In Vivo Second Near Infrared Window Imaging with Reduced Toxicity. Chem. Commun. 2016, 52, 4025–4028. [Google Scholar] [CrossRef]
- Bel Haj Mohamed, N.; Ben Brahim, N.; Mrad, R.; Haouari, M.; Ben Chaâbane, R.; Negrerie, M. Use of MPA-Capped CdS Quantum Dots for Sensitive Detection and Quantification of Co2+ Ions in Aqueous Solution. Anal. Chim. Acta 2018, 1028, 50–58. [Google Scholar] [CrossRef]
- de Lana Junior, M.L.; Cardoso, T.R.; Souza, P.D.C.; de Carvalho dos Anjos, V.; Bell, M.J.V.; Cury, L.A.; da Silva Subtil, A.G.; Brandao, M.P. Investigations on the Interaction of Water-Soluble Semiconductor Polymer with Thioglycolic Acid (TGA) Capped CdTe Quantum Dots. Opt. Mater. 2019, 93, 70–75. [Google Scholar] [CrossRef]
- Guo, Z.; Liu, Z.-G.; Yao, X.-Z.; Zhang, K.-S.; Chen, X.; Liu, J.-H.; Huang, X.-J. A Molecular-Gap Device for Specific Determination of Mercury Ions. Sci. Rep. 2013, 3, 3115. [Google Scholar] [CrossRef]
- Ramírez-Herrera, D.E.; Reyes-Cruzaley, A.P.; Dominguez, G.; Paraguay-Delgado, F.; Tirado-Guízar, A.; Pina-Luis, G. CdTe Quantum Dots Modified with Cysteamine: A New Efficient Nanosensor for the Determination of Folic Acid. Sensors 2019, 19, 4548. [Google Scholar] [CrossRef]
- Liu, P.; Wang, Q.; Li, X. Studies on CdSe/l-Cysteine Quantum Dots Synthesized in Aqueous Solution for Biological Labeling. J. Phys. Chem. C 2009, 113, 7670–7676. [Google Scholar] [CrossRef]
- Sokolov, P.; Nifontova, G.; Samokhvalov, P.; Karaulov, A.; Sukhanova, A.; Nabiev, I. Nontoxic Fluorescent Nanoprobes for Multiplexed Detection and 3D Imaging of Tumor Markers in Breast Cancer. Pharmaceutics 2023, 15, 946. [Google Scholar] [CrossRef]
- Sokolov, P.; Evsegneeva, I.; Karaulov, A.; Sukhanova, A.; Nabiev, I. Allergen Microarrays and New Physical Approaches to More Sensitive and Specific Detection of Allergen-Specific Antibodies. Biosensors 2024, 14, 353. [Google Scholar] [CrossRef] [PubMed]
- Brazhnik, K.; Nabiev, I.; Sukhanova, A. Advanced Procedure for Oriented Conjugation of Full-Size Antibodies with Quantum Dots. In Quantum Dots: Applications in Biology; Fontes, A., Santos, B.S., Eds.; Methods in Molecular Biology; Springer: New York, NY, USA, 2014; Volume 1199, pp. 55–66. ISBN 978-1-4939-1279-7. [Google Scholar]
- Sukhanova, A.; Even-Desrumeaux, K.; Kisserli, A.; Tabary, T.; Reveil, B.; Millot, J.-M.; Chames, P.; Baty, D.; Artemyev, M.; Oleinikov, V.; et al. Oriented Conjugates of Single-Domain Antibodies and Quantum Dots: Toward a New Generation of Ultrasmall Diagnostic Nanoprobes. Nanomed. Nanotechnol. Biol. Med. 2012, 8, 516–525. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Yoo, S. Aptamer-Conjugated Quantum Dot Optical Biosensors: Strategies and Applications. Chemosensors 2021, 9, 318. [Google Scholar] [CrossRef]
- Song, F.; Chan, W.C.W. Principles of Conjugating Quantum Dots to Proteins via Carbodiimide Chemistry. Nanotechnology 2011, 22, 494006. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-H.; Li, Y.-Q.; Zhang, H.-L.; Wang, H.-Q.; Lin, S.; Chen, J.; Zhao, Y.-D.; Luo, Q.-M. Bioconjugation of Concanavalin and CdTe Quantum Dots and the Detection of Glucose. Colloids Surf. A Physicochem. Eng. Asp. 2010, 364, 82–86. [Google Scholar] [CrossRef]
- Liu, J.L.; Walper, S.A.; Turner, K.B.; Lee, A.B.; Medintz, I.L.; Susumu, K.; Oh, E.; Zabetakis, D.; Goldman, E.R.; Anderson, G.P. Conjugation of Biotin-Coated Luminescent Quantum Dots with Single Domain Antibody-Rhizavidin Fusions. Biotechnol. Rep. 2016, 10, 56–65. [Google Scholar] [CrossRef]
- Zhang, T.; Tang, H.; Zhou, S.; Ding, S.; Xiao, X.; Wen, Z.; Niu, G.; Luo, X.; Wang, F.; Sun, X.W.; et al. Factors Influencing the Working Temperature of Quantum Dot Light-Emitting Diodes. Opt. Express 2020, 28, 34167–34179. [Google Scholar] [CrossRef]
- Sokolov, P.M.; Zvaigzne, M.A.; Krivenkov, V.A.; Litvin, A.P.; Baranov, A.V.; Fedorov, A.V.; Samokhvalov, P.S.; Nabiev, I.R. Graphene−Quantum Dot Hybrid Nanostructures with Controlled Optical and Photoelectric Properties for Solar Cell Applications. Russ. Chem. Rev. 2019, 88, 370. [Google Scholar] [CrossRef]
- Chen, G.-H.; Lin, C.-T.; Chen, P.-H.; Jang, T.-W.; Chen, H.-S. General Strategies for Preparing Hybrid Polymer/Quantum Dot Nanocomposites for Color Conversion. Nanomaterials 2023, 13, 3072. [Google Scholar] [CrossRef]
- Wang, S.; Qin, A.; Chau, L.Y.; Fok, E.W.T.; Choy, M.Y.; Brackman, C.J.; Siu, G.K.H.; Huang, C.-L.; Yip, S.P.; Lee, T.M.H. Amine-Functionalized Quantum Dots as a Universal Fluorescent Nanoprobe for a One-Step Loop-Mediated Isothermal Amplification Assay with Single-Copy Sensitivity. ACS Appl. Mater. Interfaces 2022, 14, 35299–35308. [Google Scholar] [CrossRef]
- Hafian, H.; Sukhanova, A.; Turini, M.; Chames, P.; Baty, D.; Pluot, M.; Cohen, J.H.M.; Nabiev, I.; Millot, J.-M. Multiphoton Imaging of Tumor Biomarkers with Conjugates of Single-Domain Antibodies and Quantum Dots. Nanomed. Nanotechnol. Biol. Med. 2014, 10, 1701–1709. [Google Scholar] [CrossRef] [PubMed]
- Bilan, R.; Fleury, F.; Nabiev, I.; Sukhanova, A. Quantum Dot Surface Chemistry and Functionalization for Cell Targeting and Imaging. Bioconjugate Chem. 2015, 26, 609–624. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Youn, Y.H.; Kwon, I.K.; Ko, N.R. Recent Advances in Quantum Dots for Biomedical Applications. J. Pharm. Investig. 2018, 48, 209–214. [Google Scholar] [CrossRef]
- Han, X.; Xu, K.; Taratula, O.; Farsad, K. Applications of Nanoparticles in Biomedical Imaging. Nanoscale 2019, 11, 799–819. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Cai, N.; Chan, V. Recent Advances in Silicon Quantum Dot-Based Fluorescent Biosensors. Biosensors 2023, 13, 311. [Google Scholar] [CrossRef]
- Brazhnik, K.; Nabiev, I.; Sukhanova, A. Oriented Conjugation of Single-Domain Antibodies and Quantum Dots. In Quantum Dots: Applications in Biology; Fontes, A., Santos, B.S., Eds.; Methods in Molecular Biology; Springer: New York, NY, USA, 2014; Volume 1199, pp. 129–140. ISBN 978-1-4939-1279-7. [Google Scholar]
- Biju, V. Chemical Modifications and Bioconjugate Reactions of Nanomaterials for Sensing, Imaging, Drug Delivery and Therapy. Chem. Soc. Rev. 2014, 43, 744–764. [Google Scholar] [CrossRef]
- Bilan, R.S.; Krivenkov, V.A.; Berestovoy, M.A.; Efimov, A.E.; Agapov, I.I.; Samokhvalov, P.S.; Nabiev, I.; Sukhanova, A. Engineering of Optically Encoded Microbeads with FRET-Free Spatially Separated Quantum-Dot Layers for Multiplexed Assays. ChemPhysChem 2017, 18, 970–979. [Google Scholar] [CrossRef]
