Short-Term Effect of Cigarette Smoke on Exhaled Volatile Organic Compounds Profile Analyzed by an Electronic Nose
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Study Design
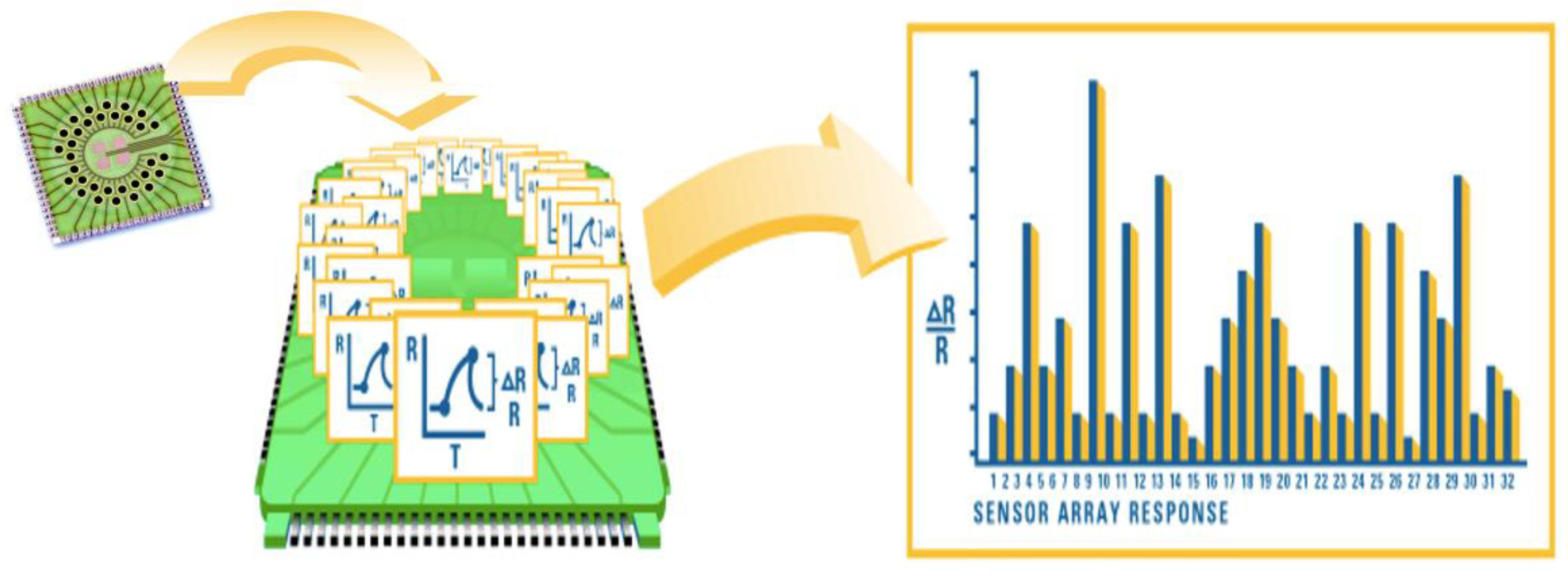
2.3. Electronic Nose
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dragonieri, S.; Pennazza, G.; Carratu, P.; Resta, O. Electronic Nose Technology in Respiratory Diseases. Lung 2017, 195, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Haddadi, S.; Koziel, J.A.; Engelken, T.J. Analytical approaches for detection of breath VOC biomarkers of cattle diseases—A review. Anal. Chim. Acta 2022, 1206, 339565. [Google Scholar] [CrossRef] [PubMed]
- Bosch, S.; Lemmen, J.P.M.; Menezes, R.; Van Der Hulst, R.; Kuijvenhoven, J.; Stokkers, P.C.F.; De Meij, T.G.J.; De Boer, N.K. The influence of lifestyle factors on fecal volatile organic compound composition as measured by an electronic nose. J. Breath Res. 2019, 13, 046001. [Google Scholar] [CrossRef] [PubMed]
- Horváth, I.; Barnes, P.J.; Loukides, S.; Sterk, P.J.; Högman, M.; Olin, A.-C.; Amann, A.; Antus, B.; Baraldi, E.; Bikov, A.; et al. A European Respiratory Society technical standard: Exhaled biomarkers in lung disease. Eur. Respir. J. 2017, 49, 1600965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zarogoulidis, P.; Freitag, L.; Besa, V.; Teschler, H.; Kurth, I.; Khan, A.M.; Sommerwerck, U.; Baumbach, J.I.; Darwiche, K. Exhaled volatile organic compounds discriminate patients with chronic obstructive pulmonary disease from healthy subjects. Int. J. Chronic Obstr. Pulm. Dis. 2015, 10, 399–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamimi, A.; Serdarevic, D.; Hanania, N.A. The effects of cigarette smoke on airway inflammation in asthma and COPD: Therapeutic implications. Respir. Med. 2012, 106, 319–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, P.; Huang, Q.; Meng, S.; Mu, T.; Liu, Z.; He, M.; Li, Q.; Zhao, S.; Wang, S.; Qiu, M. Identification of lung cancer breath biomarkers based on perioperative breathomics testing: A prospective observational study. EClinicalMedicine 2022, 47, 101384. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Yu, M.; Chen, C.; Liu, L.; Zhao, P.; Shen, B.; Sun, R. The Emission of VOCs and CO from Heated Tobacco Products, Electronic Cigarettes, and Conventional Cigarettes, and Their Health Risk. Toxics 2021, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Raspagliesi, F.; Bogani, G.; Benedetti, S.; Grassi, S.; Ferla, S.; Buratti, S. Detection of Ovarian Cancer through Exhaled Breath by Electronic Nose: A Prospective Study. Cancers 2020, 12, 2408. [Google Scholar] [CrossRef] [PubMed]
