A Review of Commercial and Non-Commercial Wearables Devices for Monitoring Motor Impairments Caused by Neurodegenerative Diseases
Abstract
1. Introduction
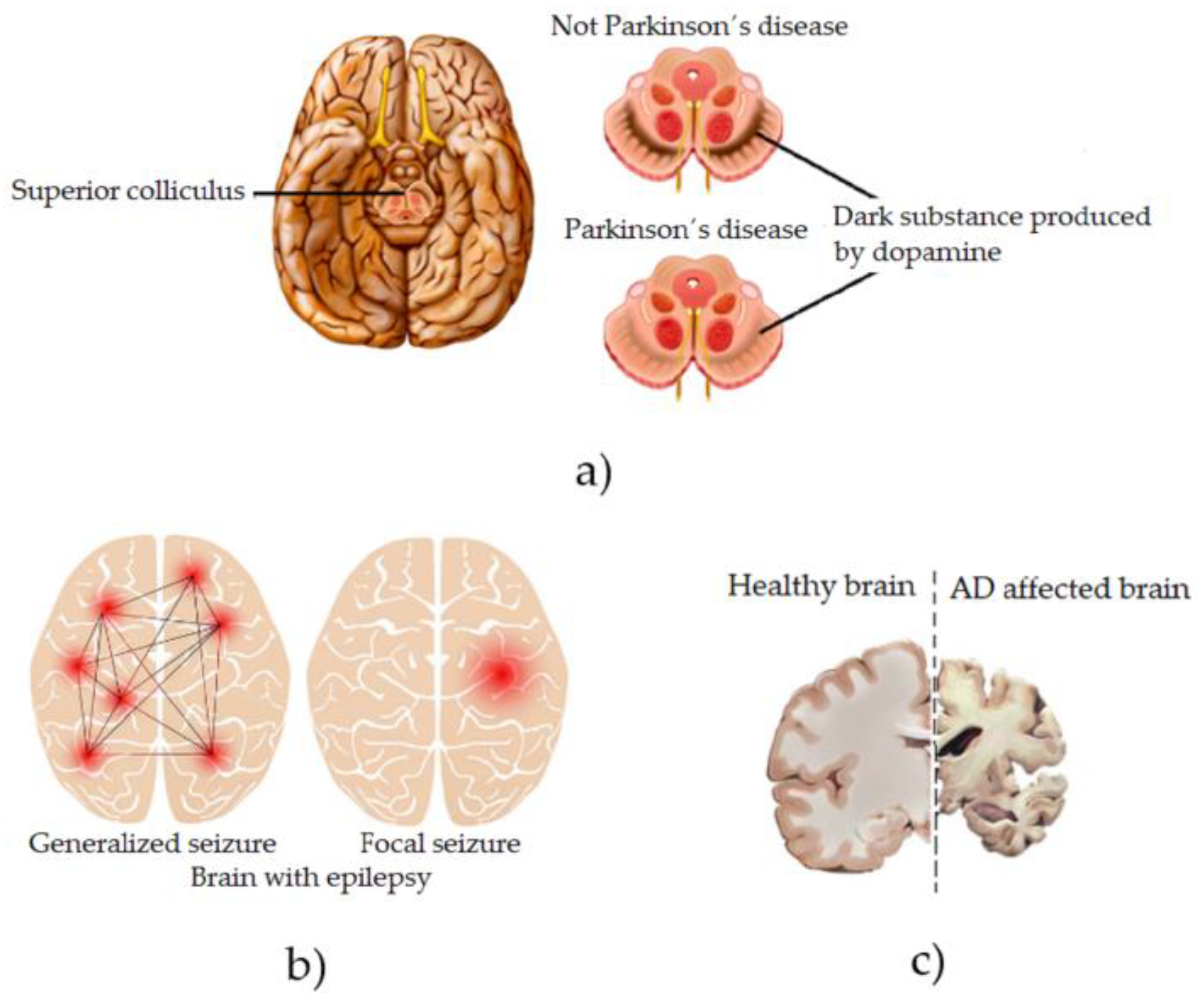
Common Motor Impairments Caused by NDDs
2. Research Goal and Need for Literature Review
3. Methods
3.1. Research Questions and Motivations
3.2. Search Strategy
3.3. Selection of Primary Studies
3.3.1. Collection of Sources
3.3.2. Inclusion and Exclusion Criteria
3.3.3. Information Sources
3.3.4. Search Strategy
- Main motor impairments related to NDDs.
- Wearable devices used to monitor NDD-related impairments.
- Commercial and non-commercial wearable devices for monitoring NDDs.
- Commercial sensors used in wearable devices.
- FDA status of commercial wearable devices.
3.3.5. Selection Process
3.3.6. Data Collection and Analysis
3.4. Data Extraction
4. Results
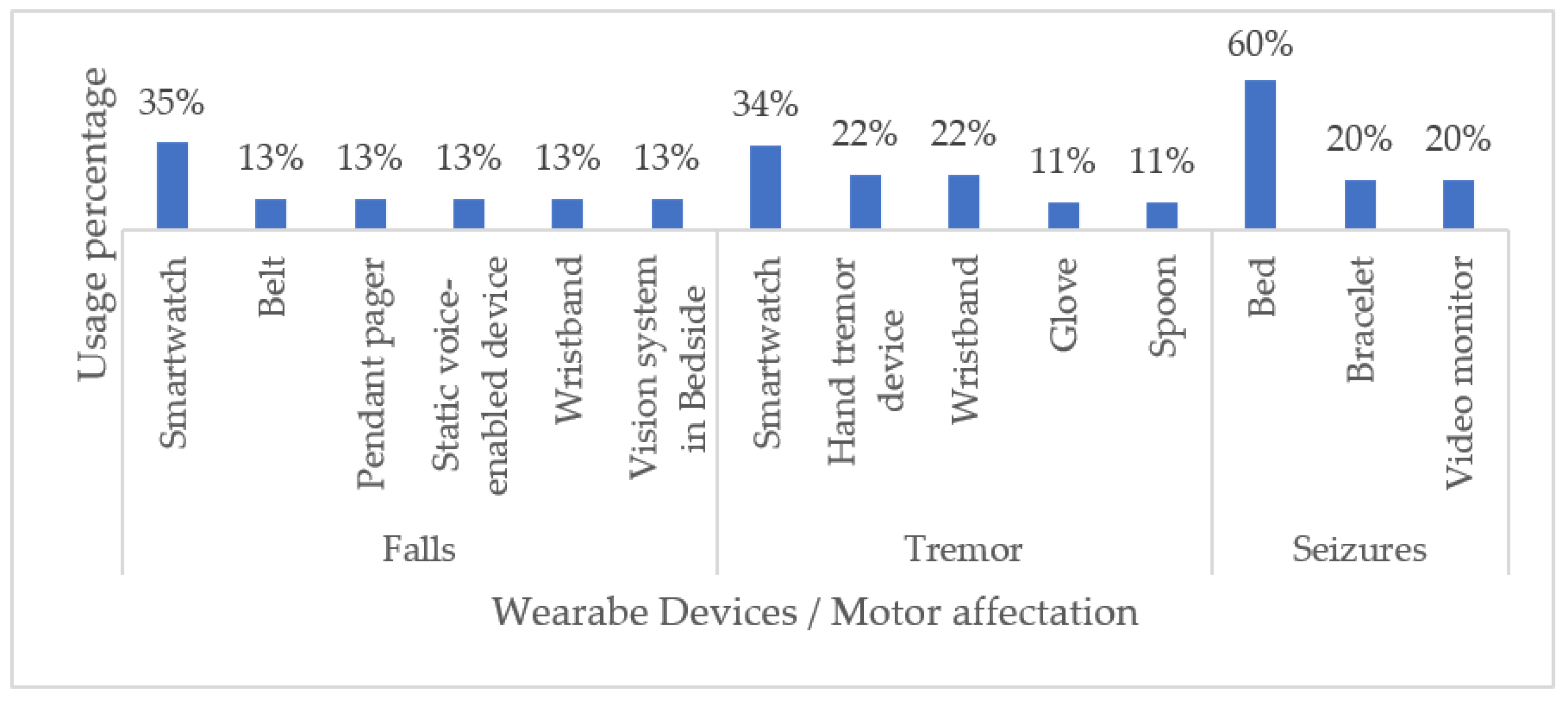
4.1. RQ1. Which Are Commercial Wearables for Monitoring NDD-Related Motor Impairments Currently Available?
4.2. RQ2. Which Are the Top Most Used Commercial Wearables for Monitoring Motor Impairment in Patients with NDDs?
4.3. RQ3. Which Are Technical Characteristics of Non-Commercial Wearables for Monitoring NDD-Related Motor Impairments Currently Available?
