Wearables for Engagement Detection in Learning Environments: A Review
Abstract
:1. Introduction
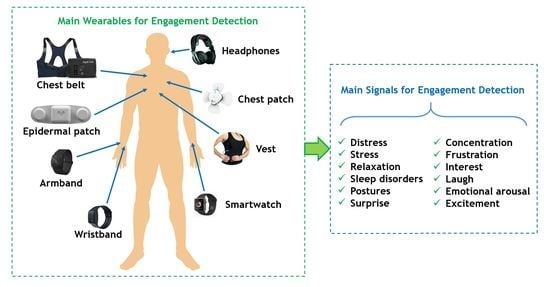
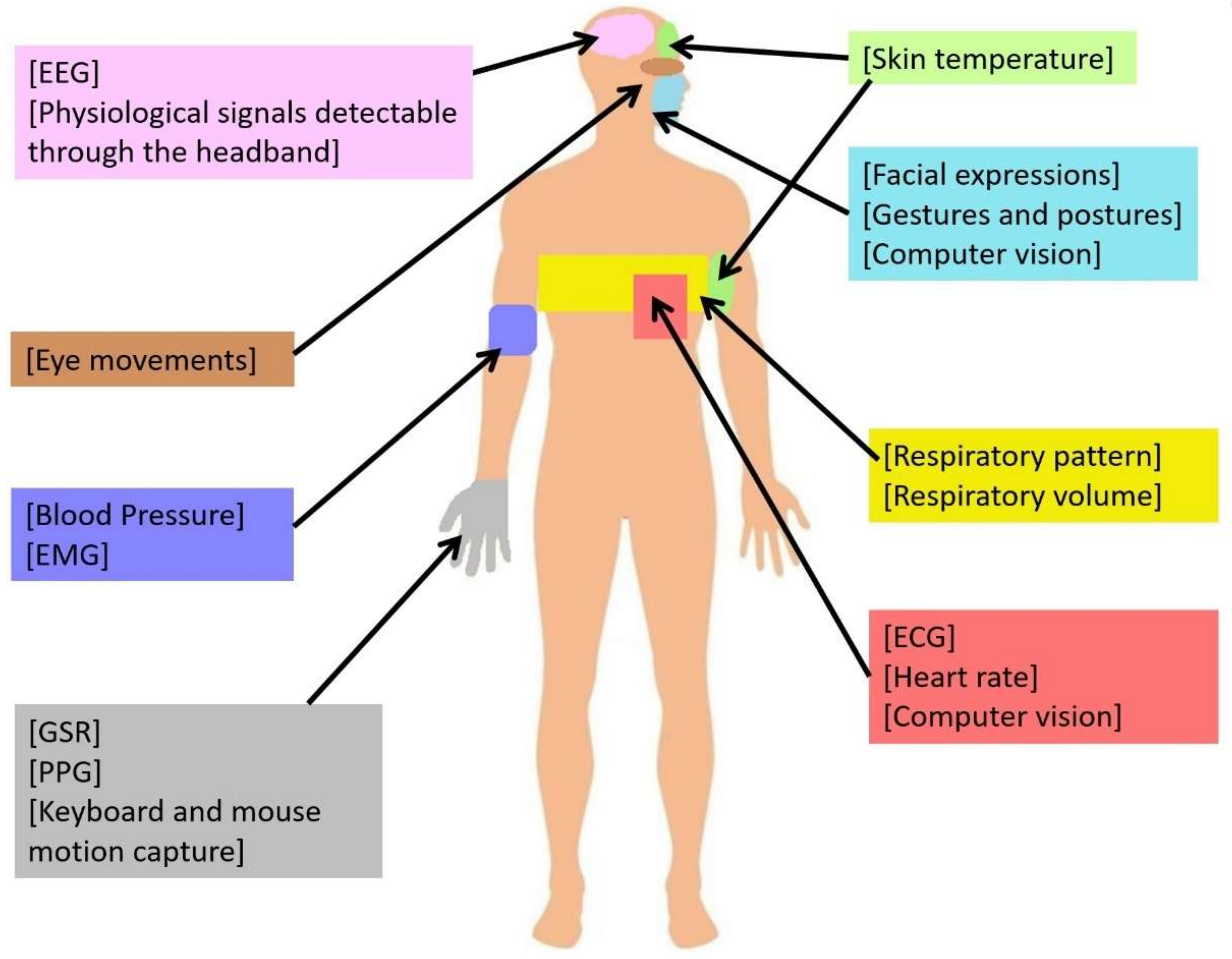
2. Main Physiological Signals for Student Engagement Detection
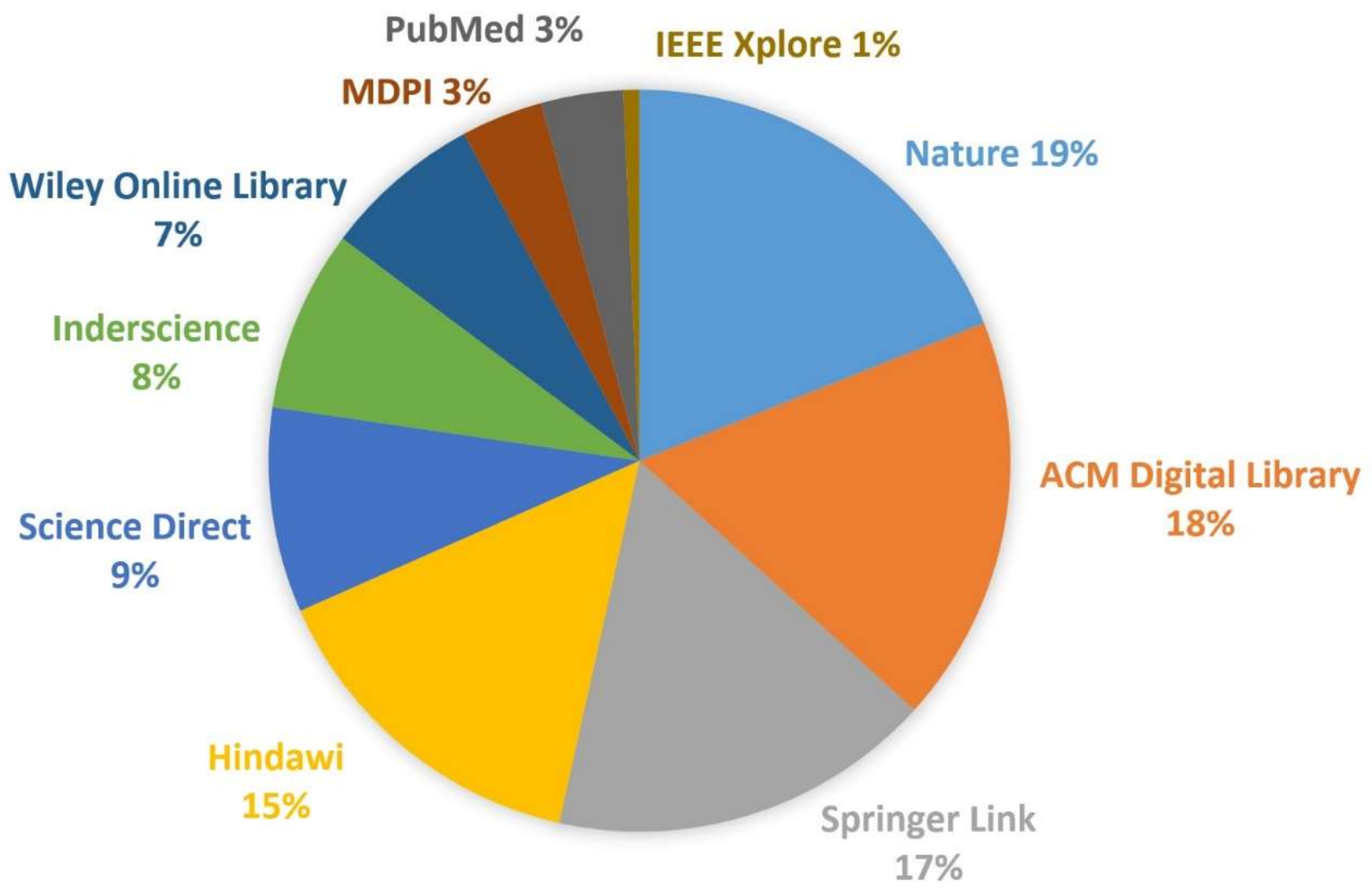
3. Methods
- Sensors and biosensors that measure these physiological variables;
- FDA-approved commercial wearable devices for engagement detection in learning environments;
- Commercially available consumer wearable devices using sensors for engagement detection in learning environments;
- Non-commercial wearable devices using sensors for engagement detection in learning environments;
- Physiological variables involved in engagement detection in learning environments.
