Reliability, Validity, and Identification Ability of a Commercialized Waist-Attached Inertial Measurement Unit (IMU) Sensor-Based System in Fall Risk Assessment of Older People
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Equipment
2.3. Experimental Protocol
2.4. Data and Statistical Analysis
2.4.1. Reliability Evaluation of the IMU Sensor-Based System
2.4.2. Validity Evaluation of the IMU Sensor-Based System
2.4.3. Identification Ability Evaluation of the IMU Sensor-Based System
2.4.4. Identification Ability Evaluation of the Mini-BESTest
3. Results
3.1. Demographic Data
3.2. Reliability of the IMU Sensor-Based System
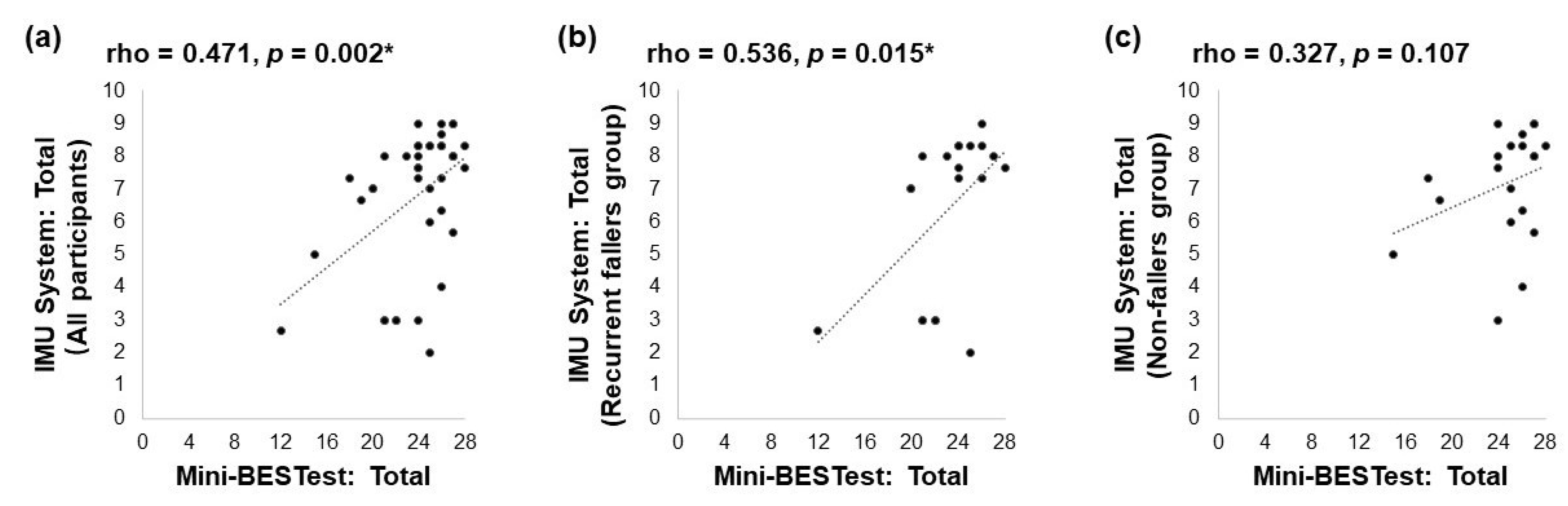
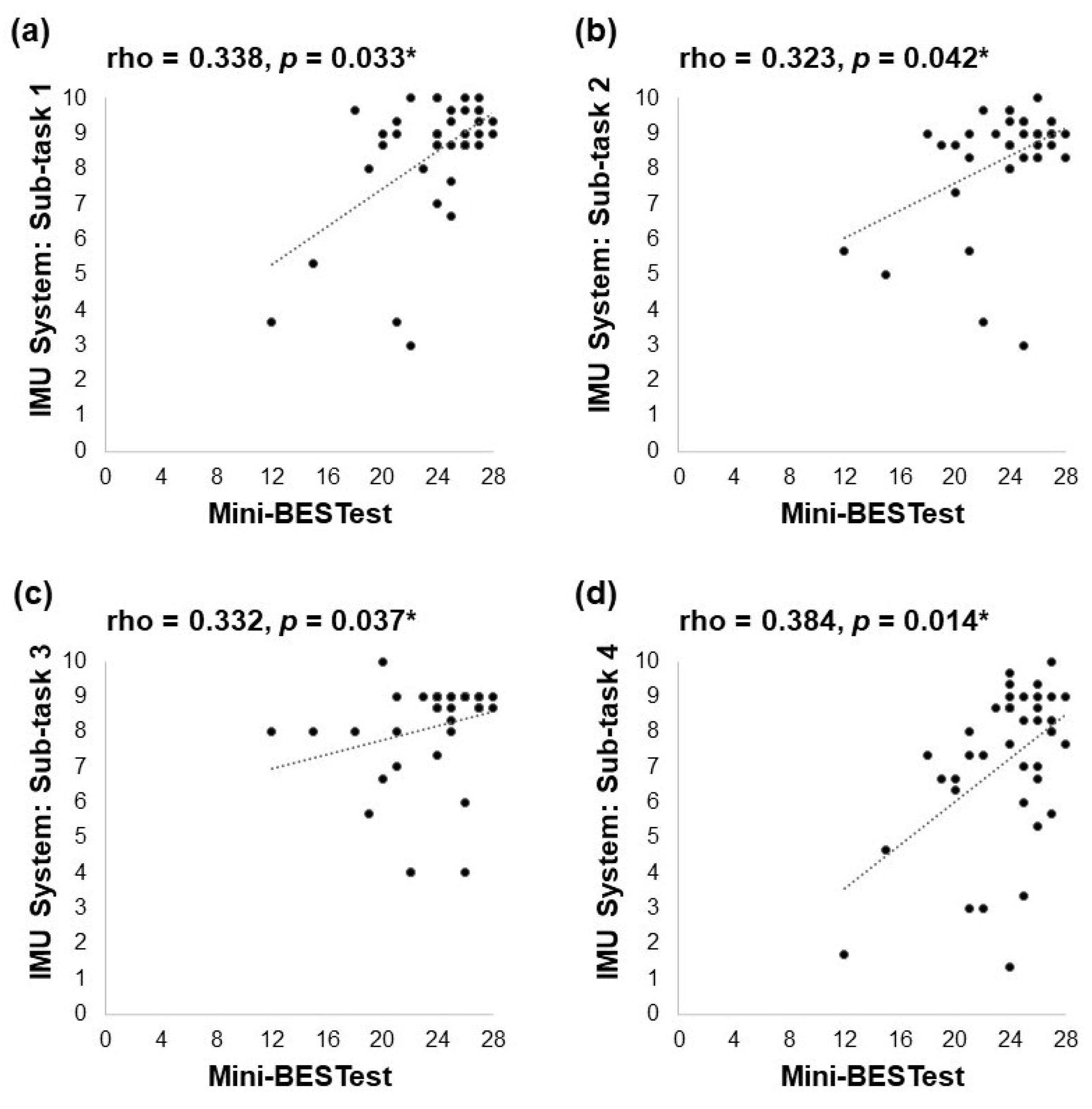
3.3. Validity of the IMU Sensor-Based System
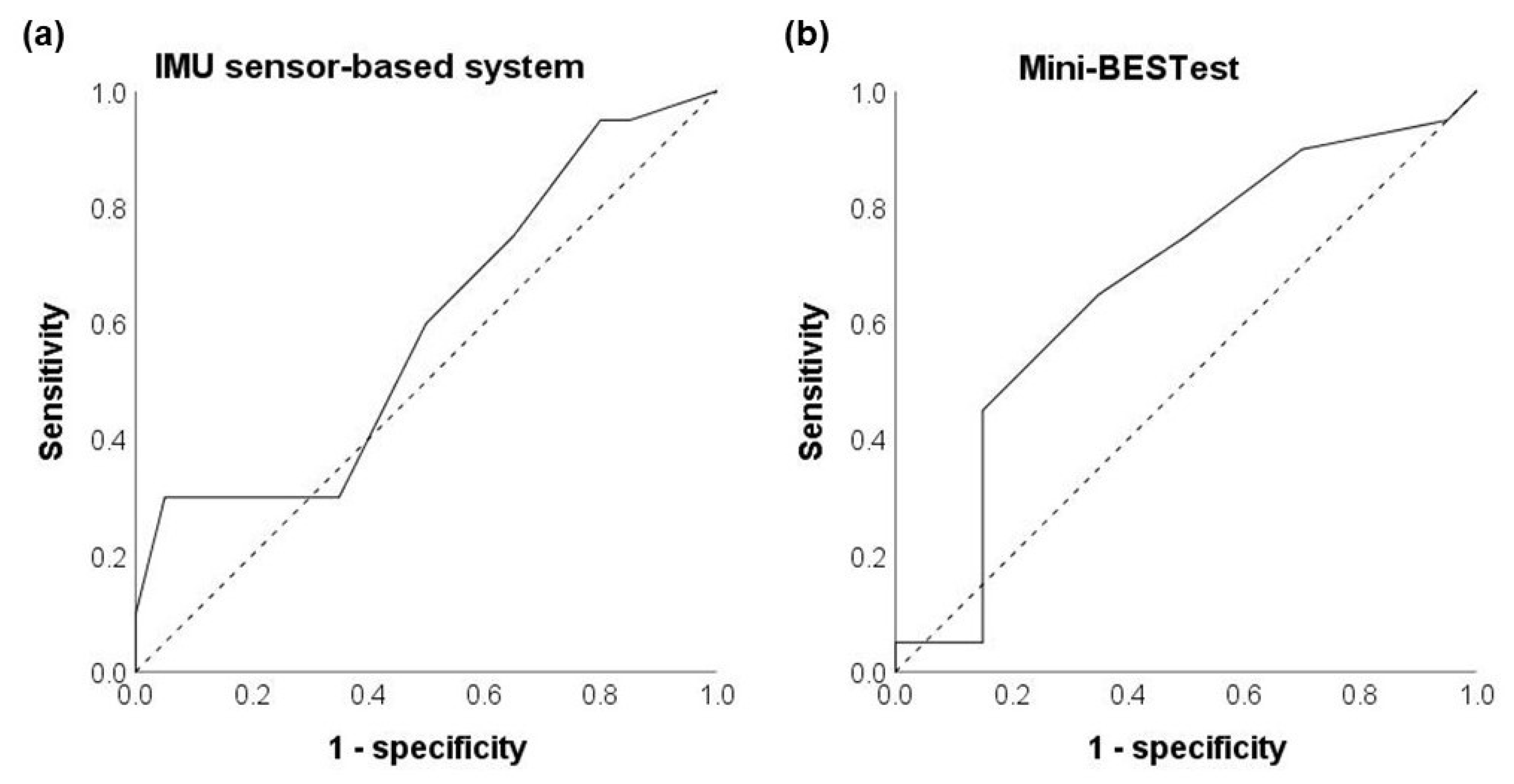
3.4. Fall Risk Identification Ability of the IMU Sensor-Based System
3.5. Fall Risk Identification Ability of the Mini-BESTest
4. Discussion
4.1. Good Reliability of the IMU Sensor-Based System
4.2. Acceptable Validity of the IMU Sensor-Based System
4.3. Poor Identification Ability of the IMU Sensor-Based System
4.4. Inconclusive Identification Ability of the Mini-BESTest
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ganz, D.A.; Latham, N.K. Prevention of Falls in Community-Dwelling Older Adults. N. Engl. J. Med. 2020, 382, 734–743. [Google Scholar] [CrossRef]
- Wang, H.; Chen, H. Aging in China: Challenges and opportunities. China CDC Weekly 2022, 4, 601–602. [Google Scholar]
- Montero-Odasso, M.; van der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.J.A.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef]