- Year of publication of the research;
- Aimed NDD;
- Type of wearable device;
- Brief research description;
- Sensors or technology used;
- Real-time device monitoring capability.
4.4. RQ4. Which Are the FDA Status of Commercial Wearables for Monitoring NDD-Related Motor Impairments Currently Available?
4.5. RQ5. What Are the Gaps in the Monitoring of NDDs Using Commercial Wearables Devices? And How Are These Gaps Covered by the Non-Commercial Wearables Devices?
5. Discussion
5.1. Challenges and Trends
- Research new risk factors (biomarkers and/or biometric factors) for NDDs.
- Optimize monitoring and measuring algorithms.
- Develop non-invasive and transparent technology for users.
- Optimize the connectivity of the data transmitted/received by these devices through wireless networks and personal area networks (PANs).
- Develop devices that optimally manage power consumption and rely on alternative sources of energy, such as solar energy.
- Guarantee the security and privacy of patient data.
5.2. Emerging Solutions
5.3. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gugliandolo, G.; Campobello, G.; Capra, P.P.; Marino, S.; Bramanti, A.; di Lorenzo, G.; Donato, N. A movement-tremors recorder for patients of neurodegenerative diseases. IEEE Trans. Instrum. Meas. 2019, 68, 1451–1457. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Available online: https://www.who.int (accessed on 10 July 2022).
- World Health Organization. World Health Statistics 2022: Monitoring Health for the SDGs, Sustainable Development Goals; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Castelpietra, G.; Knudsen, A.K.S.; Agardh, E.E.; Armocida, B.; Beghi, M.; Iburg, K.M.; Monasta, L. The burden of mental disorders, substance use disorders and self-harm among young people in Europe, 1990–2019: Findings from the Global Burden of Disease Study 2019. Lancet Reg. Health-Eur. 2022, 16, 100341. [Google Scholar] [CrossRef]
- WHO Reveals Leading Causes of Death and Disability Worldwide: 2000–2019? Available online: https://www.who.int/es/news/item/09-12-2020-who-reveals-leading-causes-of-death-and-disability-worldwide-2000–2019 (accessed on 10 July 2022).
- Dementia. Available online: https://www.who.int/es/news-room/fact-sheets/detail/dementia (accessed on 10 July 2022).
- Kiper, P.; Richard, M.; Stefanutti, F.; Pierson-Poinsignon, R.; Cacciante, L.; Perin, C.; Meroni, R. Combined Motor and Cognitive Rehabilitation: The Impact on Motor Performance in Patients with Mild Cognitive Impairment. Systematic Review and Meta-Analysis. J. Pers. Med. 2022, 12, 276. [Google Scholar] [CrossRef]
- Cicirelli, G.; Impedovo, D.; Dentamaro, V.; Marani, R.; Pirlo, G.; D’Orazio, T. Human gait analysis in neurodegenerative diseases: A review. IEEE J. Biomed. Health Inform. 2021, 26, 229–242. [Google Scholar] [CrossRef]
- Seneviratne, S.; Hu, Y.; Nguyen, T.; Lan, G.; Khalifa, S.; Thilakarathna, K.; Seneviratne, A. A survey of wearable devices and challenges. IEEE Commun. Surv. Tutor. 2017, 19, 2573–2620. [Google Scholar] [CrossRef]
- Feng, L.; Jing-Long, H.; Ji, Q.I.; Zhang, Y.; Jia-Luo, Y.; Wen-Peng, L.; Bo-Wei, L. Research and application progress of intelligent wearable devices. Chin. J. Anal. Chem. 2021, 49, 159–171. [Google Scholar]
- Syaifudin, Y.W.; Funabiki, N.; Kuribayashi, M.; Kao, W.C. A proposal of Advanced Widgets learning topic for interactive application in Android programming learning assistance system. SN Comput. Sci. 2021, 2, 1–13. [Google Scholar] [CrossRef]
- Sarkar, A.; Goyal, A.; Hicks, D.; Sarkar, D.; Hazra, S. Android application development: A brief overview of android platforms and evolution of security systems. In Proceedings of the 2019 Third International Conference on I-SMAC (IoT in Social, Mobile, Analytics and Cloud) (I-SMAC), Palladam, India, 12–14 December 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 73–79. [Google Scholar]
- Haghi, M.; Thurow, K.; Stoll, R. Wearable devices in medical internet of things: Scientific research and commercially available devices. Healthc. Inform. Res. 2017, 23, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Won, P.; Kim, K.K.; Kim, H.; Park, J.J.; Ha, I.; Shin, J.; Ko, S.H. Transparent soft actuators/sensors and camouflage skins for imperceptible soft robotics. Adv. Mater. 2021, 33, 2002397. [Google Scholar] [CrossRef] [PubMed]
- Anwer, A.H.; Khan, N.; Ansari, M.Z.; Baek, S.S.; Yi, H.; Kim, S.; Jeong, C. Recent advances in touch sensors for flexible wearable devices. Sensors 2022, 22, 4460. [Google Scholar] [CrossRef]
- Talitckii, A.; Kovalenko, E.; Anikina, A.; Zimniakova, O.; Semenov, M.; Bril, E.; Somov, A. Avoiding misdiagnosis of Parkinson’s disease with the use of wearable sensors and artificial intelligence. IEEE Sens. J. 2020, 21, 3738–3747. [Google Scholar] [CrossRef]
- Hathaliya, J.J.; Modi, H.; Gupta, R.; Tanwar, S.; Sharma, P.; Sharma, R. Parkinson and essential tremor classification to identify the patient’s risk based on tremor severity. Comput. Electr. Eng. 2022, 101, 107946. [Google Scholar] [CrossRef]
- Ma, C.; Li, D.; Pan, L.; Li, X.; Yin, C.; Li, A.; Zong, R. Quantitative assessment of essential tremor based on machine learning methods using wearable device. Biomed. Signal Process. Control. 2022, 71, 103244. [Google Scholar] [CrossRef]
- Balestrino, R.; Schapira, A.H.V. Parkinson disease. Eur. J. Neurol. 2020, 27, 27–42. [Google Scholar] [CrossRef]
- Armstrong, M.J.; Okun, M.S. Diagnosis and treatment of Parkinson disease: A review. Jama 2020, 323, 548–560. [Google Scholar] [CrossRef]
- Blauwendraat, C.; Nalls, M.A.; Singleton, A.B. The genetic architecture of Parkinson’s disease. Lancet Neurol. 2020, 19, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Thijs, R.D.; Surges, R.; O’Brien, T.J.; Sander, J.W. Epilepsy in adults. Lancet 2019, 393, 689–701. [Google Scholar] [CrossRef]
- Walsh, S.; Donnan, J.; Fortin, Y.; Sikora, L.; Morrissey, A.; Collins, K.; MacDonald, D. A systematic review of the risks factors associated with the onset and natural progression of epilepsy. Neurotoxicology 2017, 61, 64–77. [Google Scholar] [CrossRef]
