Cost-Efficient Micro-Well Array-Based Colorimetric Antibiotic Susceptibility Testing (MacAST) for Bacteria from Culture or Community
Abstract
:1. Introduction
2. Material and Methods
2.1. Preparation of Bacterial Strains
2.2. Design of Micro-Well Array Chip
2.3. Antibiotic Susceptibility Testing in the Micro-Well Array Chip
2.4. Cell Separation and Enrichment from Wastewater Samples
2.5. Antibiotic Susceptibility Testing of the Captured Bacteria from Community
3. Results and Discussion
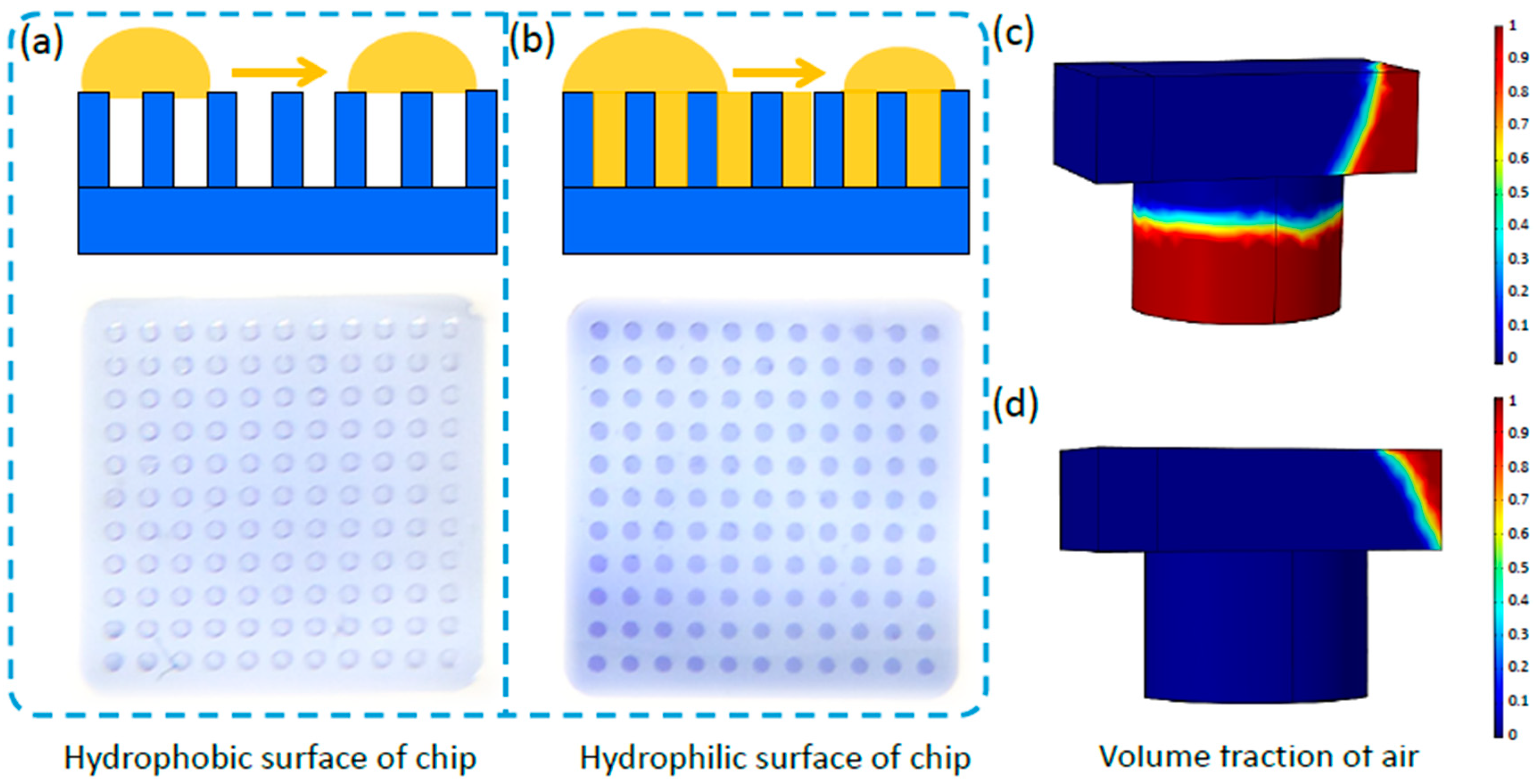
3.1. Simulation of a 3D-Printed Micro-Well Array Chip with Trapped Droplets
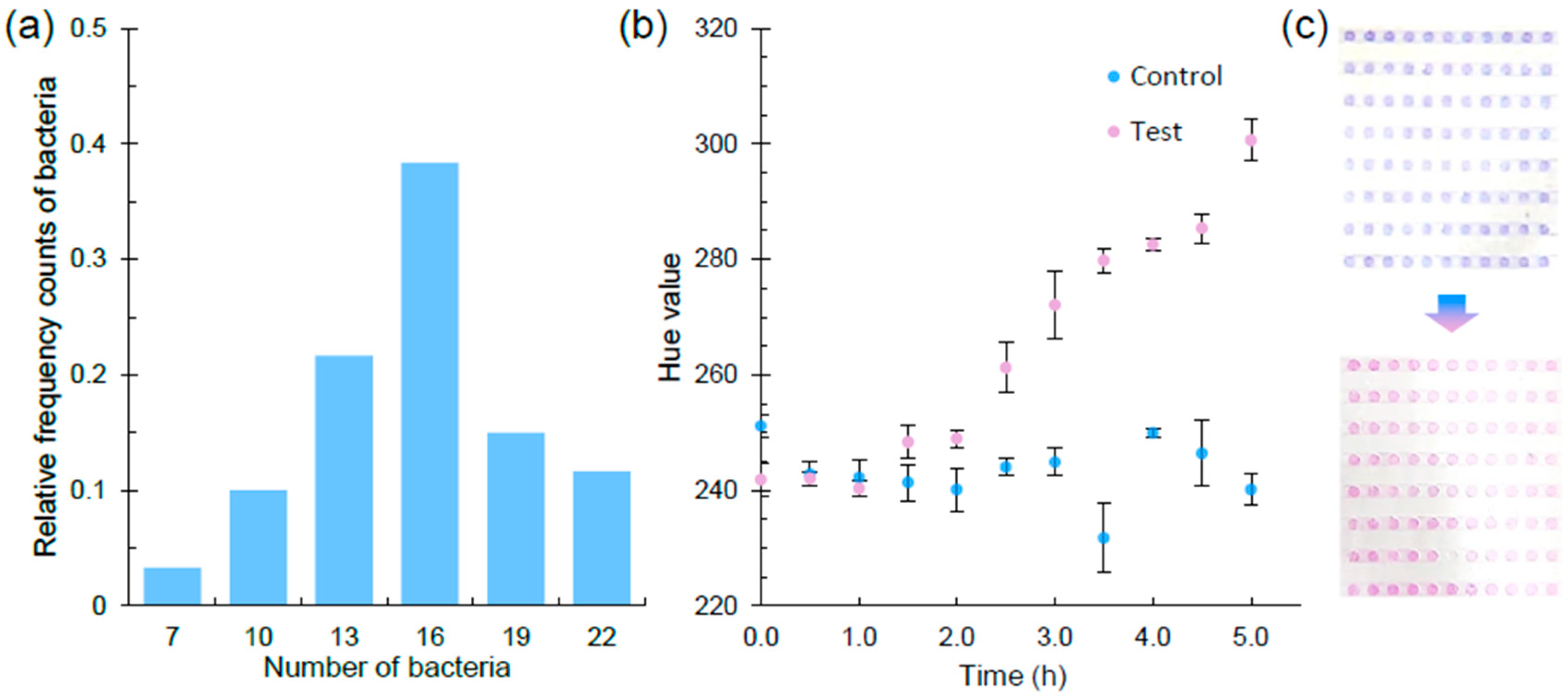
3.2. Colorimetric Antibiotic Susceptibility Reporting through Smartphone Imaging of the Micro-Well Array Chip
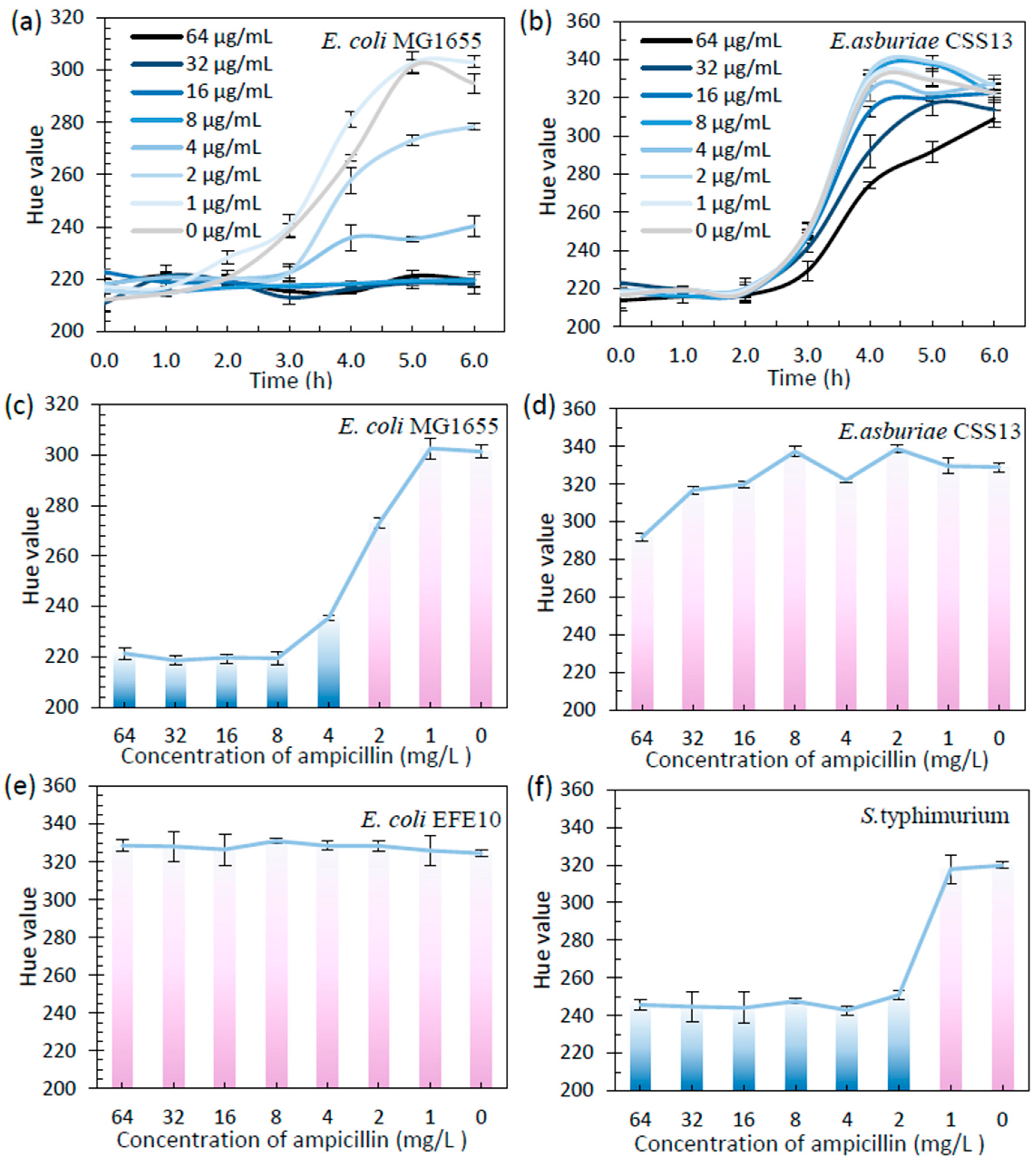
3.3. Micro-Well Array-Based Colorimetric Antibiotic Susceptibility Testing (MacAST) of Bacterial Strains
3.4. Integration of Immunomagnetic Separation with macAST System (imacAST) for Direct Susceptibility Analysis in a Microbiota Sample
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hutchings, M.I.; Truman, A.W.; Wilkinson, B. Antibiotics: Past, present and future. Curr. Opin. Microbiol. 2019, 51, 72–80. [Google Scholar] [CrossRef]
- Khan, Z.A.; Siddiqui, M.F.; Park, S. Progress in antibiotic susceptibility tests: A comparative review with special emphasis on microfluidic methods. Biotechnol. Lett. 2019, 41, 221–230. [Google Scholar] [CrossRef]
- Jernigan, J.A.; Hatfield, K.M.; Wolford, H.; Nelson, R.E.; Olubajo, B.; Reddy, S.C.; McCarthy, N.; Paul, P.; McDonald, L.C.; Kallen, A.; et al. Multidrug-Resistant Bacterial Infections in U.S. Hospitalized Patients, 2012–2017. N. Engl. J. Med. 2020, 382, 1309–1319. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhang, G.; Ju, F. Using Culture-Enriched Phenotypic Metagenomics for Targeted High-Throughput Monitoring of the Clinically Important Fraction of the beta-Lactam Resistome. Environ. Sci. Technol. 2022, 56, 11429–11439. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Show, P.L.; Ngo, H.H.; Ho, S.-H. Algae-mediated antibiotic wastewater treatment: A critical review. Environ. Sci. Ecotechnol. 2022, 9, 100145. [Google Scholar] [CrossRef] [PubMed]