- Dragonieri, S.; Quaranta, V.N.; Carratù, P.; Ranieri, T.; Buonamico, E.; Carpagnano, G.E. Breathing Rhythm Variations during Wash-In Do Not Influence Exhaled Volatile Organic Compound Profile Analyzed by an Electronic Nose. Molecules 2021, 26, 2695. [Google Scholar] [CrossRef] [PubMed]
- Dragonieri, S.; Scioscia, G.; Quaranta, V.N.; Carratu, P.; Venuti, M.P.; Falcone, M.; Carpagnano, G.E.; Foschino Barbaro, M.P.; Resta, O.; Lacedonia, D. Exhaled volatile organic compounds analysis by e-nose can detect idiopathic pulmonary fibrosis. J. Breath Res. 2020, 14, 047101. [Google Scholar] [CrossRef] [PubMed]
- Gordon, M.S.; Wallace, L.A.; Brinkman, A.C. Volatile organic compounds as breath biomparkers for active and passive smoking. Environ. Health Perspect. 2002, 110, 689–698. [Google Scholar] [CrossRef] [PubMed]
- Principe, S.; van Bragt, J.J.M.H.; Longo, C.; de Vries, R.; Sterk, P.J.; Scichilone, N.; Vijverberg, S.J.H.; Maitland-van der Zee, A.H. The Influence of Smoking Status on Exhaled Breath Profiles in Asthma and COPD Patients. Molecules 2021, 26, 1357. [Google Scholar] [CrossRef] [PubMed]
- Gaida, A.; Holz, O.; Nell, C.; Schuchardt, S.; Lavae-Mokhtari, B.; Kruse, L.; Boas, U.; Langejuergen, J.; Allers, M.; Zimmermann, S.; et al. A dual center study to compare breath volatile organic compounds from smokers and non-smokers with and without COPD. J. Breath Res. 2016, 10, 026006. [Google Scholar] [CrossRef]
- Papaefstathiou, E.; Stylianou, M.; Andreou, C.; Agapiou, A. Breath analysis of smokers, non-smokers, and e-cigarette users. J. Chromatogr. B 2020, 1160, 122349. [Google Scholar] [CrossRef]
- Van Bragt, J.J.; Brinkman, P.; De Vries, R.; Vijverberg, S.J.; Weersink, E.J.; Haarman, E.G.; De Jongh, F.H.; Kester, S.; Lucas, A.; in't Veen, J.C.C.M.; et al. Identification of recent exacerbations in COPD patients by electronic nose. ERJ Open Res. 2020, 6, 00307-2020. [Google Scholar] [CrossRef]
- De Groot, J.C.; Amelink, M.; Storm, H.; Reitsma, B.H.; Bel, E.; Ten Brinke, A. Identification of Three Subtypes of Non-Atopic. Asthma Using Exhaled Breath Analysis by Electronic Nose. Am. Thorac. Soc. 2014, 189, A2170. [Google Scholar]
- Fens, N.; De Nijs, S.B.; Peters, S.; Dekker, T.; Knobel, H.H.; Vink, T.J.; Willard, N.P.; Zwinderman, A.H.; Krouwels, F.H.; Janssen, H.-G.; et al. Exhaled air molecular profiling in relation to inflammatory subtype and activity in COPD. Eur. Respir. J. 2011, 38, 1301–1309. [Google Scholar] [CrossRef] [PubMed]