- Pitkänen, A.; Löscher, W.; Vezzani, A.; Becker, A.J.; Simonato, M.; Lukasiuk, K.; Beck, H. Advances in the development of biomarkers for epilepsy. Lancet Neurol. 2016, 15, 843–856. [Google Scholar] [CrossRef]
- Lane, C.A.; Hardy, J.; Schott, J.M. Alzheimer’s disease. Eur. J. Neurol. 2018, 25, 59–70. [Google Scholar] [CrossRef]
- Knopman, D.S.; Amieva, H.; Petersen, R.C.; Chételat, G.; Holtzman, D.M.; Hyman, B.T.; Jones, D.T. Alzheimer disease. Nat. Rev. Dis. Prim. 2021, 7, 33. [Google Scholar] [CrossRef] [PubMed]
- Uwishema, O.; Mahmoud, A.; Sun, J.; Correia, I.F.S.; Bejjani, N.; Alwan, M.; Dost, B. Is Alzheimer’s disease an infectious neurological disease? A review of the literature. Brain Behav. 2022, 12, e2728. [Google Scholar] [CrossRef] [PubMed]
- Rigas, G.; Tzallas, A.T.; Tsipouras, M.G.; Bougia, P.; Tripoliti, E.E.; Baga, D.; Konitsiotis, S. Assessment of tremor activity in the Parkinson’s disease using a set of wearable sensors. IEEE Trans. Inf. Technol. Biomed. 2012, 16, 478–487. [Google Scholar] [CrossRef]
- Ali, S.M.; Arjunan, S.P.; Peters, J.; Perju-Dumbrava, L.; Ding, C.; Eller, M.; Kumar, D.K. Wearable sensors during drawing tasks to measure the severity of essential tremor. Sci. Rep. 2022, 12, 5242. [Google Scholar] [CrossRef] [PubMed]
- Fernando, E.; Fraser, M.; Hendriksen, J.; Kim, C.H.; Muir-Hunter, S.W. Risk factors associated with falls in older adults with dementia: A systematic review. Physiother. Can. 2017, 69, 161–170. [Google Scholar] [CrossRef]
- Brims, L.; Oliver, K. Effectiveness of assistive technology in improving the safety of people with dementia: A systematic review and meta-analysis. Aging Ment. Health 2019, 23, 942–951. [Google Scholar] [CrossRef]
- Wu, X.; Zheng, Y.; Chu, C.H.; Cheng, L.; Kim, J. Applying deep learning technology for automatic fall detection using mobile sensors. Biomed. Signal Process. Control. 2022, 72, 103355. [Google Scholar] [CrossRef]
- Chowdhury, M.E.; Khandakar, A.; Alzoubi, K.; Mohammed, A.; Taha, S.; Omar, A.; Reaz, M.B.I. Wearable Real-Time Epileptic Seizure Detection and Warning System. In Biomedical Signals Based Computer-Aided Diagnosis for Neurological Disorders; Springer: Cham, Switzerland, 2022; pp. 233–265. [Google Scholar]
- Vieluf, S.; Reinsberger, C.; El Atrache, R.; Jackson, M.; Schubach, S.; Ufongene, C.; Meisel, C. Autonomic nervous system changes detected with peripheral sensors in the setting of epileptic seizures. Sci. Rep. 2020, 10, 11560. [Google Scholar] [CrossRef]
- Chen, F.; Chen, I.; Zafar, M.; Sinha, S.R.; Hu, X. Seizures detection using multimodal signals: A scoping review. Physiol. Meas. 2022, 43, 07TR01. [Google Scholar] [CrossRef]
- Kristoffersson, A.; Lindén, M. A Systematic Review of Wearable Sensors for Monitoring Physical Activity. Sensors 2022, 22, 573. [Google Scholar] [CrossRef]
- Mughal, H.; Javed, A.R.; Rizwan, M.; Almadhor, A.S.; Kryvinska, N. Parkinson’s Disease Management Via Wearable Sensors: A Systematic Review. IEEE Access 2022, 10, 35219–35237. [Google Scholar] [CrossRef]
- Sica, M.; Tedesco, S.; Crowe, C.; Kenny, L.; Moore, K.; Timmons, S.; Komaris, D.S. Continuous home monitoring of Parkinson’s disease using inertial sensors: A systematic review. PLoS ONE 2021, 16, e0246528. [Google Scholar] [CrossRef] [PubMed]
- Celik, Y.; Stuart, S.; Woo, W.L.; Godfrey, A. Gait analysis in neurological populations: Progression in the use of wearables. Med. Eng. Phys. 2021, 87, 9–29. [Google Scholar] [CrossRef] [PubMed]
- Albán-Cadena, A.C.; Villalba-Meneses, F.; Pila-Varela, K.O.; Moreno-Calvo, A.; Villalba-Meneses, C.P.; Almeida-Galárraga, D.A. Wearable sensors in the diagnosis and study of Parkinson’s disease symptoms: A systematic review. J. Med. Eng. Technol. 2021, 45, 532–545. [Google Scholar] [CrossRef]
- Storm, F.A.; Cesareo, A.; Reni, G.; Biffi, E. Wearable inertial sensors to assess gait during the 6-minute walk test: A systematic review. Sensors 2020, 20, 2660. [Google Scholar] [CrossRef]
- Zampogna, A.; Mileti, I.; Palermo, E.; Celletti, C.; Paoloni, M.; Manoni, A.; Suppa, A. Fifteen years of wireless sensors for balance assessment in neurological disorders. Sensors 2020, 20, 3247. [Google Scholar] [CrossRef]
- Rehman, R.Z.U.; Zhou, Y.; del Din, S.; Alcock, L.; Hansen, C.; Guan, Y.; Lamoth, C.J. Gait analysis with wearables can accurately classify fallers from non-fallers: A step toward better management of neurological disorders. Sensors 2020, 20, 6992. [Google Scholar] [CrossRef]
- Godoi, B.B.; Amorim, G.D.; Quiroga, D.G.; Holanda, V.M.; Júlio, T.; Tournier, M.B. Parkinson’s disease and wearable devices, new perspectives for a public health issue: An integrative literature review. Rev. Assoc. Médica Bras. 2019, 65, 1413–1420. [Google Scholar] [CrossRef]
- Chirra, M.; Marsili, L.; Wattley, L.; Sokol, L.L.; Keeling, E.; Maule, S.; Merola, A. Telemedicine in neurological disorders: Opportunities and challenges. Telemed. e-Health 2019, 25, 541–550. [Google Scholar] [CrossRef]
- Brognara, L.; Palumbo, P.; Grimm, B.; Palmerini, L. Assessing gait in Parkinson’s disease using wearable motion sensors: A systematic review. Diseases 2019, 7, 18. [Google Scholar] [CrossRef]
- Rovini, E.; Maremmani, C.; Cavallo, F. Automated systems based on wearable sensors for the management of Parkinson’s disease at home: A systematic review. Telemed. e-Health 2019, 25, 167–183. [Google Scholar] [CrossRef] [PubMed]
- Díaz, S.; Stephenson, J.B.; Labrador, M.A. Use of wearable sensor technology in gait, balance, and range of motion analysis. Appl. Sci. 2019, 10, 234. [Google Scholar] [CrossRef]
- Porciuncula, F.; Roto, A.V.; Kumar, D.; Davis, I.; Roy, S.; Walsh, C.J.; Awad, L.N. Wearable movement sensors for rehabilitation: A focused review of technological and clinical advances. Pm&r 2018, 10, S220–S232. [Google Scholar]
- Silva de Lima, A.L.; Evers, L.J.; Hahn, T.; Bataille, L.; Hamilton, J.L.; Little, M.A.; Faber, M.J. Freezing of gait and fall detection in Parkinson’s disease using wearable sensors: A systematic review. J. Neurol. 2017, 264, 1642–1654. [Google Scholar] [CrossRef] [PubMed]