4. Results
4.1. Study Selection
4.2. Study Characteristics
4.2.1. Classification of Wearables for Learning Engagement Detection in Learning Environments
4.2.2. Commercial Wearables for Engagement Detection
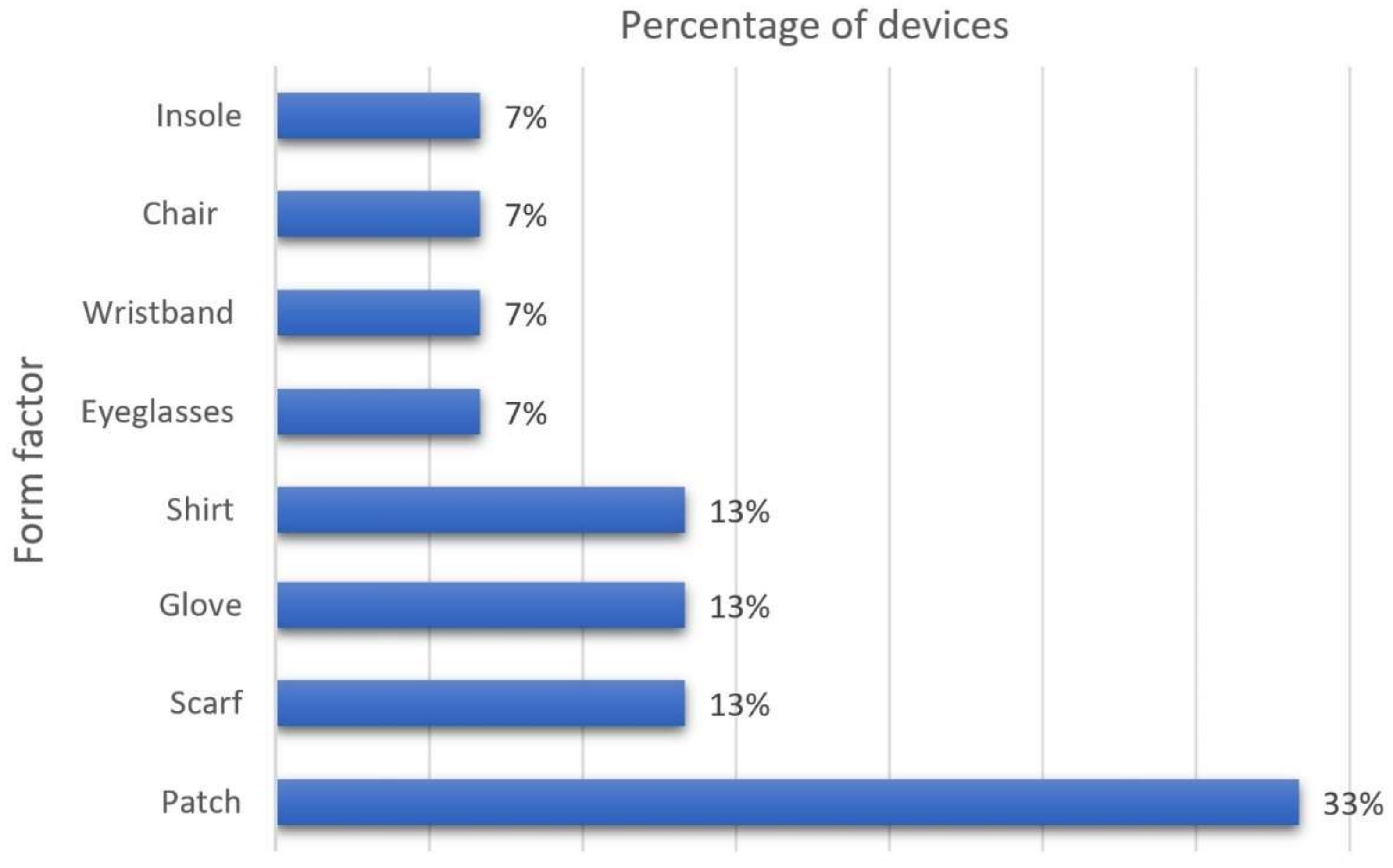
4.2.3. Non-Commercial Wearables for Engagement Level Detection
- Aim: Physiological signal(s) monitored by the wearable.
- Device type: Form factor of the device (e.g., smartwatch, bracelet, headband).
- Function: Brief description of the device’s functionality.
- Sensors: Sensor technologies used to record physiological signal data.
- Real-time monitoring capability: Whether the device can monitor physiological signals in real time.
- Educational environment: Type of educational environment where the wearable has been implemented.
| Aim | Device Type | Function | Sensors | Real-Time Monitoring Capabilities | Educational Environment |
|---|---|---|---|---|---|
| Physical exertion, health, and heart function monitoring; tracking an individual’s performance and exertion level [118]. | Patch | It consists of a patch that includes a sensor to measure a biochemical (lactate) and an electrophysiological (electrocardiogram) signal to monitor physical exertion, health, and heart. The patch can recognize emotions such as stress and anger. | Lactate sensor, electrophysiological sensors | Yes | Unstated |
| Skin temperature measuring [119]. | Patch | The patch detects multimodal biosignals, measures skin temperature with a sensitivity of 0.31 Ω/°C, skin conductance with a sensitivity of 0.28 μV/0.02 μS, and pulse wave with a response time of 70 msec. | ST, skin conductance, and pulse wave sensors | Yes | Unstated |
| Heart rate monitoring [120]. | Scarf | It helps users to reflect on their emotional state, modify their affective state, and interpret the emotional states of other people. The design of SWARM is based on a scarf so that people with different disabilities have access to this type of technology. SWARM can detect emotions such as stress, sadness, calm, happiness, and excitement. | Biosensors | Yes | Unstated |
| Heart rate and skin conductance monitoring [121]. | Scarf | It is a design of a wearable device based on a scarf form factor. The device features color-changing and olfactory properties to affect people’s emotional state. The wearable comprises two sensors: a heart rate sensor and a skin conductance sensor. When changing color and emitting an odor, the scarf potentiates positive emotions and reduces negative ones. | HR and EDA sensors | Yes | Unstated |
| Blood volume pulses and muscle contraction monitoring [122]. | Glove | It is an emotion recognition framework using machine learning of physiological patterns. The framework relies on a PPG sensor for heart rate monitoring, an EDA sensor, a skin temperature sensor, and an EMG sensor. The proposal focuses on the preprocessing of emotion recognition and supports the recognition of emotions such as happiness, anger, fear, disgust, and sadness. | PPG and EMG sensors | Yes | Unstated |
| Physiological arousal detection and monitoring [123]. | Gloves, bracelet | The device monitors the student’s psychological and physical condition using heart rate, skin conductivity, and respiration sensors. The data obtained are sent to an assistive host to process, analyze, and evaluate student moods and stress levels. | HR sensor, EDA sensor, respiratory rate sensor | Yes | Mobile |
| Detection of eye movements, eyes closed, and teeth clenching [124]. | Eyeglasses | AttentivU is a device that monitors physiological data to measure the engagement and enhance learning activities using silver electrodes. The data collected by the device can be processed in real time or sent to a separate computer. | EEG sensor or electrooculography (EOG) | Yes | Unstated |
| Monitoring of physiological characteristics related to heart rate, oximetry, skin temperature, and GSR [125]. | Patch | The proposal uses an Arduino board to obtain physiological signals from the user and connected sensors to acquire data on skin temperature, GSR, pulsometer, and a respiratory rate sensor. The data is processed using Matlab. | ST sensor, oximeter breath-flow rate sensor, HR sensor, GSR sensor | Yes | Unstated |
| Heart rate monitoring [126]. | Shirt | The prototype is based on an Arduino Uno board to which is connected a pulse sensor that uses infrared light to detect user heart rate. | Pulse sensor | Yes | Unstated |
| Human physical activity monitoring [127]. | Shirt | SensVest is a wearable prototype to monitor physical aspects. The device includes a series of sensors that allow the recording of different data related to human performance to improve the understanding of scientific concepts in students. | HR sensor, ST sensor, accelerometer | Yes | Unstated |
| Heart rate and breathing rate monitoring [128]. | Patch | The device obtains an ECG tracing using two electrodes in symmetrical positions on the user’s body and a third ground electrode placed next to one of the sensing electrodes. | Electrodes, ECG sensor | Yes | Computer video |
| Heart rate variability monitoring, skin temperature measuring [129]. | Wristband | n-Gage is a system that evaluates the engagement levels of behavioral, emotional, and cognitive students. The system detects the student’s physical and physiological signals and environmental changes in the educational environment. | EDA sensor, accelerometer, ST sensor | Unstated | Unstated |
| EDA and pulse rate monitoring [130]. | Patch | The proposal measured and recorded electrodermal activity, pulse rate, and facial recognition during an e-learning session to determine the level of student engagement. The data collected were analyzed using software developed with Matlab. | EDA sensor, HR sensor | Yes | E-learning |
| Upper body pressure distribution [131]. | Chair | While students perform e-learning reading activities, the student’s upper body pressure is recorded using a chair with a pressure mat. The data is processed using classifiers. | Pressure mat | No | E-learning |
| Feet posture and movement detection [132]. | Insole | This platform contains an insole with ground contact force (GCF) plantar pressure sensors. In addition, a microcontroller with WIFI technology collects the data and sends it to a database to be analyzed by a Human Activity Recognition classifier. | Accelerometer, gyroscope sensor, magnetometer, barometer, and range finder sensors | Yes | No specified |
5. Discussion
5.1. Challenges and Trends of Wearables for Engagement Detection
- Engagement detection proposals need to increase the number of physiological signals being monitored.
