Fungal Biofilms as a Valuable Target for the Discovery of Natural Products That Cope with the Resistance of Medically Important Fungi—Latest Findings
Abstract
:1. Introduction
1.1. Most Common Etiological Agents Causing Fungal Infections
1.2. Available Antifungal Agents
1.3. Fungal Biofilms
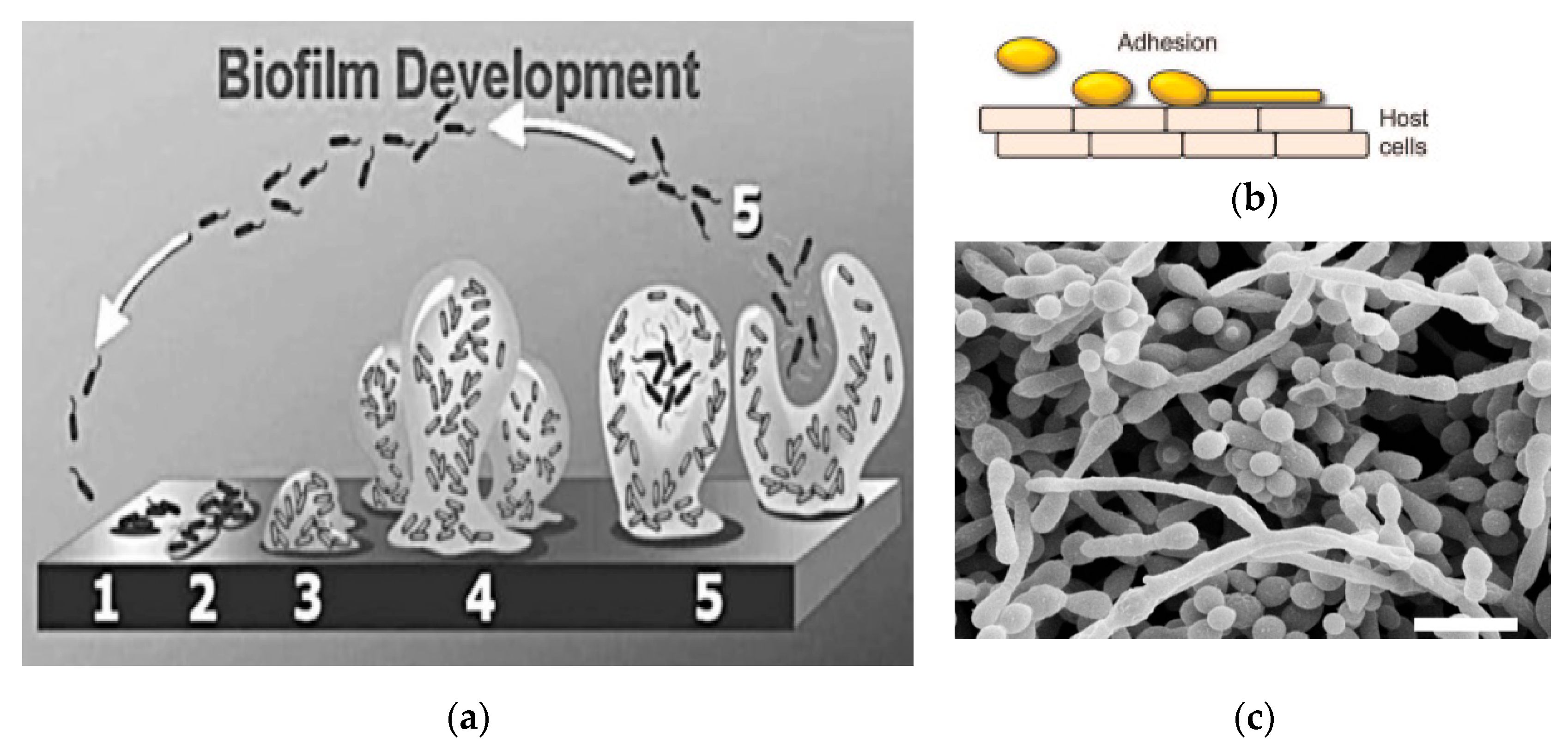
1.4. Stages in the Development of Biofifilms
1.5. Factors and Mechanisms Associated with Biofilm Resistance
1.6. Methodologies to Assess Antibiofilm Activity
1.7. Natural Products as an Important Source of Antifungal Drugs
2. Reported Antibiofilm Activities of EOs, Propolis and Extracts from Plants, Algae and Cyanobacteria
3. Reported Antibiofilm Activities of Pure Natural Compounds
4. Reported Antibiofilm Activities of Nanosystems Containing Natural Products
5. Discussion
6. Conclusions and Perspectives
7. Materials and Methods
Author Contributions
Funding
Conflicts of Interest
References
- Pathakumari, B.; Liang, G.; Liu, W. Immune defence to invasive fungal infections: A comprehensive review. Biomed. Pharmacother. 2020, 130, 110550. [Google Scholar] [CrossRef]
- Wuyts, J.; Van Dijck, P.; Holtappels, M. Fungal persister cells: The basis for recalcitrant infections? PLoS Path. 2018, 14, e1007301. [Google Scholar] [CrossRef] [PubMed]
- Nicola, A.M.; Albuquerque, P.; Paes, H.C.; Fernandes, L.; Costa, F.F.; Kioshima, E.S.; Abadio, A.K.R.; Bocca, A.L.; Felipe, M.S. Antifungal drugs: New insights in research & development. Pharmacol. Ther. 2019, 195, 21–38. [Google Scholar] [PubMed]
- Kullberg, B.J.; Vasquez, J.; Mootsikapun, P.; Nucci, M.; Paiva, J.-A.; Garbino, J.; Yan, J.L.; Aram, J.; Capparella, M.R.; Conte, U. Efficacy of anidulafungin in 539 patients with invasive candidiasis: A patient-level pooled analysis of six clinical trials. J. Antimicrob. Chemother. 2017, 72, 2368–2377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, D.W. Global and multi-national prevalence of fungal diseases—Estimate precision. J. Fungi 2017, 3, 57. [Google Scholar] [CrossRef]
- Prasad, R.; Nair, R.; Banerjee, A. Multidrug transporters of Candida species in clinical azole resistance. Fungal Genet. Biol. 2019, 132, 103252. [Google Scholar] [CrossRef] [PubMed]
- Arastehfar, A.; Gabaldón, T.; Garcia-Rubio, R.; Jenks, J.D.; Hoenigl, M.; Salzer, H.J.F.; Ilkit, M.; Lass-Flörl, C.; Perlin, D.S. Drug-resistant fungi: An emerging challenge threatening our limited antifungal armamentarium. Antibiotics 2020, 9, 877. [Google Scholar] [CrossRef] [PubMed]
- Di Mambro, T.; Guerriero, I.; Aurisicchio, L.; Magnani, M.; Marra, E. The yin and yang of current antifungal therapeutic strategies: How can we harness our natural defenses? Front. Pharmacol. 2019, 10, 80. [Google Scholar] [CrossRef] [Green Version]
- Wu, S.; Wang, Y.; Liu, N.; Dong, G.; Sheng, C. Tackling fungal resistance by biofilm inhibitors. J. Med. Chem. 2017, 60, 2193–2211. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Diekema, D.J. Epidemiology of invasive candidiasis: A persistent public health problem. Clin. Microbiol. Rev. 2007, 20, 133–163. [Google Scholar] [CrossRef] [Green Version]
- Borjian Boroujeni, Z.; Shamsaei, S.; Yarahmadi, M.; Getso, M.I.; Salimi Khorashad, A.; Haghighi, L.; Raissi, V.; Zareei, M.; Saleh Mohammadzade, A.; Moqarabzadeh, V.; et al. Distribution of invasive fungal infections: Molecular epidemiology, etiology, clinical conditions, diagnosis and risk factors: A 3-year experience with 490 patients under intensive care. Microb. Pathog. 2021, 152, 104616. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, M.W.; Walsh, T.J. Drug development challenges and strategies to address emerging and resistant fungal pathogens. Expert Rev. Anti Infect. Ther. 2017, 15, 577–584. [Google Scholar] [CrossRef]
- Wall, G.; Lopez-Ribot, J.L. Current antimycotics, new prospects, and future approaches to antifungal therapy. Antibiotics 2020, 9, 445. [Google Scholar] [CrossRef] [PubMed]
- Enoch, D.A.; Yang, H.; Aliyu, S.H.; Micallef, C. The Changing Epidemiology of Invasive Fungal Infections; Lion, T., Ed.; Humana Press: New York, NY, USA, 2017; Volume 1508, pp. 17–65. [Google Scholar]
- Campoy, S.; Adrio, J.L. Antifungals. Biochem. Pharmacol. 2017, 133, 86–96. [Google Scholar] [CrossRef] [PubMed]
- Gintjee, T.J.; Donnelley, M.A.; Thompson, G.R. Aspiring antifungals: Review of current antifungal pipeline developments. J. Fungi 2020, 6, 28. [Google Scholar] [CrossRef] [Green Version]
- Jha, A.; Vimal, A.; Kumar, A. Target shortage and less explored multiple targeting: Hurdles in the development of novel antifungals but overcome/addressed effectively through structural bioinformatics. Brief. Bioinform. 2021, 22, bbaa343. [Google Scholar] [CrossRef]
- Grela, E.; Piet, M.; Luchowski, R.; Grudzinski, W.; Paduch, R.; Gruszecki, W.I. Imaging of human cells exposed to an antifungal antibiotic amphotericin B reveals the mechanisms associated with the drug toxicity and cell defence. Sci. Rep. 2018, 8, 1–7. [Google Scholar] [CrossRef]
- Grela, E.; Wieczór, M.; Luchowski, R.; Zielinska, J.; Barzycka, A.; Grudzinski, W.; Nowak, K.; Tarkowski, P.; Czub, J.; Gruszecki, W.I. Mechanism of binding of antifungal antibiotic amphotericin B to lipid membranes: An insight from combined single-membrane imaging, microspectroscopy, and molecular dynamics. Mol. Pharm. 2018, 15, 4202–4213. [Google Scholar] [CrossRef]
- Grela, E.; Zdybicka-Barabas, A.; Pawlikowska-Pawlega, B.; Cytrynska, M.; Wlodarczyk, M.; Grudzinski, W.; Luchowski, R.; Gruszecki, W.I. Modes of the antibiotic activity of amphotericin B against Candida albicans. Sci. Rep. 2019, 9, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Silva, L.N.; Oliveira, S.S.; Magalhães, L.B.; Andrade Neto, V.V.; Torres-Santos, E.C.; Carvalho, M.D.; Pereira, M.D.; Branquinha, M.H.; Santos, A.L. Unmasking the amphotericin B resistance mechanisms in Candida haemulonii species complex. ACS Infect. Dis. 2020, 6, 1273–1282. [Google Scholar] [CrossRef]
- Ellsworth, M.; Ostrosky-Zeichner, L. Isavuconazole: Mechanism of action, clinical efficacy, and resistance. J. Fungi 2020, 6, 324. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Espeisse, O. Antimicrobial resistance. N. Engl. J. Med. 1994 2020, 17, 330–333. [Google Scholar]
- Saunte, D.M.; Hare, R.K.; Jørgensen, K.M.; Jørgensen, R.; Deleuran, M.; Zachariae, C.O.; Thomsen, S.F.; Bjørnskov-Halkier, L.; Kofoed, K.; Arendrup, M.C. Emerging terbinafine resistance in Trichophyton: Clinical characteristics, squalene epoxidase gene mutations, and a reliable EUCAST method for detection. Antimicrob. Agents Chemother. 2019, 63, e01126-19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Łagowski, D.; Gnat, S.; Nowakiewicz, A.; Osińska, M.; Dyląg, M. Intrinsic resistance to terbinafine among human and animal isolates of Trichophyton mentagrophytes related to amino acid substitution in the squalene epoxidase. Infection 2020, 48, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Nowosielski, M.; Hoffmann, M.; Wyrwicz, L.S.; Stepniak, P.; Plewczynski, D.M.; Lazniewski, M.; Ginalski, K.; Rychlewski, L. Detailed mechanism of squalene epoxidase inhibition by terbinafine. J. Chem. Inf. Model. 2011, 51, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Lima, S.L.; Colombo, A.L.; de Almeida Junior, J.N. Fungal cell wall: Emerging antifungals and drug resistance. Front. Microbiol. 2019, 10, 2573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cortés, J.C.G.; Curto, M.-Á.; Carvalho, V.S.; Pérez, P.; Ribas, J.C. The fungal cell wall as a target for the development of new antifungal therapies. Biotechnol. Adv. 2019, 37, 107352. [Google Scholar] [CrossRef]