- Beckley, A.M.; Wright, E.S. Identification of antibiotic pairs that evade concurrent resistance via a retrospective analysis of antimicrobial susceptibility test results. Lancet Microbe 2021, 2, e545–e554. [Google Scholar] [CrossRef] [PubMed]
- Khan, Z.A.; Siddiqui, M.F.; Park, S. Current and Emerging Methods of Antibiotic Susceptibility Testing. Diagnostics 2019, 9, 49. [Google Scholar] [CrossRef] [PubMed]
- Benkova, M.; Soukup, O.; Marek, J. Antimicrobial susceptibility testing: Currently used methods and devices and the near future in clinical practice. J. Appl. Microbiol. 2020, 129, 806–822. [Google Scholar] [CrossRef]
- Baltekin, O.; Boucharin, A.; Tano, E.; Andersson, D.I.; Elf, J. Antibiotic susceptibility testing in less than 30 min using direct single-cell imaging. Proc. Natl. Acad. Sci. USA 2017, 114, 9170–9175. [Google Scholar] [CrossRef]
- Abram, T.J.; Cherukury, H.; Ou, C.Y.; Vu, T.; Toledano, M.; Li, Y.; Grunwald, J.T.; Toosky, M.N.; Tifrea, D.F.; Slepenkin, A.; et al. Rapid bacterial detection and antibiotic susceptibility testing in whole blood using one-step, high throughput blood digital PCR. Lab A Chip 2020, 20, 477–489. [Google Scholar] [CrossRef]
- Puttaswamy, S.; Gupta, S.K.; Regunath, H.; Smith, L.P.; Sengupta, S. A Comprehensive Review of the Present and Future Antibiotic Susceptibility Testing (AST) Systems. Arch. Clin. Microbiol. 2018, 9, 83. [Google Scholar] [CrossRef]
- Behera, B.; Anil Vishnu, G.K.; Chatterjee, S.; Sitaramgupta, V.V.; Sreekumar, N.; Nagabhushan, A.; Rajendran, N.; Prathik, B.H.; Pandya, H.J. Emerging technologies for antibiotic susceptibility testing. Biosens. Bioelectron. 2019, 142, 111552. [Google Scholar] [CrossRef] [PubMed]
- Strommenger, B.; Kettlitz, C.; Werner, G.; Witte, W. Multiplex PCR assay for simultaneous detection of nine clinically relevant antibiotic resistance genes in Staphylococcus aureus. J. Clin. Microbiol. 2003, 41, 4089–4094. [Google Scholar] [CrossRef]
- Ho, J.Y.; Jong, M.C.; Acharya, K.; Liew, S.S.X.; Smith, D.R.; Noor, Z.Z.; Goodson, M.L.; Werner, D.; Graham, D.W.; Eswaran, J. Multidrug-resistant bacteria and microbial communities in a river estuary with fragmented suburban waste management. J. Hazard. Mater. 2021, 405, 124687. [Google Scholar] [CrossRef]