- Despite having the ability to record physiological data in real time, some wearable devices still lack mechanisms for analyzing and processing such data.
- It is important improve technical aspects of the wearables, such as battery performance and device intercommunication for data transfer.
- Engagement research is a notorious opportunity in educational research, since physiological data analysis and processing techniques can be more efficient than other techniques, such as surveys, even though they cannot always speed up findings.
- Technological trends point toward the design of non-invasive, comfortable wearable devices, and thus provide manufacturers with a great opportunity to explore the efficiency and suitability of new materials and device shapes. A clear example of this is how sensors have been innovatively incorporated into chair and insole designs. Such designs explore the suitability of measuring relatively uncommon parameters, such as pressure on some parts of the body.
- (1)
- Automatic: sensor data analysis, log-file analysis and computer vision techniques.
- (2)
- Semi-automatic: engagement tracing.
- (3)
- Manual: Observational check-list and self-reporting.
5.2. Emerging Solutions
5.3. Limitations
6. Conclusions
- In total, 32% of the commercial wearable devices reviewed are smartwatches.
- In total, 40% of the commercial wearables have either an approved FDA status or a clear status.
- Engagement detection wearables commonly assess student physiological signals such as stress and surprise through physiological signals.
- Heart rate stands as the most prominent physiological signal measured by commercial devices.
- Patches are the most common form factor of non-commercial wearables for engagement detection.
- In total, 73% of the non-commercial devices reported in the literature support real-time physiological signal monitoring.
- Physiological signals commonly recorded by non-commercial devices are related to heart rate, skin temperature, skin conductance, EDA, respiratory rate, pulse wave, and oxygen saturation.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bosch, N.; D’Mello, S.K.; Baker, R.S.; Ocumpaugh, J.; Shute, V.; Ventura, M.; Wang, L.; Zhao, W. Detecting student emotions in computer-enabled classrooms. In Proceedings of the Twenty-Fifth International Joint Conference on Artificial Intelligence, New York, NY, USA, 9–15 July 2016; pp. 4125–4129. Available online: https://pnigel.com/papers/bosch-pp-ijcai16-camera.pdf (accessed on 15 December 2021).
- Castaneda, D.; Esparza, A.; Ghamari, M.; Soltanpur, C.; Nazeran, H. A review on wearable photoplethysmography sensors and their potential future applications in health care. Int. J. Biosens. Bioelectron. 2018, 4, 195–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shabaan, M.; Arshid, K.; Yaqub, M.; Jinchao, F.; Zia, M.S.; Bojja, G.R.; Iftikhar, M.; Ghani, U.; Ambati, L.S.; Munir, R. Survey: Smartphone-based assessment of cardiovascular diseases using ECG and PPG analysis. BMC Med. Inform. Decis. Mak. 2020, 20, 177. [Google Scholar] [CrossRef] [PubMed]
- Lou, Z.; Wang, L.; Jiang, K.; Wei, Z.; Shen, G. Reviews of wearable healthcare systems: Materials, devices and system integration. Mater. Sci. Eng. R Rep. 2019, 140, 100523. [Google Scholar] [CrossRef]
- Guo, Y.; Liu, X.; Peng, S.; Jiang, X.; Xu, K.; Chen, C.; Wang, Z.; Dai, C.; Chen, W. A review of wearable and unobtrusive sensing technologies for chronic disease management. Comput. Biol. Med. 2021, 129, 104163. [Google Scholar] [CrossRef] [PubMed]
- Tandon, A.; De Ferranti, S.D. Wearable Biosensors in Pediatric Cardiovascular Disease: Promises and Pitfalls Toward Generating Actionable Insights. Circulation 2019, 140, 350–352. [Google Scholar] [CrossRef]
- Nahavandi, D.; Alizadehsani, R.; Khosravi, A.; Acharya, U.R. Application of artificial intelligence in wearable devices: Opportunities and challenges. Comput. Methods Programs Biomed. 2022, 213, 106541. [Google Scholar] [CrossRef]
- Reda, A.; El-Safty, S.A.; Selim, M.M.; Shenashen, M.A. Optical glucose biosensor built-in disposable strips and wearable electronic devices. Biosens. Bioelectron. 2021, 185, 113237. [Google Scholar] [CrossRef]
- Surantha, N.; Atmaja, P.; David; Wicaksono, M. A Review of Wearable Internet-of-Things Device for Healthcare. Procedia Comput. Sci. 2021, 179, 936–943. [Google Scholar] [CrossRef]
- Khoshmanesh, F.; Thurgood, P.; Pirogova, E.; Nahavandi, S.; Baratchi, S. Wearable sensors: At the frontier of personalised health monitoring, smart prosthetics and assistive technologies. Biosens. Bioelectron. 2021, 176, 112946. [Google Scholar] [CrossRef]
- Santo, K.; Redfern, J. Digital Health Innovations to Improve Cardiovascular Disease Care. Curr. Atheroscler. Rep. 2020, 22, 71. [Google Scholar] [CrossRef]
- Akinosun, A.S.; Polson, R.; Skeete, Y.D.; De Kock, J.H.; Carragher, L.; Leslie, S.; Grindle, M.; Gorely, T. Digital Technology Interventions for Risk Factor Modification in Patients with Cardiovascular Disease: Systematic Review and Meta-analysis. JMIR mHealth uHealth 2021, 9, e21061. [Google Scholar] [CrossRef] [PubMed]
- DeVore, A.D.; Wosik, J.; Hernandez, A.F. The Future of Wearables in Heart Failure Patients. JACC Heart Fail. 2019, 7, 922–932. [Google Scholar] [CrossRef] [PubMed]
- Burnham, J.P.; Lu, C.; Yaeger, L.; Bailey, T.C.; Kollef, M.H. Using wearable technology to predict health outcomes: A literature review. J. Am. Med. Inform. Assoc. 2018, 25, 1221–1227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.; Lu, S.; Harter, D. Multi-Sensor Eye-Tracking Systems and Tools for Capturing Student Attention and Understanding Engagement in Learning: A Review. IEEE Sens. J. 2021, 21, 22402–22413. [Google Scholar] [CrossRef]
- Apicella, A.; Arpaia, P.; Frosolone, M.; Improta, G.; Moccaldi, N.; Pollastro, A. EEG-based measurement system for monitoring student engagement in learning 4.0. Sci. Rep. 2022, 12, 5857. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Zhang, S.; Zhang, Z.; Xiao, W.; Yu, S. A framework for learning analytics using commodity wearable devices. Sensors 2017, 17, 1382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carroll, M.; Ruble, M.; Dranias, M.; Rebensky, S.; Chaparro, M.; Chiang, J.; Winslow, B. Automatic Detection of Learner Engagement Using Machine Learning and Wearable Sensors. J. Behav. Brain Sci. 2020, 10, 165–178. [Google Scholar] [CrossRef] [Green Version]
- Oh, J.; Kang, H. User engagement with smart wearables: Four defining factors and a process model. Mob. Media Commun. 2021, 9, 314–335. [Google Scholar] [CrossRef]
- Kapoor, A.; Picard, R.W. Multimodal affect recognition in learning environments. In Proceedings of the 13th Annual ACM International Conference on Multimedia, Singapore, 6–11 November 2005; pp. 677–682. [Google Scholar] [CrossRef]
- Saneiro, M.; Santos, O.C.; Salmeron-Majadas, S.; Boticario, J.G. Towards Emotion Detection in Educational Scenarios from Facial Expressions and Body Movements through Multimodal Approaches. Sci. World J. 2014, 2014, 484873. [Google Scholar] [CrossRef]
- Monkaresi, H.; Bosch, N.; Calvo, R.A.; D’Mello, S.K. Automated Detection of Engagement Using Video-Based Estimation of Facial Expressions and Heart Rate. IEEE Trans. Affect. Comput. 2017, 8, 15–28. [Google Scholar] [CrossRef]
- Angeline, R.; Nithya, A.A. A Review on Multimodal Online Educational Engagement Detection System Using Facial Expression, Eye Movement and Speech Recognition. Turk. J. Comput. Math. Educ. 2021, 12, 2013–2022. [Google Scholar] [CrossRef]
- Murshed, M.; Dewan, M.A.A.; Lin, F.; Wen, D. Engagement Detection in e-Learning Environments using Convolutional Neural Networks. In Proceedings of the 2019 IEEE Intl Conf on Dependable, Autonomic and Secure Computing, Intl Conf on Pervasive Intelligence and Computing, Intl Conf on Cloud and Big Data Computing, Intl Conf on Cyber Science and Technology Congress (DASC/PiCom/CBDCom/CyberSciTech), Fukuoka, Japan, 5–8 August 2019. [Google Scholar] [CrossRef]
- Abdellaoui, B.; Moumen, A.; Idrissi, Y.E.B.E.; Remaida, A. Face Detection to Recognize Students’ Emotion and Their Engagement: A Systematic Review. In Proceedings of the 2020 IEEE 2nd International Conference on Electronics, Control, Optimization and Computer Science (ICECOCS), Kenitra, Morocco, 2–3 December 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Salmeron-Majadas, S.; Santos, O.C.; Boticario, J.G. An Evaluation of Mouse and Keyboard Interaction Indicators towards Non-intrusive and Low Cost Affective Modeling in an Educational Context. Procedia Comput. Sci. 2014, 35, 691–700. [Google Scholar] [CrossRef] [Green Version]
