A New Antifungal-Loaded Sol-Gel Can Prevent Candida albicans Prosthetic Joint Infection
Abstract
:1. Introduction
2. Results
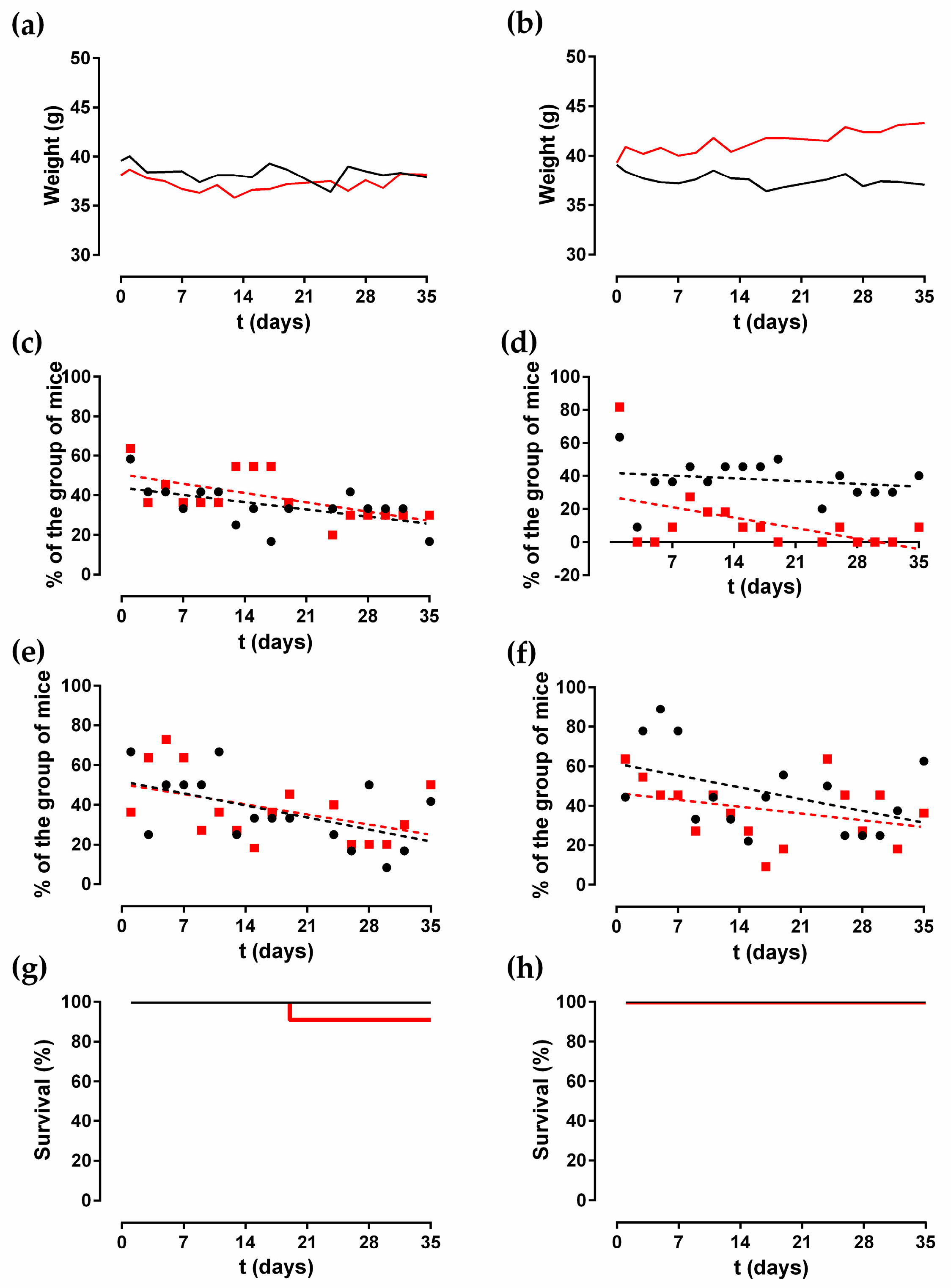
2.1. Animal Monitoring
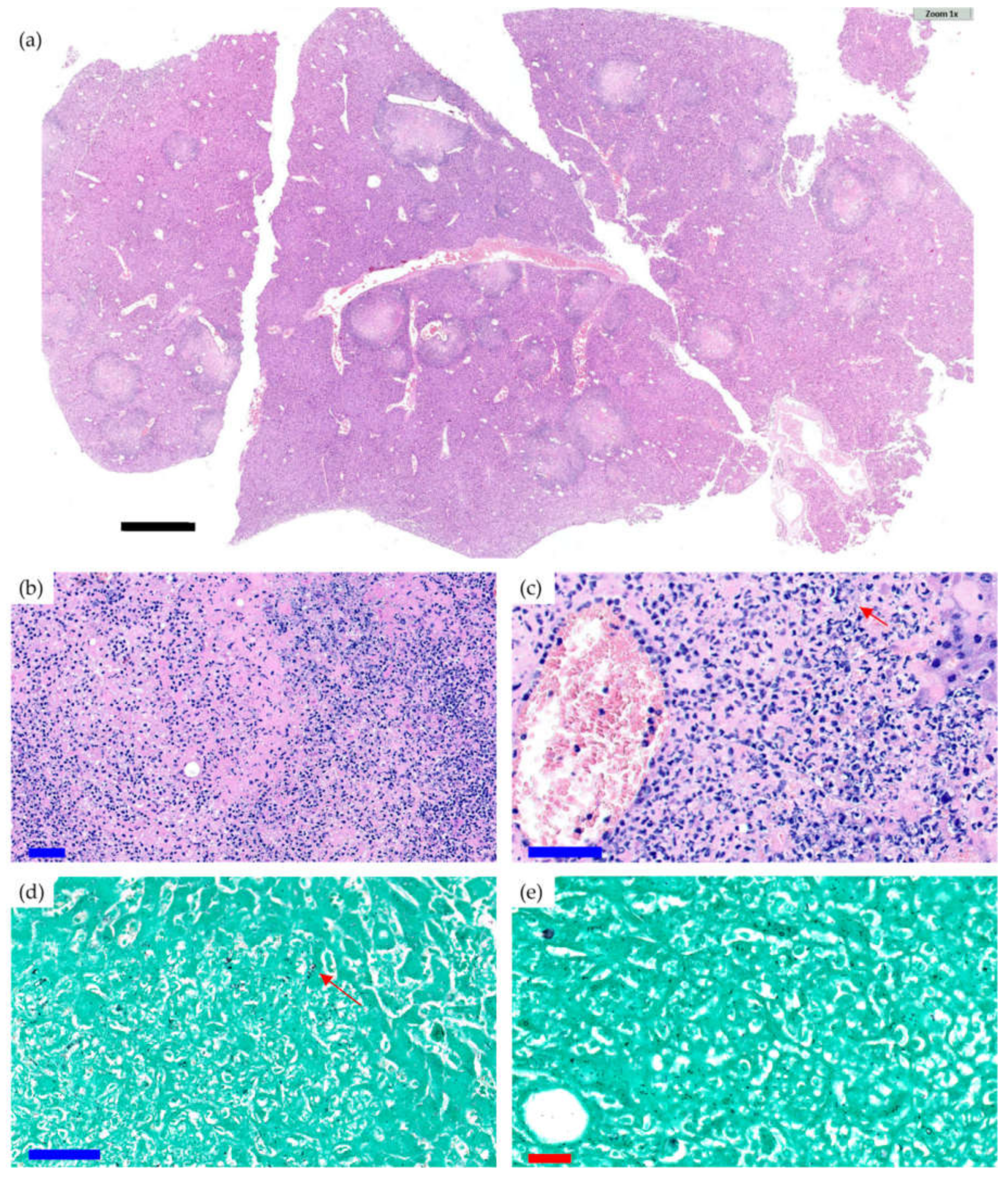