- Caruso, M.; Emma, R.; Brinkman, P.; Sterk, P.J.; Bansal, A.T.; De Meulder, B.; Lefaudeux, D.; Auffray, C.; Fowler, S.J.; Rattray, N.; et al. Volatile Organic Compounds Breathprinting of U-BIOPRED Severe Asthma smokers/ex-smokers cohort. Airw. Cell Biol. Immunopathol. 2017, 50, PA2018. [Google Scholar] [CrossRef]
- Thomson, N.C. Asthma and smoking-induced airway disease without spirometric COPD. Eur. Respir. J. 2017, 49, 1602061. [Google Scholar] [CrossRef] [Green Version]




| Parameter | Value |
|---|---|
| Subjects (n.) | 24 |
| M/F (n.) | 11\13 |
| Age (y.) | 35.4 ± 11.3 |
| FEV1%pred. | 101.5 ± 11.8 |
| BMI (kg/m2) | 25.77 ± 3.2 |
| Current smokers (n.) | 24 |
| Comorbidities (n.) | 0 |
| PC1 | PC2 | PC3 | PC4 | p | |
|---|---|---|---|---|---|
| T0 | −0.259 ± 0.499 | 0.858 ± 1.215 | −0.210 ± 0.723 | 0.654 ± 1.092 | 0.114 |
| T1 | −0.009 ± 0.644 | 0.151 ± 0.800 | 0.023 ± 1.004 | −0.114 ± 0.854 | 0.000 |
| T2 | 0.402 ± 0.506 | −0.218 ± 0.609 | 0.381 ± 0.947 | −0.235 ± 0.753 | 0.140 |
| T3 | −0.133 ± 1.718 | −0.790 ± 0.382 | −0.193 ± 1.209 | −0.305 ± 1.012 | 0.002 |
| Time | Cross Validate Value (%) | AUC [CI]; p Value |
|---|---|---|
| T0 vs. T1 | 64.6 | 0.832 [0.715–0.948]; p < 0.05 |
| T0 vs. T2 | 83.6 | 0.927 [0.853–1.000]; p < 0.01 |
| T0 vs. T3 | 89.6 | 0.933 [0.977–1.000]; p < 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dragonieri, S.; Quaranta, V.N.; Buonamico, E.; Battisti, C.; Ranieri, T.; Carratu, P.; Carpagnano, G.E. Short-Term Effect of Cigarette Smoke on Exhaled Volatile Organic Compounds Profile Analyzed by an Electronic Nose. Biosensors 2022, 12, 520. https://doi.org/10.3390/bios12070520
Dragonieri S, Quaranta VN, Buonamico E, Battisti C, Ranieri T, Carratu P, Carpagnano GE. Short-Term Effect of Cigarette Smoke on Exhaled Volatile Organic Compounds Profile Analyzed by an Electronic Nose. Biosensors. 2022; 12(7):520. https://doi.org/10.3390/bios12070520
Chicago/Turabian StyleDragonieri, Silvano, Vitaliano Nicola Quaranta, Enrico Buonamico, Claudia Battisti, Teresa Ranieri, Pierluigi Carratu, and Giovanna Elisiana Carpagnano. 2022. "Short-Term Effect of Cigarette Smoke on Exhaled Volatile Organic Compounds Profile Analyzed by an Electronic Nose" Biosensors 12, no. 7: 520. https://doi.org/10.3390/bios12070520
APA StyleDragonieri, S., Quaranta, V. N., Buonamico, E., Battisti, C., Ranieri, T., Carratu, P., & Carpagnano, G. E. (2022). Short-Term Effect of Cigarette Smoke on Exhaled Volatile Organic Compounds Profile Analyzed by an Electronic Nose. Biosensors, 12(7), 520. https://doi.org/10.3390/bios12070520