- Khalifa, H.O.; Majima, H.; Watanabe, A.; Kamei, K. In vitro characterization of twenty-one antifungal combinations against echinocandin-resistant and-susceptible Candida glabrata. J. Fungi 2021, 7, 108. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Sae-Tia, S.; Fries, B.C. Candidiasis and mechanisms of antifungal resistance. Antibiotics 2020, 9, 312. [Google Scholar] [CrossRef]
- Ueda, Y.; Tahara, Y.O.; Miyata, M.; Ogita, A.; Yamaguchi, Y.; Tanaka, T.; Fujita, K.-i. Involvement of a multidrug efflux pump and alterations in cell surface structure in the synergistic antifungal activity of nagilactone E and anethole against budding yeast Saccharomyces cerevisiae. Antibiotics 2021, 10, 537. [Google Scholar] [CrossRef] [PubMed]
- Freitas e Silva, K.S.; C Silva, L.; Gonçales, R.A.; Neves, B.J.; Soares, C.; Pereira, M. Setting new routes for antifungal drug discovery against pathogenic fungi. Curr. Pharm. Des. 2020, 26, 1509–1520. [Google Scholar] [CrossRef]
- Lee, Y.; Puumala, E.; Robbins, N.; Cowen, L.E. Antifungal drug resistance: Molecular mechanisms in Candida albicans and beyond. Chem. Rev. 2020, 121, 3390–3411. [Google Scholar] [CrossRef]
- Caldeirão, A.C.M.; Araujo, H.C.; Tomasella, C.M.; Sampaio, C.; dos Santos Oliveira, M.J.; Ramage, G.; Pessan, J.P.; Monteiro, D.R. Effects of antifungal carriers based on chitosan-coated Iron oxide nanoparticles on microcosm biofilms. Antibiotics 2021, 10, 588. [Google Scholar] [CrossRef]
- Cerqueira, F.; Maia, M.; Gabriel, C.; Medeiros, R.; Cravo, S.; Ribeiro, A.I.; Dantas, D.; Dias, A.M.; Saraiva, L.; Raimundo, L.; et al. Mechanism of antifungal activity by 5-aminoimidazole-4-carbohydrazonamide derivatives against Candida albicans and Candida krusei. Antibiotics 2021, 10, 183. [Google Scholar] [CrossRef]
- Fuentefria, A.M.; Pippi, B.; Dalla Lana, D.F.; Donato, K.K.; de Andrade, S.F. Antifungals discovery: An insight into new strategies to combat antifungal resistance. Lett. Appl. Microbiol. 2018, 66, 2–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jenks, J.D.; Cornely, O.A.; Chen, S.C.A.; Thompson III, G.R.; Hoenigl, M. Breakthrough invasive fungal infections: Who is at risk? Mycoses 2020, 63, 1021–1032. [Google Scholar] [CrossRef]
- Katragkou, A.; Roilides, E.; Walsh, T.J. Role of echinocandins in fungal biofilm–related disease: Vascular catheter–related infections, immunomodulation, and mucosal surfaces. Clin. Infect. Dis. 2015, 61, S622–S629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fanning, S.; Mitchell, A.P. Fungal biofilms. PLoS Path. 2012, 8, e1002585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tits, J.; Cammue, B.; Thevissen, K. Combination therapy to treat fungal biofilm-based infections. Int. J. Mol. Sci. 2020, 21, 8873. [Google Scholar] [CrossRef]
- Oliveira, L.T.; Lopes, L.G.; Ramos, S.B.; Martins, C.H.G.; Jamur, M.C.; Pires, R.H. Fungal biofilms in the hemodialysis environment. Microb. Pathog. 2018, 123, 206–212. [Google Scholar] [CrossRef]
- Rodrigues, M.E.; Gomes, F.; Rodrigues, C.F. Candida spp./bacteria mixed biofilms. J. Fungi 2020, 6, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirota, K.; Yumoto, H.; Sapaar, B.; Matsuo, T.; Ichikawa, T.; Miyake, Y. Pathogenic factors in Candida biofilm--related infectious diseases. J. Appl. Microbiol. 2017, 122, 321–330. [Google Scholar] [CrossRef]
- Mitchell, K.F.; Zarnowski, R.; Andes, D.R. Fungal super glue: The biofilm matrix and its composition, assembly, and functions. Plos Path. 2016, 12, e1005828. [Google Scholar] [CrossRef] [Green Version]
- Al-Fattani, M.A.; Douglas, L.J. Biofilm matrix of Candida albicans and Candida tropicalis: Chemical composition and role in drug resistance. J. Med. Microbiol. 2006, 55, 999–1008. [Google Scholar] [CrossRef] [PubMed]
- Zarnowski, R.; Westler, W.M.; Lacmbouh, G.A.; Marita, J.M.; Bothe, J.R.; Bernhardt, J.; Lounes-Hadj Sahraoui, A.; Fontaine, J.; Sanchez, H.; Hatfield, R.D. Novel entries in a fungal biofilm matrix encyclopedia. MBio 2014, 5, e01333-14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodrigues, C.F.; Henriques, M. Portrait of matrix gene expression in Candida glabrata biofilms with stress induced by different drugs. Genes 2018, 9, 205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, C.R.; Costa, P.A.; Vieira, P.S.; Gonzalez, S.E.; Correa, T.L.; Lima, E.A.; Mandelli, F.; Pirolla, R.A.; Domingues, M.N.; Cabral, L. Structural insights into β-1, 3-glucan cleavage by a glycoside hydrolase family. Nat. Chem. Biol. 2020, 16, 920–929. [Google Scholar] [CrossRef]
- Stoodley, P.; Sauer, K.; Davies, D.G.; Costerton, J.W. Biofilms as complex differentiated communities. Annu. Rev. Microbiol. 2002, 56, 187–209. [Google Scholar] [CrossRef] [Green Version]
- Ramage, G.; Saville, S.P.; Thomas, D.P.; Lopez-Ribot, J.L. Candida biofilms: An update. Eukaryot. Cell 2005, 4, 633–638. [Google Scholar] [CrossRef] [Green Version]
- Mayer, F.L.; Wilson, D.; Hube, B. Candida albicans pathogenicity mechanisms. Virulence 2013, 4, 119–128. [Google Scholar] [CrossRef] [Green Version]
- Lohse, M.B.; Gulati, M.; Johnson, A.D.; Nobile, C.J. Development and regulation of single-and multi-species Candida albicans biofilms. Nat. Rev. Microbiol. 2018, 16, 19–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alim, D.; Sircaik, S.; Panwar, S.L. The significance of lipids to biofilm formation in Candida albicans: An emerging perspective. J. Fungi 2018, 4, 140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pimentel de Barros, P.; Rossoni, R.D.; de Souza, C.M.; Scorzoni, L.; Fenley, J.D.C.; Junqueira, J.C. Candida biofilms: An update on developmental mechanisms and therapeutic challenges. Mycopathologia 2020, 185, 415–424. [Google Scholar] [CrossRef] [PubMed]
- McCall, A.D.; Pathirana, R.U.; Prabhakar, A.; Cullen, P.J.; Edgerton, M. Candida albicans biofilm development is governed by cooperative attachment and adhesion maintenance proteins. NPJ Biofilms Microbiomes 2019, 5, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Eix, E.F.; Nett, J.E. How biofilm growth affects candida-host interactions. Front. Microbiol. 2020, 11, 1437. [Google Scholar] [CrossRef]
- Uppuluri, P.; Acosta Zaldívar, M.; Anderson, M.Z.; Dunn, M.J.; Berman, J.; Lopez Ribot, J.L.; Köhler, J.R. Candida albicans dispersed cells are developmentally distinct from biofilm and planktonic cells. MBio 2018, 9, e01338-18. [Google Scholar] [CrossRef] [Green Version]