- Ju, F.; Li, B.; Ma, L.; Wang, Y.; Huang, D.; Zhang, T. Antibiotic resistance genes and human bacterial pathogens: Co-occurrence, removal, and enrichment in municipal sewage sludge digesters. Water Res. 2016, 91, 1–10. [Google Scholar] [CrossRef]
- Bhattacharyya, R.P.; Bandyopadhyay, N.; Ma, P.; Son, S.S.; Liu, J.; He, L.L.; Wu, L.; Khafizov, R.; Boykin, R.; Cerqueira, G.C.; et al. Simultaneous detection of genotype and phenotype enables rapid and accurate antibiotic susceptibility determination. Nat. Med. 2019, 25, 1858–1864. [Google Scholar] [CrossRef]
- Spencer, D.C.; Paton, T.F.; Mulroney, K.T.; Inglis, T.J.J.; Sutton, J.M.; Morgan, H. A fast impedance-based antimicrobial susceptibility test. Nat. Commun. 2020, 11, 5328. [Google Scholar] [CrossRef]
- Hassan, S.U.; Tariq, A.; Noreen, Z.; Donia, A.; Zaidi, S.Z.J.; Bokhari, H.; Zhang, X. Capillary-Driven Flow Microfluidics Combined with Smartphone Detection: An Emerging Tool for Point-of-Care Diagnostics. Diagnostics 2020, 10, 509. [Google Scholar] [CrossRef]
- Lee, W.B.; Fu, C.Y.; Chang, W.H.; You, H.L.; Wang, C.H.; Lee, M.S.; Lee, G.B. A microfluidic device for antimicrobial susceptibility testing based on a broth dilution method. Biosens. Bioelectron. 2017, 87, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.L.; Zhang, J.X.; Min, D.; Lv, J.L.; Liu, D.F.; Yu, H.Q. Detection and Quantification of Antimicrobial-Resistant Cells in Aquatic Environments by Bioorthogonal Noncanonical Amino Acid Tagging. Environ. Sci. Technol. 2022, 56, 15685–15694. [Google Scholar] [CrossRef]
- Xu, X.; Chen, S.; Yu, Y.; Virtanen, P.; Wu, J.; Hu, Q.; Koskiniemi, S.; Zhang, Z. All-electrical antibiotic susceptibility testing within 30 min using silicon nano transistors. Sens. Actuators B Chem. 2022, 357, 131458. [Google Scholar] [CrossRef]
- Liao, C.C.; Chen, Y.Z.; Lin, S.J.; Cheng, H.W.; Wang, J.K.; Wang, Y.L.; Han, Y.Y.; Huang, N.T. A microfluidic microwell device operated by the automated microfluidic control system for surface-enhanced Raman scattering-based antimicrobial susceptibility testing. Biosens. Bioelectron. 2021, 191, 113483. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Dong, H.; Shen, W.; Yang, Y.; Li, Z.; Liu, Y.; Wang, C.; Gu, B.; Zhang, L. Rapid SERS identification of methicillin-susceptible and methicillin-resistant Staphylococcus aureus via aptamer recognition and deep learning. RSC Adv. 2021, 11, 34425–34431. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Qin, S.; Wu, S.; Liang, Y.; Li, J. Microfluidic systems for rapid antibiotic susceptibility tests (ASTs) at the single-cell level. Chem. Sci. 2020, 11, 6352–6361. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Banaei, N.; Ren, K. Microfluidics for Combating Antimicrobial Resistance. Trends Biotechnol. 2017, 35, 1129–1139. [Google Scholar] [CrossRef] [PubMed]
- Dai, J.; Hamon, M.; Jambovane, S. Microfluidics for Antibiotic Susceptibility and Toxicity Testing. Bioengineering 2016, 3, 25. [Google Scholar] [CrossRef]
- Hassan, S.-u.; Zhang, X. Microfluidics as an Emerging Platform for Tackling Antimicrobial Resistance (AMR): A Review. Curr. Anal. Chem. 2020, 16, 41–51. [Google Scholar] [CrossRef]
- Kao, Y.T.; Kaminski, T.S.; Postek, W.; Guzowski, J.; Makuch, K.; Ruszczak, A.; von Stetten, F.; Zengerle, R.; Garstecki, P. Gravity-driven microfluidic assay for digital enumeration of bacteria and for antibiotic susceptibility testing. Lab A Chip 2020, 20, 54–63. [Google Scholar] [CrossRef]
- Ding, C.; Liu, Y.; Guo, Y.; Guo, X.; Kang, Q.; Yan, X.; He, Z. Precise digital bacteria enumeration and antibiotic susceptibility testing via a portable vibrating capillary-based droplet platform. Sens. Actuators B Chem. 2023, 380, 133254. [Google Scholar] [CrossRef]
- Avesar, J.; Rosenfeld, D.; Truman-Rosentsvit, M.; Ben-Arye, T.; Geffen, Y.; Bercovici, M.; Levenberg, S. Rapid phenotypic antimicrobial susceptibility testing using nanoliter arrays. Proc. Natl. Acad. Sci. USA 2017, 114, E5787–E5795. [Google Scholar] [CrossRef]
- Zhang, H.; Yao, Y.; Hui, Y.; Zhang, L.; Zhou, N.; Ju, F. A 3D-printed microfluidic gradient concentration chip for rapid antibiotic-susceptibility testing. Bio-Des. Manuf. 2021, 5, 210–219. [Google Scholar] [CrossRef]
- Huang, H.K.; Cheng, H.W.; Liao, C.C.; Lin, S.J.; Chen, Y.Z.; Wang, J.K.; Wang, Y.L.; Huang, N.T. Bacteria encapsulation and rapid antibiotic susceptibility test using a microfluidic microwell device integrating surface-enhanced Raman scattering. Lab A Chip 2020, 20, 2520–2528. [Google Scholar] [CrossRef] [PubMed]