- Rousserie, G.; Sukhanova, A.; Even-Desrumeaux, K.; Fleury, F.; Chames, P.; Baty, D.; Oleinikov, V.; Pluot, M.; Cohen, J.H.M.; Nabiev, I. Semiconductor Quantum Dots for Multiplexed Bio-Detection on Solid-State Microarrays. Crit. Rev. Oncol./Hematol. 2010, 74, 1–15. [Google Scholar] [CrossRef]
- Ding, C.; Zhu, A.; Tian, Y. Functional Surface Engineering of C-Dots for Fluorescent Biosensing and in Vivo Bioimaging. Acc. Chem. Res. 2014, 47, 20–30. [Google Scholar] [CrossRef]
- Sarkar, L.H.; Kumari, S. Nanocarriers for Mycobacterium tuberculosis. J. Sci. Res. 2021, 65, 33–37. [Google Scholar] [CrossRef]
- El-Shabasy, R.M.; Zahran, M.; Ibrahim, A.H.; Maghraby, Y.R.; Nayel, M. Advances in the Fabrication of Potential Nanomaterials for Diagnosis and Effective Treatment of Tuberculosis. Mater. Adv. 2024, 5, 1772–1782. [Google Scholar] [CrossRef]
- Ahmad, F.; Pandey, N.; Singh, K.; Ahmad, S.; Khubaib, M.; Sharma, R. Recent Advances in Nanocarrier Based Therapeutic and Diagnostic Approaches in Tuberculosis. Precis. Nanomed. 2023, 6, 1134–1156. [Google Scholar] [CrossRef]
- Pati, R.; Sahu, R.; Panda, J.; Sonawane, A. Encapsulation of Zinc-Rifampicin Complex into Transferrin-Conjugated Silver Quantum-Dots Improves Its Antimycobacterial Activity and Stability and Facilitates Drug Delivery into Macrophages. Sci. Rep. 2016, 6, 24184. [Google Scholar] [CrossRef] [PubMed]
- Gliddon, H.D.; Howes, P.D.; Kaforou, M.; Levin, M.; Stevens, M.M. A Nucleic Acid Strand Displacement System for the Multiplexed Detection of Tuberculosis-Specific mRNA Using Quantum Dots. Nanoscale 2016, 8, 10087–10095. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Li, J.; Shi, S.; Yan, Y.; Zhang, M.; Wang, P.; Zeng, G.; Jiang, Z. Detection of Interferon-Gamma for Latent Tuberculosis Diagnosis Using an Immunosensor Based on CdS Quantum Dots Coupled to Magnetic Beads as Labels. Int. J. Electrochem. Sci. 2015, 10, 2580–2593. [Google Scholar] [CrossRef]
- Januarie, K.C.; Oranzie, M.; Feleni, U.; Iwuoha, E. Quantum Dot Amplified Impedimetric Aptasensor for Interferon-Gamma. Electrochim. Acta 2023, 463, 142825. [Google Scholar] [CrossRef]
- Zhou, B.; Zhu, M.; Hao, Y.; Yang, P. Potential-Resolved Electrochemiluminescence for Simultaneous Determination of Triple Latent Tuberculosis Infection Markers. ACS Appl. Mater. Interfaces 2017, 9, 30536–30542. [Google Scholar] [CrossRef]
- Hu, O.; Li, Z.; Wu, J.; Tan, Y.; Chen, Z.; Tong, Y. A Multicomponent Nucleic Acid Enzyme-Cleavable Quantum Dot Nanobeacon for Highly Sensitive Diagnosis of Tuberculosis with the Naked Eye. ACS Sens. 2023, 8, 254–262. [Google Scholar] [CrossRef]
- Kabwe, K.P.; Nsibande, S.A.; Pilcher, L.A.; Forbes, P.B.C. Development of a Mycolic Acid-graphene Quantum Dot Probe as a Potential Tuberculosis Biosensor. Luminescence 2022, 37, 1881–1890. [Google Scholar] [CrossRef]
- Kabwe, K.P.; Nsibande, S.A.; Lemmer, Y.; Pilcher, L.A.; Forbes, P.B.C. Synthesis and Characterisation of Quantum Dots Coupled to Mycolic Acids as a Water-soluble Fluorescent Probe for Potential Lateral Flow Detection of Antibodies and Diagnosis of Tuberculosis. Luminescence 2022, 37, 278–289. [Google Scholar] [CrossRef]
- Zou, F.; Zhou, H.; Tan, T.V.; Kim, J.; Koh, K.; Lee, J. Dual-Mode SERS-Fluorescence Immunoassay Using Graphene Quantum Dot Labeling on One-Dimensional Aligned Magnetoplasmonic Nanoparticles. ACS Appl. Mater. Interfaces 2015, 7, 12168–12175. [Google Scholar] [CrossRef]
- Hu, O.; Li, Z.; He, Q.; Tong, Y.; Tan, Y.; Chen, Z. Fluorescence Biosensor for One-Step Simultaneous Detection of Mycobacterium tuberculosis Multidrug-Resistant Genes Using nanoCoTPyP and Double Quantum Dots. Anal. Chem. 2022, 94, 7918–7927. [Google Scholar] [CrossRef] [PubMed]
- Shi, T.; Jiang, P.; Peng, W.; Meng, Y.; Ying, B.; Chen, P. Nucleic Acid and Nanomaterial Synergistic Amplification Enables Dual Targets of Ultrasensitive Fluorescence Quantification to Improve the Efficacy of Clinical Tuberculosis Diagnosis. ACS Appl. Mater. Interfaces 2024, 16, 14510–14519. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Qin, L.; Wang, Y.; Zhang, B.; Liu, Z.; Ma, H.; Lu, J.; Huang, X.; Shi, D.; Hu, Z. Detection of Mycobacterium tuberculosis Based on H37Rv Binding Peptides Using Surface Functionalized Magnetic Microspheres Coupled with Quantum Dots – a Nano Detection Method for Mycobacterium tuberculosis. Int. J. Nanomed. 2014, 10, 77–88. [Google Scholar] [CrossRef]
- Ma, H.; Hu, Z.; Wang, Y.; Qing, L.; Chen, H.; Lu, J.; Yang, H. [Methodology research and preliminary assessment of Mycobacterium tuberculosis detection by immunomagnetic beads combined with functionalized fluorescent quantum dots]. Zhonghua Jie He He Hu Xi Za Zhi 2013, 36, 100–105. [Google Scholar] [PubMed]
- Shojaei, T.R.; Mohd Salleh, M.A.; Tabatabaei, M.; Ekrami, A.; Motallebi, R.; Rahmani-Cherati, T.; Hajalilou, A.; Jorfi, R. Development of Sandwich-Form Biosensor to Detect Mycobacterium tuberculosis Complex in Clinical Sputum Specimens. Braz. J. Infect. Dis. 2014, 18, 600–608. [Google Scholar] [CrossRef]
- Liang, L.; Chen, M.; Tong, Y.; Tan, W.; Chen, Z. Detection of Mycobacterium tuberculosis IS6110 Gene Fragment by Fluorescent Biosensor Based on FRET between Two-Dimensional Metal-Organic Framework and Quantum Dots-Labeled DNA Probe. Anal. Chim. Acta 2021, 1186, 339090. [Google Scholar] [CrossRef]
- Kim, E.J.; Kim, E.B.; Lee, S.W.; Cheon, S.A.; Kim, H.-J.; Lee, J.; Lee, M.-K.; Ko, S.; Park, T.J. An Easy and Sensitive Sandwich Assay for Detection of Mycobacterium tuberculosis Ag85B Antigen Using Quantum Dots and Gold Nanorods. Biosens. Bioelectron. 2017, 87, 150–156. [Google Scholar] [CrossRef]
- Huang, Z.; Huang, H.; Hu, J.; Xia, L.; Liu, X.; Qu, R.; Huang, X.; Yang, Y.; Wu, K.; Ma, R.; et al. A Novel Quantitative Urine LAM Antigen Strip for Point-of-Care Tuberculosis Diagnosis in Non-HIV Adults. J. Infect. 2024, 88, 194–198. [Google Scholar] [CrossRef]
- Tufa, L.T.; Oh, S.; Tran, V.T.; Kim, J.; Jeong, K.-J.; Park, T.J.; Kim, H.-J.; Lee, J. Electrochemical Immunosensor Using Nanotriplex of Graphene Quantum Dots, Fe3O4, and Ag Nanoparticles for Tuberculosis. Electrochim. Acta 2018, 290, 369–377. [Google Scholar] [CrossRef]
- Bhattacharyya, D.; Sarswat, P.K.; Free, M.L. Quantum Dots and Carbon Dots Based Fluorescent Sensors for TB Biomarkers Detection. Vacuum 2017, 146, 606–613. [Google Scholar] [CrossRef]