- Wall, G.; Montelongo-Jauregui, D.; Bonifacio, B.V.; Lopez-Ribot, J.L.; Uppuluri, P. Candida albicans biofilm growth and dispersal: Contributions to pathogenesis. Curr. Opin. Microbiol. 2019, 52, 1–6. [Google Scholar] [CrossRef]
- Mehmood, A.; Liu, G.; Wang, X.; Meng, G.; Wang, C.; Liu, Y. Fungal quorum-sensing molecules and inhibitors with potential antifungal activity: A review. Molecules 2019, 24, 1950. [Google Scholar] [CrossRef] [Green Version]
- Kovács, R.; Majoros, L. Fungal quorum-sensing molecules: A review of their antifungal effect against Candida biofilms. J. Fungi 2020, 6, 99. [Google Scholar] [CrossRef]
- Barriuso, J.; Hogan, D.A.; Keshavarz, T.; Martínez, M.J. Role of quorum sensing and chemical communication in fungal biotechnology and pathogenesis. Fems Microbiol. Rev. 2018, 42, 627–638. [Google Scholar] [CrossRef]
- Rodrigues, C.F.; Černáková, L. Farnesol and tyrosol: Secondary metabolites with a crucial quorum-sensing role in Candida biofilm development. Genes 2020, 11, 444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padder, S.A.; Prasad, R.; Shah, A.H. Quorum sensing: A less known mode of communication among fungi. Microbiol. Res. 2018, 210, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Zawrotniak, M.; Wojtalik, K.; Rapala-Kozik, M. Farnesol, a quorum-sensing molecule of Candida albicans triggers the release of neutrophil extracellular traps. Cells 2019, 8, 1611. [Google Scholar] [CrossRef] [Green Version]
- Kean, R.; Delaney, C.; Sherry, L.; Borman, A.; Johnson, E.M.; Richardson, M.D.; Rautemaa-Richardson, R.; Williams, C.; Ramage, G. Transcriptome assembly and profiling of Candida auris reveals novel insights into biofilm-mediated resistance. Msphere 2018, 3, e00334-18. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, C.F.; Rodrigues, M.E.; Silva, S.; Henriques, M. Candida glabrata biofilms: How far have we come? J. Fungi 2017, 3, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, C.; Liu, J.; Li, W.; Zhao, Y.; Meng, L.; Xiang, M. Expression of fluconazole resistance-associated genes in biofilm from 23 clinical isolates of Candida albicans. Braz. J. Microbiol. 2019, 50, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Chaabane, F.; Graf, A.; Jequier, L.; Coste, A.T. Review on antifungal resistance mechanisms in the emerging pathogen Candida auris. Front. Microbiol. 2019, 10, 2788. [Google Scholar] [CrossRef] [PubMed]
- Deng, K.; Jiang, W.; Jiang, Y.; Deng, Q.; Cao, J.; Yang, W.; Zhao, X. ALS3 expression as an indicator for Candida albicans biofilm formation and drug resistance. Front. Microbiol. 2021, 12, 655242. [Google Scholar] [CrossRef]
- Chong, P.P.; Chin, V.K.; Wong, W.F.; Madhavan, P.; Yong, V.C.; Looi, C.Y. Transcriptomic and genomic approaches for unravelling Candida albicans biofilm formation and drug resistance—An update. Genes 2018, 9, 540. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.-H.; Kim, Y.-G.; Gupta, V.K.; Manoharan, R.K.; Lee, J. Suppression of fluconazole resistant Candida albicans biofilm formation and filamentation by methylindole derivatives. Front. Microbiol. 2018, 9, 2641. [Google Scholar] [CrossRef] [PubMed]
- Sasani, E.; Khodavaisy, S.; Rezaie, S.; Salehi, M.; Yadegari, M.H. The relationship between biofilm formation and mortality in patients with Candida tropicalis candidemia. Microb. Pathog. 2021, 155, 104889. [Google Scholar] [CrossRef]
- Vega-Chacón, Y.; de Albuquerque, M.C.; Pavarina, A.C.; Goldman, G.H.; Mima, E.G.d.O. Verapamil inhibits efflux pumps in Candida albicans, exhibits synergism with fluconazole, and increases survival of Galleria mellonella. Virulence 2021, 12, 231–243. [Google Scholar] [CrossRef]
- Beauvais, A.; Schmidt, C.; Guadagnini, S.; Roux, P.; Perret, E.; Henry, C.; Paris, S.; Mallet, A.; Prévost, M.C.; Latgé, J.P. An extracellular matrix glues together the aerial--grown hyphae of Aspergillus fumigatus. Cell. Microbiol. 2007, 9, 1588–1600. [Google Scholar] [CrossRef] [PubMed]
- Córdova-Alcántara, I.M.; Venegas-Cortés, D.L.; Martínez-Rivera, M.Á.; Pérez, N.O.; Rodriguez-Tovar, A.V. Biofilm characterization of Fusarium solani keratitis isolate: Increased resistance to antifungals and UV light. J. Microbiol. 2019, 57, 485–497. [Google Scholar] [CrossRef]
- Nett, J.E.; Sanchez, H.; Cain, M.T.; Andes, D.R. Genetic basis of Candida biofilm resistance due to drug-sequestering matrix glucan. Jinfect. Dis. 2010, 202, 171–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuhn, D.; George, T.; Chandra, J.; Mukherjee, P.; Ghannoum, M. Antifungal susceptibility of Candida biofilms: Unique efficacy of amphotericin B lipid formulations and echinocandins. Antimicrob. Agents Chemother. 2002, 46, 1773–1780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mukherjee, P.K.; Chandra, J.; Kuhn, D.M.; Ghannoum, M.A. Mechanism of fluconazole resistance in Candida albicans biofilms: Phase-specific role of efflux pumps and membrane sterols. Infect. Immun. 2003, 71, 4333–4340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, X.; Zhang, S.; Xu, X.; Shen, L.; Xu, B.; Qu, W.; Zhuang, W.; Locock, K.; Deighton, M.; Qu, Y. RAFT-derived polymethacrylates as a superior treatment for recurrent vulvovaginal candidiasis by targeting biotic biofilms and persister cells. Front. Microbiol. 2019, 10, 2592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- da Silva, M.A.; Baronetti, J.L.; Páez, P.L.; Paraje, M.G. Oxidative imbalance in Candida tropicalis biofilms and its relation with persister cells. Front. Microbiol. 2021, 11, 598834. [Google Scholar] [CrossRef] [PubMed]
- Lewis, K. Persister cells, dormancy and infectious disease. Nat. Rev. Microbiol. 2007, 5, 48–56. [Google Scholar] [CrossRef]
- Wu, X.; Zhang, S.; Li, H.; Shen, L.; Dong, C.; Sun, Y.; Chen, H.; Xu, B.; Zhuang, W.; Deighton, M. Biofilm formation of Candida albicans facilitates fungal infiltration and persister cell formation in vaginal candidiasis. Front. Microbiol. 2020, 11, 1117. [Google Scholar] [CrossRef] [PubMed]
- Galdiero, E.; de Alteriis, E.; De Natale, A.; D’Alterio, A.; Siciliano, A.; Guida, M.; Lombardi, L.; Falanga, A.; Galdiero, S. Eradication of Candida albicans persister cell biofilm by the membranotropic peptide gH625. Sci. Rep. 2020, 10, 5780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- K Redhu, A.; Shah, A.H.; Prasad, R. MFS transporters of Candida species and their role in clinical drug resistance. Fems Yeast Res. 2016, 16, fow043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, N.; Li, D.; Fonzi, W.; Li, X.; Zhang, L.; Calderone, R. Multidrug-resistant transporter Mdr1p-mediated uptake of a novel antifungal compound. Antimicrob. Agents Chemother. 2013, 57, 5931–5939. [Google Scholar] [CrossRef] [Green Version]
- Van Acker, H.; Van Dijck, P.; Coenye, T. Molecular mechanisms of antimicrobial tolerance and resistance in bacterial and fungal biofilms. Trends Microbiol. 2014, 22, 326–333. [Google Scholar] [CrossRef]