- Wei, Y.; Wu, Y.; Tudor, J. A real-time wearable emotion detection headband based on EEG measurement. Sens. Actuators A Phys. 2017, 263, 614–621. [Google Scholar] [CrossRef] [Green Version]
- Anil Kumar, K.M.; Kiran, B.R.; Shreyas, B.R.; Sylvester, J.V. A Multimodal Approach to Detect User’s Emotion. Procedia Comput. Sci. 2015, 70, 296–303. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Caballero, A.; Martínez-Rodrigo, A.; Pastor, J.M.; Castillo, J.C.; Lozano-Monasor, E.; López, M.T.; Zangroniz, R.; Latorre, J.M.; Fernández-Sotos, A. Smart environment architecture for emotion detection and regulation. J. Biomed. Inform. 2016, 64, 55–73. [Google Scholar] [CrossRef]
- Egger, M.; Ley, M.; Hanke, S. Emotion Recognition from Physiological Signal Analysis: A Review. Electron. Notes Theor. Comput. Sci. 2019, 343, 35–55. [Google Scholar] [CrossRef]
- Costa, A.; Rincon, J.A.; Carrascosa, C.; Julian, V.; Novais, P. Emotions detection on an ambient intelligent system using wearable devices. Future Gener. Comput. Syst. 2019, 92, 479–489. [Google Scholar] [CrossRef] [Green Version]
- Salama, E.S.; El-Khoribi, R.A.; Shoman, M.E.; Shalaby, M.A.W. A 3D-convolutional neural network framework with ensemble learning techniques for multi-modal emotion recognition. Egypt. Inform. J. 2020, 22, 167–176. [Google Scholar] [CrossRef]
- Zhang, J.; Yin, Z.; Chen, P.; Nichele, S. Emotion recognition using multi-modal data and machine learning techniques: A tutorial and review. Inf. Fusion 2020, 59, 103–126. [Google Scholar] [CrossRef]
- Domínguez-Jiménez, J.A.; Campo-Landines, K.C.; Martínez-Santos, J.C.; Delahoz, E.J.; Contreras-Ortiz, S.H. A machine learning model for emotion recognition from physiological signals. Biomed. Signal Process. Control 2020, 55, 101646. [Google Scholar] [CrossRef]
- Bulagang, A.F.; Weng, N.G.; Mountstephens, J.; Teo, J. A review of recent approaches for emotion classification using electrocardiography and electrodermography signals. Inform. Med. Unlocked 2020, 20, 100363. [Google Scholar] [CrossRef]
- Dzedzickis, A.; Kaklauskas, A.; Bucinskas, V. Human Emotion Recognition: Review of Sensors and Methods. Sensors 2020, 20, 592. [Google Scholar] [CrossRef] [Green Version]
- Raheel, A.; Majid, M.; Anwar, S.M. DEAR-MULSEMEDIA: Dataset for emotion analysis and recognition in response to multiple sensorial media. Inf. Fusion 2021, 65, 37–49. [Google Scholar] [CrossRef]
- Kanjo, E.; Younis, E.M.G.; Ang, C.S. Deep learning analysis of mobile physiological, environmental and location sensor data for emotion detection. Inf. Fusion 2019, 49, 46–56. [Google Scholar] [CrossRef]
- Sánchez, F.L.; Hupont, I.; Tabik, S.; Herrera, F. Revisiting crowd behaviour analysis through deep learning: Taxonomy, anomaly detection, crowd emotions, datasets, opportunities and prospects. Inf. Fusion 2020, 64, 318–335. [Google Scholar] [CrossRef]
- Bhardwaj, P.; Gupta, P.K.; Panwar, H.; Siddiqui, M.K.; Morales-Menendez, R.; Bhaik, A. Application of Deep Learning on Student Engagement in e-learning environments. Comput. Electr. Eng. 2021, 93, 107277. [Google Scholar] [CrossRef]
- Dewan, M.A.A.; Murshed, M.; Lin, F. Engagement detection in online learning: A review. Smart Learn. Environ. 2019, 6, 1–20. [Google Scholar] [CrossRef]
- Henrie, C.R.; Halverson, L.R.; Graham, C.R. Measuring student engagement in technology-mediated learning: A review. Comput. Educ. 2015, 90, 36–53. [Google Scholar] [CrossRef]
- Kasatkina, D.A.; Kravchenko, A.M.; Kupriyanov, R.B.; Nekhorosheva, E.V. Automatic engagement detection in the education: Critical review. J. Mod. Foreign Psychol. 2020, 9, 59–68. [Google Scholar] [CrossRef]
- Toti, D.; Capuano, N.; Campos, F.; Dantas, M.; Neves, F.; Caballé, S. Detection of Student Engagement in e-Learning Systems Based on Semantic Analysis and Machine Learning. Netw. Syst. 2021, 158, 211–223. [Google Scholar] [CrossRef]
- Liao, J.; Liang, Y.; Pan, J. Deep facial spatiotemporal network for engagement prediction in online learning. Appl. Intell. 2021, 51, 6609–6621. [Google Scholar] [CrossRef]
- Altuwairqi, K.; Jarraya, S.K.; Allinjawi, A.; Hammami, M. Student behavior analysis to measure engagement levels in online learning environment. Signal Image Video Processing 2021, 15, 1387–1395. [Google Scholar] [CrossRef]
- Hew, K.F.; Qiao, C.; Tang, Y. Understanding student engagement in large-scale open online courses: A machine learning facilitated analysis of student’s reflections in 18 highly rated MOOCs. Int. Rev. Res. Open Distance Learn. 2018, 19, 69–93. [Google Scholar] [CrossRef]
- Imani, M.; Montazer, G.A. A survey of emotion recognition methods with emphasis on E-Learning environments. J. Netw. Comput. Appl. 2019, 147, 102423. [Google Scholar] [CrossRef]
- Hasnine, M.N.; Bui, H.T.; Tran, T.T.T.; Nguyen, H.T.; Akçapınar, G.; Ueda, H. Students’ emotion extraction and visualization for engagement detection in online learning. Procedia Comput. Sci. 2021, 192, 3423–3431. [Google Scholar] [CrossRef]
- Vanneste, P.; Oramas, J.; Verelst, T.; Tuytelaars, T.; Raes, A.; Depaepe, F.; Van den Noortgate, W. Computer vision and human behaviour, emotion and cognition detection: A use case on student engagement. Mathematics 2021, 9, 287. [Google Scholar] [CrossRef]
- Kumar, N.; Deepak, G.; Santhanavijayan, A. A Novel Semantic Approach for Intelligent Response Generation using Emotion Detection Incorporating NPMI Measure. Procedia Comput. Sci. 2020, 167, 571–579. [Google Scholar] [CrossRef]
- Panicker, S.S.; Gayathri, P. A survey of machine learning techniques in physiology based mental stress detection systems. Biocybern. Biomed. Eng. 2019, 39, 444–469. [Google Scholar] [CrossRef]
- Feidakis, M. A Review of Emotion-Aware Systems for e-Learning in Virtual Environments. In Formative Assessment, Learning Data Analytics and Gamification; Elsevier: Berkeley, CA, USA, 2016; pp. 217–242. [Google Scholar] [CrossRef]
- Rogers, K. Electroencephalography; Britannica: Chicago, IL, USA, 2017; Available online: https://www.britannica.com/science/electroencephalography (accessed on 15 November 2021).
- Health, Electrocardiogram. Available online: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/electrocardiogram (accessed on 25 September 2021).
- American Heart Association. What Is Blood Pressure? South Carolina State Documents Depository; American Heart Association: Dallas, TX, USA, 2017. [Google Scholar]
- Taj-Eldin, M.; Ryan, C.; O’Flynn, B.; Galvin, P. A Review of Wearable Solutions for Physiological and Emotional Monitoring for Use by People with Autism Spectrum Disorder and Their Caregivers. Sensors 2018, 18, 4271. [Google Scholar] [CrossRef] [Green Version]
- Healthwise Staff. Electromyogram. 2021. Available online: https://www.cigna.com/es-us/individuals-families/health-wellness/hw/electromyogram-ste122043 (accessed on 25 September 2021).
- Yasuma, F.; Hayano, J. Respiratory Sinus Arrhythmia: Why does the heartbeat synchronize with respiratory rhythm? Chest 2004, 125, 683–690. [Google Scholar] [CrossRef]
- Jamal, S.K.M.; Kamioka, E. Emotions detection scheme using facial skin temperature and heart rate variability. MATEC Web Conf. 2019, 277, 02037. [Google Scholar] [CrossRef]
- Villarejo, M.V.; Zapirain, B.G.; Zorrilla, A.M. A Stress Sensor Based on Galvanic Skin Response (GSR) Controlled by ZigBee. Sensors 2012, 12, 6075–6101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNeal, K.S.; Spry, J.M.; Mitra, R.; Tipton, J.L. Measuring Student Engagement, Knowledge, and Perceptions of Climate Change in an Introductory Environmental Geology Course. J. Geosci. Educ. 2014, 62, 655–667. [Google Scholar] [CrossRef]
- Allen, J. Photoplethysmography and its application in clinical physiological measurement. Physiol. Meas. 2007, 28, R1–R39. [Google Scholar] [CrossRef] [Green Version]
- Braun, S.R. Respiratory Rate and Pattern. In Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed.; Walker, H.K., Hall, W.D., Hurst, J.W., Eds.; Butterworths: Boston, MA, USA, 1990. Available online: https://www.ncbi.nlm.nih.gov/books/NBK365/ (accessed on 15 December 2021).