- Perell, K.L.; Nelson, A.; Goldman, R.L.; Luther, S.L.; Prieto-Lewis, N.; Rubenstein, L.Z. Fall risk assessment measures: An analytic review. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M761–M766. [Google Scholar] [CrossRef] [PubMed]
- Cuevas-Trisan, R. Balance problems and fall risks in the elderly. Clin. Geriatr. Med. 2019, 35, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Mancini, M.; Horak, F.B. The relevance of clinical balance assessment tools to differentiate balance deficits. Eur. J. Phys. Rehabil. Med. 2010, 46, 239. [Google Scholar] [PubMed]
- Franchignoni, F.; Horak, F.; Godi, M.; Nardone, A.; Giordano, A. Using psychometric techniques to improve the Balance Evaluation Systems Test: The mini-BESTest. J. Rehabil. Med. 2010, 42, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Yingyongyudha, A.; Saengsirisuwan, V.; Panichaporn, W.; Boonsinsukh, R. The Mini-Balance Evaluation Systems Test (Mini-BESTest) Demonstrates Higher Accuracy in Identifying Older Adult Participants with History of Falls Than Do the BESTest, Berg Balance Scale, or Timed Up and Go Test. J. Geriatr. Phys. Ther. 2016, 39, 64–70. [Google Scholar] [CrossRef]
- Viveiro, L.A.P.; Gomes, G.C.V.; Bacha, J.M.R.; Carvas Junisor, N.; Kallas, M.E.; Reis, M.; Jacob Filho, W.; Pompeu, J.E. Reliability, Validity, and Ability to Identity Fall Status of the Berg Balance Scale, Balance Evaluation Systems Test (BESTest), Mini-BESTest, and Brief-BESTest in Older Adults Who Live in Nursing Homes. J. Geriatr. Phys. Ther. 2019, 42, E45–E54. [Google Scholar] [CrossRef]