- García-Sánchez, S.; Aubert, S.; Iraqui, I.; Janbon, G.; Ghigo, J.-M.; d’Enfert, C. Candida albicans biofilms: A developmental state associated with specific and stable gene expression patterns. Eukaryot. Cell 2004, 3, 536–545. [Google Scholar] [CrossRef] [Green Version]
- Dižová, S.; Černáková, L.; Bujdáková, H. The impact of farnesol in combination with fluconazole on Candida albicans biofilm: Regulation of ERG20, ERG9, and ERG11 genes. Folia Microbiol. 2018, 63, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Alizadeh, F.; Khodavandi, A.; Esfandyari, S.; Nouripour-Sisakht, S. Analysis of ergosterol and gene expression profiles of sterol∆ 5, 6-desaturase (ERG3) and lanosterol 14α-demethylase (ERG11) in Candida albicans treated with carvacrol. J. Herbmed Pharmacol. 2018, 7, 79–87. [Google Scholar] [CrossRef] [Green Version]
- Fattouh, N.; Hdayed, D.; Geukgeuzian, G.; Tokajian, S.; Khalaf, R.A. Molecular mechanism of fluconazole resistance and pathogenicity attributes of Lebanese Candida albicans hospital isolates. Fungal Genet. Biol. 2021, 153, 103575. [Google Scholar] [CrossRef]
- Fernandes, T.; Silva, S.; Henriques, M. Effect of voriconazole on Candida tropicalis biofilms: Relation with ERG genes expression. Mycopathologia 2016, 181, 643–651. [Google Scholar] [CrossRef] [Green Version]
- Nailis, H.; Vandenbosch, D.; Deforce, D.; Nelis, H.J.; Coenye, T. Transcriptional response to fluconazole and amphotericin B in Candida albicans biofilms. Res. Microbiol. 2010, 161, 284–292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coenye, T.; Nelis, H.J. In vitro and in vivo model systems to study microbial biofilm formation. J. Microbiol. Methods 2010, 83, 89–105. [Google Scholar] [CrossRef]
- Pierce, C.G.; Uppuluri, P.; Tristan, A.R.; Wormley, F.L.; Mowat, E.; Ramage, G.; Lopez-Ribot, J.L. A simple and reproducible 96-well plate-based method for the formation of fungal biofilms and its application to antifungal susceptibility testing. Nat. Protoc. 2008, 3, 1494–1500. [Google Scholar] [CrossRef]
- Stockert, J.C.; Horobin, R.W.; Colombo, L.L.; Blázquez-Castro, A. Tetrazolium salts and formazan products in cell biology: Viability assessment, fluorescence imaging, and labeling perspectives. Acta Histochem. 2018, 120, 159–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azeredo, J.; Azevedo, N.F.; Briandet, R.; Cerca, N.; Coenye, T.; Costa, A.R.; Desvaux, M.; Di Bonaventura, G.; Hébraud, M.; Jaglic, Z. Critical review on biofilm methods. Crit. Rev. Microbiol. 2017, 43, 313–351. [Google Scholar] [CrossRef] [Green Version]
- Kowalski, C.H.; Kerkaert, J.D.; Liu, K.-W.; Bond, M.C.; Hartmann, R.; Nadell, C.D.; Stajich, J.E.; Cramer, R.A. Fungal biofilm morphology impacts hypoxia fitness and disease progression. Nat. Microbiol. 2019, 4, 2430–2441. [Google Scholar] [CrossRef] [PubMed]
- Pamp, S.J.; Sternberg, C.; Tolker--Nielsen, T. Insight into the microbial multicellular lifestyle via flow--cell technology and confocal microscopy. Cytom. Part A J. Int. Soc. Anal. Cytol. 2009, 75, 90–103. [Google Scholar] [CrossRef] [PubMed]
- Shao, J.; Lu, K.; Tian, G.; Cui, Y.; Yan, Y.; Wang, T.; Zhang, X.; Wang, C. Lab-scale preparations of Candida albicans and dual Candida albicans–Candida glabrata biofilms on the surface of medical-grade polyvinyl chloride (PVC) perfusion tube using a modified gravity-supported free-flow biofilm incubator (GS-FFBI). J. Microbiol. Methods 2015, 109, 41–48. [Google Scholar] [CrossRef]
- Thieme, L.; Hartung, A.; Tramm, K.; Klinger-Strobel, M.; Jandt, K.D.; Makarewicz, O.; Pletz, M.W. MBEC versus MBIC: The lack of differentiation between biofilm reducing and inhibitory effects as a current problem in biofilm methodology. Biol. Proced. Online 2019, 21, 1–5. [Google Scholar] [CrossRef]
- Van Dijck, P.; Sjollema, J.; Cammue, B.P.; Lagrou, K.; Berman, J.; d’Enfert, C.; Andes, D.R.; Arendrup, M.C.; Brakhage, A.A.; Calderone, R. Methodologies for in vitro and in vivo evaluation of efficacy of antifungal and antibiofilm agents and surface coatings against fungal biofilms. Microb. Cell 2018, 5, 300. [Google Scholar] [CrossRef]
- Pukkila-Worley, R.; Peleg, A.Y.; Tampakakis, E.; Mylonakis, E. Candida albicans hyphal formation and virulence assessed using a Caenorhabditis elegans infection model. Eukaryot. Cell 2009, 8, 1750–1758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nett, J.E.; Andes, D.R. Fungal biofilms: In vivo models for discovery of anti--biofilm drugs. Microb. Biofilms 2015, 33–49. [Google Scholar] [CrossRef] [Green Version]
- Baria, D.; Shah, U.; Egbuna, C.; Mtewa, A.G. Secondary Metabolites and Toxins of Microbial Origin for the Treatment of Diseases; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2020; pp. 225–248. [Google Scholar]
- Huang, K.; Zhang, B.; Shen, Z.-Y.; Cai, X.; Liu, Z.-Q.; Zheng, Y.-G. Enhanced amphotericin B production by genetically engineered Streptomyces nodosus. Microbiol. Res. 2021, 242, 126623. [Google Scholar] [CrossRef] [PubMed]
- Valente, S.; Cometto, A.; Piombo, E.; Meloni, G.R.; Ballester, A.-R.; González-Candelas, L.; Spadaro, D. Elaborated regulation of griseofulvin biosynthesis in Penicillium griseofulvum and its role on conidiation and virulence. Int. J. Food Microbiol. 2020, 328, 108687. [Google Scholar] [CrossRef] [PubMed]
- Wei, T.-Y.; Wu, Y.-J.; Xie, Q.-P.; Tang, J.-W.; Yu, Z.-T.; Yang, S.-B.; Chen, S.-X. CRISPR/Cas9-based genome editing in the filamentous fungus Glarea lozoyensis and its application in manipulating gloF. ACS Synth. Biol. 2020, 9, 1968–1977. [Google Scholar] [CrossRef]
- Ebadzadsahrai, G.; Higgins Keppler, E.A.; Soby, S.D.; Bean, H.D. Inhibition of fungal growth and induction of a novel volatilome in response to Chromobacterium vaccinii volatile organic compounds. Front. Microbiol. 2020, 11, 1035. [Google Scholar] [CrossRef]
- Butts, A.; Krysan, D.J. Antifungal drug discovery: Something old and something new. Plos Pathog. 2012, 8, e1002870. [Google Scholar] [CrossRef]
- Giordani, C.; Simonetti, G.; Natsagdorj, D.; Choijamts, G.; Ghirga, F.; Calcaterra, A.; Quaglio, D.; De Angelis, G.; Toniolo, C.; Pasqua, G. Antifungal activity of Mongolian medicinal plant extracts. Nat. Prod. Res. 2020, 34, 449–455. [Google Scholar] [CrossRef]
- Oltu, I.; Cepoi, L.; Rudic, V.; Rudi, L.; Chiriac, T.; Valuta, A.; Codreanu, S. Current Research and New Perspectives in Antifungal Drug Development; Springer Nature: Cham, Switzeralnd, 2019; pp. 71–83. [Google Scholar]
- Powers, C.N.; Osier, J.L.; McFeeters, R.L.; Brazell, C.B.; Olsen, E.L.; Moriarity, D.M.; Satyal, P.; Setzer, W.N. Antifungal and cytotoxic activities of sixty commercially available essential oils. Molecules 2018, 23, 1549. [Google Scholar] [CrossRef] [Green Version]
- Dewi, I.C.; Falaise, C.; Hellio, C.; Bourgougnon, N.; Mouget, J.-L. Anticancer, Antiviral, Antibacterial, and Antifungal Properties in Microalgae; Academic Press, Elsevier: London, UK, 2018; pp. 235–261. [Google Scholar]