- Physiopedia, Lung Volumes. 2021. Available online: https://www.physio-pedia.com/Lung_Volumes (accessed on 25 September 2021).
- Darnell, D.K.; Krieg, P.A. Student engagement, assessed using heart rate, shows no reset following active learning sessions in lectures. PLoS ONE 2019, 14, e0225709. [Google Scholar] [CrossRef] [Green Version]
- Neuromarketing. Qué Son Los Análisis de Expresión Facial. 2021. Available online: https://neuromarketing.la/2016/12/los-analisis-expresion-facial-funcionan/ (accessed on 7 October 2021).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Tamsin, M. Wearable Biosensor Technologies. Int. J. Innov. Sci. Res. 2015, 13, 697–703. [Google Scholar]
- Dunn, J.; Runge, R.; Snyder, M. Wearables and the medical revolution. Pers. Med. 2018, 15, 429–448. [Google Scholar] [CrossRef] [Green Version]
- Seshadri, D.R.; Davies, E.V.; Harlow, E.R.; Hsu, J.J.; Knighton, S.C.; Walker, T.A.; Voos, J.E.; Drummond, C.K. Wearable Sensors for COVID-19: A Call to Action to Harness Our Digital Infrastructure for Remote Patient Monitoring and Virtual Assessments. Front. Digit. Health 2020, 2, 8. [Google Scholar] [CrossRef]
- Boscari, F.; Galasso, S.; Acciaroli, G.; Facchinetti, A.; Marescotti, M.C.; Avogaro, A.; Bruttomesso, D. Head-to-head comparison of the accuracy of Abbott FreeStyle Libre and Dexcom G5 mobile. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 425–427. [Google Scholar] [CrossRef]
- NeuroInstitute. Halo Sport 2.0. 2019. Available online: http://www.neuroinstitute.mx/index.php/tienda/halo-sport (accessed on 4 November 2021).
- Scosche. Scosche Rhythm24 Waterproof Heart Monitor Armband; Scosche: Oxnard, CA, USA, 2021. [Google Scholar]
- Akintola, A.A.; Van De Pol, V.; Bimmel, D.; Maan, A.C.; Van Heemst, D. Comparative Analysis of the Equivital EQ02 Lifemonitor with Holter Ambulatory ECG Device for Continuous Measurement of ECG, Heart Rate, and Heart Rate Variability: A Validation Study for Precision and Accuracy. Front. Physiol. 2016, 7, 391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- GlucoWISE. Imagine Living a Healthier Life with Glucowise®. Available online: http://gluco-wise.com/ (accessed on 28 July 2021).
- G-Tech Medical. G-Tech Medical. 2021. Available online: http://www.gtechmedical.com/ (accessed on 27 November 2021).
- Health Care Originals. ADAMM-RSM-SM: Health & Wellness—Health Care Originals. 2021. Available online: https://www.healthcareoriginals.com/professional/health-wellness/ (accessed on 27 November 2021).
- iRhythm. Uninterrupted Ambulatory Cardiac Monitoring. 2021. Available online: https://www.irhythmtech.com/ (accessed on 27 November 2021).
- Preventice. Listens to the Beat—Preventice Solutions. 2021. Available online: https://www.preventicesolutions.com/patients/body-guardian-heart (accessed on 27 November 2021).
- VitalConnect. VitalPatch—VitalConnect. 2021. Available online: https://vitalconnect.com/solutions/vitalpatch/ (accessed on 27 November 2021).
- ePatch. ePatch—BioTelemetry, Inc. 2021. Available online: https://www.gobio.com/clinical-research/cardiac-safety/epatch/ (accessed on 27 November 2021).
- Kenzen. KENZEN|KENZEN. 2021. Available online: https://kenzen.com/author/kenzen/page/5/ (accessed on 27 November 2021).
- Medical Device Network. Nerivio Migra Wearable Neurostimulation Device, USA. 2021. Available online: https://www.medicaldevice-network.com/projects/nerivio-migra/ (accessed on 27 November 2021).
- Medtronic. ZephyrTM Performance Systems|Performance Monitoring Technology. 2021. Available online: https://www.zephyranywhere.com/ (accessed on 3 December 2021).
- Bose Corporation. Audífonos Inalámbricos SoundSport Pulse. 28 July 2021. Available online: https://www.bose.mx/es_mx/products/headphones/earbuds/soundsport-wireless-pulse.html#ProductTabs_tab4&v=soundsport_pulse_wireless_power_red (accessed on 3 November 2021).
- VivaLink. Wearable Products. 2021. Available online: https://www.vivalink.com/wearable-products (accessed on 27 November 2021).
- Wearable Tech. Spire Health Tag Review. 2021. Available online: https://www.wareable.com/wearable-tech/spire-health-tag-review-6541 (accessed on 27 November 2021).
- Muse. MuseTM—Meditation Made Easy with the Muse Headband. 2021. Available online: https://choosemuse.com/ (accessed on 27 November 2021).
- Motiv. Motiv Ring|24/7 Smart Ring|Fitness + Sleep Tracking|Online Security Motiv Ring. 2021. Available online: https://www.mymotiv.com/ (accessed on 27 November 2021).
- Oura. Oura Ring: Accurate Health Information Accessible to Everyone. 2021. Available online: https://ouraring.com/ (accessed on 27 November 2021).
- Komodo. AIO Smart Sleeve—HRV Monitor of the Year|Best Fitness Tracker. 2021. Available online: https://komodotec.com/ (accessed on 27 November 2021).
- Apple. Apple. 2021. Available online: https://www.apple.com/ (accessed on 28 May 2021).
- Empatica. Empatica|Medical Devices, AI and Algorithms for Remote Patient Monitoring. 2021. Available online: https://www.empatica.com/en-int/embrace2/ (accessed on 27 November 2021).
- Fitbit. Sitio Oficial de Fitbit Para Smartwatches, Pulseras de Actividad, Monitores Deportivos y Mucho Más. 2021. Available online: https://www.fitbit.com/global/es/home (accessed on 27 November 2021).
- Gyenno Spoon. Gyenno, 28 July 2021. Available online: https://www.gyenno.com/spoon-en.html (accessed on 31 October 2021).
- Spiegel, B.M.R.; Kaneshiro, M.; Russell, M.M.; Lin, A.; Patel, A.; Tashjian, V.C.; Zegarski, V.; Singh, D.; Cohen, S.E.; Reid, M.W.; et al. Validation of an Acoustic Gastrointestinal Surveillance Biosensor for Postoperative Ileus. J. Gastrointest. Surg. 2014, 18, 1795–1803. [Google Scholar] [CrossRef] [PubMed]
- Garmin. Garmin|Mexico. 2021. Available online: https://www.garmin.com/es-MX/ (accessed on 28 May 2021).
- Honor. Catálogo de Productos y Lista de Precios HONOR|HONOR México. 2021. Available online: https://www.hihonor.com/mx/products/?categories=wearables (accessed on 27 November 2021).
- Huawei. HUAWEI Wearables—HUAWEI México. 2021. Available online: https://consumer.huawei.com/mx/wearables/ (accessed on 28 May 2021).
- Mobvoi. TicWatch Smartwatch/Audio|Mobvoi. 2021. Available online: https://www.mobvoi.com/la/types/smartwatches (accessed on 27 November 2021).
- Lazersport. Lazer LifeBEAM Cycling Helmet Heart Rate Monitor|Lazer Sport Helmets. 2021. Available online: https://lazersport.us/products/lifebeamdiykit (accessed on 5 November 2021).
- Kickstarter, P. KUAI—World’s First Multisport Biometric Headphones by Kuaiwear—Kickstarter. 2021. Available online: https://www.kickstarter.com/projects/carlosmarco/kuai-worlds-first-multisport-biometric-headphones (accessed on 4 November 2021).
- Omron. Wrist Blood Pressure Monitor & Watch|HeartGuide by OMRON. 2021. Available online: https://omronhealthcare.com/products/heartguide-wearable-blood-pressure-monitor-bp8000m/ (accessed on 27 November 2021).
- Code, R. Wearable technology in healthcare. Nat. Biotechnol. 2019, 37, 376. [Google Scholar] [CrossRef]
- Samsung. Samsung Gear Sport:Características, El Mejor Precio y Opiniones|Samsung España. 2021. Available online: https://www.samsung.com/es/gear-sport/highlights/ (accessed on 28 May 2021).
- Verily. Advancing Health Outcomes Through Technology, Data Science, and a Team of Experts across Clinical Research, Care, and Devices|Verily Life Sciences. 2021. Available online: https://verily.com/ (accessed on 27 November 2021).
- Withings. Hybrid Smartwatch with ECG, Heart Rate & Oximeter—ScanWatch|Withings. 2021. Available online: https://www.withings.com/de/en/scanwatch (accessed on 27 November 2021).