- Aslankhani, M.A.; Farsi, A.; Fathirezaie, Z.; Zamani Sani, S.H.; Aghdasi, M.T. Validity and reliability of the timed up and go and the anterior functional reach tests in evaluating fall risk in the elderly. Iran. J. Ageing 2015, 10, 16–25. [Google Scholar]
- Montesinos, L.; Castaldo, R.; Pecchia, L. Wearable Inertial Sensors for Fall Risk Assessment and Prediction in Older Adults: A Systematic Review and Meta-Analysis. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 573–582. [Google Scholar] [CrossRef]
- Howcroft, J.; Kofman, J.; Lemaire, E.D. Review of fall risk assessment in geriatric populations using inertial sensors. J. Neuroeng. Rehabil. 2013, 10, 91. [Google Scholar] [CrossRef]
- Piirtola, M.; Era, P.J.G. Force platform measurements as predictors of falls among older people—A review. Gerontology 2006, 52, 1–16. [Google Scholar] [CrossRef]
- Menz, H.B.; Latt, M.D.; Tiedemann, A.; San Kwan, M.M.; Lord, S.R. Reliability of the GAITRite® walkway system for the quantification of temporo-spatial parameters of gait in young and older people. Gait Posture 2004, 20, 20–25. [Google Scholar] [CrossRef]
- Battaglia, G.; Giustino, V.; Messina, G.; Faraone, M.; Brusa, J.; Bordonali, A.; Barbagallo, M.; Palma, A.; Dominguez, L.-J. Walking in natural environments as geriatrician’s recommendation for fall prevention: Preliminary outcomes from the “passiata day” model. Sustainability 2020, 12, 2684. [Google Scholar] [CrossRef]
- Chen, M.; Wang, H.; Yu, L.; Yeung, E.H.K.; Luo, J.; Tsui, K.-L.; Zhao, Y. A Systematic Review of Wearable Sensor-Based Technologies for Fall Risk Assessment in Older Adults. Sensors 2022, 22, 6752. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.Z.-H.; Lee, W.C.-C. A wearable vibrotactile biofeedback system improves balance control of healthy young adults following perturbations from quiet stance. Hum. Mov. Sci. 2017, 55, 54–60. [Google Scholar] [CrossRef]