- Mickymaray, S.; Alturaiki, W. Antifungal efficacy of marine macroalgae against fungal isolates from bronchial asthmatic cases. Molecules 2018, 23, 3032. [Google Scholar] [CrossRef] [Green Version]
- Deshmukh, S.K.; Gupta, M.K.; Prakash, V.; Saxena, S. Endophytic fungi: A source of potential antifungal compounds. J. Fungi 2018, 4, 77. [Google Scholar] [CrossRef] [Green Version]
- Xu, L.; Meng, W.; Cao, C.; Wang, J.; Shan, W.; Wang, Q. Antibacterial and antifungal compounds from marine fungi. Mar. Drugs 2015, 13, 3479–3513. [Google Scholar] [CrossRef]
- Alves, C.T.; Ferreira, I.C.; Barros, L.; Silva, S.; Azeredo, J.; Henriques, M. Antifungal activity of phenolic compounds identified in flowers from North Eastern Portugal against Candida species. Future Microbiol. 2014, 9, 139–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seleem, D.; Pardi, V.; Murata, R.M. Review of flavonoids: A diverse group of natural compounds with anti-Candida albicans activity in vitro. Arch. Oral Biol. 2017, 76, 76–83. [Google Scholar] [CrossRef]
- Futuro, D.O.; Ferreira, P.G.; Nicoletti, C.D.; Borba-Santos, L.P.; SILVA, F.C.; Rozental, S.; Ferreira, V.F. The antifungal activity of naphthoquinones: An integrative review. An. Acad. Bras. Cienc. 2018, 90, 1187–1214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shang, Z.-C.; Han, C.; Xu, J.-L.; Liu, R.-H.; Yin, Y.; Wang, X.-B.; Yang, M.-H.; Kong, L.-Y. Twelve formyl phloroglucinol meroterpenoids from the leaves of Eucalyptus robusta. Phytochemistry 2019, 163, 111–117. [Google Scholar] [CrossRef]
- Aldholmi, M.; Marchand, P.; Ourliac-Garnier, I.; Le Pape, P.; Ganesan, A. A decade of antifungal leads from natural products: 2010–2019. Pharmaceuticals 2019, 12, 182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Girardot, M.; Imbert, C. Natural sources as innovative solutions against fungal biofilms. Fungal Biofilms Relat. Infect. 2016, 931, 105–125. [Google Scholar]
- Nazzaro, F.; Fratianni, F.; Coppola, R.; Feo, V.D. Essential oils and antifungal activity. Pharmaceuticals 2017, 10, 86. [Google Scholar] [CrossRef] [Green Version]
- Singla, R.K.; Dubey, A.K. Molecules and metabolites from natural products as inhibitors of biofilm in Candida spp. pathogens. Curr. Top. Med. Chem. 2019, 19, 2567–2578. [Google Scholar] [CrossRef]
- Song, X.; Xia, Y.-X.; He, Z.-D.; Zhang, H.-J. A review of natural products with anti-biofilm activity. Curr. Org. Chem. 2018, 22, 789–817. [Google Scholar] [CrossRef]
- Stringaro, A.; Colone, M.; Angiolella, L. Antioxidant, antifungal, antibiofilm, and cytotoxic activities of Mentha spp. essential oils. Medicines 2018, 5, 112. [Google Scholar] [CrossRef] [Green Version]
- Peixoto, L.R.; Rosalen, P.L.; Ferreira, G.L.S.; Freires, I.A.; de Carvalho, F.G.; Castellano, L.R.; de Castro, R.D. Antifungal activity, mode of action and anti-biofilm effects of Laurus nobilis Linnaeus essential oil against Candida spp. Arch. Oral Biol. 2017, 73, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Manoharan, R.K.; Lee, J.-H.; Kim, Y.-G.; Kim, S.-I.; Lee, J. Inhibitory effects of the essential oils α-longipinene and linalool on biofilm formation and hyphal growth of Candida albicans. Biofouling 2017, 33, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Serra, E.; Hidalgo-Bastida, L.A.; Verran, J.; Williams, D.; Malic, S. Antifungal activity of commercial essential oils and biocides against Candida albicans. Pathogens 2018, 7, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banu, S.F.; Rubini, D.; Shanmugavelan, P.; Murugan, R.; Gowrishankar, S.; Pandian, S.K.; Nithyanand, P. Effects of patchouli and cinnamon essential oils on biofilm and hyphae formation by Candida species. J. Mycol. Med. 2018, 28, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Bassyouni, R.H.; Wali, I.E.; Kamel, Z.; Kassim, M.F. Fennel oil: A promising antifungal agent against biofilm forming fluconazole resistant Candida albicans causing vulvovaginal candidiasis. J. Herb. Med. 2019, 15, 100227. [Google Scholar] [CrossRef]
- Sahal, G.; Woerdenbag, H.J.; Hinrichs, W.L.; Visser, A.; Tepper, P.G.; Quax, W.J.; van der Mei, H.C.; Bilkay, I.S. Antifungal and biofilm inhibitory effect of Cymbopogon citratus (lemongrass) essential oil on biofilm forming by Candida tropicalis isolates; an in vitro study. J. Ethnopharmacol. 2020, 246, 112188. [Google Scholar] [CrossRef]
- Choonharuangdej, S.; Srithavaj, T.; Thummawanit, S. Fungicidal and inhibitory efficacy of cinnamon and lemongrass essential oils on Candida albicans biofilm established on acrylic resin: An in vitro study. J. Prosthet. Dent. 2021, 125, 707-e1. [Google Scholar] [CrossRef]
- Galletti, J.; Tobaldini-Valerio, F.K.; Silva, S.; Kioshima, É.S.; Trierveiler-Pereira, L.; Bruschi, M.; Negri, M.; Estivalet Svidzinski, T.I. Antibiofilm activity of propolis extract on Fusarium species from onychomycosis. Future Microbiol. 2017, 12, 1311–1321. [Google Scholar] [CrossRef] [Green Version]
- Lainhart, W. Fusarium spp., a genus of common plant pathogens that can cause devastating, opportunistic human disease. Clin. Microbiol. Newsl. 2018, 40, 1–5. [Google Scholar] [CrossRef]
- Martorano-Fernandes, L.; Cavalcanti, Y.W.; de Almeida, L.d.F.D. Inhibitory effect of Brazilian red propolis on Candida biofilms developed on titanium surfaces. BMC Complement. Med. Ther. 2020, 20, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Sardi, J.d.C.O.; Freires, I.A.; Lazarini, J.G.; Infante, J.; de Alencar, S.M.; Rosalen, P.L. Unexplored endemic fruit species from Brazil: Antibiofilm properties, insights into mode of action, and systemic toxicity of four Eugenia spp. Microb. Pathog. 2017, 105, 280–287. [Google Scholar] [CrossRef]
- Alizadeh, F.; Khodavandi, A.; Faraji, F.S. Malva sylvestris inhibits Candida albicans biofilm formation. J. Herbmed Pharmacol. 2017, 6, 62–68. [Google Scholar]
- Silva, D.R.; Rosalen, P.L.; Freires, I.A.; Sardi, J.d.C.O.; Lima, R.F.; Lazarini, J.G.; Costa, T.K.V.L.d.; Pereira, J.V.; Godoy, G.P.; Costa, E.M.M.d.B. Anadenanthera colubrina vell Brenan: Anti-Candida and antibiofilm activities, toxicity and therapeutical action. Braz. Oral Res. 2019, 33, e023. [Google Scholar] [CrossRef] [Green Version]
- Ourabah, A.; Atmani-Kilani, D.; Debbache-Benaida, N.; Kolesova, O.; Azib, L.; Yous, F.; Benloukil, M.; Botta, B.; Atmani, D.; Simonetti, G. Anti-Candida albicans biofilm activity of extracts from two selected indigenous Algerian plants: Clematis flammula and Fraxinus angustifolia. J. Herb. Med. 2020, 20, 100319. [Google Scholar] [CrossRef]
- Dwivedi, M.; Muralidhar, S.; Saluja, D. Hibiscus sabdariffa extract inhibits adhesion, biofilm initiation and formation in Candida albicans. Indian J. Microbiol. 2020, 60, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Rahmasari, R.; Chairunissa, A.H.; Irianti, M.I.; Forestrania, R.C.; Arifianti, A.E.; Suryadi, H.; Makau, J.N.; Jantan, I.; Elya, B. Inhibitory and anti-biofilm effects of Orthoshipon aristatus against Candida albicans. Pharm. Sci. Res. 2020, 7, 2. [Google Scholar] [CrossRef]