- Xiaomi. Xiaomi Smartwatch Mi Band 5 Versión Global—Xiaomi Store México. 2021. Available online: https://www.xiaomi-store.mx/products/mi-band-5 (accessed on 27 November 2021).
- Sensoria. Sensoria Fitness: Motion and Activity Tracking Smart Clothing for Sports and Fitness. 2021. Available online: https://store.sensoriafitness.com/ (accessed on 27 November 2021).
- Ambiotex. Smart-Tech—Ambiotex—EN Wearable for a Better Body Understanding. 2021. Available online: https://www.ambiotex.com/en/smart-tech/ (accessed on 27 November 2021).
- Hexoskin. Available online: https://www.hexoskin.com/ (accessed on 11 November 2021).
- Nuubo. Nuubo. 2021. Available online: https://www.nuubo.com/en-us (accessed on 27 November 2021).
- Zoll. ZOLL LifeVest Wearable Defibrillator|ZOLL Medical Corporation. 2021. Available online: https://lifevest.zoll.com/ (accessed on 28 May 2021).
- AliveCor. AliveCor. 2021. Available online: https://www.alivecor.com/ (accessed on 27 November 2021).
- IHealth. iHealth Feel Wireless Monitor—iHealth Labs Inc. 2021. Available online: https://ihealthlabs.com/es/products/ihealth-feel-wireless-monitor (accessed on 27 November 2021).
- Mocacare. MOCACuff—Wrist Blood Pressure Monitor. 2021. Available online: https://www.mocacare.com/mocacuff/ (accessed on 27 November 2021).
- Imani, S.; Bandodkar, A.J.; Mohan, A.M.V.; Kumar, R.; Yu, S.; Wang, J.; Mercier, P.P. A wearable chemical–electrophysiological hybrid biosensing system for real-time health and fitness monitoring. Nat. Commun. 2016, 7, 11650. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.; Sim, J.K.; Cho, Y.-H. A Flexible and Wearable Human Stress Monitoring Patch. Sci. Rep. 2016, 6, 23468. [Google Scholar] [CrossRef] [Green Version]
- Williams, M.A.; Roseway, A.; O’Dowd, C.; Czerwinski, M.; Morris, M.R. SWARM: An actuated wearable for mediating affect. In Proceedings of the 9th International Conference on Tangible, Embedded, and Embodied Interaction, Stanford, CA, USA, 15–19 January 2015; pp. 293–300. [Google Scholar] [CrossRef]
- Guo, C.; Chen, Y.V.; Qian, Z.C.; Ma, Y.; Dinh, H.; Anasingaraju, S. Designing a Smart Scarf to Influence Group Members’ Emotions in Ambience: Design Process and User Experience. In Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer: Cham, Switzerland, 2016; Volume 9738, pp. 392–402. [Google Scholar] [CrossRef]
- Hui, T.K.; Sherratt, R.S. Coverage of Emotion Recognition for Common Wearable Biosensors. Biosensors 2018, 8, 30. [Google Scholar] [CrossRef] [Green Version]
- Trmcic, B.R.; Stanojevic, G.; Sapic, R.; Labus, A.; Bogdanovic, Z. Wearable solution for assessing physiological arousal towards students’ interest and engagement in the classroom, In Proceedings of the The 11th International Conference on Virtual Learning, Craiova, Romania, 29 October 2016.
- Kosmyna, N.; Morris, C.; Sarawgi, U.; Nguyen, T.; Maes, P. AttentivU: A Wearable Pair of EEG and EOG Glasses for Real-Time Physiological Processing. In Proceedings of the 2019 IEEE 16th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Chicago, IL, USA, 19–22 May 2019. [Google Scholar] [CrossRef]
- Rodríguez-Arce, J.; Lara-Flores, L.; Portillo-Rodríguez, O.; Martínez-Méndez, R. Towards an anxiety and stress recognition system for academic environments based on physiological features. Comput. Methods Programs Biomed. 2020, 190, 105408. [Google Scholar] [CrossRef]
- Norooz, L.; Mauriello, M.L.; Jorgensen, A.; McNally, B.; Froehlich, J.E. Body Vis: A new approach to body learning through wearable sensing and visualization. In Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems, Seoul, Korea, 18–23 April 2015; pp. 1025–1034. [Google Scholar] [CrossRef]
- Theodoros, N.A.; James, F.K.; Chris, B.; Antony, S. Wearable Technologies in Education: The Lab of Tomorrow Project. Teach. Prof. Dev. 2005, 163, 163–169. [Google Scholar]
- Kanna, S.; Von Rosenberg, W.; Goverdovsky, V.; Constantinides, A.G.; Mandic, D.P. Bringing Wearable Sensors into the Classroom: A Participatory Approach [SP Education]. IEEE Signal Process. Mag. 2018, 35, 110–130. [Google Scholar] [CrossRef]
- Gao, N.; Shao, W.; Rahaman, M.S.; Salim, F.D. n-Gage: Predicting in-class Emotional, Behavioural and Cognitive Engagement in the Wild. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2020, 4, 1–26. [Google Scholar] [CrossRef]
- Al-Alwani, A. A Combined Approach to Improve Supervised E-Learning using Multi-Sensor Student Engagement Analysis. Am. J. Appl. Sci. 2016, 13, 1377–1384. [Google Scholar] [CrossRef]
- Nomura, K.; Iwata, M.; Augereau, O.; Kise, K. Estimation of Student’s Engagement Using a Smart Chair. In Proceedings of the 2018 ACM International Joint Conference and 2018 International Symposium on Pervasive and Ubiquitous Computing and Wearable Computers, Singapore, 8–12 October 2018; pp. 186–189. [Google Scholar] [CrossRef]
- André, R.D.P.; Raposo, A.B.; Fuks, H. A Platform for Assessing Physical Education Activity Engagement. In Advances in Intelligent Systems and Computing; Springer: Cham, Switzerland, 2019; Volume 903, pp. 271–276. [Google Scholar] [CrossRef]
- Rajavenkatanarayanan, A.; Babu, A.R.; Tsiakas, K.; Makedon, F. Monitoring task engagement using facial expressions and body postures. In Proceedings of the 3rd International Workshop on Interactive and Spatial Computing, Richardson, TX, USA, 12–13 April 2018; pp. 103–108. [Google Scholar] [CrossRef]
- Haveman, M.E.; van Melzen, R.; Schuurmann, R.C.; El Moumni, M.; Hermens, H.J.; Tabak, M.; de Vries, J.-P.P. Continuous monitoring of vital signs with the Everion biosensor on the surgical ward: A clinical validation study. Expert Rev. Med. Devices 2021, 18, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Nazari, G.; Bobos, P.; MacDermid, J.C.; Sinden, K.E.; Richardson, J.; Tang, A. Psychometric properties of the Zephyr bioharness device: A systematic review. BMC Sports Sci. Med. Rehabil. 2018, 10, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaman, S.U.; Tao, X.; Cochrane, C.; Koncar, V. Smart E-Textile Systems: A Review for Healthcare Applications. Electronics 2022, 11, 99. [Google Scholar] [CrossRef]
- Moldovan, O.; Iñiguez, B.; Deen, M.J.; Marsal, L.F. Graphene electronic sensors—Review of recent developments and future challenges. IET Circuits Devices Syst. 2015, 9, 446–453. [Google Scholar] [CrossRef]
- Zhang, K.; Wang, J.; Liu, T.; Luo, Y.; Loh, X.J.; Chen, X. Machine Learning-Reinforced Noninvasive Biosensors for Healthcare. Adv. Healthc. Mater. 2021, 10, 2100734. [Google Scholar] [CrossRef]




| Type of Wearable Biosensor | Description | Wearable Biosensor Technologies | Wearable Device | Applications |
|---|---|---|---|---|
| Mechanical (Accelerometers and motion sensors) [69,70]. | Accelerometers and motion sensors require the integration of another wearable physiological monitoring device as well as some type of computer software interface equipped with specific algorithms for signal manipulation and analysis. They are especially valuable when combined with wireless heart rate and ECG monitoring. | Accelerometer with ECG necklace Accelerometer and wireless heart rate monitor Motion sensor algorithm | Leap Motion Smartwatch Armband Headband Chest strap | Tracking gait Motion sensing |
| Physiological [69,70]. | Physiological sensors can be used for predicting obstructive sleep apnea and monitoring heart rate, oxygen saturation, heart rate variability, breathing rate, and oxygen saturation. Further, these sensors can measure stress levels and mental fatigue. | PPG ring sensor PPG biosensors with smartphones PPG ECG magnetic earring and wireless earpiece PPG biosensors with GSR | Ring Muse band S Armband Headband Smartwatch Wristband Abdominal patch Chest patch Chest strap Vest Abdominal respiration belt GSR Velcro electrodes | Concentration monitoring |