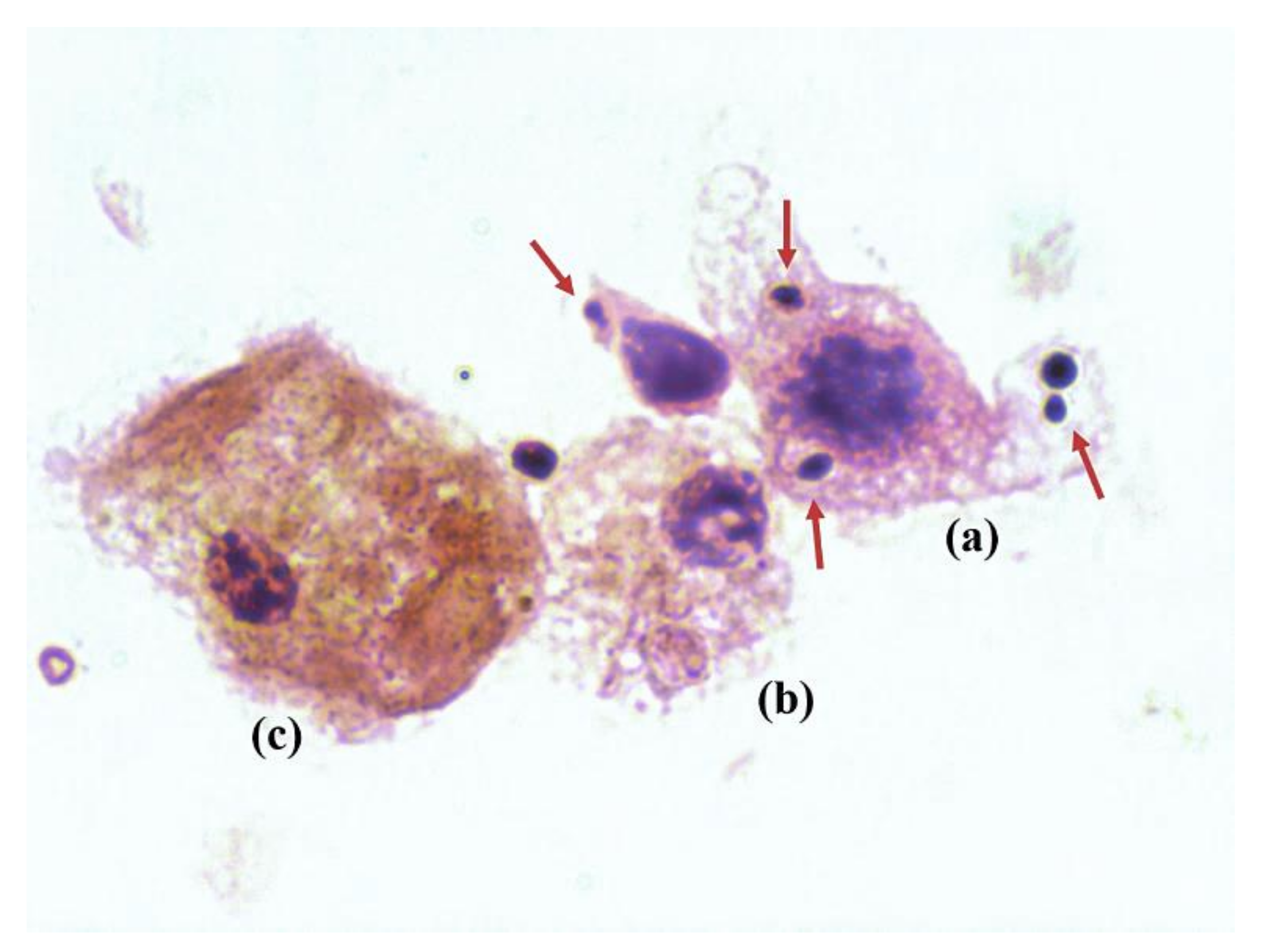
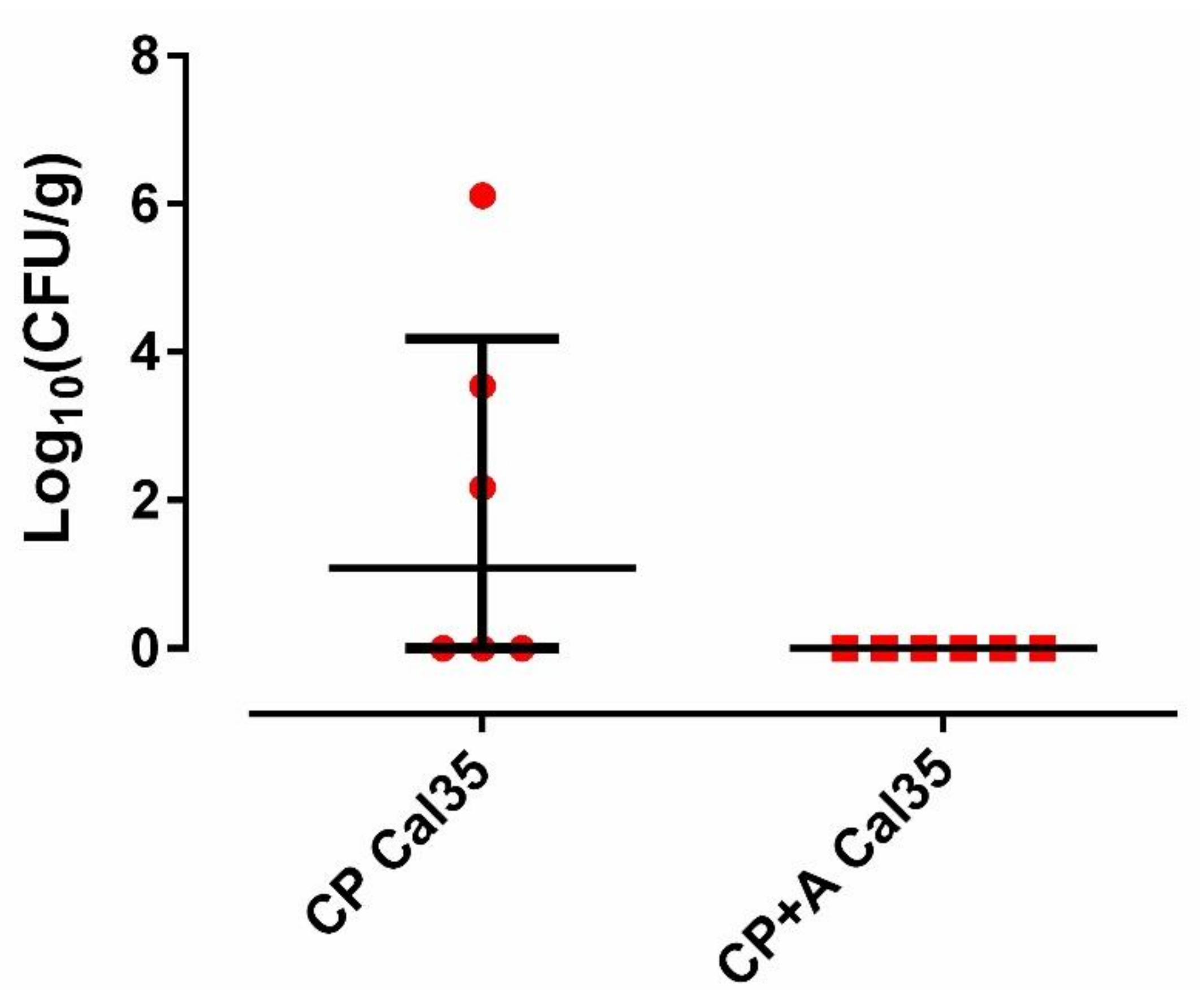
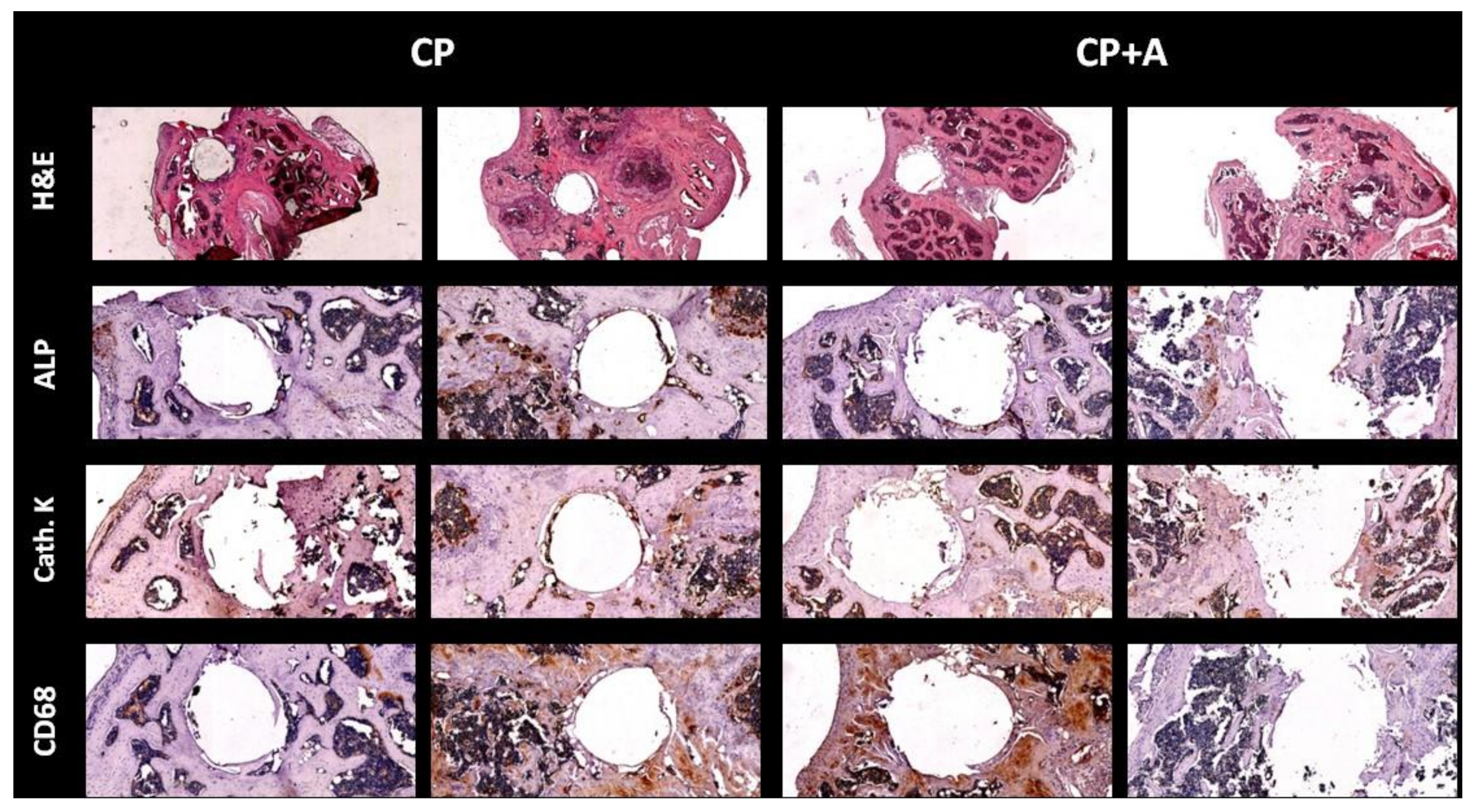
2.2. Microbiological and Pathological Results
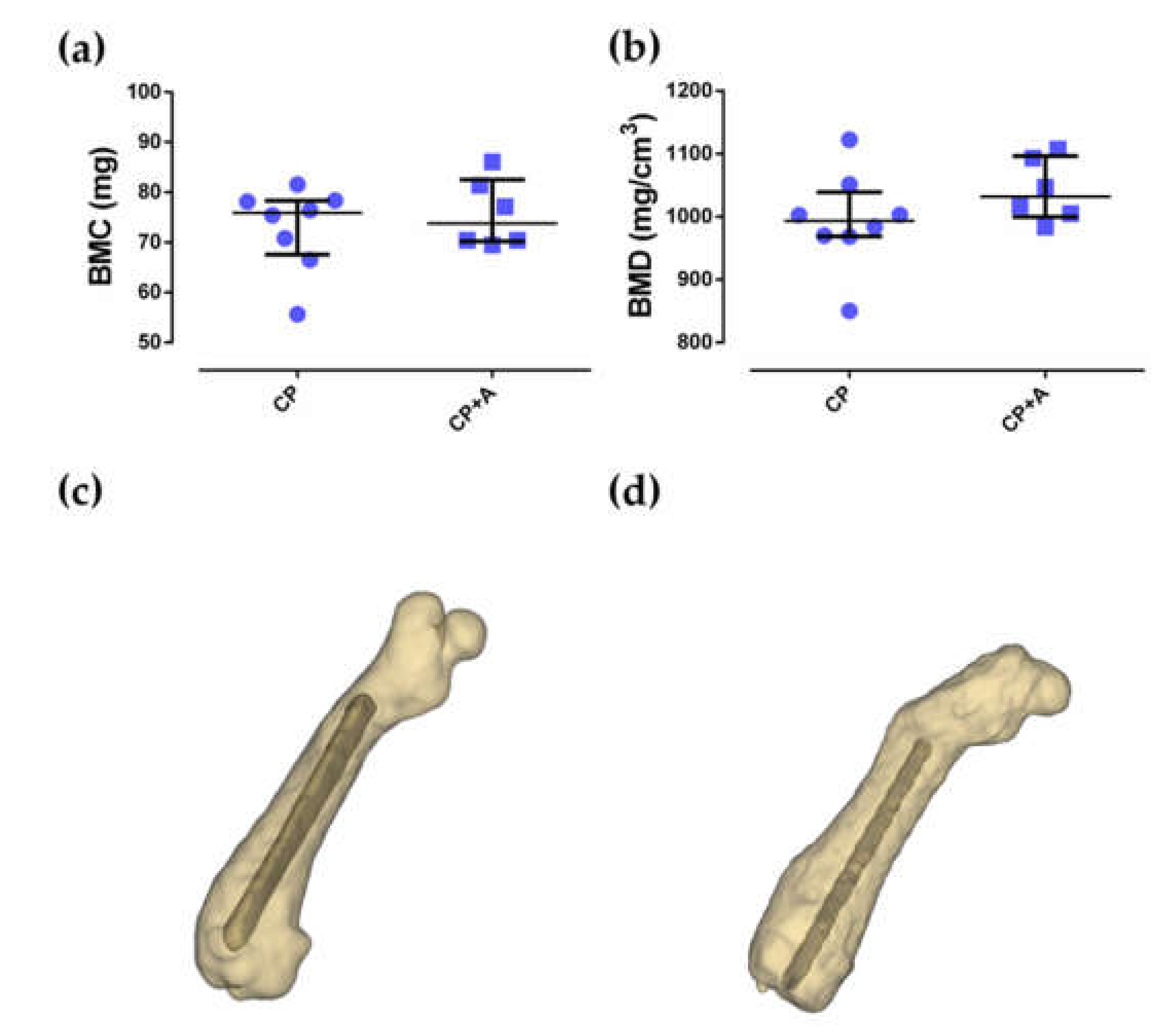
2.3. Microcomputed Tomography and Bone Histology