- Millot, M.; Girardot, M.; Dutreix, L.; Mambu, L.; Imbert, C. Antifungal and anti-biofilm activities of acetone lichen extracts against Candida albicans. Molecules 2017, 22, 651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cepas, V.; López, Y.; Gabasa, Y.; Martins, C.B.; Ferreira, J.D.; Correia, M.J.; Santos, L.; Oliveira, F.; Ramos, V.; Reis, M. Inhibition of bacterial and fungal biofilm formation by 675 extracts from microalgae and cyanobacteria. Antibiotics 2019, 8, 77. [Google Scholar] [CrossRef] [Green Version]
- Liu, R.-H.; Shang, Z.-C.; Li, T.-X.; Yang, M.-H.; Kong, L.-Y. In vitro antibiofilm activity of eucarobustol E against Candida albicans. Antimicrob. Agents Chemother. 2017, 61, e02707–e02716. [Google Scholar] [CrossRef] [Green Version]
- Shi, G.; Shao, J.; Wang, T.; Wu, D.; Wang, C. Mechanism of berberine-mediated fluconazole-susceptibility enhancement in clinical fluconazole-resistant Candida tropicalis isolates. Biomed. Pharmacother. 2017, 93, 709–712. [Google Scholar] [CrossRef] [PubMed]
- Behbehani, J.; Shreaz, S.; Irshad, M.; Karched, M. The natural compound magnolol affects growth, biofilm formation, and ultrastructure of oral Candida isolates. Microb. Pathog. 2017, 113, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Kumari, P.; Mishra, R.; Arora, N.; Chatrath, A.; Gangwar, R.; Roy, P.; Prasad, R. Antifungal and anti-biofilm activity of essential oil active components against Cryptococcus neoformans and Cryptococcus laurentii. Front. Microbiol. 2017, 8, 2161. [Google Scholar] [CrossRef] [PubMed]
- Qu, J.; Zhang, X.; Lu, Y.; Liu, X.; Lv, X. Clinical analysis in immunocompetent and immunocompromised patients with pulmonary cryptococcosis in western China. Sci. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kumari, P.; Arora, N.; Chatrath, A.; Gangwar, R.; Pruthi, V.; Poluri, K.M.; Prasad, R. Delineating the biofilm inhibition mechanisms of phenolic and aldehydic terpenes against Cryptococcus neoformans. ACS Omega 2019, 4, 17634–17648. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Shi, H.; Chang, W.; Li, Y.; Zhang, M.; Qiao, Y.; Lou, H. Eudesmane sesquiterpenes from Chinese liverwort are substrates of Cdrs and display antifungal activity by targeting Erg6 and Erg11 of Candida albicans. Bioorg. Med. Chem. 2017, 25, 5764–5771. [Google Scholar] [CrossRef] [PubMed]
- Alalwan, H.; Rajendran, R.; Lappin, D.F.; Combet, E.; Shahzad, M.; Robertson, D.; Nile, C.J.; Williams, C.; Ramage, G. The anti-adhesive effect of curcumin on Candida albicans biofilms on denture materials. Front. Microbiol. 2017, 8, 659. [Google Scholar] [CrossRef]
- Lee, J.-H.; Kim, Y.-G.; Choi, P.; Ham, J.; Park, J.G.; Lee, J. Antibiofilm and antivirulence activities of 6-gingerol and 6-shogaol against Candida albicans due to hyphal inhibition. Front. Cell. Infect. Microbiol. 2018, 8, 299. [Google Scholar] [CrossRef]
- Yan, Y.; Tan, F.; Miao, H.; Wang, H.; Cao, Y. Effect of shikonin against Candida albicans biofilms. Front. Microbiol. 2019, 10, 1085. [Google Scholar] [CrossRef] [Green Version]
- Saibabu, V.; Fatima, Z.; Ahmad, K.; Khan, L.; Hameed, S. Efficiency of vanillin in impeding metabolic adaptability and virulence of Candida albicans by inhibiting glyoxylate cycle, morphogenesis, and biofilm formation. Curr. Med. Mycol. 2020, 6, 1–8. [Google Scholar]
- Kischkel, B.; Souza, G.K.; Chiavelli, L.U.R.; Pomini, A.M.; Svidzinski, T.I.E.; Negri, M. The ability of farnesol to prevent adhesion and disrupt Fusarium keratoplasticum biofilm. Appl. Microbiol. Biotechnol. 2020, 104, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Jin, X.-Y.; Zhou, J.-C.; Zhu, R.-X.; Qiao, Y.-N.; Zhang, J.-Z.; Li, Y.; Zhang, C.-Y.; Chen, W.; Chang, W.-Q. Terpenoids from the Chinese liverwort Heteroscyphus coalitus and their anti-virulence activity against Candida albicans. Phytochemistry 2020, 174, 112324. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Czuni, L.; Báló, V.; Papp, G.; Gazdag, Z.; Papp, N.; Kőszegi, T. Cytotoxic action of artemisinin and scopoletin on planktonic forms and on biofilms of Candida species. Molecules 2020, 25, 476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lemos, A.S.; Florêncio, J.R.; Pinto, N.C.; Campos, L.M.; Silva, T.P.; Grazul, R.M.; Pinto, P.F.; Tavares, G.D.; Scio, E.; Apolônio, A.C.M. Antifungal activity of the natural coumarin scopoletin against planktonic cells and biofilms from a multidrug-resistant Candida tropicalis strain. Front. Microbiol. 2020, 11, 1525. [Google Scholar] [CrossRef] [PubMed]
- Kipanga, P.N.; Liu, M.; Panda, S.K.; Mai, A.H.; Veryser, C.; Van Puyvelde, L.; De Borggraeve, W.M.; Van Dijck, P.; Matasyoh, J.; Luyten, W. Biofilm inhibiting properties of compounds from the leaves of Warburgia ugandensis Sprague subsp ugandensis against Candida and staphylococcal biofilms. J. Ethnopharmacol. 2020, 248, 112352. [Google Scholar] [CrossRef]
- Liu, Y.; Ren, H.; Wang, D.; Zhang, M.; Sun, S.; Zhao, Y. The synergistic antifungal effects of gypenosides combined with fluconazole against resistant Candida albicans via inhibiting the drug efflux and biofilm formation. Biomed. Pharmacother. 2020, 130, 110580. [Google Scholar] [CrossRef]
- Zhao, M.; Zhang, F.; Zarnowski, R.; Barns, K.; Jones, R.; Fossen, J.; Sanchez, H.; Rajski, S.R.; Audhya, A.; Bugni, T.S. Turbinmicin inhibits Candida biofilm growth by disrupting fungal vesicle–mediated trafficking. J. Clin. Investig. 2021, 131, e145123. [Google Scholar] [CrossRef]
- Zarnowski, R.; Sanchez, H.; Covelli, A.S.; Dominguez, E.; Jaromin, A.; Bernhardt, J.; Mitchell, K.F.; Heiss, C.; Azadi, P.; Mitchell, A. Candida albicans biofilm–induced vesicles confer drug resistance through matrix biogenesis. Plos Biol. 2018, 16, e2006872. [Google Scholar] [CrossRef]
- Zainal, M.; Zain, N.M.; Amin, I.M.; Ahmad, V.N. The antimicrobial and antibiofilm properties of allicin against Candida albicans and Staphylococcus aureus–A therapeutic potential for denture stomatitis. Saudi Dent. J. 2021, 33, 105–111. [Google Scholar] [CrossRef]
- Feldman, M.; Sionov, R.V.; Mechoulam, R.; Steinberg, D. Anti-biofilm activity of cannabidiol against Candida albicans. Microorganisms 2021, 9, 441. [Google Scholar] [CrossRef]
- Ivanov, M.; Kannan, A.; Stojković, D.S.; Glamočlija, J.; Calhelha, R.C.; Ferreira, I.C.; Sanglard, D.; Soković, M. Camphor and eucalyptol—aticandidal spectrum, antivirulence effect, efflux pumps interference and cytotoxicity. Int. J. Mol. Sci. 2021, 22, 483. [Google Scholar] [CrossRef]
- Kovács, R.; Nagy, F.; Tóth, Z.; Forgács, L.; Tóth, L.; Váradi, G.; Tóth, G.K.; Vadászi, K.; Borman, A.M.; Majoros, L. The Neosartorya fischeri antifungal protein 2 (NFAP2): A new potential weapon against multidrug-resistant Candida auris biofilms. Int. J. Mol. Sci. 2021, 22, 771. [Google Scholar] [CrossRef]