- Juskova, P.; Schmitt, S.; Kling, A.; Rackus, D.G.; Held, M.; Egli, A.; Dittrich, P.S. Real-Time Respiration Changes as a Viability Indicator for Rapid Antibiotic Susceptibility Testing in a Microfluidic Chamber Array. ACS Sens. 2021, 6, 2202–2210. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, V.K.; Bakthavathsalam, P.; Bergquist, P.L.; Sunna, A. Smartphone detection of antibiotic resistance using convective PCR and a lateral flow assay. Sens. Actuators B Chem. 2019, 298, 126849. [Google Scholar] [CrossRef]
- Ju, F.; Zhang, T. Bacterial assembly and temporal dynamics in activated sludge of a full-scale municipal wastewater treatment plant. ISME J. 2015, 9, 683–695. [Google Scholar] [CrossRef] [PubMed]
- Daza, R.; Gutiérrez, J.; Piédrola, G. Antibiotic susceptibility of bacterial strains isolated from patients with community-acquired urinary tract infections. Int. J. Antimicrob. A 2000, 18, 5. [Google Scholar] [CrossRef]
- Bouchrif, B.; Paglietti, B.; Murgia, M.; Piana, A.; Cohen, N.; Ennaji, M.M.; Rubino, S.; Timinouni, M. Prevalence and antibiotic-resistance of Salmonella isolated from food in Morocco. J. Infect. Dev. Ctries. 2009, 3, 6. [Google Scholar]
- Aloni-Grinstein, R.; Schuster, O.; Yitzhaki, S.; Aftalion, M.; Maoz, S.; Steinberger-Levy, I.; Ber, R. Isolation of Francisella tularensis and Yersinia pestis from Blood Cultures by Plasma Purification and Immunomagnetic Separation Accelerates Antibiotic Susceptibility Determination. Front. Microbiol. 2017, 8, 312. [Google Scholar] [CrossRef]
- Huang, F.; Xue, L.; Zhang, H.; Guo, R.; Li, Y.; Liao, M.; Wang, M.; Lin, J. An enzyme-free biosensor for sensitive detection of Salmonella using curcumin as signal reporter and click chemistry for signal amplification. Theranostics 2018, 8, 6263–6273. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhou, N.; Ju, F. Immunoreaction-Based Sensors to Improve Bacterial Detection. In Handbook of Biochips; Springer: New York, NY, USA, 2020; pp. 1–16. [Google Scholar]
- Willyard, C. The drug-resistant bacteria that pose the greatest health threats. Nature 2017, 543, 1. [Google Scholar] [CrossRef]