3. Discussion
4. Materials and Methods
4.1. Sol-Gel Synthesis and Coating of Titanium Implants
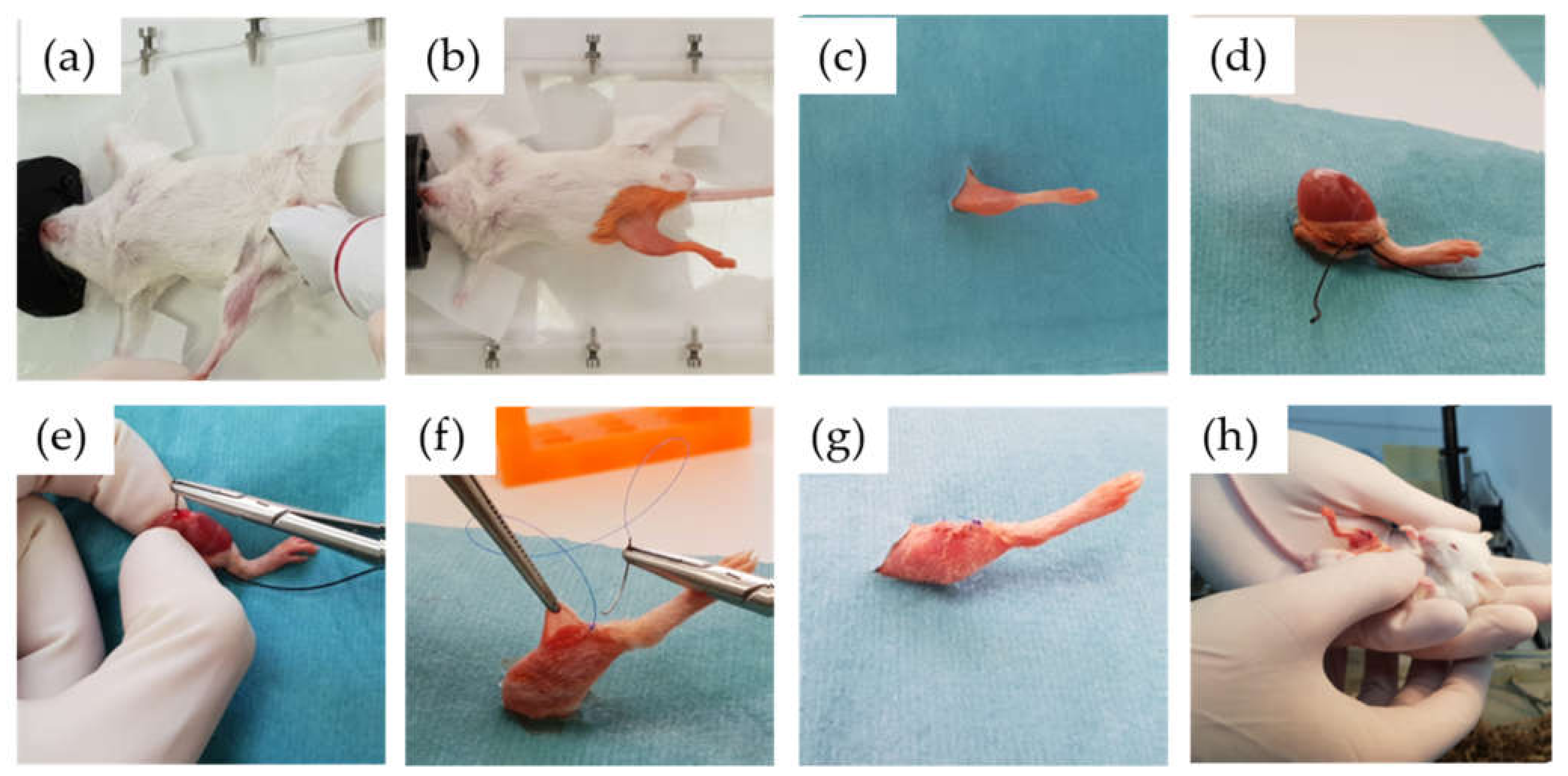
4.2. Animal Surgical Model and Monitoring
4.3. Microbiological and Pathological Studies
- Acute osteomyelitis was defined as bone tissue evidencing moderate-to-high–intensity polymorphonuclear (PMN) inflammatory response with tissue necrosis phenomena and trapping of trabecular bone remains;
- Chronic osteomyelitis was defined as bone tissue that presents a variable inflammatory reaction, partially consisting of a PMN response, but mainly of plasma cells and lymphocytes;
- PJI was diagnosed when any type of osteomyelitis and the presence of yeast were evidenced.