- Lin, C.-H.; Kabrawala, S.; Fox, E.P.; Nobile, C.J.; Johnson, A.D.; Bennett, R.J. Genetic control of conventional and pheromone-stimulated biofilm formation in Candida albicans. PLoS Pathog. 2013, 9, e1003305. [Google Scholar] [CrossRef] [Green Version]
- Quatrin, P.M.; Verdi, C.M.; de Souza, M.E.; de Godoi, S.N.; Klein, B.; Gundel, A.; Wagner, R.; de Almeida Vaucher, R.; Ourique, A.F.; Santos, R.C.V. Antimicrobial and antibiofilm activities of nanoemulsions containing Eucalyptus globulus oil against Pseudomonas aeruginosa and Candida spp. Microb. Pathog. 2017, 112, 230–242. [Google Scholar] [CrossRef]
- Sudjana, A.N.; Carson, C.F.; Carson, K.C.; Riley, T.V.; Hammer, K.A. Candida albicans adhesion to human epithelial cells and polystyrene and formation of biofilm is reduced by sub-inhibitory Melaleuca alternifolia (tea tree) essential oil. Med. Mycol. 2012, 50, 863–870. [Google Scholar] [CrossRef] [Green Version]
- Souza, M.; Lopes, L.; Bonez, P.; Gündel, A.; Martinez, D.; Sagrillo, M.; Giongo, J.; Vaucher, R.; Raffin, R.; Boligon, A.; et al. Melaleuca alternifolia nanoparticles against Candida species biofilms. Microb. Pathog. 2017, 104, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Moser, D.; Han, F.; Leonhard, M.; Schneider-Stickler, B.; Tan, Y. Preparation and antibiofilm studies of curcumin loaded chitosan nanoparticles against polymicrobial biofilms of Candida albicans and Staphylococcus aureus. Carbohydr. Polym. 2020, 241, 116254. [Google Scholar] [CrossRef]
- Gumus, B.; Acar, T.; Atabey, T.; Derman, S.; Sahin, F.; Arasoglu, T. The battle against biofilm infections: Juglone loaded nanoparticles as an anticandidal agent. J. Biotechnol. 2020, 316, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Rajasekar, V.; Darne, P.; Prabhune, A.; Kao, R.Y.; Solomon, A.P.; Ramage, G.; Samaranayake, L.; Neelakantan, P. A curcumin-sophorolipid nanocomplex inhibits Candida albicans filamentation and biofilm development. Colloids Surf. B. Biointerfaces 2021, 200, 111617. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, C.F.; Silva, S.; Henriques, M. Candida glabrata: A review of its features and resistance. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 673–688. [Google Scholar] [CrossRef] [Green Version]
- Sabino, R.; Veríssimo, C.; Pereira, Á.A.; Antunes, F. Candida auris, an agent of hospital-associated outbreaks: Which challenging issues do we need to have in mind? Microorganisms 2020, 8, 181. [Google Scholar] [CrossRef] [Green Version]
- Ademe, M.; Girma, F. Candida auris: From multidrug resistance to pan-resistant strains. Infect. Drug Resist. 2020, 13, 1287. [Google Scholar]
- Zhang, Y.; Yang, H.; Turra, D.; Zhou, S.; Ayhan, D.H.; DeIulio, G.A.; Guo, L.; Broz, K.; Wiederhold, N.; Coleman, J.J.; et al. The genome of opportunistic fungal pathogen Fusarium oxysporum carries a unique set of lineage-specific chromosomes. Commun. Biol. 2020, 3, 50. [Google Scholar] [CrossRef] [Green Version]
- Oliveira dos Santos, C.; Kolwijck, E.; van Rooij, J.; Stoutenbeek, R.; Visser, N.; Cheng, Y.Y.; Santana, N.T.; Verweij, P.E.; Eggink, C.A. Epidemiology and clinical management of Fusarium keratitis in the Netherlands, 2005–2016. Front. Cell. Infect. Microbiol. 2020, 10, 133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mukherjee, P.K.; Chandra, J.; Yu, C.; Sun, Y.; Pearlman, E.; Ghannoum, M.A. Characterization of Fusarium keratitis outbreak isolates: Contribution of biofilms to antimicrobial resistance and pathogenesis. Invest. Ophthalmol. Vis. Sci. 2012, 53, 4450–4457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hino, Y.; Muraosa, Y.; Oguchi, M.; Yahiro, M.; Yarita, K.; Watanabe, A.; Sakaida, E.; Yokote, K.; Kamei, K. Drain outlets in patient rooms as sources for invasive fusariosis: An analysis of patients with haematological disorders. J. Hosp. Infect. 2020, 105, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Qian, W.; Yang, M.; Li, X.; Sun, Z.; Li, Y.; Wang, X.; Wang, T. Anti-microbial and anti-biofilm activities of combined chelerythrine-sanguinarine and mode of action against Candida albicans and Cryptococcus neoformans in vitro. Colloids Surf. B. Biointerfaces 2020, 191, 111003. [Google Scholar] [CrossRef]
- Harding, M.W.; Marques, L.L.; Howard, R.J.; Olson, M.E. Can filamentous fungi form biofilms? Trends Microbiol. 2009, 17, 475–480. [Google Scholar] [CrossRef] [PubMed]
- Costa-Orlandi, C.; Sardi, J.; Santos, C.; Fusco-Almeida, A.; Mendes-Giannini, M.J.S. In vitro characterization of Trichophyton rubrum and T. mentagrophytes biofilms. Biofouling 2014, 30, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Hu, W.; Tian, Z.; Yuan, D.; Yi, G.; Zhou, Y.; Cheng, Q.; Zhu, J.; Li, M. Developing natural products as potential anti-biofilm agents. Chin. Med. 2019, 14, 1–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Year | Essential Oil From | Fungal spp. Biofilm | In Vitro Type of Studies | Reference | |||
|---|---|---|---|---|---|---|---|
| Inhibition of Cell Adhesion or Hyphal Formation | Inhibition of Biofilm Formation | Eradication of Mature Biofilms | Mechanism of Action or In Vivo Assays | ||||
| 2017 | Laurus nobilis | C. albicans ATCC 60193; CBS 562; C. tropicalis ATCC 750; CBS 94 and C. krusei ATCC 3413; CBS 73 | L. nobilis EO at 1000 µg/mL inhibited the initial adhesion of C. albicans biofilms | At 1000 and 2000 µg/mL, the EO showed significant inhibition of biofilm formation | L. nobilis EO at 1000 and 2000 µg/mL reduced the amount of mature biofilms | [127] | |
| 2017 | 83 EOs | C. albicans ATCC 10231, 18804, 24433 and DAY185 | Croton eluteria reduced the Candida adherence by 75% | Six EOs, C. eluteria, Helichrysum coriaceum, Eucalyptus globulus, Cymbopogon citratus andCoriandrum sativum inhibited 90% of biofilm formation | In vivo assay: C. eluteria EO diminished Caenorhabditis elegans virulence | [128] | |
| 2018 | 12 EOs | C. albicans 135, BM2/94 and NYCY 1363 | Out of the 12 EOs tested, only Pelargonium graveolens and Melissa officinalis eradicated mature biofilms | [129] | |||
| 2018 | Pogostemon heyneanus, Cinnamomum tamalaand Cinnamomum camphora | C. albicans ATCC 90028; C. glabrata MTCC 6507 and C. tropicalis MTCC 310 | The three EOs produced a reduction in the hyphal formation with P. heyneanus EO showing the maximum inhibition | P. heyneanus and C. tamala disrupted mature biofilms | Candida biofilms EPM was reduced. A large reduction of sugars was observed | [130] | |
| 2019 | Foeniculm vulgare EO (fennel oil) | 10 isolates of C. albicans | The MBEC50 of fennel oil for 7/10 tested strains was 2-to 6-fold the MIC | [131] | |||
| 2020 | Cymbopogon citratus, Cuminum cyminum, Citrus limon and Cinnamomum verum | C. tropicalis isolates T26, U7 and V89 | C. citratus EO reduced biofilm formation of all C. tropicalis tested strains. C. limon and C. cyminum EOs showed minor effects | [132] | |||