- Ma, C.Z.; Zheng, Y.P.; Lee, W.C. Changes in gait and plantar foot loading upon using vibrotactile wearable biofeedback system in patients with stroke. Top. Stroke Rehabil. 2018, 25, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Regterschot, G.R.H.; Ribbers, G.M.; Bussmann, J.B. Wearable movement sensors for rehabilitation: From technology to clinical practice. Sensors 2021, 21, 4744. [Google Scholar] [CrossRef] [PubMed]
- Subramaniam, S.; Faisal, A.I.; Deen, M.J. Wearable sensor systems for fall risk assessment: A review. Front. Digit. Health 2022, 4, 921506. [Google Scholar] [CrossRef]
- Ahmad, N.; Ghazilla, R.A.R.; Khairi, N.M.; Kasi, V. Reviews on various inertial measurement unit (IMU) sensor applications. Int. J. Signal Process. Syst. 2013, 1, 256–262. [Google Scholar] [CrossRef]
- Ma, C.Z.-H.; Wong, D.; Lam, W.; Wan, A.; Lee, W. Balance improvement effects of biofeedback systems with state-of-the-art wearable sensors: A systematic review. Sensors 2016, 16, 434. [Google Scholar] [CrossRef] [PubMed]
- Sample, R.B.; Kinney, A.L.; Jackson, K.; Diestelkamp, W.; Bigelow, K.E. Identification of Key Outcome Measures When Using the Instrumented Timed Up and Go and/or Posturography for Fall Screening. Gait Posture 2017, 57, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Greene, B.R.; O’Donovan, A.; Romero-Ortuno, R.; Cogan, L.; Scanaill, C.N.; Kenny, R.A. Quantitative Falls Risk Assessment Using the Timed Up and Go Test. IEEE Trans. Biomed. Eng. 2010, 57, 2918–2926. [Google Scholar] [CrossRef]