4.4. Microcomputed Tomography
4.5. Immunohistochemistry
4.6. Statistical Analysis
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, Y.; Jordan, J.M. Epidemiology of Osteoarthritis. Clin. Geriatr. Med. 2010, 26, 355–369. [Google Scholar] [CrossRef] [Green Version]
- Tande, A.J.; Patel, R. Prosthetic Joint Infection. Clin. Microbiol. Rev. 2014, 27, 302–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, C.-H.; Lee, S.-H.; Lin, Y.-C.; Wang, Y.-C.; Chang, C.-J.; Hsieh, P.-H. Increased periprosthetic hip and knee infection projected from 2014 to 2035 in Taiwan. J. Infect. Public Heal. 2020, 13, 1768–1773. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Lau, E.; Watson, H.; Schmier, J.K.; Parvizi, J. Economic Burden of Periprosthetic Joint Infection in the United States. J. Arthroplast. 2012, 27, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Azzam, K.; Parvizi, J.; Jungkind, D.; Hanssen, A.; Fehring, T.; Springer, B.; Bozic, K.; Della Valle, C.; Pulido, L.; Barrack, R. Microbiological, Clinical, and Surgical Features of Fungal Prosthetic Joint Infections: A Multi-Institutional Experience. J. Bone Jt. Surg. Am. Vol. 2009, 91, 142–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kapadia, B.H.; Berg, R.A.; Daley, J.A.; Fritz, J.; Bhave, A.; Mont, M.A. Periprosthetic joint infection. Lancet 2016, 387, 386–394. [Google Scholar] [CrossRef]
- Lerario, D.; Ferreira, S.; Miranda, W.; Chacra, A. Influence of dexamethasone and weight loss on the regulation of serum leptin levels in obese individuals. Braz. J. Med Biol. Res. 2001, 34, 479–487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malkawi, A.K.; Alzoubi, K.H.; Jacob, M.; Matic, G.; Ali, A.; Al Faraj, A.; Almuhanna, F.; Dasouki, M.; Rahman, A.M.A. Metabolomics Based Profiling of Dexamethasone Side Effects in Rats. Front. Pharmacol. 2018, 9, 46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marx, J.; Vudathala, D.; Murphy, L.; Rankin, S.; Hankenson, F.C. Antibiotic Administration in the Drinking Water of Mice. J. Am. Assoc. Lab. Anim. Sci. 2014, 53, 301–306. [Google Scholar] [PubMed]
- Malani, P.N.; McNeil, S.A.; Bradley, S.F.; Kauffman, C.A. Candida albicans Sternal Wound Infections: A Chronic and Recurrent Complication of Median Sternotomy. Clin. Infect. Dis. 2002, 35, 1316–1320. [Google Scholar] [CrossRef] [Green Version]
- Orlowski, H.L.P.; McWilliams, S.; Mellnick, V.M.; Bhalla, S.; Lubner, M.G.; Pickhardt, P.J.; Menias, C.O. Imaging Spectrum of Invasive Fungal and Fungal-like Infections. Radiographics 2017, 37, 1119–1134. [Google Scholar] [CrossRef]
- Cheng, A.G.; McAdow, M.; Kim, H.K.; Bae, T.; Missiakas, D.M.; Schneewind, O. Contribution of Coagulases towards Staphylococcus aureus Disease and Protective Immunity. PLoS Pathog. 2010, 6, e1001036. [Google Scholar] [CrossRef] [Green Version]
- Zawrotniak, M.; Wojtalik, K.; Rapala-Kozik, M. Farnesol, a Quorum-Sensing Molecule of Candida albicans Triggers the Release of Neutrophil Extracellular Traps. Cells 2019, 8, 1611. [Google Scholar] [CrossRef] [Green Version]
- Mutua, V.; Gershwin, L.J. A Review of Neutrophil Extracellular Traps (NETs) in Disease: Potential Anti-NETs Therapeutics. Clin. Rev. Allergy Immunol. 2020, 1–18. [Google Scholar] [CrossRef]
- Schauer, C.; Janko, C.; Munoz, L.E.; Zhao, Y.; Kienhöfer, D.; Frey, B.; Lell, M.; Manger, B.; Rech, J.; Naschberger, E.; et al. Aggregated neutrophil extracellular traps limit inflammation by degrading cytokines and chemokines. Nat. Med. 2014, 20, 511–517. [Google Scholar] [CrossRef]
- Karlowicz, M. Candidal renal and urinary tract infection in neonates. Semin. Perinatol. 2003, 27, 393–400. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Diekema, D.J. Epidemiology of Invasive Candidiasis: A Persistent Public Health Problem. Clin. Microbiol. Rev. 2007, 20, 133–163. [Google Scholar] [CrossRef] [Green Version]
- Tsai, N.Y.; Laforce-Nesbitt, S.S.; Tucker, R.; Bliss, J.M. A Murine Model for Disseminated Candidiasis in Neonates. Pediatr. Res. 2011, 69, 189–193. [Google Scholar] [CrossRef] [Green Version]
- Thorn, J.L.; Gilchrist, K.B.; Sobonya, R.E.; Gaur, N.K.; Lipke, P.N.; Klotz, S.A. Postmortem candidaemia: Marker of disseminated disease. J. Clin. Pathol. 2009, 63, 337–340. [Google Scholar] [CrossRef]