- He, Q.; Cai, S.; Wu, J.; Hu, O.; Liang, L.; Chen, Z. Determination of Tuberculosis-Related Volatile Organic Biomarker Methyl Nicotinate in Vapor Using Fluorescent Assay Based on Quantum Dots and Cobalt-Containing Porphyrin Nanosheets. Microchim. Acta 2022, 189, 108. [Google Scholar] [CrossRef] [PubMed]
- Gazouli, M.; Liandris, E.; Andreadou, M.; Sechi, L.A.; Masala, S.; Paccagnini, D.; Ikonomopoulos, J. Specific Detection of Unamplified Mycobacterial DNA by Use of Fluorescent Semiconductor Quantum Dots and Magnetic Beads. J. Clin. Microbiol. 2010, 48, 2830–2835. [Google Scholar] [CrossRef] [PubMed]
- Cimaglia, F.; Aliverti, A.; Chiesa, M.; Poltronieri, P.; De Lorenzis, E.; Santino, A.; Sechi, L.A. Quantum Dots Nanoparticle-Based Lateral Flow Assay for Rapid Detection of Mycobacterium Species Using Anti-FprA Antibodies. Nanotechnol. Dev. 2012, 2, 5. [Google Scholar] [CrossRef]
- Jiang, X.; Zeng, H.; Duan, C.; Hu, Q.; Wu, Q.; Yu, Y.; Yang, X. One-Pot Synthesis of Stable and Functional Hydrophilic CsPbBr3 Perovskite Quantum Dots for “Turn-on” Fluorescence Detection of Mycobacterium tuberculosis. Dalton Trans. 2022, 51, 3581–3589. [Google Scholar] [CrossRef]
- Mohd Bakhori, N.; Yusof, N.A.; Abdullah, J.; Wasoh, H.; Ab Rahman, S.K.; Abd Rahman, S.F. Surface Enhanced CdSe/ZnS QD/SiNP Electrochemical Immunosensor for the Detection of Mycobacterium tuberculosis by Combination of CFP10-ESAT6 for Better Diagnostic Specificity. Materials 2019, 13, 149. [Google Scholar] [CrossRef]
- Gliddon, H.D.; Kaforou, M.; Alikian, M.; Habgood-Coote, D.; Zhou, C.; Oni, T.; Anderson, S.T.; Brent, A.J.; Crampin, A.C.; Eley, B.; et al. Identification of Reduced Host Transcriptomic Signatures for Tuberculosis Disease and Digital PCR-Based Validation and Quantification. Front. Immunol. 2021, 12, 637164. [Google Scholar] [CrossRef]
- Boyle, D.S.; McNerney, R.; Teng Low, H.; Leader, B.T.; Pérez-Osorio, A.C.; Meyer, J.C.; O’Sullivan, D.M.; Brooks, D.G.; Piepenburg, O.; Forrest, M.S. Rapid Detection of Mycobacterium tuberculosis by Recombinase Polymerase Amplification. PLoS ONE 2014, 9, e103091. [Google Scholar] [CrossRef]
- Verma, S.; Dubey, A.; Singh, P.; Tewerson, S.; Sharma, D. Adenosine Deaminase (ADA) Level in Tubercular Pleural Effusion. Lung India 2008, 25, 109. [Google Scholar] [CrossRef]
- DeVito, J.A.; Morris, S. Exploring the Structure and Function of the Mycobacterial KatG Protein Using Trans-Dominant Mutants. Antimicrob. Agents Chemother. 2003, 47, 188–195. [Google Scholar] [CrossRef]
- Clifford, V.; Tebruegge, M.; Zufferey, C.; Germano, S.; Forbes, B.; Cosentino, L.; Matchett, E.; McBryde, E.; Eisen, D.; Robins-Browne, R.; et al. Cytokine Biomarkers for the Diagnosis of Tuberculosis Infection and Disease in Adults in a Low Prevalence Setting. Tuberculosis 2019, 114, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Hao, Y.; Chen, S.; Yang, P. A Quartz Crystal Microbalance Modified with Antibody-Coated Silver Nanoparticles Acting as Mass Signal Amplifiers for Real-Time Monitoring of Three Latent Tuberculosis Infection Biomarkers. Microchim. Acta 2019, 186, 212. [Google Scholar] [CrossRef] [PubMed]
- Parate, K.; Rangnekar, S.V.; Jing, D.; Mendivelso-Perez, D.L.; Ding, S.; Secor, E.B.; Smith, E.A.; Hostetter, J.M.; Hersam, M.C.; Claussen, J.C. Aerosol-Jet-Printed Graphene Immunosensor for Label-Free Cytokine Monitoring in Serum. ACS Appl. Mater. Interfaces 2020, 12, 8592–8603. [Google Scholar] [CrossRef] [PubMed]
- Renshaw, P.S.; Panagiotidou, P.; Whelan, A.; Gordon, S.V.; Hewinson, R.G.; Williamson, R.A.; Carr, M.D. Conclusive Evidence That the Major T-Cell Antigens of theMycobacterium tuberculosis Complex ESAT-6 and CFP-10 Form a Tight, 1:1 Complex and Characterization of the Structural Properties of ESAT-6, CFP-10, and the ESAT-6·CFP-10 Complex. J. Biol. Chem. 2002, 277, 21598–21603. [Google Scholar] [CrossRef] [PubMed]
- Welin, A.; Björnsdottir, H.; Winther, M.; Christenson, K.; Oprea, T.; Karlsson, A.; Forsman, H.; Dahlgren, C.; Bylund, J. CFP-10 from Mycobacterium tuberculosis Selectively Activates Human Neutrophils through a Pertussis Toxin-Sensitive Chemotactic Receptor. Infect. Immun. 2015, 83, 205–213. [Google Scholar] [CrossRef]
- Chai, Q.; Wang, X.; Qiang, L.; Zhang, Y.; Ge, P.; Lu, Z.; Zhong, Y.; Li, B.; Wang, J.; Zhang, L.; et al. A Mycobacterium tuberculosis Surface Protein Recruits Ubiquitin to Trigger Host Xenophagy. Nat. Commun. 2019, 10, 1973. [Google Scholar] [CrossRef]
- P, M.; Ahmad, J.; Samal, J.; Sheikh, J.A.; Arora, S.K.; Khubaib, M.; Aggarwal, H.; Kumari, I.; Luthra, K.; Rahman, S.A.; et al. Mycobacterium tuberculosis Specific Protein Rv1509 Evokes Efficient Innate and Adaptive Immune Response Indicative of Protective Th1 Immune Signature. Front. Immunol. 2021, 12, 706081. [Google Scholar] [CrossRef]
- Lakshmipriya, T.; Gopinath, S.C.B.; Tang, T.-H. Biotin-Streptavidin Competition Mediates Sensitive Detection of Biomolecules in Enzyme Linked Immunosorbent Assay. PLoS ONE 2016, 11, e0151153. [Google Scholar] [CrossRef]
- Omar, R.A.; Verma, N.; Arora, P.K. Development of ESAT-6 Based Immunosensor for the Detection of Mycobacterium tuberculosis. Front. Immunol. 2021, 12, 653853. [Google Scholar] [CrossRef]
- Diouani, M.F.; Ouerghi, O.; Refai, A.; Belgacem, K.; Tlili, C.; Laouini, D.; Essafi, M. Detection of ESAT-6 by a Label Free Miniature Immuno-Electrochemical Biosensor as a Diagnostic Tool for Tuberculosis. Mater. Sci. Eng. C 2017, 74, 465–470. [Google Scholar] [CrossRef]
- Arora, J.; Kumar, G.; Verma, A.; Bhalla, M.; Sarin, R.; Myneedu, V. Utility of MPT64 Antigen Detection for Rapid Confirmation of Mycobacterium tuberculosis Complex. J. Glob. Infect. Dis. 2015, 7, 66. [Google Scholar] [CrossRef] [PubMed]
- Saengdee, P.; Chaisriratanakul, W.; Bunjongpru, W.; Sripumkhai, W.; Srisuwan, A.; Hruanun, C.; Poyai, A.; Phunpae, P.; Pata, S.; Jeamsaksiri, W.; et al. A Silicon Nitride ISFET Based Immunosensor for Ag85B Detection of Tuberculosis. Analyst 2016, 141, 5767–5775. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.-N.; Chen, J.-P.; Chen, D.-L. Serodiagnosis Efficacy and Immunogenicity of the Fusion Protein of Mycobacterium tuberculosis Composed of the 10-Kilodalton Culture Filtrate Protein, ESAT-6, and the Extracellular Domain Fragment of PPE68. Clin. Vaccine Immunol. 2012, 19, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Boshoff, H.I.M.; Harrison, J.R.; Ray, P.C.; Green, S.R.; Wyatt, P.G.; Barry, C.E. PE/PPE Proteins Mediate Nutrient Transport across the Outer Membrane of Mycobacterium tuberculosis. Science 2020, 367, 1147–1151. [Google Scholar] [CrossRef]