- Yan, Q.; Dong, H.; Su, J.; Han, J.; Song, B.; Wei, Q.; Shi, Y. A Review of 3D Printing Technology for Medical Applications. Engineering 2018, 4, 729–742. [Google Scholar] [CrossRef]
- He, Y.; Nie, J.; Xie, M.; Gao, Q. Why choose 3D bioprinting? Part III: Printing in vitro 3D models for drug screening. Bio-Des. Manuf. 2020, 3, 160–163. [Google Scholar] [CrossRef]
- Lei, W.; Huang, F.; Cai, G.; Lan, Y.; Lin, J.J.N. An Electrochemical Aptasensor Using Coaxial Capillary with Magnetic Nanoparticle Urease Catalysis and PCB Electrode for Rapid and Sensitive Detection of Escherichia coli O157:H7. Nanotheranostics 2017, 1, 403–414. [Google Scholar]
- Xiong, Q.; Cui, X.; Saini, J.K.; Liu, D.; Shan, S.; Jin, Y.; Lai, W. Development of an immunomagnetic separation method for efficient enrichment of Escherichia coli O157:H7. Food Control 2014, 37, 41–45. [Google Scholar] [CrossRef]
- Erbil, H.Y.; Cansoy, C.E. Range of applicability of the Wenzel and Cassie-Baxter equations for superhydrophobic surfaces. Langmuir 2009, 25, 14135–14145. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Xue, L.; Huang, F.; Wang, S.; Wang, L.; Liu, N.; Lin, J. A capillary biosensor for rapid detection of Salmonella using Fe-nanocluster amplification and smart phone imaging. Biosens. Bioelectron. 2019, 127, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Azizi, M.; Zaferani, M.; Dogan, B.; Zhang, S.; Simpson, K.W.; Abbaspourrad, A. Nanoliter-Sized Microchamber/Microarray Microfluidic Platform for Antibiotic Susceptibility Testing. Anal. Chem. 2018, 90, 14137–14144. [Google Scholar] [CrossRef]
- Chen, F.E.; Kaushik, A.; Hsieh, K.; Chang, E.; Chen, L.; Zhang, P.; Wang, T.H. Toward Decentralizing Antibiotic Susceptibility Testing via Ready-to-Use Microwell Array and Resazurin-Aided Colorimetric Readout. Anal. Chem. 2021, 93, 1260–1265. [Google Scholar] [CrossRef]
- González-Pinzón, R.; Haggerty, R.; Myrold, D.D. Measuring aerobic respiration in stream ecosystems using the resazurin-resorufin system. J. Geophys. Res. Biogeosci. 2012, 117, G00N. [Google Scholar] [CrossRef]
- Needs, S.H.; Saiprom, N.; Rafaque, Z.; Imtiaz, W.; Chantratita, N.; Runcharoen, C.; Thammachote, J.; Anun, S.; Peacock, S.J.; Ray, P.; et al. Miniaturised broth microdilution for simplified antibiotic susceptibility testing of Gram negative clinical isolates using microcapillary devices. Analyst 2022, 147, 3558–3569. [Google Scholar] [CrossRef]