- Gamaletsou, M.N.; Rammaert, B.; Bueno, M.A.; Sipsas, N.V.; Moriyama, B.; Kontoyiannis, D.P.; Roilides, E.; Zeller, V.; Tajaldeen, S.J.; Miller, A.O.; et al. Candida Arthritis: Analysis of 112 Pediatric and Adult Cases. Open Forum Infect. Dis. 2016, 3, ofv207. [Google Scholar] [CrossRef] [Green Version]
- Komori, A.; Abe, T.; Kushimoto, S.; Ogura, H.; Shiraishi, A.; Ma, G.A.D.; Saitoh, D.; Fujishima, S.; Mayumi, T.; Gando, S.; et al. Clinical features of patients with candidemia in sepsis. J. Gen. Fam. Med. 2019, 20, 161–163. [Google Scholar] [CrossRef] [PubMed]
- Kao, A.S.; Brandt, M.E.; Pruitt, W.R.; Conn, L.A.; Perkins, B.A.; Stephens, D.S.; Baughman, W.S.; Reingold, A.L.; Rothrock, G.A.; Pfaller, M.A.; et al. The Epidemiology of Candidemia in Two United States Cities: Results of a Population-Based Active Surveillance. Clin. Infect. Dis. 1999, 29, 1164–1170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia-Casas, A.; Aguilera-Correa, J.; Mediero, A.; Esteban, J.; Jimenez-Morales, A. Functionalization of sol-gel coatings with organophosphorus compounds for prosthetic devices. Colloids Surfaces B Biointerfaces 2019, 181, 973–980. [Google Scholar] [CrossRef] [PubMed]
- Aguilera-Correa, J.J.; Vidal-Laso, R.; Carias-Cálix, R.A.; Toirac, B.; García-Casas, A.; Velasco-Rodríguez, D.; Llamas-Sillero, P.; Jiménez-Morales, A.; Esteban, J. A New Antibiotic-Loaded Sol-Gel can Prevent Bacterial Intravenous Catheter-Related Infections. Materials 2020, 13, 2946. [Google Scholar] [CrossRef]
- Romera, D.; Toirac, B.; Aguilera-Correa, J.-J.; García-Casas, A.; Mediero, A.; Jiménez-Morales, A.; Esteban, J. A Biodegradable Antifungal-Loaded Sol–Gel Coating for the Prevention and Local Treatment of Yeast Prosthetic-Joint Infections. Materials 2020, 13, 3144. [Google Scholar] [CrossRef]
- Poggioli, R.; Ueta, C.B.; Drigo, R.A.E.; Castillo, M.; Fonseca, T.L.; Bianco, A.C. Dexamethasone reduces energy expenditure and increases susceptibility to diet-induced obesity in mice. Obesity 2013, 21, E415–E420. [Google Scholar] [CrossRef] [Green Version]
- Lazzarini, L.; Manfrin, V.; De Lalla, F. Candidal prosthetic hip infection in a patient with previous candidal septic arthritis. J. Arthroplast. 2004, 19, 248–252. [Google Scholar] [CrossRef]
- Hwang, B.-H.; Yoon, J.-Y.; Nam, C.-H.; Jung, K.-A.; Lee, S.-C.; Han, C.-D.; Moon, S.-H. Fungal peri-prosthetic joint infection after primary total knee replacement. J. Bone Jt. Surg. Br. Vol. 2012, 94, 656–659. [Google Scholar] [CrossRef]
- Dale, H.; Fenstad, A.M.; Hallan, G.; Havelin, L.I.; Furnes, O.; Overgaard, S.; Pedersen, A.B.; Kärrholm, J.; Garellick, G.; Pulkkinen, P.; et al. Increasing risk of prosthetic joint infection after total hip arthroplasty. Acta Orthop. 2012, 83, 449–458. [Google Scholar] [CrossRef] [Green Version]
- Aguilera-Correa, J.J.; Garcia-Casas, A.; Mediero, A.; Romera, D.; Mulero, F.; Cuevas-López, I.; Jiménez-Morales, A.; Esteban, J. A New Antibiotic-Loaded Sol-Gel Can Prevent Bacterial Prosthetic Joint Infection: From in vitro Studies to an in vivo Model. Front. Microbiol. 2020, 10, 2935. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.-J.; Huh, J.; Odrobina, R.; Kim, J.H. Systemic Review of Published Literature on Candida Infection Following Total Hip Arthroplasty. Mycopathology 2014, 179, 173–185. [Google Scholar] [CrossRef]
- Baker, D.G. Natural Pathogens of Laboratory Mice, Rats, and Rabbits and Their Effects on Research. Clin. Microbiol. Rev. 1998, 11, 231–266. [Google Scholar] [CrossRef] [Green Version]
- Wright, A.M.; Mody, D.R.; Anton, R.C.; Schwartz, M.R. Aberrant staining with Grocott’s methenamine silver: Utility beyond fungal organisms. J. Am. Soc. Cytopathol. 2017, 6, 223–227. [Google Scholar] [CrossRef]
- Cobo, F.; Rodríguez-Granger, J.; López, E.M.; Jiménez, G.; Sampedro, A.; Aliaga-Martínez, L.; Navarro-Marí, J.M. Candida-induced prosthetic joint infection. A literature review including 72 cases and a case report. Infect. Dis. 2016, 49, 81–94. [Google Scholar] [CrossRef]
- Riaz, T.; Tande, A.J.; Steed, L.L.; Demos, H.A.; Salgado, C.D.; Osmon, D.R.; Marculescu, C.E. Risk Factors for Fungal Prosthetic Joint Infection. J. Bone Jt. Infect. 2020, 5, 76–81. [Google Scholar] [CrossRef] [Green Version]
- Grasso, R.J.; West, L.A.; Guay, R.C.; Klein, T.W. Inhibition of Yeast Phagocytosis by Dexamethasone in Macrophage Cultures: Reversibility of the Effect and Enhanced Suppression in Cultures of Stimulated Macrophages. J. Immunopharmacol. 1982, 4, 265–278. [Google Scholar] [CrossRef]