- García, J.; Puentes, A.; Rodríguez, L.; Ocampo, M.; Curtidor, H.; Vera, R.; Lopez, R.; Valbuena, J.; Cortes, J.; Vanegas, M.; et al. Mycobacterium tuberculosis Rv2536 Protein Implicated in Specific Binding to Human Cell Lines. Protein Sci. 2005, 14, 2236–2245. [Google Scholar] [CrossRef]
- Shirshikov, F.V.; Bespyatykh, J.A. TB-ISATEST: A Diagnostic LAMP Assay for Differentiation of Mycobacterium tuberculosis. Russ. J. Bioorganic Chem. 2023, 49, 1279–1292. [Google Scholar] [CrossRef]
- Jackett, P.S.; Bothamley, G.H.; Batra, H.V.; Mistry, A.; Young, D.B.; Ivanyi, J. Specificity of Antibodies to Immunodominant Mycobacterial Antigens in Pulmonary Tuberculosis. J. Clin. Microbiol. 1988, 26, 2313–2318. [Google Scholar] [CrossRef]
- Verbon, A.; Hartskeerl, R.A.; Moreno, C.; Kolk, A.H.J. Characterization of B Cell Epitopes on the 16K Antigen of Mycobacterium tuberculosis. Clin. Exp. Immunol. 2008, 89, 395–401. [Google Scholar] [CrossRef]
- Salata, R.A.; Sanson, A.J.; Malhotra, I.J.; Wiker, H.G.; Harboe, M.; Phillips, N.B.; Daniel, T.M. Purification and Characterization of the 30,000 Dalton Native Antigen of Mycobacterium tuberculosis and Characterization of Six Monoclonal Antibodies Reactive with a Major Epitope of This Antigen. J. Lab. Clin. Med. 1991, 118, 589–598. [Google Scholar]
- Andersen, A.B.; Hansen, E.B. Structure and Mapping of Antigenic Domains of Protein Antigen b, a 38,000-Molecular-Weight Protein of Mycobacterium tuberculosis. Infect. Immun. 1989, 57, 2481–2488. [Google Scholar] [CrossRef]
- Attallah, A.M.; Osman, S.; Saad, A.; Omran, M.; Ismail, H.; Ibrahim, G.; Abo-Naglla, A. Application of a Circulating Antigen Detection Immunoassay for Laboratory Diagnosis of Extra-Pulmonary and Pulmonary Tuberculosis. Clin. Chim. Acta 2005, 356, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Hunter, S.W.; Gaylord, H.; Brennan, P.J. Structure and Antigenicity of the Phosphorylated Lipopolysaccharide Antigens from the Leprosy and Tubercle Bacilli. J. Biol. Chem. 1986, 261, 12345–12351. [Google Scholar] [CrossRef] [PubMed]
- Cocito, C.; Vanlinden, F. Preparation and Properties of Antigen 60 from Mycobacterium Bovis BCG. Clin. Exp. Immunol. 1986, 66, 262–272. [Google Scholar] [PubMed]
- Hendrickson, R.C.; Douglass, J.F.; Reynolds, L.D.; McNeill, P.D.; Carter, D.; Reed, S.G.; Houghton, R.L. Mass Spectrometric Identification of Mtb81, a Novel Serological Marker for Tuberculosis. J. Clin. Microbiol. 2000, 38, 2354–2361. [Google Scholar] [CrossRef] [PubMed]
- Arend, S.M.; Ottenhoff, T.H.; Andersen, P.; van Dissel, J.T. Uncommon Presentations of Tuberculosis: The Potential Value of a Novel Diagnostic Assay Based on the Mycobacterium tuberculosis-Specific Antigens ESAT-6 and CFP-10. Int. J. Tuberc. Lung Dis. 2001, 5, 680–686. [Google Scholar]
- Wilkinson, S.T.; Vanpatten, K.A.; Fernandez, D.R.; Brunhoeber, P.; Garsha, K.E.; Glinsmann-Gibson, B.J.; Grogan, T.M.; Teruya-Feldstein, J.; Rimsza, L.M. Partial Plasma Cell Differentiation as a Mechanism of Lost Major Histocompatibility Complex Class II Expression in Diffuse Large B-Cell Lymphoma. Blood 2012, 119, 1459–1467. [Google Scholar] [CrossRef]
- Dewan, P.K.; Grinsdale, J.; Kawamura, L.M. Low Sensitivity of a Whole-Blood Interferon-Gamma Release Assay for Detection of Active Tuberculosis. Clin. Infect. Dis. 2007, 44, 69–73. [Google Scholar] [CrossRef]
- Wang, X.; Jiang, J.; Cao, Z.; Yang, B.; Zhang, J.; Cheng, X. Diagnostic Performance of Multiplex Cytokine and Chemokine Assay for Tuberculosis. Tuberculosis 2012, 92, 513–520. [Google Scholar] [CrossRef]
- La Manna, M.P.; Orlando, V.; Li Donni, P.; Sireci, G.; Di Carlo, P.; Cascio, A.; Dieli, F.; Caccamo, N. Identification of Plasma Biomarkers for Discrimination between Tuberculosis Infection/Disease and Pulmonary Non Tuberculosis Disease. PLoS ONE 2018, 13, e0192664. [Google Scholar] [CrossRef]
- Bilan, R.; Ametzazurra, A.; Brazhnik, K.; Escorza, S.; Fernández, D.; Uríbarri, M.; Nabiev, I.; Sukhanova, A. Quantum-Dot-Based Suspension Microarray for Multiplex Detection of Lung Cancer Markers: Preclinical Validation and Comparison with the Luminex xMAP® System. Sci. Rep. 2017, 7, 44668. [Google Scholar] [CrossRef]
- Mutavdžić, D.; Xu, J.; Thakur, G.; Triulzi, R.; Kasas, S.; Jeremić, M.; Leblanc, R.; Radotić, K. Determination of the Size of Quantum Dots by Fluorescence Spectroscopy. Analyst 2011, 136, 2391–2396. [Google Scholar] [CrossRef] [PubMed]
- Bagga, A.; Chattopadhyay, P.K.; Ghosh, S. Stokes Shift in Quantum Dots: Origin of Dark Exciton. In Proceedings of the 2007 International Workshop on Physics of Semiconductor Devices, Mumbai, India, 16–20 December 2007; pp. 876–879. [Google Scholar]
- Moule, M.G.; Cirillo, J.D. Mycobacterium tuberculosis Dissemination Plays a Critical Role in Pathogenesis. Front. Cell. Infect. Microbiol. 2020, 10, 65. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Consolidated Guidelines on Tuberculosis: Module 1: Prevention: Tuberculosis Preventive Treatment; World Health Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-000150-3. [Google Scholar]
- Hamada, Y.; Cirillo, D.M.; Matteelli, A.; Penn-Nicholson, A.; Rangaka, M.X.; Ruhwald, M. Tests for Tuberculosis Infection: Landscape Analysis. Eur. Respir. J. 2021, 58, 2100167. [Google Scholar] [CrossRef] [PubMed]
- Pai, M.; Denkinger, C.M.; Kik, S.V.; Rangaka, M.X.; Zwerling, A.; Oxlade, O.; Metcalfe, J.Z.; Cattamanchi, A.; Dowdy, D.W.; Dheda, K.; et al. Gamma Interferon Release Assays for Detection of Mycobacterium tuberculosis Infection. Clin. Microbiol. Rev. 2014, 27, 3–20. [Google Scholar] [CrossRef]
- Talbot, E.A.; Maro, I.; Ferguson, K.; Adams, L.V.; Mtei, L.; Matee, M.; Von Reyn, C.F. Maintenance of Sensitivity of the T-SPOT. TB Assay after Overnight Storage of Blood Samples, Dar Es Salaam, Tanzania. Tuberc. Res. Treat. 2012, 2012, 345290. [Google Scholar] [CrossRef][Green Version]
- Wang, S.-H.; Rajaram, M.V.S.; Trollip, A.; Wu, Q.; Ayala, D.; Garza, D.; Benavidez, M.A.; Fox, K.; Aguillón-Durán, G.P.; Vargas-Orozco, E.A.; et al. Novel Automation of an Enzyme-Linked Immunosorbent Spot Assay Testing Method: Comparable Diagnostic Performance of the T-SPOT. TB Test Using Manual Density Gradient Cell Isolation versus Automated Positive Selection with the T-Cell Select Kit. J. Clin. Microbiol. 2022, 60, e00551-22. [Google Scholar] [CrossRef]