- Nouredanesh, M.; Godfrey, A.; Howcroft, J.; Lemaire, E.D.; Tung, J. Fall risk assessment in the wild: A critical examination of wearable sensor use in free-living conditions. Gait Posture 2021, 85, 178–190. [Google Scholar] [CrossRef] [PubMed]
- Baker, N.; Gough, C.; Gordon, S.J. Inertial sensor reliability and validity for static and dynamic balance in healthy adults: A systematic review. Sensors 2021, 21, 5167. [Google Scholar] [CrossRef] [PubMed]
- Salmond, S.S. Evaluating the Reliability and Validity of Measurement Instruments. Orthop. Nurs. 2008, 27, 28–30. [Google Scholar] [CrossRef]
- Parikh, R.; Mathai, A.; Parikh, S.; Sekhar, G.C.; Thomas, R. Understanding and using sensitivity, specificity and predictive values. Indian J. Ophthalmol. 2008, 56, 45. [Google Scholar] [CrossRef]
- Kelsey, J.L.J.L.; Procter-Gray, E.E.; Berry, S.D.S.D.; Hannan, M.T.M.T.; Kiel, D.P.D.P.; Lipsitz, L.A.L.A.; Li, W.W. Re-evaluating the Implications of Recurrent Falls in Older Adults: Location Changes the Inference. J. Am. Geriatr. Soc. (JAGS) 2012, 60, 517–524. [Google Scholar] [CrossRef]
- Diao, Y.; Lou, N.; Liang, S.; Zhang, Y.; Ning, Y.; Li, G.; Zhao, G. A Novel Environment-Adaptive Timed Up and Go Test System for Fall Risk Assessment With Wearable Inertial Sensors. IEEE Sens. J. 2021, 21, 18287–18297. [Google Scholar] [CrossRef]
- Early Prevention of Elderly Falls (booguu.bio). Available online: https://www.booguu.bio/aspire?lang=en (accessed on 11 September 2023).
- Booguu Aspire (TM) AI Mobile Fall Risk Assessment—YouTube. Available online: https://www.youtube.com/watch?v=kIcZ6o8kJNk (accessed on 11 September 2023).