- Swartjes, J.J.T.M.; Sharma, P.K.; Van Kooten, T.G.; Van Der Mei, H.C.; Mahmoudi, M.; Busscher, H.J.; Rochford, E.T.J. Current Developments in Antimicrobial Surface Coatings for Biomedical Applications. Curr. Med. Chem. 2015, 22, 2116–2129. [Google Scholar] [CrossRef] [Green Version]
- Civantos, A.; Martínez-Campos, E.; Ramos, V.; Elvira, C.; Gallardo, A.; Abarrategi, A. Titanium Coatings and Surface Modifications: Toward Clinically Useful Bioactive Implants. ACS Biomater. Sci. Eng. 2017, 3, 1245–1261. [Google Scholar] [CrossRef]
- Tsiapalis, D.; De Pieri, A.; Biggs, M.; Pandit, A.; Zeugolis, D.I. Biomimetic Bioactive Biomaterials: The Next Generation of Implantable Devices. ACS Biomater. Sci. Eng. 2016, 3, 1172–1174. [Google Scholar] [CrossRef] [Green Version]
- Li, K.; Liu, S.; Hu, T.; Razanau, I.; Wu, X.; Ao, H.; Huang, L.; Xie, Y.; Zheng, X. Optimized Nanointerface Engineering of Micro/Nanostructured Titanium Implants to Enhance Cell–Nanotopography Interactions and Osseointegration. ACS Biomater. Sci. Eng. 2020, 6, 969–983. [Google Scholar] [CrossRef]
- Siedenbiedel, F.; Tiller, J.C. Antimicrobial Polymers in Solution and on Surfaces: Overview and Functional Principles. Polymer 2012, 4, 46–71. [Google Scholar] [CrossRef] [Green Version]
- Botequim, D.; Maia, J.; Lino, M.; Lopes, L.M.F.; Simões, P.N.; Ilharco, L.; Ferreira, L. Nanoparticles and Surfaces Presenting Antifungal, Antibacterial and Antiviral Properties. Langmuir 2012, 28, 7646–7656. [Google Scholar] [CrossRef]
- Phelan, D.M.; Osmon, D.R.; Keating, M.R.; Hanssen, A.D. Delayed Reimplantation Arthroplasty for Candidal Prosthetic Joint Infection: A Report of 4 Cases and Review of the Literature. Clin. Infect. Dis. 2002, 34, 930–938. [Google Scholar] [CrossRef] [Green Version]
- Arenas, M.A.; Pérez-Jorge, C.; Conde, A.; Matykina, E.; Hernández-López, J.M.; Perez-Tanoira, R.; de Damborenea, J.J.; Gómez-Barrena, E.; Esteban, J. Doped TiO2 anodic layers of enhanced antibacterial properties. Colloids Surfaces B Biointerfaces 2013, 105, 106–112. [Google Scholar] [CrossRef]
- Walzer, P.D.; Runck, J.; Steele, P.; White, M.; Linke, M.J.; Sidman, C.L. Immunodeficient and immunosuppressed mice as models to test anti-Pneumocystis carinii drugs. Antimicrob. Agents Chemother. 1997, 41, 251–258. [Google Scholar] [CrossRef] [Green Version]
- Slate, A.R.; Bandyopadhyay, S.; Francis, K.P.; Papich, M.G.; Karolewski, B.; Hod, E.A.; Prestia, K.A. Efficacy of Enrofloxacin in a Mouse Model of Sepsis. J. Am. Assoc. Lab. Anim. Sci. 2014, 53, 381–386. [Google Scholar] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Esteban, J.; Gomez-Barrena, E.; Cordero, J.; Martín-De-Hijas, N.Z.; Kinnari, T.J.; Fernandez-Roblas, R. Evaluation of Quantitative Analysis of Cultures from Sonicated Retrieved Orthopedic Implants in Diagnosis of Orthopedic Infection. J. Clin. Microbiol. 2008, 46, 488–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grocott, B.R.G. A Stain for Fungi in Tissue Sections and Smears. Am. J. Clin. Pathol. 1955, 25, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Mediero, A.; Frenkel, S.R.; Wilder, T.; He, W.; Mazumder, A.; Cronstein, B.N. Adenosine A2A Receptor Activation Prevents Wear Particle-Induced Osteolysis. Sci. Transl. Med. 2012, 4, 135ra65. [Google Scholar] [CrossRef] [Green Version]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garlito-Díaz, H.; Esteban, J.; Mediero, A.; Carias-Cálix, R.A.; Toirac, B.; Mulero, F.; Faus-Rodrigo, V.; Jiménez-Morales, A.; Calvo, E.; Aguilera-Correa, J.J. A New Antifungal-Loaded Sol-Gel Can Prevent Candida albicans Prosthetic Joint Infection. Antibiotics 2021, 10, 711. https://doi.org/10.3390/antibiotics10060711
Garlito-Díaz H, Esteban J, Mediero A, Carias-Cálix RA, Toirac B, Mulero F, Faus-Rodrigo V, Jiménez-Morales A, Calvo E, Aguilera-Correa JJ. A New Antifungal-Loaded Sol-Gel Can Prevent Candida albicans Prosthetic Joint Infection. Antibiotics. 2021; 10(6):711. https://doi.org/10.3390/antibiotics10060711
Chicago/Turabian StyleGarlito-Díaz, Hugo, Jaime Esteban, Aranzazu Mediero, Rafael Alfredo Carias-Cálix, Beatriz Toirac, Francisca Mulero, Víctor Faus-Rodrigo, Antonia Jiménez-Morales, Emilio Calvo, and John Jairo Aguilera-Correa. 2021. "A New Antifungal-Loaded Sol-Gel Can Prevent Candida albicans Prosthetic Joint Infection" Antibiotics 10, no. 6: 711. https://doi.org/10.3390/antibiotics10060711