- Ortiz-Brizuela, E.; Apriani, L.; Mukherjee, T.; Lachapelle-Chisholm, S.; Miedy, M.; Lan, Z.; Korobitsyn, A.; Ismail, N.; Menzies, D. Assessing the Diagnostic Performance of New Commercial Interferon-γ Release Assays for Mycobacterium tuberculosis Infection: A Systematic Review and Meta-Analysis. Clin. Infect. Dis. 2023, 76, 1989–1999. [Google Scholar] [CrossRef]
- Metcalfe, J.Z.; Cattamanchi, A.; McCulloch, C.E.; Lew, J.D.; Ha, N.P.; Graviss, E.A. Test Variability of the QuantiFERON-TB Gold In-Tube Assay in Clinical Practice. Am. J. Respir. Crit. Care Med. 2013, 187, 206–211. [Google Scholar] [CrossRef]
- Whitworth, W.C.; Hamilton, L.R.; Goodwin, D.J.; Barrera, C.; West, K.B.; Racster, L.; Daniels, L.J.; Chuke, S.O.; Campbell, B.H.; Bohanon, J.; et al. Within-Subject Interlaboratory Variability of QuantiFERON-TB Gold In-Tube Tests. PLoS ONE 2012, 7, e43790. [Google Scholar] [CrossRef]
- Loureiro, R.B.; Maciel, E.L.N.; Caetano, R.; Peres, R.L.; Fregona, G.; Golub, J.E.; Braga, J.U. Cost-Effectiveness of QuantiFERON-TB Gold In-Tube versus Tuberculin Skin Test for Diagnosis and Treatment of Latent Tuberculosis Infection in Primary Health Care Workers in Brazil. PLoS ONE 2019, 14, e0225197. [Google Scholar] [CrossRef]
- Xiong, X.-S.; Zhang, X.-D.; Yan, J.-W.; Huang, T.-T.; Liu, Z.-Z.; Li, Z.-K.; Wang, L.; Li, F. Identification of Mycobacterium tuberculosis Resistance to Common Antibiotics: An Overview of Current Methods and Techniques. Infect. Drug Resist. 2024, 17, 1491–1506. [Google Scholar] [CrossRef] [PubMed]
- Dicks, K.V.; Stout, J.E. Molecular Diagnostics for Mycobacterium tuberculosis Infection. Annu. Rev. Med. 2019, 70, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.K.; Dahiya, B.; Sharma, S.; Singh, N.; Dharra, R.; Thakur, Z.; Mehta, N.; Gupta, K.B.; Gupta, M.C.; Chaudhary, D. Immuno-PCR, a New Technique for the Serodiagnosis of Tuberculosis. J. Microbiol. Methods 2017, 139, 218–229. [Google Scholar] [CrossRef] [PubMed]
- Heidebrecht, C.L.; Podewils, L.J.; Pym, A.S.; Cohen, T.; Mthiyane, T.; Wilson, D. Assessing the Utility of Xpert® MTB/RIF as a Screening Tool for Patients Admitted to Medical Wards in South Africa. Sci. Rep. 2016, 6, 19391. [Google Scholar] [CrossRef]
- Denkinger, C.M.; Schumacher, S.G.; Boehme, C.C.; Dendukuri, N.; Pai, M.; Steingart, K.R. Xpert MTB/RIF Assay for the Diagnosis of Extrapulmonary Tuberculosis: A Systematic Review and Meta-Analysis. Eur. Respir. J. 2014, 44, 435–446. [Google Scholar] [CrossRef]
- Theron, G.; Peter, J.; Calligaro, G.; Meldau, R.; Hanrahan, C.; Khalfey, H.; Matinyenya, B.; Muchinga, T.; Smith, L.; Pandie, S.; et al. Determinants of PCR Performance (Xpert MTB/RIF), Including Bacterial Load and Inhibition, for TB Diagnosis Using Specimens from Different Body Compartments. Sci. Rep. 2014, 4, 5658. [Google Scholar] [CrossRef]
- Zeka, A.N.; Tasbakan, S.; Cavusoglu, C. Evaluation of the GeneXpert MTB/RIF Assay for Rapid Diagnosis of Tuberculosis and Detection of Rifampin Resistance in Pulmonary and Extrapulmonary Specimens. J. Clin. Microbiol. 2011, 49, 4138–4141. [Google Scholar] [CrossRef]
- Mathys, V.; Van De Vyvere, M.; De Droogh, E.; Soetaert, K.; Groenen, G. False-Positive Rifampicin Resistance on Xpert® MTB/RIF Caused by a Silent Mutation in the rpoB Gene. Int. J. Tuberc. Lung Dis. 2014, 18, 1255–1257. [Google Scholar] [CrossRef]
- Walzl, G.; McNerney, R.; Du Plessis, N.; Bates, M.; McHugh, T.D.; Chegou, N.N.; Zumla, A. Tuberculosis: Advances and Challenges in Development of New Diagnostics and Biomarkers. Lancet Infect. Dis. 2018, 18, e199–e210. [Google Scholar] [CrossRef]
- Sanati, A.; Esmaeili, Y.; Khavani, M.; Bidram, E.; Rahimi, A.; Dabiri, A.; Rafienia, M.; Arbab Jolfaie, N.; Mofrad, M.R.K.; Haghjooy Javanmard, S.; et al. Smartphone-Assisted Lab-in-a-Tube Device Using Gold Nanocluster-Based Aptasensor for Detection of MUC1-Overexpressed Tumor Cells. Anal. Chim. Acta 2023, 1252, 341017. [Google Scholar] [CrossRef]
- Khan, K.; Tareen, A.K.; Iqbal, M.; Wang, L.; Ma, C.; Shi, Z.; Ye, Z.; Ahmad, W.; Rehman Sagar, R.U.; Shams, S.S.; et al. Navigating Recent Advances in Monoelemental Materials (Xenes)-Fundamental to Biomedical Applications. Prog. Solid State Chem. 2021, 63, 100326. [Google Scholar] [CrossRef]
- Szuplewska, A.; Kulpińska, D.; Dybko, A.; Chudy, M.; Jastrzębska, A.M.; Olszyna, A.; Brzózka, Z. Future Applications of MXenes in Biotechnology, Nanomedicine, and Sensors. Trends Biotechnol. 2020, 38, 264–279. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Dong, C.; Feng, W.; Wang, Y.; Huang, B.; Chen, Y. Biomedical Engineering of Two-Dimensional MXenes. Adv. Drug Deliv. Rev. 2022, 184, 114178. [Google Scholar] [CrossRef] [PubMed]
- Lozovoy, K.A.; Izhnin, I.I.; Kokhanenko, A.P.; Dirko, V.V.; Vinarskiy, V.P.; Voitsekhovskii, A.V.; Fitsych, O.I.; Akimenko, N.Y. Single-Element 2D Materials beyond Graphene: Methods of Epitaxial Synthesis. Nanomaterials 2022, 12, 2221. [Google Scholar] [CrossRef]
- Ouyang, J.; Rao, S.; Liu, R.; Wang, L.; Chen, W.; Tao, W.; Kong, N. 2D Materials-Based Nanomedicine: From Discovery to Applications. Adv. Drug Deliv. Rev. 2022, 185, 114268. [Google Scholar] [CrossRef]
- Du, C.; Du, T.; Chang, Z.; Yin, C.; Cheng, Y. On the Interface between Biomaterials and Two-Dimensional Materials for Biomedical Applications. Adv. Drug Deliv. Rev. 2022, 186, 114314. [Google Scholar] [CrossRef]
- Lin, X.; Chen, T. A Review of in Vivo Toxicity of Quantum Dots in Animal Models. Int. J. Nanomed. 2023, 18, 8143–8168. [Google Scholar] [CrossRef]
- González De La Cruz, G.; Rodríguez-Fragoso, L.; Rodríguez-Fragoso, P.; Rodríguez-López, A. Toxicity of Quantum Dots. In Toxicity of Nanoparticles-Recent Advances and New Perspectives; Muzibur Rahman, M., Uddin, J., Mohamed Asiri, A., Rezaur Rahman, M., Eds.; IntechOpen: London, UK, 2024; ISBN 978-1-83768-452-6. [Google Scholar]
- Abdellatif, A.A.H.; Younis, M.A.; Alsharidah, M.; Al Rugaie, O.; Tawfeek, H.M. Biomedical Applications of Quantum Dots: Overview, Challenges, and Clinical Potential. Int. J. Nanomed. 2022, 17, 1951–1970. [Google Scholar] [CrossRef]
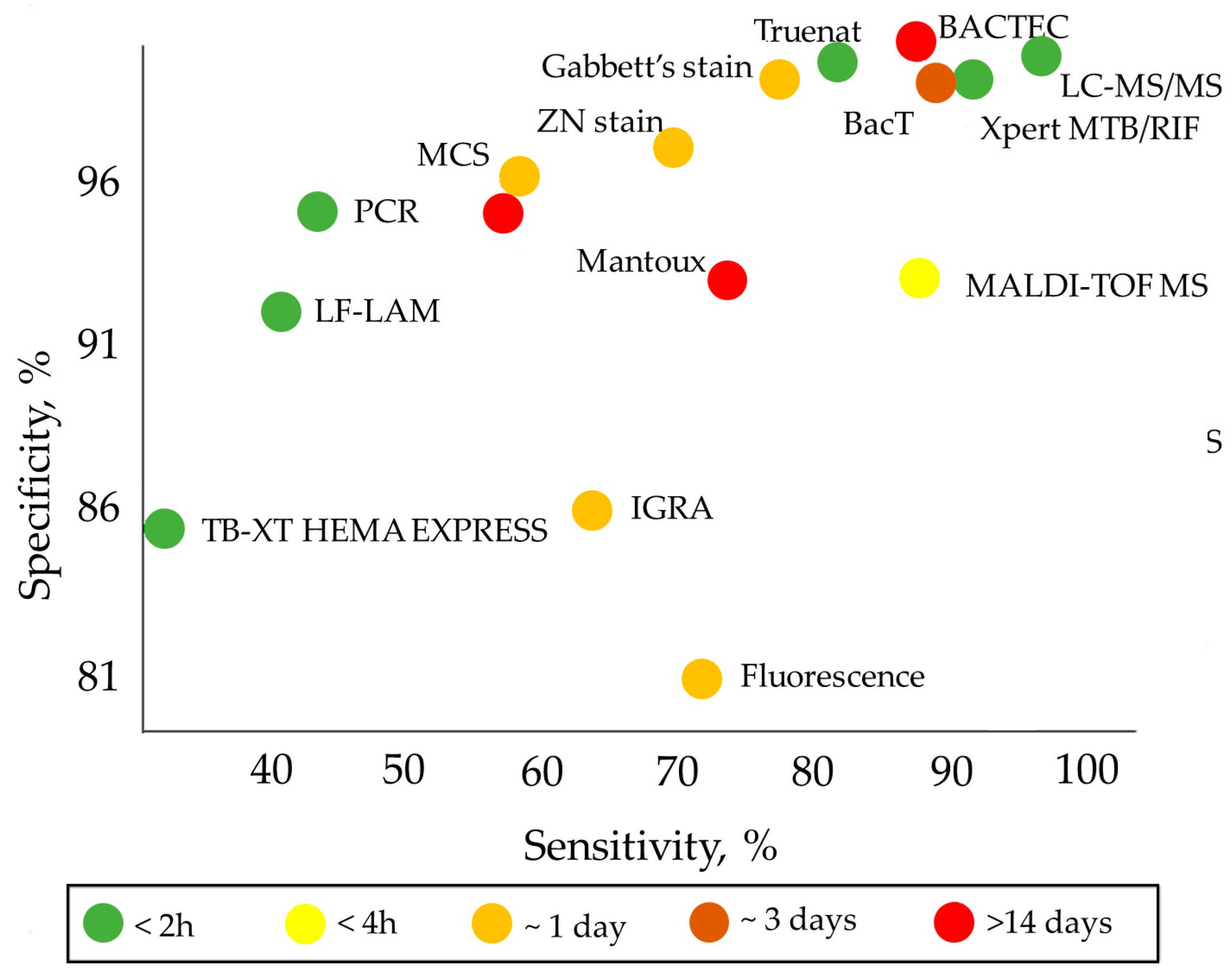

| Assay | Biomaterial Analyzed | Time of Analysis | Advantages | Drawbacks | Sensitivity, Specificity | Ref. | Comment |
|---|---|---|---|---|---|---|---|
| Molecular Diagnostic Tests | |||||||
| Polymerase chain reaction (PCR) | Serum, urine, blood, sputum, saliva, lung biopsy specimens, BALF, pleural fluid | 4–5 h | High specificity; short time of analysis; high informativeness | High cost; limited availability; low sensitivity for non-respiratory specimens | Sensitivity: 47% (42–51%) Specificity: 95% (93–97%) CrI: 95% | [10] | The sensitivity and specificity are averaged results of 9 studies on 709 subjects |