- Yi, X.; Song, Y.; Xu, X.; Peng, D.; Wang, J.; Qie, X.; Lin, K.; Yu, M.; Ge, M.; Wang, Y.; et al. Development of a Fast Raman-Assisted Antibiotic Susceptibility Test (FRAST) for the Antibiotic Resistance Analysis of Clinical Urine and Blood Samples. Anal. Chem. 2021, 93, 5098–5106. [Google Scholar] [CrossRef] [PubMed]
- Mulroney, K.T.; Hall, J.M.; Huang, X.; Turnbull, E.; Bzdyl, N.M.; Chakera, A.; Naseer, U.; Corea, E.M.; Ellington, M.J.; Hopkins, K.L.; et al. Rapid susceptibility profiling of carbapenem-resistant Klebsiella pneumoniae. Sci. Rep. 2017, 7, 1903–1915. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Gupta, K.; Ekinci, K.L. All-electrical monitoring of bacterial antibiotic susceptibility in a microfluidic device. Proc. Natl. Acad. Sci. USA 2020, 117, 10639–10644. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; Li, H.Z.; Zhu, X.; Su, J.Q.; Ren, B.; Zhu, Y.G.; Cui, L. Rapid Antibiotic Susceptibility Testing of Pathogenic Bacteria Using Heavy-Water-Labeled Single-Cell Raman Spectroscopy in Clinical Samples. Anal. Chem. 2019, 91, 6296–6303. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Ryu, J.; Liu, L.; Choi, S. A simple, inexpensive, and rapid method to assess antibiotic effectiveness against exoelectrogenic bacteria. Biosens. Bioelectron. 2020, 168, 112518. [Google Scholar] [CrossRef]
- Lin, S.-J.; Chao, P.-H.; Cheng, H.-W.; Wang, J.-K.; Wang, Y.-L.; Han, Y.-Y.; Huang, N.-T. An antibiotic concentration gradient microfluidic device integrating surface-enhanced Raman spectroscopy for multiplex antimicrobial susceptibility testing. Lab A Chip 2022, 22, 1805–1814. [Google Scholar] [CrossRef]
- Chan, C.W.; Sun, H.; Wang, Y.; Zhao, Z.; O’Neill, R.; Siu, S.Y.; Chu, X.; Banaei, N.; Ren, K. “Barcode” cell sensor microfluidic system: Rapid and sample-to-answer antimicrobial susceptibility testing applicable in resource-limited conditions. Biosens. Bioelectron. 2021, 192, 113516. [Google Scholar] [CrossRef]
- Heuer, C.; Preuss, J.-A.; Buttkewitz, M.; Scheper, T.; Segal, E.; Bahnemann, J. A 3D-printed microfluidic gradient generator with integrated photonic silicon sensors for rapid antimicrobial susceptibility testing. Lab A Chip 2022, 22, 4950–4961. [Google Scholar] [CrossRef]