- Vienne, A.; Barrois, R.P.; Buffat, S.; Ricard, D.; Vidal, P.P. Inertial sensors to assess gait quality in patients with neurological disorders: A systematic review of technical and analytical challenges. Front. Psychol. 2017, 8, 817. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Markopoulos, P.; Yu, B.; Chen, W.; Timmermans, A. Interactive wearable systems for upper body rehabilitation: A systematic review. J. Neuroeng. Rehabil. 2017, 14, 20. [Google Scholar] [CrossRef]
- Giggins, O.M.; Clay, I.; Walsh, L. Physical activity monitoring in patients with neurological disorders: A review of novel body-worn devices. Digit. Biomark. 2017, 1, 14–42. [Google Scholar] [CrossRef]
- Hubble, R.P.; Naughton, G.A.; Silburn, P.A.; Cole, M.H. Wearable sensor use for assessing standing balance and walking stability in people with Parkinson’s disease: A systematic review. PLoS ONE 2015, 10, e0123705. [Google Scholar] [CrossRef]
- Oung, Q.W.; Hariharan, M.; Basah, S.N.; Yaacob, S.; Sarillee, M.; Lee, H.L. Use of technological tools for Parkinson’s disease early detection: A review. In Proceedings of the 2014 IEEE International Conference on Control System, Computing and Engineering (ICCSCE 2014), Penang, Malaysia, 28–30 November 2014; IEEE: Piscataway, NJ, USA, 2014; pp. 343–348. [Google Scholar]
- Steins, D.; Dawes, H.; Esser, P.; Collett, J. Wearable accelerometry-based technology capable of assessing functional activities in neurological populations in community settings: A systematic review. J. Neuroeng. Rehabil. 2014, 11, 36. [Google Scholar] [CrossRef]
- Stavropoulos, T.G.; Papastergiou, A.; Mpaltadoros, L.; Nikolopoulos, S.; Kompatsiaris, I. IoT wearable sensors and devices in elderly care: A literature review. Sensors 2020, 20, 2826. [Google Scholar] [CrossRef] [PubMed]
- Pasluosta, C.F.; Gassner, H.; Winkler, J.; Klucken, J.; Eskofier, B.M. An emerging era in the management of Parkinson’s disease: Wearable technologies and the internet of things. IEEE J. Biomed. Health Inform. 2015, 19, 1873–1881. [Google Scholar] [CrossRef]
- Tăuţan, A.M.; Ionescu, B.; Santarnecchi, E. Artificial intelligence in neurodegenerative diseases: A review of available tools with a focus on machine learning techniques. Artif. Intell. Med. 2021, 117, 102081. [Google Scholar] [CrossRef] [PubMed]
- Ghannam, R.; Curia, G.; Brante, G.; Fan, H.; Heidari, H. Wearable electronics for neurological applications: A review of undergraduate engineering programmes. In Proceedings of the 2020 Transnational Engineering Education Using Technology (TREET), Glasgow, UK, 31 July 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 1–4. [Google Scholar]
- Buckley, C.; Alcock, L.; McArdle, R.; Rehman, R.Z.U.; del Din, S.; Mazzà, C.; Rochester, L. The role of movement analysis in diagnosing and monitoring neurodegenerative conditions: Insights from gait and postural control. Brain Sci. 2019, 9, 34. [Google Scholar] [CrossRef] [PubMed]
- Belić, M.; Bobić, V.; Badža, M.; Šolaja, N.; Đurić-Jovičić, M.; Kostić, V.S. Artificial intelligence for assisting diagnostics and assessment of Parkinson’s disease—A review. Clin. Neurol. Neurosurg. 2019, 184, 105442. [Google Scholar] [CrossRef]
- Sivathamboo, S.; Nhu, D.; Piccenna, L.; Yang, A.; Antonic-Baker, A.; Vishwanath, S.; Kwan, P. Preferences and User Experiences of Wearable Devices in Epilepsy: A Systematic Review and Mixed-Methods Synthesis. Neurology 2022, 99, e1380–e1392. [Google Scholar] [CrossRef]
- Olsen, L.S.; Nielsen, J.M.; Simonÿ, C.; Kjær, T.W.; Beck, M. Wearables in real life: A qualitative study of experiences of people with epilepsy who use home seizure monitoring devices. Epilepsy Behav. 2021, 125, 108398. [Google Scholar] [CrossRef]
- Rukasha, T.; Woolley, S.I.; Kyriacou, T.; Collins, T. Evaluation of wearable electronics for epilepsy: A systematic review. Electronics 2020, 9, 968. [Google Scholar] [CrossRef]
- Simblett, S.K.; Biondi, A.; Bruno, E.; Ballard, D.; Stoneman, A.; Lees, S.; Wykes, T. Patients’ experience of wearing multimodal sensor devices intended to detect epileptic seizures: A qualitative analysis. Epilepsy Behav. 2020, 102, 106717. [Google Scholar] [CrossRef]
- Johansson, D.; Malmgren, K.; Alt Murphy, M. Wearable sensors for clinical applications in epilepsy, Parkinson’s disease, and stroke: A mixed-methods systematic review. J. Neurol. 2018, 265, 1740–1752. [Google Scholar] [CrossRef]
- Ryvlin, P.; Ciumas, C.; Wisniewski, I.; Beniczky, S. Wearable devices for sudden unexpected death in epilepsy prevention. Epilepsia 2018, 59, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Naganur, V.; Sivathamboo, S.; Chen, Z.; Kusmakar, S.; Antonic-Baker, A.; O’Brien, T.J.; Kwan, P. Automated seizure detection with non-invasive wearable devices: A systematic review and meta-analysis. Epilepsia 2022, 63, 1930–1941. [Google Scholar] [CrossRef] [PubMed]
- Ong, J.S.; Wong, S.N.; Arulsamy, A.; Watterson, J.L.; Shaikh, M. Medical Technology: A Systematic Review on Medical Devices Utilized for Epilepsy Prediction and Management. Curr. Neuropharmacol. 2022, 20, 950–964. [Google Scholar] [CrossRef] [PubMed]
- Cullen, A.; Mazhar, M.K.A.; Smith, M.D.; Lithander, F.E.; Ó Breasail, M.; Henderson, E.J. Wearable and Portable GPS Solutions for Monitoring Mobility in Dementia: A Systematic Review. Sensors 2022, 22, 3336. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, J.M.; Rades, D.; Kjaer, T.W. Wearable electroencephalography for ultra-long-term seizure monitoring: A systematic review and future prospects. Expert Rev. Med. Devices 2021, 18 (Suppl. 1), 57–67. [Google Scholar] [CrossRef]
- Beniczky, S.; Wiebe, S.; Jeppesen, J.; Tatum, W.O.; Brazdil, M.; Wang, Y.; Ryvlin, P. Automated seizure detection using wearable devices: A clinical practice guideline of the International League Against Epilepsy and the International Federation of Clinical Neurophysiology. Clin. Neurophysiol. 2021, 132, 1173–1184. [Google Scholar] [CrossRef]