| Xpert MTB/RIF Ultra | Raw sputum or concentrated sediment | 1.5 h | Detection of specific rpoB gene mutations associated with rifampicin resistance | High cost | Sensitivity: 89% (85–92%) Specificity: 99% (98–99%) CrI: 95% | [11] | The sensitivity and specificity are averaged results of 22 studies on 8998 subjects, 2953 of them with confirmed TB |
| Truenat | Raw sputum | 1 h | A portable, chip-based, battery-operated device. Suitability for poorly equipped laboratories | Lower accuracy compared to Xpert MTB/RIF Ultra | Sensitivity: 80% (70.2–88.4%) Specificity: 98% (94.5–99.6%) | [12] | The sensitivity and specificity have been estimated in a sample of 250 subjects |
| LF-LAM | Urine | 0.5 h | High efficiency; ease of use; low cost; simple technology; no special equipment required. Detection of TB in subjects for whom other diagnostic methods cannot be used (e.g., HIV patients) | Lower sensitivity compared to Xpert MTB/RIF (though it is higher compared to microscopy methods). Suitability for a limited group of patients. Inability to distinguish M. tb. from other mycobacteria, which requires using other diagnostic methods along with the test | Sensitivity: 45% (29–63%) Specificity: 92% (80–97%) CrI: 95% | [13] | The sensitivity and specificity are averaged results of 5 studies on 2313 subjects, 35% of them with confirmed TB |
| TB-XT HEMA EXPRESS | Blood, serum | 0.5 h | Short time of analysis; relatively low cost | Low sensitivity; suboptimal performance in the case of high TB prevalence | Sensitivity: 31% (3.9–78%) Specificity: 85% так (52–93%) | [14] | The sensitivity and specificity have been estimated in a sample of 1386 subjects, 290 of them with confirmed TB |
| TB tests based on T-cell analysis | |||||||
| IGRA, (T-SPOT.TB, QuantiFERON-TB Gold (QFT)) | Blood, serum | Up to 2 days | Insensitivity to previous BCG vaccination or contact with atypical mycobacteria; high efficiency. One-time tests. T-SPOT.TB is less susceptible to immunosuppression than other TB tests and is preferable for patients with HIV or autoimmunity patients under immunosuppression treatment; it can be used before the start of therapy with biological drugs | Low specificity and sensitivity; high cost; inability to distinguish between the active and latent forms of TB; unsuitability as a primary diagnostic test for LTBI or active TB. The bacterium itself is not detected. The result depends on the state of the patient’s immune system | QFT Sensitivity: 66% (47–81%) Specificity: 87% (68–94%) T-SPOT Sensitivity: 60% (48–72%) Specificity: 86% (65–95%) | [15] | The sensitivity and specificity have been estimated in a sample of 6525 HIV-positive patients, 3467 of them with confirmed TB, including 806 with LTBI and 2661 with active TB |
| Culture methods | |||||||
| BBL Septi-Chek AFB | Sputum | Up to 23 days | Higher M.tb growth rate compared to methods using an isolated dense medium | Low sensitivity; long time of analysis | Sensitivity: 73% Specificity: 93% | [16] | The sensitivity and specificity have been estimated in a sample of 274 specimens |
| BАСТЕС (MGIT 460 and MGIT 960) | Sputum | Up to 14 days | Rapid identification of M.tb and its drug sensitivity. Accelerated testing of all first-line drugs | High cost, justified only for large laboratories. Semi-automatic monitoring of bacterium growth requiring many labor-intensive operations. Use of radioisotopes and the need for disposal of radioactive waste. Long time of analysis | MGIT 960 Sensitivity: 81.5% Specificity: 99.6% MGIT 460 Sensitivity: 85.8% Specificity: 99.9% | [17] | The sensitivity and specificity have been estimated in samples of ~8000 clinical specimens per year. The number after MGIT is the number of wells in the plate. |
| BacT/ALERT 3D | Sputum | 24–72 h | Detection of M.tb growth; detection of M.tb and fungi in blood cultures. Full automation; no radioactive waste | Long time; high cost | Sensitivity: 87.80% Specificity: 99.21% | [18] | The sensitivity and specificity have been estimated in a sample of 2659 clinical specimens |
| Skin tests | |||||||
| Tuberculin skin tests, Mantoux tests, and Diaskintest (in vivo) | Skin tests | 72 h | Availability; low cost; ease of use | Low specificity and sensitivity; unsuitability for diagnosing active TB forms. False-positive results in subjects previously infected with M.tb, because their memory T-cells still secrete interferon. Inability to distinguish between the active and latent forms of TB | Sensitivity: 59% Specificity: 95% | [19] | The sensitivity and specificity have been estimated in a sample of 643,694 US Navy recruits |
| Tests based on mycobacterium staining | |||||||
| Gabbett’s stain, Ziehl–Neelsen stain, modified cold stain (MCS) | Sputum | ~24 h | Simplicity; short time of analysis; ease of use; low cost | Low sensitivity and specificity; suitability for pulmonary tuberculosis only; inaccuracy in children and subjects with HIV; multistage and complex procedure. Inability to distinguish between different mycobacteria | Gabbett’s stain Sensitivity: 77% Specificity: 98% Ziehl–Neelsen stain Sensitivity: 70% Specificity: 97% MCS Sensitivity: 60% Specificity: 96% | [20] | The sensitivity and specificity have been estimated in a sample of 100 patients |
| Fluorescence microscopy | Sputum | ~24 h | Short time of analysis; ease of use; specificity | High cost; frequent burn-out of expensive mercury vapor lamps; need for continuous power supply; need for a dark room | Sensitivity: 72% Specificity: 81% | [21] | The sensitivity and specificity have been estimated in a sample of 426 patients |
| Other methods | |||||||
| X-ray | Radiographic test | 1 h | Short time of analysis | High cost; low specificity | Sensitivity: 96% Specificity: 46% | [22] | The sensitivity and specificity are averaged results of 13 studies |
| MALDI-TOF MS | BALF, sputum | 2.5 h | Short time of analysis; reliability; high cost efficiency | Sample preprocessing is required to generate high-quality proteomic profiles, especially for proteins/peptides or other low-abundance analytes in which MS spectra are obscured by more abundant or higher-molecular-weight species. Low specificity because of the noise caused by matrix proteins | Sensitivity: 83% Specificity: 93% CrI: 95% | [23] | The sensitivity and specificity have been estimated in a sample of 214 patients |