| Biochemical [69,70]. | Biochemical sensors can be used for non-invasive sweat monitoring through epidermal tattoo potentiometric sodium sensors with wireless signal transduction. Further, they are used for one-point wireless ECG acquisition with flexible polydimethylsiloxane (PDMS) electrodes. | Epidermal tattoo potentiometric sodium sensor Flexible PDMS electrode Flexible thick-film glucose biosensor Hydrogel-based (PAAM) photonic sensor Textile based patch with optical detection system Knitted fabric biocloth | Finger and limb motion detection |
| Manufacturer | Model | Form Factor | Sensors Used | Parameters | Physiological Signs | API | FDA |
|---|---|---|---|---|---|---|---|
| Biovotion™ [71] | Everion | Armband | HR sensor, PPG sensor | ST, SpO2, RR, HR, HRV, Sleep | Stress, relaxation | Everion device | Approved |
| Abbott [72] | FreeStyle Libre | Semi-invasive | Continuous Glucose Monitoring (CGM) sensor | ST, BP | Distress | Ambrosia | Approved (2020) |
| Halo Sport [73] | Halo Sport 2.0 | Headphones | Electro neurostimulator | Neuropriming | Halo Sport | Approved | |
| Scosche™ [74] | Scosche Rhythm24 | Armband | HR optical sensor | PPG, HR, HRV, cadence, step tracking, burned calories, distance, speed | Stress, postures, surprise | ScoscheSDK24 Framework | Not Approved |
| Equivital™ [75] | LifeMonitor | Chest belt | ECG biosensor, HR sensor, medical-grade thermometer, and tri-axis accelerometer | ST, SpO2, RR, HR, HRV, GSR | Stress, engagement | Equivital | Approved |
| Med/Wise [76] | Gluco Wise ® | Clip (thumb, forefinger or earlobe) | CGM radio wave Sensor | Continuous glucose monitor (CGM) | No specified | Gluco Wise ® | - |
| Biobeat™ [71] | Biobeat™ Chest patch | Chest patch, wrist monitor | PPG | ST, SpO2, RR, HR, HRV, BP, ECG | Stress, surprise | Biobeat | Approved (2019) |
| G-Tech Medical™ [77] | G-Tech Medical™ | Chest patch | EMG | EMG | Surprise | G-Tech Medical | - |
| Health Care Originals™ [78] | ADAMM-RSM | Chest patch | Acoustic sensor, HR sensor, temperature sensor | HR, ST, RR, cough | Stress, surprise | Health Care Originals | - |
| iRhythm™ [79] | Zio patch | Chest patch | HR sensor | ECG | Surprise | iRhythm™ | Clear (2021) |
| Preventice™ [80] | Bodyguardian Heart | Chest patch | Accelerometer, ECG sensor | ECG | Surprise | Preventice™ | Clear (2012) |
| VitalConnect™ [81] | Vital Patch | Chest patch | Accelerometer, ECG sensor, thermistor | ECG, HR, HRV, RR, ST, body posture, activity, BP, SpO2 | Stress, surprise | VitalConnect™ website | Cleared |
| BioTelemetry™ [82] | BioTelemetry™ | Chest patch | ECG sensor | ECG | Surprise | BioTelemetry™ | Cleared |
| Kenzen™ [83] | Kenzen™ | Chest patch | HR biosensor | Sweat, HR, ST | Stress, surprise | Kenzen™ | No Approved |
| Theranica Nerivio Migra™ [84] | Theranica Nerivio Migra™ | Chest patch | EMG sensor | EMG | Surprise | Theranica | Approved (2019) |
| Medtronic™ [85] | Zephyr BioHarness | Chest Strap | CGM sensor | HR, HRV, RR, body posture, activity intensity, acceleration, accelerometry, ST, burned calories, speed, distance, elevation, BP, SpO2 | Stress, surprise | Zephyr: Developer and User Tools | Approved (2012) |
| Beddit™ [71] | Beddit Sleep Monitor | Contactless in-bed sensor | PPG sensor | RR, HR, sleep measures | Stress, relaxation | Beddit™ | - |
| Beurer™ [71] | Beurer SE80 | Contactless In-bed sensor | Respiratory rate sensor, HR sensor | RR, HR, sleep measures | Stress, relaxation | Beurer™ | - |
| Cosinuss™ [71] | Cosinuss Two | Earbud | HR sensor, body temperature sensor, 3D accelerometer | HR, HRV, SpO2, activity | Stress | Cosinuss™ | - |
| Yono™ [70] | Earbud | Earbud | Thermometer | ST | Stress | Yono™ | - |
| BioIntellisense™ [71] | BioIntellisense Epidermal patch | Epidermal patch | HR sensor | ST, RR, HR, coughing, sneezing | Stress | BioIntellisense™ | Approved (2019) |
| Bose® [86] | SoundSport ® Pulse | Wireless headphones | HR sensor | HR, PPG | Stress | Bose® Connect | - |
| VivaLNK™ [87] | Fever Scout | Epidermal patch | ECG and HR sensors | ST | Stress, relaxation, surprise | VivaLINK | Approved (2017) |
| Vital Scout | Epidermal patch | ECG and HR sensors | HR, HRV, RR, activity, sleep, stress levels | Stress, relaxation | VivaLINK | Approved (2019) | |
| Spire Health™ [88] | Spire Health Tag | Fitness Tracker | HR, ECG, and RR sensors | HR, RR, breathing pattern, activity | Stress, relaxation, surprise | Spire Health™ | Not Approved |
| Muse™ [89] | Muse S | Headband | EEG sensor | EEG, PPG, SpO2, breathing pattern, sleep tracking | Relaxation, concentration, postures, surprise, frustration, interest, laugh | Muse Developers | - |
| Motiv™ [90] | Motiv Ring | Ring | Accelerometer and PPG and HR sensor | PPG, HR | Stress, surprise | Motiv™ | - |
| Oura™ [91] | Oura Ring | Ring | Body temperature sensor, optical, infrared sensors, 3D accelerometer and gyroscope sensor | PPG, HR, HRV, ST, RR, activity, sleep | Stress, surprise, relaxation | Oura Cloud API | - |
| Komodo Technologies™ [92] | AIO smart sleeve | Sleeve | ECG sensor | ECG, HR, HRV, activity intensity, SpO2, step tracking, distance | Stress, postures, surprise, interest, laugh | AIO Sleeve App | No Approved |
| Kinsa™ [71] | Kinsa | Smart thermometer | ST sensor | ST | Stress | Kinsa™ | Approved (2013) |
| Orpyx™ [70] | Surro Gait Rx | Smartwatch, shoe insert, shoe pod | Pressure sensor | BP | Stress, surprise | Orpyx™ | - |
| Surro Sense Rx | Watch, shoe insert, shoe pod | Pressure sensor | BP | Stress, surprise | Orpyx | Cleared | |
| Apple™ [93] | Watch Series 3,4,5 | Smartwatch | Oximeter, electrical HR sensor, optical HR sensor, accelerometer, gyroscope sensor | Fitness and activity-tracking, ECG, PPG, HR, HRV, sleep quality, stress levels, RR | Stress, relaxation, postures, surprise, laugh, interest | Apple™ Developer | Approved |
| Empatica™ [94] | Embrace 2 | Smartwatch | EDA sensor, peripheral temperature sensor, 3-axis accelerometer, gyroscope sensor | HR, HRV, EDA, ST, activity | Stress, engagement, laugh | Empatica™ for Developers | Approved (2018) |
| E4 | Bracelet | PPG sensor, 3-axis accelerometer, EDA sensor (GSR Sensor), infrared thermopile sensor | BVP, GSR, SC, HR, HRV | Stress, relaxation, arousal, excitement | Empatica™ for Developers | Not Approved | |
| Fitbit™ [95] | Charge 4 | Smartwatch | 3-axis accelerometer, optical HR monitor, altimeter | PPG, HR, SpO2, activity, sleep | Stress, surprise, relaxation | Fitbit™ | Not Approved |
| Ionic | Smartwatch | 3-axis accelerometer 3-axis gyroscope sensor, optical HR monitor, altimeter, ambient light sensor, vibration motor | HR, SpO2, activity, sleep | Relaxation | Fitbit™ | Approved | |
| Versa 2 | Smartwatch | 3-axis accelerometer, optical HR monitor, altimeter, ambient light sensor, relative SpO2 sensor, built-in microphone | HR, guided breathing, SpO2, step tracking, distance, stress level, sleep | Stress, relaxation, postures, surprise | Fitbit™ | Approved | |
| Gyenno [96] | Gyenno Spoon | Spoon | Accelerometer | No specified | Stress | Gyenno | - |
| Gl Logic [97] | AbStats | Abdominal device | Vibration sensor, acoustic sensor | A telemetry monitor | GI Logic | - | |
| Garmin™ [98] | Fenix 5 | Smartwatch | HR sensor | HR, SpO2, activity, sleep | Stress, relaxation | Garmin™ Connect Developer | - |
| Forerunner 945 | Smartwatch | HR sensor | HR, SpO2, RR, activity, sleep | Stress, relaxation | Garmin™ Connect Developer | - | |
| Venu | Smartwatch | Pulse oximeter, HR sensor | HR, SpO2, RR, activity, sleep | Stress, relaxation | Garmin™ Connect Developer | - | |