- Shum, J.; Friedman, D. Commercially available seizure detection devices: A systematic review. J. Neurol. Sci. 2021, 428, 117611. [Google Scholar] [CrossRef]
- Breasail, M.Ó.; Biswas, B.; Smith, M.D.; Mazhar, M.K.A.; Tenison, E.; Cullen, A.; Henderson, E.J. Wearable GPS and Accelerometer Technologies for Monitoring Mobility and Physical Activity in Neurodegenerative Disorders: A Systematic Review. Sensors 2021, 21, 8261. [Google Scholar] [CrossRef]
- De la Fuente García, S.; Ritchie, C.W.; Luz, S. Artificial intelligence, speech, and language processing approaches to monitoring Alzheimer’s disease: A systematic review. J. Alzheimer’s Dis. 2022, 78, 1547–1574. [Google Scholar] [CrossRef]
- Machado, S.D.; Barbosa, J.L.V. Technologies applied in the care of patients with Alzheimer’s disease: A systematic review. In Proceedings of the Brazilian Symposium on Multimedia and the Web, New York, NY, USA, 7–11 November 2022; pp. 29–32. [Google Scholar]
- Gillani, N.; Arslan, T. Intelligent sensing technologies for the diagnosis, monitoring and therapy of alzheimer’s disease: A systematic review. Sensors 2021, 21, 4249. [Google Scholar] [CrossRef]
- Anderson, M.S.; Homdee, N.; Bankole, A.; Alam, R.; Mitchell, B.; Hayes, J.; Lach, J. Behavioral interventions for Alzheimer’s management using technology: Home-based monitoring. Curr. Geriatr. Rep. 2020, 9, 90–100. [Google Scholar] [CrossRef]
- Bruno, E.; Biondi, A.; Böttcher, S.; Lees, S.; Schulze-Bonhage, A.; Richardson, M.P.; RADAR-CNS Consortium. Day and night comfort and stability on the body of four wearable devices for seizure detection: A direct user-experience. Epilepsy Behav. 2020, 112, 107478. [Google Scholar] [CrossRef] [PubMed]
- Vinals, L.; Akinola, T.; Sarri, G. Pnd93 what good are digital technologies in Alzheimer’s disease research?—A systematic literature review. Value Health 2019, 22, S754. [Google Scholar] [CrossRef]
- Kurada, A.V.; Srinivasan, T.; Hammond, S.; Ulate-Campos, A.; Bidwell, J. Seizure detection devices for use in antiseizure medication clinical trials: A systematic review. Seizure 2019, 66, 61–69. [Google Scholar] [CrossRef]
- Klimova, B.; Valis, M.; Kuca, K. Exploring assistive technology as a potential beneficial intervention tool for people with Alzheimer’s disease—A systematic review. Neuropsychiatr. Dis. Treat. 2018, 14, 3151. [Google Scholar] [CrossRef]
- Ienca, M.; Fabrice, J.; Elger, B.; Caon, M.; Scoccia Pappagallo, A.; Kressig, R.W.; Wangmo, T. Intelligent assistive technology for Alzheimer’s disease and other dementias: A systematic review. J. Alzheimer’s Dis. 2017, 56, 1301–1340. [Google Scholar] [CrossRef] [PubMed]
- Brereton, P.; Kitchenham, B.A.; Budgen, D.; Turner, M.; Khalil, M. Lessons from applying the systematic literature review process within the software engineering domain. J. Syst. Softw. 2017, 80, 571–583. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Moher, D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 372. [Google Scholar] [CrossRef]
- Apple Watch Series 7—Apple. Available online: https://www.apple.com/apple-watch-series-7/ (accessed on 15 May 2022).
- Watchseniors—Smartwatch GPS Para La Tercera Edad. Available online: https://watchseniors.com (accessed on 15 May 2022).
- FallSafety Home—iPhone, Android, & Apple Watch Fall Detection. Available online: https://fallsafetyapp.com/fallsafety-home (accessed on 14 May 2022).
- FallSkip Scientific Basis—Technology for Fall Risk Evaluation in Older Adults. Available online: https://fallskip.com/en/fallskip-scientific-basis/ (accessed on 16 May 2022).
- Neki—Solutions and GPS Devices for the Security of Your Family. Available online: https://www.nekiglobal.com (accessed on 16 May 2022).
- Alexa Together. Available online: https://www.amazon.com/Alexa-Together/b?ie=UTF8&node=21390531011 (accessed on 14 May 2022).
- MyNotifi. Available online: https://www.mynotifi.com (accessed on 29 March 2022).
- VirtuSense Technologies|Fall Prevention and RPM with AI. Available online: https://www.virtusense.ai (accessed on 17 May 2022).
- Emma Watch: A Device to Ease Tremors. Available online: https://parkinsonsdisease.net/news/emma-watch-wearable-device-tremors (accessed on 29 March 2022).
- How RPM Works|Global Kinetics. Available online: https://pkgcare.com/healthcare-professionals/how-it-works/ (accessed on 29 March 2022).
- Parkinson Smartwatch—Parkinson Smartwatch. Available online: https://parkinsonsmartwatch.com/en/ (accessed on 11 May 2022).
- Essential Tremor Glove|Hand Tremor Devices—Steadiwear Inc. Available online: https://steadiwear.com/?_atid=KHPdPvqWHDNFddV1UcSTePmtuyiIbl (accessed on 12 May 2022).
- Certified Medical Class 2a Hand Therapeutic Tremor Device—Vilim Ball. Available online: https://www.vilim.lt/en/1630-2/ (accessed on 13 May 2022).
- Hand Tremor Device for Essential Tremor by Five Microns. Available online: https://fivemicrons.com/?gclid=Cj0KCQjw3IqSBhCoARIsAMBkTb1P2xnOz9ViAqYXGuwTL2OS_Tn0JFzimtP_OOjcN0VQ20E_HkBD0B4aAmF6EALw_wcB (accessed on 29 March 2022).
- Gyenno Spoon. Available online: https://www.gyenno.com/spoon-en (accessed on 29 March 2022).
- Parkinson’s KinetiGraph (PKG)|Dementech Neurosciences. Available online: https://dementech.com/parkinsons-kinetigraph-pkg/ (accessed on 11 May 2022).
- Essential Tremor Bracelet—Wrist Device for Tremors—Cala Trio. Available online: https://calatrio.com (accessed on 12 May 2022).
- Movement Monitor|Epi USA. Available online: https://www.epiusa.net/movement-monitor (accessed on 29 March 2022).
- Commercial Care Systems. Available online: https://www.medpage-ltd.com/epilepsy/epilepsy-commercial-care-systems (accessed on 29 March 2022).
- EpiUSA. Emfit Movement Monitor Epilepsy Seizure Alarm, United States and Canada. Available online: https://www.epiusa.net/ (accessed on 29 March 2022).
- Embrace2 Seizure Monitoring|Smarter Epilepsy Management|Embrace Watch|Empatica. Available online: https://www.empatica.com/en-eu/embrace2/ (accessed on 29 March 2022).
- Standard SAMi-3 Kit (US and Canada) — SAMi: The Sleep Activity Monitor. Available online: https://www.samialert.com (accessed on 29 March 2022).