| LC-MS/MS | Urine, blood | 1 h | Proteomic analysis of urine; identification of proteins characteristic of TB with high molecular specificity and sensitivity; simultaneous diagnosis of HIV-1 and TB using a blood sample. Structural identity of individual components | Changes in ionization efficiency in the presence of not only proteins, phospholipids, and salts, but also reagents and contaminants | Sensitivity: 94% Specificity: 100% | [24] | The sensitivity and specificity have been estimated in a sample of 57 patients |
| No. | Biomaterial Analyzed | Biomarker | Capture Molecule | Nanosensor | Method of Detection | Wavelength, nm (Where Relevant) | LOD | Ref. |
|---|---|---|---|---|---|---|---|---|
| 1 | Blood | TMCC1, GBP6 | Oligonucleotides specific for M.tb mRNA biomarkers | QD655 and QD525 conjugated with the capture molecules | Toehold-mediated strand displacement with fluorescence quenching by FRET | Emission: 525 Emission: 655 Excitation: 480 | GBP6: 1.6 nM TMCC1: 6.4 nM | [83] |
| 2 | Blood | IFN-γ | Anti-human IFN-γ antibodies | CdS QDs coupled to magnetic beads conjugated with the capture molecules. Sandwich-type sensor is fabricated on a glassy carbon electrode coated with a well-ordered gold nanoparticle monolayer, which offers a solid support to immobilize the capture molecules | Square-wave anodic stripping voltammetry for quantifying the metal cadmium, which indirectly reflects the amount of the analyte | N/A | 0.34 pg/mL | [84] |
| 3 | Serum | IFN-γ | IFN-γ aptamer | Gold electrode coated with L-cysteine-SnTeSe QDs functionalized with the capture molecules | Electrochemical impedance spectroscopy detection of the change in the electron transfer resistance upon IFN-γ binding | N/A | 0.151 pg/mL | [85] |
| 4 | Serum | IFN-γ, TNF-α, IL-2 | Antibody pairs for IFN-γ-, TNF-α and IL-2 | Sandwich immunoassay sensor consisting of luminol and carbon and CdS QDs integrated with gold nanoparticles and magnetic beads functionalized with the capture molecules, as well as the same capture molecules separately immobilized in three spatially resolved areas of a patterned indium tin oxide electrode to capture the corresponding triple latent TB biomarkers | Electrochemiluminescence detection | N/A | 1.6 pg/mL | [86] |
| 5 | Sputum | DNA IS1081 | Specific DNA nanobeacon | QD-based nanobeacon fluorescence probes containing QDs and black hole quenchers. After the target DNA hybridizes with the nanobeacon, the nanobeacon is cleaved into two DNA fragments, and the QDs fluoresce upon moving away from the black hole quenchers | Fluorescence detection by naked eye | Excitation: 280 Emission: 330 | 3.3 amol/L (2 copies/μL) | [87] |
| 6 | N/A | Anti-MA antibodies | MAs | Graphene QDs covalently functionalized with MAs as detection tags for anti-MA antibodies | Fluorescence detection (fluorescent lateral flow assay) | Excitation: 360 Emission: 470 | N/A | [88] |
| 7 | N/A | Anti-MA antibodies | MAs | CdSe/ZnS QDs covalently functionalized with MAs as detection tags for anti-MA antibodies | Fluorescence detection (fluorescent lateral flow assay) | Excitation: 390 Emission: 474 | N/A | [89] |
| 8 | Pure CFP-10 solution | CFP-10 | Pair of anti-CFP-10 antibodies (G2 and G3) | Glass slide coated with magnetoplasmonic core/shell nanoparticles (Fe3O4/Au) functionalized with G2. Graphene QDs functionalized with conjugate of gold-binding protein with G3. Upon binding of CFP-10 by a G2–G3 sandwich, immunoassay is formed | Dual metal-enhanced fluorescence and surface-enhanced Raman scattering detection | Excitation: 320 Emission: 436, 516 | 0.0511 pg/mL | [90] |
| 9 | Pure DNA | rpoB531, katG315 | ssDNA specific for target DNA | QD535 and QD648 functionalized with specific ssDNA. When the target DNA is absent, the nanosensor is attached to a quencher. Binding with the target DNA leads to detachment of the nanosensor and recovery of fluorescence | Fluorescence detection | Excitation: 380 Emission (rpoB531): 535 Emission (katG315): 648 | rpoB531: 24 pM; katG315: 20 pM | [91] |
| 10 | Blood | IFN-γ, IP-10 | Aptamers specific for IFN-γ and IP-10 | Cytosine–Ag+–cytosine and thymine–Hg2+–thymine hairpin structures releasing the metal ions upon specific interaction with different biomarker–aptamer complexes. Ag+ and Hg2+ are bound by CdTe and carbon QDs, which are detected by fluorescence | Fluorescence detection | - | IP-10: 0.3 × 10−6 pg/mL; IFN-γ: 0.5 × 10−6 pg/mL | [92] |
| 11 | Sputum | M.tb cells | M.tb-binding peptide H8, anti-M.tb polyclonal antibodies, and anti-HSP65 monoclonal antibodies | QDs conjugated with H8 or anti-HSP65 antibodies and MMS conjugated with H8 or anti-M.tb polyclonal antibodies. Magnetic separation of the QD–M.tb–MMS complex | Fluorescence detection (fluorescence microscopy) | Excitation: 405 Emission: 610 | 103 CFU/mL | [93] |
| 12 | M.tb suspension; sputum | M.tb cells | M.tb-binding peptide H8 | Magnetic beads and QDs conjugated with H8. Magnetic separation of the QD–M.tb–magnetic bead complex | Fluorescence detection (fluorescence microscopy) | N/A | 103 CFU/mL | [94] |
| 13 | Sputum | ESAT-6 gene | Oligonucleotides specific for ESAT-6 gene | FRET-based sandwich biosensor containing CdTe QDs and gold nanoparticles (quenchers) conjugated with the capture molecules (obtained by PCR). When the marker is bound, QD fluorescence is quenched via FRET to gold nanoparticles | Fluorescence detection | Excitation: 370 Emission: 400–680 | 10 fg | [95] |
| 14 | Sputum | IS6110 DNA | ssDNA complementary to the IS6110 gene fragment | FRET-based biosensor where CdTe QDs conjugated with the capture molecule serve as a donor and Cu-TCPP, which has a greater affinity for ssDNA than double-stranded DNA, serves as an acceptor. In the absence of the marker, the QD fluorescence is quenched. Hybridization of the ssDNA with the marker results in fluorescence, the intensity of which depends on the marker concentration | Fluorescence detection | Excitation: 365 Emission: 586 | 35 pM | [96] |
| 15 | Urine | Secretory antigen Ag85B | Anti-Ag85B antibodies (GBP-50B14 and SiBP-8B3) | FRET-based biosensor where gold nanorods conjugated with GBP-50B14 serve as acceptors and silica-coated CdTe QDs conjugated with SiBP-8B3 serve as donors. When both tags bind Ag85B, FRET between the QDs and nanorods quenches the QD fluorescence | Fluorescence detection | Excitation: 350 Emission: 630 | 13 pg/mL | [97] |