- Cheung, T.K.J. Gait Measurement with 3-Axes Accelerometer/Gyro in Mobile Devices. U.S. Patent 10307086, 20 August 2015. [Google Scholar]
- Cheung, J.T.K. Algorithms for Gait Measurement with 3-Axes Accelerometer/Gyro in Mobile Devices. U.S. Patent 10327671, 16 February 2017. [Google Scholar]
- Zhang, D.J. Gait Measurement with 3-Axes Accelerometer/Gyro in Mobile Devices. CN Patent 106061384A, 9 August 2019. (In Chinese). [Google Scholar]
- King, L.; Horak, F. On the Mini-BESTest: Scoring and the reporting of total scores. Phys. Ther. 2013, 93, 571–575. [Google Scholar] [CrossRef]
- Koo, T.; Li, M. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Taber, K.S. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Lane, H.; Brown, T. Convergent validity of two motor skill tests used to assess school-age children. Scand. J. Occup. Ther. 2015, 22, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Hajjar, S. Statistical analysis: Internal-consistency reliability and construct validity. Int. J. Quant. Qual. Res. Methods 2018, 6, 27–38. [Google Scholar]
- Florkowski, C.M. Sensitivity, specificity, receiver-operating characteristic (ROC) curves and likelihood ratios: Communicating the performance of diagnostic tests. Clin. Biochem. Rev. 2008, 29 (Suppl. S1), S83. [Google Scholar]
- Marques, A.; Almeida, S.; Carvalho, J.; Cruz, J.; Oliveira, A.; Jácome, C. Reliability, validity, and ability to identify fall status of the balance evaluation systems test, mini–balance evaluation systems test, and brief–balance evaluation systems test in older people living in the community. Arch. Phys. Med. Rehabil. 2016, 97, 2166–2173.e1. [Google Scholar] [CrossRef]
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Bautmans, I.; Jansen, B.; Van Keymolen, B.; Mets, T. Reliability and clinical correlates of 3D-accelerometry based gait analysis outcomes according to age and fall-risk. Gait Posture 2011, 33, 366–372. [Google Scholar] [CrossRef]
- Pappas, I.P.I.; Keller, T.; Mangold, S.; Popovic, M.R.; Dietz, V.; Morari, M. A reliable gyroscope-based gait-phase detection sensor embedded in a shoe insole. IEEE Sens. J. 2004, 4, 268–274. [Google Scholar] [CrossRef]
- Craig, J.J.; Bruetsch, A.P.; Lynch, S.G.; Horak, F.B.; Huisinga, J.M. Instrumented balance and walking assessments in persons with multiple sclerosis show strong test-retest reliability. J. Neuroeng. Rehabil. 2017, 14, 43. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.-R.; Chiu, Y.-L.; Chiang, S.-L.; Chen, H.-Y.; Sung, W.-H. Development of a smartphone-based balance assessment system for subjects with stroke. Sensors 2019, 20, 88. [Google Scholar] [CrossRef]
- Di Carlo, S.; Bravini, E.; Vercelli, S.; Massazza, G.; Ferriero, G. The Mini-BESTest: A review of psychometric properties. Int. J. Rehabil. Res. 2016, 39, 97–105. [Google Scholar] [CrossRef]
- Marschollek, M.; Nemitz, G.; Gietzelt, M. Predicting in-patient falls in a geriatric clinic: A clinical study combining assessment data and simple sensory gait measurements. Z. Gerontol. Geriatr. 2009, 42, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Shahzad, A.; Seunguk, K.; Samgyu, L.; Jeong, A.L.; Kiseon, K. Quantitative Assessment of Balance Impairment for Fall-Risk Estimation Using Wearable Triaxial Accelerometer. IEEE Sens. J. 2017, 17, 6743–6751. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, X.; Lockhart, T.E. Fall Risk Assessments Based on Postural and Dynamic Stability Using Inertial Measurement Unit. Saf. Health Work. 2012, 3, 192–198. [Google Scholar] [CrossRef]