- Pulliam, C.L.; Heldman, D.A.; Brokaw, E.B.; Mera, T.O.; Mari, Z.K.; Burack, M.A. Continuous assessment of levodopa response in Parkinson’s disease using wearable motion sensors. IEEE Trans. Biomed. Eng. 2017, 65, 159–164. [Google Scholar] [CrossRef]
- Greene, B.R.; Caulfield, B.; Lamichhane, D.; Bond, W.; Svendsen, J.; Zurski, C.; Pratt, D. Longitudinal assessment of falls in patients with Parkinson’s disease using inertial sensors and the Timed Up and Go test. J. Rehabil. Assist. Technol. Eng. 2018, 5, 2055668317750811. [Google Scholar] [CrossRef] [PubMed]
- Daneault, J.F.; Vergara-Diaz, G.; Parisi, F.; Admati, C.; Alfonso, C.; Bertoli, M.; Bonato, P. Accelerometer data collected with a minimum set of wearable sensors from subjects with Parkinson’s disease. Sci. Data 2021, 8, 48. [Google Scholar] [CrossRef]
- Marcante, A.; di Marco, R.; Gentile, G.; Pellicano, C.; Assogna, F.; Pontieri, F.E.; Antonini, A. Foot pressure wearable sensors for freezing of gait detection in Parkinson’s disease. Sensors 2022, 21, 128. [Google Scholar] [CrossRef] [PubMed]
- Huo, W.; Angeles, P.; Tai, Y.F.; Pavese, N.; Wilson, S.; Hu, M.T.; Vaidyanathan, R. A heterogeneous sensing suite for multisymptom quantification of Parkinson’s disease. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 1397–1406. [Google Scholar] [CrossRef] [PubMed]
- Vergara-Diaz, G.; Daneault, J.F.; Parisi, F.; Admati, C.; Alfonso, C.; Bertoli, M.; Bonato, P. Limb and trunk accelerometer data collected with wearable sensors from subjects with Parkinson’s disease. Sci. Data 2021, 8, 47. [Google Scholar] [CrossRef]
- Raiano, L.; di Pino, G.; di Biase, L.; Tombini, M.; Tagliamonte, N.L.; Formica, D. PDMeter: A Wrist Wearable Device for an at-home Assessment of the Parkinson’s Disease Rigidity. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 1325–1333. [Google Scholar] [CrossRef] [PubMed]
- Ileșan, R.R.; Cordoș, C.G.; Mihăilă, L.I.; Fleșar, R.; Popescu, A.S.; Perju-Dumbravă, L.; Faragó, P. Proof of Concept in Artificial-Intelligence-Based Wearable Gait Monitoring for Parkinson’s Disease Management Optimization. Biosensors 2020, 12, 189. [Google Scholar] [CrossRef]
- Stuart, S.; Godfrey, A.; Mancini, M. Staying UpRight in Parkinson’s disease: A pilot study of a novel wearable postural intervention. Gait Posture 2022, 91, 86–93. [Google Scholar] [CrossRef]
- Dang, Q.K.; Seo, H.G.; Pham, D.D.; Chee, Y. Wearable sensor based stooped posture estimation in simulated Parkinson’s disease gaits. Sensors 2019, 19, 223. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; El Atrache, R.; Yu, S.; Asif, U.; Jackson, M.; Roy, S.; Loddenkemper, T. Seizure detection using wearable sensors and machine learning: Setting a benchmark. Epilepsia 2021, 62, 1807–1819. [Google Scholar] [CrossRef]
- Jeppesen, J.; Fuglsang-Frederiksen, A.; Johansen, P.; Christensen, J.; Wüstenhagen, S.; Tankisi, H.; Beniczky, S. Seizure detection based on heart rate variability using a wearable electrocardiography device. Epilepsia 2019, 60, 2105–2113. [Google Scholar] [CrossRef]
- Johansson, D.; Ohlsson, F.; Krýsl, D.; Rydenhag, B.; Czarnecki, M.; Gustafsson, N.; Malmgren, K. Tonic-clonic seizure detection using accelerometry-based wearable sensors: A prospective, video-EEG controlled study. Seizure 2019, 65, 48–54. [Google Scholar] [CrossRef]
- Dong, C.; Ye, T.; Long, X.; Aarts, R.M.; van Dijk, J.P.; Shang, C.; Wang, Y. A Two-Layer Ensemble Method for Detecting Epileptic Seizures Using a Self-Annotation Bracelet with Motor Sensors. IEEE Trans. Instrum. Meas. 2022, 71, 164. [Google Scholar] [CrossRef]
- Ertuğrul, Ö.F.; Sönmez, Y.; Sezgin, N.; Eşref, A.K.I.L. Assessment of Epileptic Seizures and Non-Epileptic Seizures via Wearable Sensors and Priori Detection of Epileptic Seizures. Balk. J. Electr. Comput. Eng. 2022, 10, 150–155. [Google Scholar] [CrossRef]
- Nielsen, J.M.; Zibrandtsen, I.C.; Masulli, P.; Sørensen, T.L.; Andersen, T.S.; Kjær, T.W. Towards a wearable multi-modal seizure detection system in epilepsy: A pilot study. Clin. Neurophysiol. 2022, 136, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Kusmakar, S.; Karmakar, C.K.; Yan, B.; O’Brien, T.J.; Muthuganapathy, R.; Palaniswami, M. Automated detection of convulsive seizures using a single wrist-worn accelerometer device. IEEE Trans. Biomed. Eng. Submitt. 2019, 66, 421–432. [Google Scholar] [CrossRef]
- Halimeh, M.; Yang, Y.; Sheehan, T.; Vieluf, S.; Jackson, M.; Loddenkemper, T.; Meisel, C. Wearable device assessments of antiseizure medication effects on diurnal patterns of electrodermal activity, heart rate, and heart rate variability. Epilepsy Behav. 2022, 129, 108635. [Google Scholar] [CrossRef]
- Japaridze, G.; Loeckx, D.; Buckinx, T.; Armand Larsen, S.; Proost, R.; Jansen, K.; Beniczky, S. Automated detection of absence seizures using a wearable electroencephalographic device: A phase 3 validation study and feasibility of automated behavioral testing. Epilepsia 2022, 1–7. [Google Scholar] [CrossRef]
- Cogan, D.; Birjandtalab, J.; Nourani, M.; Harvey, J.; Nagaraddi, V. Multi-biosignal analysis for epileptic seizure monitoring. Int. J. Neural Syst. 2017, 27, 1650031. [Google Scholar] [CrossRef]
- Varatharajan, R.; Manogaran, G.; Priyan, M.K.; Sundarasekar, R. Wearable sensor devices for early detection of Alzheimer disease using dynamic time warping algorithm. Clust. Comput. 2018, 21, 681–690. [Google Scholar] [CrossRef]
- Perez-Valero, E.; Lopez-Gordo, M.Á.; Gutiérrez, C.M.; Carrera-Muñoz, I.; Vílchez-Carrillo, R.M. A Self-driven Approach for Multi-class Discrimination in Alzheimer’s Disease Based on Wearable EEG. Comput. Methods Programs Biomed. 2022, 220, 106841. [Google Scholar] [CrossRef]
- Godfrey, A.; Brodie, M.; van Schooten, K.S.; Nouredanesh, M.; Stuart, S.; Robinson, L. Inertial wearables as pragmatic tools in dementia. Maturitas 2019, 127, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Roopaei, M.; Rad, P.; Prevost, J.J. A wearable IoT with complex artificial perception embedding for Alzheimer patients. In Proceedings of the 2018 World Automation Congress (WAC), Stevenson, WA, USA, 3–6 June 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 1–6. [Google Scholar]
- Goel, I.; Kumar, D. Design and implementation of android based wearable smart locator band for people with autism, dementia, and Alzheimer. Adv. Electron. 2015, 2015, 8. [Google Scholar] [CrossRef]
- Pontoriero, A.D.; Charlton, P.H.; Alastruey, J. Alzheimer’s disease: A step towards prognosis using smart wearables. Proceedings 2019, 4, 8. [Google Scholar]
- Hsu, Y.L.; Chung, P.C.; Wang, W.H.; Pai, M.C.; Wang, C.Y.; Lin, C.W.; Wang, J.S. Gait and balance analysis for patients with Alzheimer’s disease using an inertial-sensor-based wearable instrument. IEEE J. Biomed. Health Inform. 2014, 18, 1822–1830. [Google Scholar] [CrossRef] [PubMed]
- Costa, L.; Gago, M.F.; Yelshyna, D.; Ferreira, J.; David Silva, H.; Rocha, L.; Bicho, E. Application of machine learning in postural control kinematics for the diagnosis of Alzheimer’s disease. Comput. Intell. Neurosci. 2016, 2016, 3891253. [Google Scholar] [CrossRef]






| Research Question (RQ) | Question | Motivation |
|---|---|---|
| 1 | Which are commercial wearables for monitoring NDD-related motor impairments currently available? | To identify the main commercial wearables for monitoring NDD-related motor impairments currently available. |
| 2 | Which are the top most used commercial wearables for monitoring motor impairment in patients with NDDs? | To identify the top most used commercial wearables for monitoring motor impairment in patients with NDDs. |