- Xue, L.; Jiang, F.; Xi, X.; Li, Y.; Lin, J. Lab-on-chip separation and biosensing of pathogens in agri-food. Trends Food Sci. Technol. 2023, 137, 92–103. [Google Scholar] [CrossRef]
- Huang, T.; Yang, J.; Zhou, W.; Liu, X.; Pan, Y.; Song, Y. Rapid identification of urinary tract infections based on ultrasensitive bacteria detection using volumetric bar-chart chip. Sens. Actuators B Chem. 2019, 298, 126885. [Google Scholar] [CrossRef]


| Fabrication of Chip | Time of Detection | Equipment | Throughput (per Chip) | Bacterial Isolation | Ref. |
|---|---|---|---|---|---|
| Paper-based | 5 h | Multimeters | 8 | Classical culture (days) | [56] |
| Photolithography | 2 h | Raman | 1 | [32] | |
| Photolithography | 5 h | Raman | 64 | [57] | |
| Photolithography | 2 h | Electrodes | 1 | [54] | |
| Photolithography | 2–3 h | Microscope | 4 | [33] | |
| Photolithography | 5 h | Naked eyes | 12 | [49] | |
| Polypropylene | 2–3 h | Smartphone | 6 | [58] | |
| CNC-milled | ~5 h | Microscope | 4 | [28] | |
| 3D printing | 1.5 h | Spectrometer | 6 | [59] | |
| 3D printing | 5 h | Microscope | 6 | [29] | |
| — | 2.5 h | Raman | — | Filtration (non-specificity) | [55] |
| Photolithography | 4.5–5.5 h | Microscope | 2 | [30] | |
| 3D printing | 5 h | Smartphone | 128 | Specific separation (<1 h) | This work |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, H.; Wang, L.; Zhang, Z.; Lin, J.; Ju, F. Cost-Efficient Micro-Well Array-Based Colorimetric Antibiotic Susceptibility Testing (MacAST) for Bacteria from Culture or Community. Biosensors 2023, 13, 1028. https://doi.org/10.3390/bios13121028
Zhang H, Wang L, Zhang Z, Lin J, Ju F. Cost-Efficient Micro-Well Array-Based Colorimetric Antibiotic Susceptibility Testing (MacAST) for Bacteria from Culture or Community. Biosensors. 2023; 13(12):1028. https://doi.org/10.3390/bios13121028
Chicago/Turabian StyleZhang, Huilin, Lei Wang, Zhiguo Zhang, Jianhan Lin, and Feng Ju. 2023. "Cost-Efficient Micro-Well Array-Based Colorimetric Antibiotic Susceptibility Testing (MacAST) for Bacteria from Culture or Community" Biosensors 13, no. 12: 1028. https://doi.org/10.3390/bios13121028