- Moore, J.; Stuart, S.; McMeekin, P.; Walker, R.; Celik, Y.; Pointon, M.; Godfrey, A. Enhancing Free-Living Fall Risk Assessment: Contextualizing Mobility Based IMU Data. Sensors 2023, 23, 891. [Google Scholar] [CrossRef]
- McManus, K.; Greene, B.R.; Ader, L.G.M.; Caulfield, B. Development of Data-Driven Metrics for Balance Impairment and Fall Risk Assessment in Older Adults. IEEE Trans. Biomed. Eng. 2022, 69, 2324–2332. [Google Scholar] [CrossRef]
- Cates, B.; Sim, T.; Heo, H.M.; Kim, B.; Kim, H.; Mun, J.H. A novel detection model and its optimal features to classify falls from low-and high-acceleration activities of daily life using an insole sensor system. Sensors 2018, 18, 1227. [Google Scholar] [CrossRef]
- Lockhart, T.E.; Soangra, R.; Yoon, H.; Wu, T.; Frames, C.W.; Weaver, R.; Roberto, K.A. Prediction of fall risk among community-dwelling older adults using a wearable system. Sci. Rep. 2021, 11, 20976. [Google Scholar] [CrossRef]
- Lin, C.-L.; Chiu, W.-C.; Chu, T.-C.; Ho, Y.-H.; Chen, F.-H.; Hsu, C.-C.; Hsieh, P.-H.; Chen, C.-H.; Lin, C.-C.K.; Sung, P.-S. Innovative head-mounted system based on inertial sensors and magnetometer for detecting falling movements. Sensors 2020, 20, 5774. [Google Scholar] [CrossRef] [PubMed]
- Kiprijanovska, I.; Gjoreski, H.; Gams, M. Detection of gait abnormalities for fall risk assessment using wrist-worn inertial sensors and deep learning. Sensors 2020, 20, 5373. [Google Scholar] [CrossRef] [PubMed]
- Tunca, C.; Salur, G.; Ersoy, C. Deep learning for fall risk assessment with inertial sensors: Utilizing domain knowledge in spatio-temporal gait parameters. IEEE J. Biomed. Health Inform. 2019, 24, 1994–2005. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Rehman, R.Z.U.; Yu, X.; Xiong, S. Application of wearable inertial sensors and a new test battery for distinguishing retrospective fallers from non-fallers among community-dwelling older people. Sci. Rep. 2018, 8, 16349. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, L.S.; Bamberg, S.J.M. Insole sensor system for real-time detection of biped slip. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; pp. 1449–1452. [Google Scholar]
- Anson, E.; Thompson, E.; Ma, L.; Jeka, J. Reliability and Fall Risk Detection for the BESTest and Mini-BESTest in Older Adults. J. Geriatr. Phys. Ther. 2019, 42, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Magnani, P.E.; Genovez, M.B.; Porto, J.M.; Zanellato, N.F.G.; Alvarenga, I.C.; Freire, R.C.; De Abreu, D.C.C. Use of the BESTest and the Mini-BESTest for fall risk prediction in community-dwelling older adults between 60 and 102 years of age. J. Geriatr. Phys. Ther. 2020, 43, 179–184. [Google Scholar] [CrossRef]
- Lu, Z.; Lam, F.M.H.; Leung, J.C.S.; Kwok, T.C.Y. The U-Shaped Relationship Between Levels of Bouted Activity and Fall Incidence in Community-Dwelling Older Adults: A Prospective Cohort Study. J. Gerontol. Ser. A 2020, 75, e145–e151. [Google Scholar] [CrossRef]
- Hurtig-Wennlöf, A.; Hagströmer, M.; Olsson, L.A. The International Physical Activity Questionnaire modified for the elderly: Aspects of validity and feasibility. Public Health Nutr. 2010, 13, 1847–1854. [Google Scholar] [CrossRef]
- Minhee, S.; Kim, D.H.; Insook, C.; Ham, O.K. Age and gender differences in fall-related factors affecting community-dwelling older adults. J. Nurs. Res. 2023, 31, e270. [Google Scholar]
- Lo, J.K.; Robinson, L.R. Postpolio syndrome and the late effects of poliomyelitis. Part 1. pathogenesis, biomechanical considerations, diagnosis, and investigations: Postpolio Syndrome, Part 1. Muscle Nerve 2018, 58, 751–759. [Google Scholar] [CrossRef]