| 3 | Which are the technical characteristics of non-commercial wearables for monitoring NDD-related motor impairments currently available? | To identify the technical characteristics of non-commercial wearables for monitoring NDD-related motor impairments currently available. |
| 4 | Which are the FDA status of commercial wearables for monitoring NDD-related motor impairments currently available? | To determine if the patient can confidently use the commercial wearables for monitoring NDD-related motor impairments currently available. |
| 5 | What are the gaps in the monitoring of NDDs using commercial wearables devices? How are these gaps covered by non-commercial wearables devices? | To identify the areas of opportunity that must be strengthened in commercial wearables devices. |
| Area | Keywords | Related Concepts |
|---|---|---|
| Neurodegenerative Disease | Motor impairments | Falls |
| Mental health | Wearables and sensors devices | Tremor |
| Seizures | ||
| Parkinson | ||
| Epileptic | ||
| Alzheimer |
| Category | |
|---|---|
| Information Technologies | Healthcare |
| Google Scholar, Hindawi, IEEE Xplore, IOP science, JACC, MDPI, Nature, Science Direct, Springer Link, and Wiley Online Library. | AHA Journals, Annual Reviews, BioMed Central, Clinical Trials, JMIR, and PubMed |
| Motor Disability | Device Type | Device Brand | Device Model | Monitoring Features | Sensors Used | FDA Status/Year/AP (AP: Accuracy Percentage) | Android Compatibility |
|---|---|---|---|---|---|---|---|
| Falls | Smartwatch | Apple | Watch Series 7 [87] | Detect user idleness for about a minute. It begins a 30-s countdown while tapping you on the wrist and sounding an alert. | Blood oxygen, electric HR, optical HR, GPS, compass, microphone, altimeter, and horn. | Approved/2018 /98%/(Only for ECG) | No |
| Smartwatch | Watchseniors | Plus 4 G [88] | Detect falls, trajectories, and user location. | Blood pressure sensor, temperature sensor, and heart rate sensor | Unknown | Yes | |
| Smart Phone | Freeus | FallSafety [89] | Detect user falls with automatic generation of alerts to the emergency systems. | Information not available | Unknown | Yes | |
| Belt | Fallskip | TF11-MP005-ES [90] | Assess the risk of falling in older adults. | IMU (Inertial Measurement Unit) | Unknown/Unknow/75% | No | |
| Pendant pager | Neki | Nock Senior [91] | Fall detector with GPS locator monitorable with its application on the cell phone. | Fall detector sensor | Unknown | Yes | |
| Static voice-enabled device | Amazon | Alexa together [92] | Virtual assistant equipped with functions that help the user in case of falls. | Speech processor | Unknown | Yes | |
| Wristband | MyNotifi® | MYNOTIFI FALL DETECTION SYSTEM [93] | Detect falls and alert the user’s family and friends if a fall occurs. | AI sensor | Class I (Exempt)/2020/73% | Yes | |
| Vision system in Bedside | VIRTUSENSETM | VSTOne [94] | Predict a crash around 30–65 s before it occurs. | AI and LiDAR sensors | Unknown/Unknown/98% | No | |
| Tremor | Smartwatch | Microsoft | Emma Watch [95] | Reduce tremors associated with Parkinson’s disease. | Movement is regulated by a sensorimotor feedback loop involving the perception of movement and position of the body. | Unknown | No |
| Smartwatch | Detekt | PKG watch (The Parkinson’s KinetiGraph) [96] | Analyze user movements throughout the day and output a graph that allows the doctor to analyze and compare user movement speed and overall user capability to move throughout the day. | Gyroscopic stabilization | 510(k) Cleared/2014/96% | No | |
| Smartwatch | Parkinson Smartwatch | Parkinson Smartwatch [97] | User (i.e., patient) manually records information on their perception of well-being during the day (for example, after taking their medication). The information that is recorded on the device is sent to the cloud, where it is stored. The user and their doctor have online access to the graphs of the data recorded from anywhere in the world using a computer, tablet, or mobile phone. | Information not available | Unknown | No | |
| Glove | Steadiwear | Steadi-Two [98] | Reduce tremor magnitude using two magnets to control a disk that moves in the opposite direction of the tremor. | The technology is based on a seismic design and works similarly to a see-saw in a park. The disk, which is controlled by magnets, responds to the tremor by providing an equal and opposite force, lowering its magnitude. | Class I/2021/80% | No | |
| Handheld Therapeutic device | VILIM | VILIM ball [99] | Reduces the hand tremors of the patient while performing daily tasks. | Embedded algorithm that analyzes tremors and adapts to each patient’s symptoms individually. | Unknown | Yes | |
| Hand Tremor Device | Five Microns® | Tremelo [100] | Reduces intermediate-degree tremors in the arms and hands by 85 to 90%. | Non-invasive and mechanical (no electricity: no batteries) device relying on vibration absorbers and tuned mass damper. | Class 1/Unknown/90% | No | |
| Spoon | GYENNO | GYENNO SPOON [101] | Stabilize unwanted tremors by 85% to stop intentional hand movement and help people with PD or tremors to eat more easily. | Intelligent rehabilitation robotics, Intelligent high-speed servo control system, algorithm technology of unmanned aerial vehicles, and self-adapted ML. | Unknown | Yes | |
| Wristband | Parkinson’s KinetiGraph (PKG) | PKGTM [102] | Collect data on motor disabilities and other complications caused by PD (e.g., slowness of movement, tremor, stiffness). | Sensors that monitor the wearer’s activity and buzzes for medication reminders. | Cleared/Unknown/Unknown | No | |
| Wristband | The Cala Trio therapy | Cala Trio™ [103] | Deliver electrical stimulation—also known as neuromodulation—to the nerves in the effective wrist. The stimulation disrupts the tremor network in the brain and delivers meaningful tremor reduction in the affected hand. | Information not available | Cleared Class II /2020/68% | No | |
| Seizures | Bed | EpiUSA | Emfit Movement Monitor [104] | Nightly monitoring of a person’s movements to alert their caregivers if necessary. | Motion sensor installed in a pad, which is installed under the patient’s mattress. | Unknown | No |
| Bed | MedPage | BMA-01 [105] | Detect certain types of movements (e.g., muscular spasms) that people make while sleeping using a movement-sensing alarm. | Sophisticated software algorithms that continually analyze the signals produced by a special sensor positioned under the bed mattress, even a memory foam type. | Unknown | No | |
| Bed | Epi USA | Emfit [106] | Detect most movements, including light movements in patients with epileptic disease. The company states that this product is also suitable for small children. | Flexible and durable bed sensor, a bedside monitor, a bed clip, and a wall bracket. The movement monitor detects movement over a preset amount of time and triggers an alarm if a person moves more than it expects. | Unknown | No | |
| Bracelet | Empatica | Embrace 2 [107] | Detect seizures | Information not available | FDA cleared/2018/98% | Yes | |
| Video monitor | SAMi | SAMi-3 [108] | Process and record patient movements in real-time. Send alerts to caregivers in case of patient seizures. | Information not available | Unknown | Yes |
| NDD Type | Device Type | Research Description | Sensors or Technology Used | Real-Time Monitoring |
|---|---|---|---|---|
| Parkinson | Bracelet (2017) | Use wearable sensors to quantify doses in patients with PD to address motor affections such as tremors, bradykinesia, and dyskinesia [109]. | Wrist and ankle motion sensors | Yes |
| Parkinson | Bracelet (2018) | Evaluate a fall prediction test using body sensors in patients with PD [110]. | Inertial sensor and software system (Kinesis QTUG™, Kinesis Health Technologies, Dublin, Ireland) | Yes |