| Vivoactive 4 | Smartwatch | Pulse oximeter, HR sensor | HR, SpO2, RR, activity, sleep | Stress, relaxation | Garmin™ Connect Developer | - | |
| Vivomove 3 | Smartwatch | Pulse oximeter, HR sensor | Step tracking, sleep quality, HR, stress levels, body composition, SpO2, intensity minutes, details of physical activity, breathing frequency | Stress, relaxation, postures, surprise | Garmin™ Connect Developer | - | |
| Holter [75] | Stat-On™ | Portable sensor | ECG sensor | HR, HRV | Stress | No specified | - |
| Honor™ [99] | Honor Watch Magic 2 | Smartwatch | Accelerometer, gyroscope, magnetometer, optical HR sensor, ambient light measurement, and barometer | HR, stress levels, sleep quality, distance, speed, SpO2 | Stress, relaxation, surprise | Huawei™ Developers | - |
| Huawei™ [100] | Huawei Watch fit | Smartwatch | 6-axis IMU sensor (accelerometer sensor, gyroscope sensor), Optical HR sensor, capacitive sensor | HR, SpO2, sleep quality, stress levels, step tracking, distance | Stress, relaxation, postures, surprise | Huawei™ Developers | - |
| Band 6 | Smart Watch | Accelerometer, three electrodes, ECG sensor, barometric altimeter | ECG, SpO2 | Stress, relaxation, postures, surprise | Huawei™ Developers | - | |
| Mobvoi™ [101] | TicWatch Pro 2020 | Smartwatch | HR sensor | HR, step tracking | Stress, postures, surprise | Mobvoi™ Developers | - |
| LifeBeam [102] | LifeBeam diy kit | Helmet | Optical sensor | HR, blood flow, and oxygen saturation | LifeBeam | - | |
| Kuaiwear Kuai [103] | KUAI-Sport Headphones | Headphones | HR sensor and accelerometer | HR | Stress | No specified | - |
| Omron™ [104] | Heart Guide | Smartwatch | Accelerometer, PPG HR and oscillometer | PPG, HR, BP, ECG, step tracking, distance | Stress, postures, surprise, laugh, interest | OMRON API for Developers | Approved (2019) |
| OnePulse™ [105] | OnePulse™ | Smartwatch | ECG sensor | HR, activity, sleep patterns | Stress, relaxation, surprise | Not specified | Approved |
| Samsung™ [106] | Samsung™ Gear Sport | Smartwatch | Accelerometer, Gyro Sensor, Barometer, HR monitoring sensor | HR, step tracking, sleep quality | Stress, relaxation, postures, surprise | Samsung™ Developers | - |
| Samsung™ Galaxy Watch Active 2 | Smartwatch | Accelerometer, barometer, gyroscope sensor, HR sensor | HR, sleep quality, stress levels, BP, distance, step tracking | Stress, relaxation, postures, surprise | Samsung™ Developers | - | |
| SmartMonitor™ [105] | SmartMonitor™ | Smartwatch | Accelerometer | Detects repetitive shaking motions, HR, activity | Stress, surprise | SmartMonitor™ | - |
| Verily Life Sciences™ [107] | Verily Study Watch | Smartwatch | CGM sensor | Wireless monitor for pulse, HR, ECG, ST | Stress, surprise, laugh, interest | Verily | Approved (2019) |
| Viatom Technology™ [105] | Viatom Checkme O2 | Smartwatch | Oximeter, HR sensor | HR, ECG, SpO2, activity tracker, ST, sleep monitoring | Stress, relaxation, surprise, laugh, interest | Viatom | Approved |
| Withings™ [108] | Withings™ ScanWatch | Smartwatch | ECG, oximeter | ECG, HR, SpO2, step tracking, distance, sleep quality | Stress, relaxation, postures, surprise, laugh, interest | Withings™ Developer | Approved |
| Move ECG | Analog watch | Heart rate sensor, 3-axis accelerometer, 3-axis gyroscope sensor | HR, ECG | Stress | Withings Developer | - | |
| Xiaomi™ [109] | Huami Amazfit Health Band | Smartwatch | ECG sensor, pedometer | HR, movement tracking | Stress, postures, surprise | Mi Developer | Approved (2019) |
| Mi Smart Band 5 | Smartwatch | ECG sensor | HR, sleep quality, step tracking, stress level, BP | Stress, relaxation, postures, surprise | Mi Developer | Not Approved | |
| Sensoria™ [110] | T-Shirt Short Sleeve + HRM | T-Shirt | HR monitor | HR, speed, distance, step tracking | Stress, postures, surprise | Sensoria™ Platform | - |
| Ambiotex™ [111] | Ambiotex Smart Shirt | T-Shirt | ECG and HR sensors | Stress level, ECG, HR, HRV, step tracking | Stress, postures, surprise, laugh, interest | Ambiotex™ | - |
| Tempdrop™ [70] | Tempdrop™ | Underarm armband | Thermometer | ST | Stress | Tempdrop™ | - |
| Carré Technologies™ [112] | Hexoskin Smart Garments | Vest | ECG sensor | ECG, HR, HRV, RR, stress level, effort, fatigue, activity intensity, acceleration, step tracking, sleep quality, SpO2 | Stress, relaxation, postures, surprise, laugh, interest | Hexoskin Developers | - |
| Nuubo™ [113] | Nuubo Wearable ECG | Vest | ECG sensor | ECG | Surprise, laugh, interest | Nuubo™ Wearable ECG | Approved |
| Zoll™ [114] | Lifevest | Vest | Temperature sensor | ECG | Surprise, laugh, interest | Lifevest | Approved (2018) |
| AliveCor™ [115] | Kardia Band | Wristband | Electrodes | ECG | Surprise, laugh, interest | AliveCor™ | Approved (2019) |
| Ava Science™ [70] | Ava Wristband | Wristband | 2-wavelength optical PPG sensor | EDA, PPG, HR, ST | Stress, surprise, engagement, laugh | Ava | Approved |
| Sentio Solutions™ [70] | Feel | Wristband | EDA, PPG HR, and skin temperature sensors | EDA, PPG, HR, ST | Stress, surprise, engagement, laugh | Feel | - |
| iHealth™ [116] | Wireless Blood Pressure Monitor | Wristband | Oscillometer | BP, HR | Stress, surprise | iHealth™ | Approved |
| MOCACARE™ [117] | MOCACuff | Wristband | HR sensor | BP, HR, SpO2 | Stress, surprise | Mocacare™ | - |
| Wavelet™ [105] | Biostrap Wristband | Wristband | 3-axis accelerometer 3-axis gyroscope sensor | HR, HRV, SpO2, RR, in-depth sleep tracking | Stress, relaxation, postures, surprise | Biostrap | - |
| WHOOP™ [71] | WHOOP Wristband | Wristband | HR sensor | RR, HR, HRV, EDA, sleep | Stress, engagement, laugh | WHOOP™ | - |
| Physiological Signal | FDA-Approved Devices | Non-FDA Devices | Total |
|---|---|---|---|
| Distress | 1 | 0 | 1 |
| Stress | 22 | 39 | 61 |
| Relaxation | 10 | 19 | 29 |
| Sleep disorders | 1 | 0 | 1 |
| Postures | 4 | 14 | 18 |
| Surprise | 23 | 25 | 48 |
| Concentration | 0 | 1 | 1 |
| Frustration | 0 | 1 | 1 |
| Interest | 11 | 6 | 12 |
| Laugh | 10 | 6 | 16 |
| Emotional arousal | 0 | 1 | 1 |
| Excitement | 0 | 1 | 1 |
| Real-Time Monitoring | No. of Devices | Percentage |
|---|---|---|
| Yes | 13 | 87% |
| No | 2 | 13% |
| Target Parameter | No. of Devices | Percentage |
|---|---|---|
| Heart Rate | 11 | 73% |
| Skin Temperature | 5 | 33% |
| Skin Conductance | 4 | 27% |
| Electrodermal activity | 4 | 27% |
| Respiratory Rate | 2 | 13% |
| Pulse Wave | 1 | 7% |
| Oxygen Saturation | 1 | 7% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bustos-López, M.; Cruz-Ramírez, N.; Guerra-Hernández, A.; Sánchez-Morales, L.N.; Cruz-Ramos, N.A.; Alor-Hernández, G. Wearables for Engagement Detection in Learning Environments: A Review. Biosensors 2022, 12, 509. https://doi.org/10.3390/bios12070509
Bustos-López M, Cruz-Ramírez N, Guerra-Hernández A, Sánchez-Morales LN, Cruz-Ramos NA, Alor-Hernández G. Wearables for Engagement Detection in Learning Environments: A Review. Biosensors. 2022; 12(7):509. https://doi.org/10.3390/bios12070509
Chicago/Turabian StyleBustos-López, Maritza, Nicandro Cruz-Ramírez, Alejandro Guerra-Hernández, Laura Nely Sánchez-Morales, Nancy Aracely Cruz-Ramos, and Giner Alor-Hernández. 2022. "Wearables for Engagement Detection in Learning Environments: A Review" Biosensors 12, no. 7: 509. https://doi.org/10.3390/bios12070509
APA StyleBustos-López, M., Cruz-Ramírez, N., Guerra-Hernández, A., Sánchez-Morales, L. N., Cruz-Ramos, N. A., & Alor-Hernández, G. (2022). Wearables for Engagement Detection in Learning Environments: A Review. Biosensors, 12(7), 509. https://doi.org/10.3390/bios12070509