| 16 | Urine | LAM | Pair of anti-LAM recombinant monoclonal antibodies | Lateral flow test using CdSe/ZnS QDs encapsulated in polymeric beads conjugated with the capture molecules; test strip with the immobilized capture molecules | Portable fluorescence detector | Excitation: 375 Emission: 620 | 50 pg/mL | [98] |
| 17 | Urine | CFP-10 | Pair of anti-CFP-10 antibodies | Glassy carbon electrode modified with graphene QD-coated Fe3O4@Ag nanoparticles and gold nanoparticles conjugated with the capture antibody. Binding of CFP-10 to the electrode results in an immune sandwich, gold nanoparticles conjugated with the detection antibody serving as signal-amplification labels | Differential pulse voltammetry | N/A | 330 pg/mL | [99] |
| 18 | Exhaled air | TB-related volatile organic biomarkers | No | Suspension of CdSe or carbon QDs. The biomarker causes changes in the absorbance and fluorescence spectra | Spectroscopic analysis | Excitation: 360–650 Emission: 300–800 | N/A | [100] |
| 19 | Exhaled air | MN | Co ion | CoTCPP nanosheets with attached CdTe QDs. The QD fluorescence is quenched in the absence of MN and is recovered upon MN binding to CoTCPP, causing QD release | Fluorescence detection | Excitation: 370 Emission: 658 | 0.59 µM | [101] |
| 20 | BALS; feces; paraffin-embedded tissues | IS6110 and IS900 DNA | M.tb-specific oligonucleotides | CdSe QDs conjugated with streptavidin and species-specific probes; magnetic beads conjugated with streptavidin and genus-specific probes. Sandwich hybridization is used to bind the biomarkers and subsequent magnet separation to concentrate the biomarker | Fluorescence detection | Excitation: 260 Emission: 655 | 12.5 ng | [102] |
| 21 | Pure fprA | fprA | Anti-fprA antibodies | Direct and double antibody sandwich lateral flow tests with CdSe/ZnS QDs conjugated with the capture molecule | Fluorescence detection | Emission: 565 | 12.5 pg/mL | [103] |
| 22 | M.tb strains | M.tb DNA | M.tb-specific ssDNA | FRET-based sensor composed of water-stable CsPbBr3 perovskite QDs conjugated to DNA probe serving as a donor and MoS2 nanosheets serving as an acceptor | Fluorescence detection | N/A | 51.9 pM | [104] |
| 23 | Pure antigens | CFP10-ESAT6 | Anti-CFP10–ESAT6 monoclonal antibody | Electrochemical immunosensor consisting of SPCE functionalized with Si nanoparticles and CdSe/ZnS QDs. The target biomarker is adsorbed on the electrode and then captured by the primary antibody, the secondary antibody being labeled with catalase, whose activity is detected electrochemically | Differential pulse voltammetry | N/A | 15 pg/mL | [105] |
| Biomarker | Already Detected with QD-Based Nanosensors | Comment | Latent Form Detection | Ref. |
|---|---|---|---|---|
| Host RNA Transcript/DNA Signatures | ||||
| GBP2, GBP5, GBP6, TMCC1 | + | Oligonucleotides (RNA, DNA) | + | [83,106] |
| PRDM1 | − | PR domain zinc finger protein 1 gene | + | [106] |
| ARG1 | − | Arginase 1 gene (encoding the arginase enzyme) | + | [106] |
| IS6110 | + | IS6110 gene | + | [96] |
| IS1081 | − | IS1081 gene | + | [107] |
| rpoB531 | + | rpoB531 gene | + | [91] |
| katG315 | + | katG315 gene | + | [91] |
| Acids and their derivatives | ||||
| MN | + | Menthyl nicotinate | − | [100] |
| MAs | + | Mycolic acids | + | [88,89] |
| Enzymes | ||||
| MNAzymes | + | Multicomponent nucleic acid enzyme | N/A | [87] |
| ADA | − | Adenosine deaminase (enzyme of purine metabolism) | + | [108] |
| KatGs | − | Catalase−peroxidase enzymes (responsible for the activation of the antituberculosis drug isoniazid) | − | [109] |
| Сytokines | ||||
| IL-1ra | Interleukin-1 receptor antagonist | − | [110] | |
| IL-2 | + | Interleukin-2 | + | [110,111] |
| IL-10 | + | Interleukin-10 | + | [110,112] |
| IL-13 | Interleukin-13 | − | [110] | |
| INF-y | + | Interferon gamma | + | [84,111,112] |
| TNF-α | + | Tumor necrosis factor alpha | + | [111] |
| INF-y IP-10 | + | Interferon-gamma-inducible protein 10 | + | [25] |
| MIP-1β | − | Macrophage inflammatory protein | N/A | [110] |
| Specific surface proteins | ||||
| CFP-10 | + | 10 kDa culture-filtered protein | + | [105,113,114] |
| Mtb Rv1468c (PE_PGRS29) | − | M.tb surface protein | N/A | [115] |
| Rv1509 | − | M.tb-specific protein | N/A | [116] |
| ESAT-6 | − | 6 kDa early secreted antigenic target | + | [113,117,118,119] |
| MPT-64 | − | M.tb protein 64 | + | [120] |
| Ag85A, Ag85B | + | Secreted protein antigen 85 complex A & B | + | [97,121] |
| PPE-68 | − | Proline–proline–glutamic acid | + | [122,123] |
| Rv2536 | − | Potential membrane protein | + | [124] |
| Rv2341 | Probable conserved lipoprotein LppQ | + | [125] | |
| Mycobacterial antigens | ||||
| 14 kDa antigen | − | 14 kDa protein antigen | N/A | [126] |
| 116 kDa antigen | − | M.tb-specific antigens | N/A | [127] |
| 19 kDa antigen | − | 19 kDa lipoprotein | + | [126] |
| 30 kDa antigen | − | Immunodominant phosphate-binding protein | N/A | [128] |
| 38 kDa antigen | − | Immunodominant lipoprotein antigen | N/A | [129] |
| 55 kDa antigen | − | M.tb-specific antigens | N/A | [130] |
| LAM | − | A glycolipid and a virulence factor associated with M.tb | + | [131] |
| A60 | − | Tuberculosis antigen | + | [132] |
| Mtb81 | − | Recombinant protein | + | [133] |
| ESAT-6 | + | M.tb-specific antigens | + | [105,134] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nikolaev, V.V.; Lepekhina, T.B.; Alliluev, A.S.; Bidram, E.; Sokolov, P.M.; Nabiev, I.R.; Kistenev, Y.V. Quantum Dot-Based Nanosensors for In Vitro Detection of Mycobacterium tuberculosis. Nanomaterials 2024, 14, 1553. https://doi.org/10.3390/nano14191553
Nikolaev VV, Lepekhina TB, Alliluev AS, Bidram E, Sokolov PM, Nabiev IR, Kistenev YV. Quantum Dot-Based Nanosensors for In Vitro Detection of Mycobacterium tuberculosis. Nanomaterials. 2024; 14(19):1553. https://doi.org/10.3390/nano14191553
Chicago/Turabian StyleNikolaev, Viktor V., Tatiana B. Lepekhina, Alexander S. Alliluev, Elham Bidram, Pavel M. Sokolov, Igor R. Nabiev, and Yury V. Kistenev. 2024. "Quantum Dot-Based Nanosensors for In Vitro Detection of Mycobacterium tuberculosis" Nanomaterials 14, no. 19: 1553. https://doi.org/10.3390/nano14191553
APA StyleNikolaev, V. V., Lepekhina, T. B., Alliluev, A. S., Bidram, E., Sokolov, P. M., Nabiev, I. R., & Kistenev, Y. V. (2024). Quantum Dot-Based Nanosensors for In Vitro Detection of Mycobacterium tuberculosis. Nanomaterials, 14(19), 1553. https://doi.org/10.3390/nano14191553