| Parkinson | Bracelet and Belt (2021) | Evaluate motor disabilities in patients with PD [111]. | Accelerometer | Yes |
| Parkinson | Shoe accessory (2020) | Using a 3D accelerometer, they validated a pair of pressure insoles in shoes to detect walking problems in patients with PD [112]. | Accelerometer 3D and pressure insoles | Yes |
| Parkinson | Armband | Propose a wearable device for the diagnosis of motor affections such as rigidity, tremor, and bradykinesia in patients with PD [113]. | Sensor system composed of a force sensor, three inertial measurement units (IMUs), and four custom mechanomyography (MMG) sensors | Yes |
| Parkinson | Bracelet and Belt (2021) | Evaluate the data obtained from a group of patients with PD by means of wearable sensors to quantify the severity of symptoms in the extremities of the patients [114]. | Accelerometer | Yes |
| Parkinson | Wrist (2020) | Validate a mechatronic wearable device that seeks to mitigate wrist stiffness in patients affected by PD [115]. | One actuated joint and four passive revolute joints with a high overall intrinsic back drivability. | Yes |
| Parkinson | Shoe accessory and Belt (2022) | Monitor and evaluate gait in patients with PD through a portable physiograph [116]. | Pressure sensors, electromyography (EMG) sensors, and accelerometers. | Yes |
| Parkinson | Device on the back (2022) | Evaluate the performance of a device to monitor and improve postural alignment, balance, and gait in patients with PD [117]. | Device Up Right Go | Yes |
| Parkinson | Device on the neck and back (2019) | Propose a method to estimate stooped posture through sensors (i.e., accelerometers) mounted on the patient’s neck or upper back [118]. | Accelerometer | Yes |
| Epileptic | Bracelet (2021) | Evaluate the performance of the bracelet in detecting seizures through algorithms implemented with ML using multisignal biosensors worn on the patient’s wrist and ankle [119]. | Wrist- and ankle-worn multisignal biosensors in conjunction with machine learning algorithms (MLAs) | No |
| Epileptic | Chest patch (2019) | Evaluate seizure detection through heart rate variability using a portable electrocardiography device [120]. | Portable Electrocardiogram (ECG) in conjunction with algorithms implemented in LabView | No |
| Epileptic | Wristband (2019) | Evaluate a portable system based on accelerometry to detect tonic–clonic seizures [121]. | Inertial sensors | No |
| Epileptic | Bracelet (2022) | Propose an automated method based on machine learning to classify seizures [122]. | Accelerometer and gyroscope | Yes |
| Epileptic | Bracelet (2022) | Develop a system to detect seizures (epileptic / non-epileptic) using wearable sensors [123]. | Electroencephalography (EEG), Electromyography (EMG), and ECG | Yes |
| Epileptic | Electrodes (2022) | Monitor patients with epilepsy disease to propose effective strategies for seizure detection [124]. | EEG, ECG, and accelerometer | Yes |
| Epileptic | Wrist-Worn (2018) | Develop a wireless monitoring system (with an accelerometer as a sensor) worn on the patient’s wrist for seizure detection [125]. | Accelerometer | Yes |
| Epileptic | Wrist and ankle Bracelet (2022) | Investigate the effects of anticonvulsant medications monitored by a wearable device in patients with epilepsy [126]. | Body temperature sensor, optical, infrared sensors, and a 3D accelerometer and gyroscope. | Yes |
| Epileptic | Diadem (2022) | Evaluate the accuracy of absence seizure detection using an electroencephalographic wearable device [127]. | EEG | No |
| Epileptic | Wrist-Worn and Electrodes (2017) | Develop a wearable system that detects seizures and alerts patient caregivers [128]. | EEG, gyroscope, 3D accelerometer, optical, infrared sensors, and body temperature. | No |
| Alzheimer | Ankle Bracelet (2018) | Evaluate an algorithm to monitor and record gait movements in patients with AD [129]. | Accelerometer and gyroscope | No |
| Alzheimer | Electrodes (2022) | Develop and evaluate a multiclass classification system for AD based on a commercial EEG acquisition system that uses sixteen channels [130]. | EEG | No |
| Alzheimer | Wrist and ankle Bracelet (2019) | Review wearable devices that monitor and control posture and gait in patients with dementia [131]. | Accelerometer and gyroscope | No |
| Alzheimer | Video camera (2018) | Develop a platform to support patients suffering from impaired facial perception with an assistive intelligence device [132]. | Algorithm- Facial Perception Model | No |
| Alzheimer | Wrist band (2015) | They developed a localization band targeted at people suffering from memory diseases [133]. | GPS and global system for mobile (GSM) communication | Yes |
| Alzheimer | Wrist band (2018) | Determine whether characteristics extracted from arterial pulse waves (PWs) measured by wearable sensors could be useful for stratifying patients at risk of AD [134]. | Photoplethysmography (PPG) | No |
| Alzheimer | Feet mounted (2014) | Develop gait and balance analysis algorithms for the diagnosis of patients with AD [135]. | Inertial sensor | No |
| Alzheimer | Belt (2016) | Investigate ML classifiers applied in postural control in patients with AD [136]. | Multiple Layer Perceptrons (MLPs), accelerometer, and gyroscope | No |
| NDD Type | Real-Time Monitoring | Distribution |
|---|---|---|
| Alzheimer’s disease | Yes | 13% |
| No | 87% | |
| Epilepsy | Yes | 50% |
| No | 50% | |
| Parkinson’s disease | Yes | 100% |
| No | 0% |
| NDD Type | Sensor/Technology Used | Usage Percentage |
|---|---|---|
| Parkinson’s disease | Accelerometer | 30% |
| Mechanical joint | 14% | |
| Pressure sensors | 14% | |
| MMG sensors | 7% | |
| EMG | 7% | |
| Force sensor | 7% | |
| Inertial sensor | 7% | |
| Software system | 7% | |
| Wrist and ankle motion | 7% | |
| Epilepsy | Accelerometer | 21% |
| EEG | 21% | |
| Body temperature sensor | 11% | |
| ECG | 11% | |
| Gyroscope | 11% | |
| Biosensors with Machine Learning Algorithms (MLAs) | 5% | |
| EMG | 5% | |
| Inertial sensors | 5% | |
| Infrared sensors | 5% | |
| Optical sensors | 5% | |
| Alzheimer’s disease | Accelerometer | 20% |
| Gyroscope | 20% | |
| MLAs | 20% | |
| EEG | 10% | |
| GPS and GSM | 10% | |
| Inertial sensor | 10% | |
| PPG | 10% |
| Motor Disabilities | FDA Devices | Non-FDA Devices |
|---|---|---|
| Falls | 38% | 62% |
| Tremor | 33% | 67% |
| Seizures | 20% | 80% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prieto-Avalos, G.; Sánchez-Morales, L.N.; Alor-Hernández, G.; Sánchez-Cervantes, J.L. A Review of Commercial and Non-Commercial Wearables Devices for Monitoring Motor Impairments Caused by Neurodegenerative Diseases. Biosensors 2023, 13, 72. https://doi.org/10.3390/bios13010072
Prieto-Avalos G, Sánchez-Morales LN, Alor-Hernández G, Sánchez-Cervantes JL. A Review of Commercial and Non-Commercial Wearables Devices for Monitoring Motor Impairments Caused by Neurodegenerative Diseases. Biosensors. 2023; 13(1):72. https://doi.org/10.3390/bios13010072
Chicago/Turabian StylePrieto-Avalos, Guillermo, Laura Nely Sánchez-Morales, Giner Alor-Hernández, and José Luis Sánchez-Cervantes. 2023. "A Review of Commercial and Non-Commercial Wearables Devices for Monitoring Motor Impairments Caused by Neurodegenerative Diseases" Biosensors 13, no. 1: 72. https://doi.org/10.3390/bios13010072
APA StylePrieto-Avalos, G., Sánchez-Morales, L. N., Alor-Hernández, G., & Sánchez-Cervantes, J. L. (2023). A Review of Commercial and Non-Commercial Wearables Devices for Monitoring Motor Impairments Caused by Neurodegenerative Diseases. Biosensors, 13(1), 72. https://doi.org/10.3390/bios13010072