- Schwartz, A.V.; Hillier, T.A.; Sellmeyer, D.E.; Resnick, H.E.; Gregg, E.; Ensrud, K.E.; Schreiner, P.J.; Margolis, K.L.; Cauley, J.A.; Nevitt, M.C.; et al. Older women with diabetes have a higher risk of falls: A prospective study. Diabetes Care 2002, 25, 1749–1754. [Google Scholar] [CrossRef] [PubMed]
- Matarese, M.; Ivziku, D.; Bartolozzi, F.; Piredda, M.; De Marinis, M.G. Systematic review of fall risk screening tools for older patients in acute hospitals. J. Adv. Nurs. 2015, 71, 1198–1209. [Google Scholar] [CrossRef] [PubMed]

| Items | Specifications |
|---|---|
| Dimensions | 72.6 mm × 40.5 mm × 12.6 mm |
| Weight | 32 g |
| Processor | ARM® Cortex™-M4F 32-bit processor |
| Accelerometer/Gyroscope | Bosch ® 6-axis accelerometer/gyroscope |
| Magnetometer | Bosch ® 3-axis magnetometer |
| Inertial sensor platform | Bosch ® 9-axis sensor fusion |
| Battery | Rechargeable lithium ion/polymer battery |
| Females (n = 22) | Males (n = 18) | Recurrent Fallers (n = 20) | Non-Fallers (n = 20) | All Participants (n = 40) | |
|---|---|---|---|---|---|
| Age (year) | 70.6 ± 6.8 | 70.1 ± 4.7 | 70.8 ± 6.7 | 70.0 ± 5.2 | 70.4 ± 5.9 |
| Height (cm) | 154.2 ± 7.5 | 167.3 ± 6.4 | 158.6 ± 10.5 | 161.5 ± 8.5 | 160.1 ± 9.6 |
| Weight (kg) | 54.2 ± 8.8 | 68.0 ± 9.4 | 61.3 ± 10.3 | 59.6 ± 12.4 | 60.4 ± 11.3 |
| BMI (kg/m²) | 22.9 ± 4.0 | 24.3 ± 3.2 | 24.3 ± 3.0 | 22.8 ± 4.2 | 23.5 ± 3.7 |
| Total score of the IMU sensor-based system | 6.7 ± 2.0 | 6.9 ± 2.4 | 6.4 ± 2.5 | 7.2 ± 1.7 | 6.8 ± 2.1 |
| Total score of the Mini-BESTest | 22.8 ± 3.6 | 25.0 ± 3.0 | 23.1 ± 3.5 | 24.5 ± 3.4 | 23.8 ± 3.5 |
| Score | ICC Value | 95% Confidence Interval | p-Value | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Total | 0.838 | 0.745 | 0.904 | <0.001 |
| 1st task (postural stability with eyes open) | 0.717 | 0.576 | 0.827 | <0.001 |
| 2nd task (postural stability with eyes closed) | 0.698 | 0.553 | 0.814 | <0.001 |
| 3rd task (dynamic movement and gait I) | 0.653 | 0.495 | 0.783 | <0.001 |
| 4th task (dynamic movement and gait II) | 0.843 | 0.753 | 0.907 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, K.-J.; Wong, N.L.-Y.; Law, M.-C.; Lam, F.M.-H.; Wong, H.-C.; Chan, T.-O.; Wong, K.-N.; Zheng, Y.-P.; Huang, Q.-Y.; Wong, A.Y.-L.; et al. Reliability, Validity, and Identification Ability of a Commercialized Waist-Attached Inertial Measurement Unit (IMU) Sensor-Based System in Fall Risk Assessment of Older People. Biosensors 2023, 13, 998. https://doi.org/10.3390/bios13120998
Li K-J, Wong NL-Y, Law M-C, Lam FM-H, Wong H-C, Chan T-O, Wong K-N, Zheng Y-P, Huang Q-Y, Wong AY-L, et al. Reliability, Validity, and Identification Ability of a Commercialized Waist-Attached Inertial Measurement Unit (IMU) Sensor-Based System in Fall Risk Assessment of Older People. Biosensors. 2023; 13(12):998. https://doi.org/10.3390/bios13120998
Chicago/Turabian StyleLi, Ke-Jing, Nicky Lok-Yi Wong, Man-Ching Law, Freddy Man-Hin Lam, Hoi-Ching Wong, Tsz-On Chan, Kit-Naam Wong, Yong-Ping Zheng, Qi-Yao Huang, Arnold Yu-Lok Wong, and et al. 2023. "Reliability, Validity, and Identification Ability of a Commercialized Waist-Attached Inertial Measurement Unit (IMU) Sensor-Based System in Fall Risk Assessment of Older People" Biosensors 13, no. 12: 998. https://doi.org/10.3390/bios13120998
APA StyleLi, K. -J., Wong, N. L. -Y., Law, M. -C., Lam, F. M. -H., Wong, H. -C., Chan, T. -O., Wong, K. -N., Zheng, Y. -P., Huang, Q. -Y., Wong, A. Y. -L., Kwok, T. C. -Y., & Ma, C. Z. -H. (2023). Reliability, Validity, and Identification Ability of a Commercialized Waist-Attached Inertial Measurement Unit (IMU) Sensor-Based System in Fall Risk Assessment of Older People. Biosensors, 13(12), 998. https://doi.org/10.3390/bios13120998