| 2021 | Cymbopogon citratus and (lemongrass) Cinnamomum verum EOs (cinnamom) | C. albicans ATCC 10231 biofilms, coated on polymethyl methacrylate (PMMA) resin | C. verum EO at 8× MIC and C. citratus EO at 16× MIC, precoated on PMMA, inhibited C. albicans biofilm formation by 73% and 68%, respectively | At 8× MIC, both EOs eradicated totally the pre-established fungal biofilms in 1 h | [133] | ||
| Year | Extracts | Fungal Biofilms spp. | In Vitro Type of Studies | Reference | ||
|---|---|---|---|---|---|---|
| Inhibition of Cell Adhesion or Hyphal Formation | Biofilm Formation | Eradication of Mature Biofilms | ||||
| 2017 | Propolis from Paraná state (Brazil) diluted in EtOH (PE) quantified in its total phenol content | Fusarium spp. isolated from onichomycoses and deposited in UEM; F. oxysporum FO42; F. solani FS04 and ATCC 36031 and F. subglutinans (FSub39) | The total mass of biofilms and the number of viable cells were significantly reduced by PE | [134] | ||
| 2020 | EtOH-H2O extract of red propolis (RPE) from Paraiba state, Brazil | C. albicans ATCC 90028 mono sp. biofilm and C. albicans-C. glabrata ATCC 2001 co-cultures biofilms | RPE at 3% showed a high and low inhibitory capacity of inhibiting the formation of mono sp.- and co-cultured two spp. –biofilms, respectively | [136] | ||
| Year | Extracts Source and Solvent | Fungal Biofilms spp. | In Vitro Type of Studies | Reference | ||
|---|---|---|---|---|---|---|
| Inhibition of Cell Adhesion or Hyphal Formation | Biofilm Formation | Eradication of Mature Biofilms | ||||
| PLANT EXTRACTS | ||||||
| 2017 | Eugenia leitonii, E. brasiliensis, E. myrcianthes, E. involucrata leaf, pulp, seed and bark EtOH-H2O extracts | C. albicans ATCC 90028 | Treatment with E. leitonii seed and E. brasiliensis seed and leaf extracts at 10 × MIC, reduced C. albicans biofilm viability | [137] | ||
| 2017 | Malva sylvestris root EtOH extract | C. albicans ATCC 10231 | M. sylvestris extract at 0.19 mg/mL (1/4 MIC), down-regulated the expression of the hypha-specific gene HWP1 | M. sylvestris EtOH extract at 0.78 and 1.56 mg/mL (MIC and 2× MIC) reduced biofilm formation | [138] | |
| 2019 | Anadenantera colubrina bark EtOH-H2O extract | C. albicans ATCC MYA2876, ATCC 90028 and a clinical isolate; C. parapsilopsis ATCC 22019 and C. krusei ATCC 6258 | Candida biofilms at 500× MIC underwent a decrease in the number of CFU/mL. Biofilm structural alterations and cellular destruction were observed, being C. parapsilosis and C. krusei the most affected biofilms. | [139] | ||
| 2020 | Clematis flammula fresh leaves (CFL) and Fraxinus angustifolia fresh leaves (FAL) and bark (FAB) EtOH extracts | C. albicans ATCC 10231 | CFL, FAL and FAB produced a very low germ tube formation of 7.57, 2.29 and 1.17%, respectively in comparison to a growth of 50.89% for the control group | The extracts inhibited biofilm formation with MBIC50 = 250 μg/mL for FAL and 500 μg/mL for FAB, while CFL showed a MBIC50 > 1000 μg/mL | [140] | |
| 2020 | Hibiscus sabdariffa flower (Hs) DMSO extract | C. albicans isolated from vulvo-vaginal candidiasis | Hs extract inhibits the yeast-to-hyphal transition and biofilm adherence (50% at 1.5 mg/mL and 80% at 6.25 mg/mL) | Fungal cells incubated with Hs extract at 2.5 mg/mL (½ MIC), inhibited the biofilm maturation and, thus, the biofilm formation | Hs extract eradicated C. albicans biofilms at 3.12 mg/mL. In vivo assay with Caenorhabtidis elegans showed that Hs decreased the CFU of C. albicans i | [141] |
| 2020 | Orthoshipon aristatus purple leaf n-hexane extract | C. albicans ATCC 10231 | O. aristatus extract at 2 mg/mL reduced the adhesion of C. albicans cells | Mild inhibition of C. albicans growth at the biofilm development stage at 2 mg/mL | [142] | |
| LICHENS | ||||||
| 2017 | Thirty eight lichen acetone extracts of nine different families (mainly Parmeliaceae and Cladoniaceae) | C. albicans ATCC 3153 | Seven extracts displayed anti-maturation effect. Among them, Evernia prunastri and Ramalina fastigiata were the most promising lichens (IC50 < 4 µg/mL) | Seven extracts showed antibiofilm capacity. Among them, E.prunastri, Cladonia uncialis (R. fastigiata and Xanthoparmelia conspersa (showed IC50 values <10 µg/mL | [143] | |
| MICROALGAE AND CYANOBACTERIA | ||||||
| 2019 | 675 hexane, ethyl acetate and methanol extracts obtained from 225 microalgae and cyanobacteria | C. albicans and C. parapsilopsis (voucher N°s not stated) | C. albicans and C. parapsilopsis biofilm formation was inhibited by 308 extracts. C. albicans biofilms were particularly sensitive to extracts from Cryptophyta, Euglenophyta, and Glaucophyta (three completely unrelated lineages), with MBIC50 = 8 µg/mL. Instead, Rhodophyta spp. showed activity against C. parapsilopsis with MBIC50 = 64 µg/mL | [144] | ||
| Year | Type of Compound/ Natural Source | Structure and Name | Strains | In Vitro Type of Studies | Reference | ||||
|---|---|---|---|---|---|---|---|---|---|
| Inhibition of Cell Adhesion or Hyphal Formation | Biofilm Formation | Eradication of Mature Biofilms | Studies of Mechanisms of Action | ||||||
| 2017 | Formyl-phloroglucinol meroterpenoid Source Eucalyptus spp. and Psidium spp. |  eucarobustol E (EE) | C. albicans SC5314 and ATCC 24433; 10 Fluconazole-resistant C. albicans and 8 Fluconazole-susceptible C. albicans | EE inhibited C. albicans yeast-to-hyphal transition in both liquid and solid hypha-inducing media | EE inhibited 60 and 73% biofilm formation at 16 and 32 µg/mL, respectively and 100% at >32 µg/mL | EE eradicated mature biofilm at 128 µg/mL | At 8 and 16 µg/ml EE reduced by 9.2% and 65.3% the ergosterol production and increased by 3.95- and 5.43-fold the farnesol production, respectively | [145] | |
| 2017 | Isoquinoline alkaloid Source Not informed |  berberine (BBR) | C. albicans SC5314; C. parapsilosis ATCC 22019; C. glabrata ATCC 15126; C. tropicalis ATCC 750 and other C tropicalis strains (2203, 2317, 2006, 2718, 333, 087, 20026) | BBR inhibited Candida biofilm formation with MBIC values of 64–256 µg/mL | [146] | ||||
| 2017 | 3-3’-Neolignan Source Magnolia officinalis |  magnolol. (2-(2-hydroxy-5-prop-2-enylphenyl)-4-prop-2-enylphenol) | C. dubliniensis CDC 27897; C. albicans CDC 27907 and ATCC 24433; C. glabrata CDC 28621 | Magnolol inhibited 35.6%–69.5% preformed biofilms of the three fungi at 32 µg/mL | [147] | ||||
| 2017 | 5 terpenes and one phenylpropanoid. Sources. EOs from Origanum vulgare, Mentha piperita, Thymus vulgaris Cinamomum verum Cymbopogon citratus and Syzygium aromaticum |  |  | C. neoformans NCIM 3541 and C. laurentii NCIM 3373 | MBIC80 against C. neoformans and C. laurentii: for thymol: 32 and 16 µg/mL; for carvacrol, 64 and 32 µg/mL and for citral, 128 and 64 µg/mL, respectively. | MBEC80 of thymol and carvacrol against C. neoformans were 128 and 256 µg/mL, respectively, and against C. laurentii 64 and 128 µg/mL, respectively. MBEC80 for citral was 256 µg/mL for both fungi | The compounds reduced EPM, cellular density and altered the surface morphology of biofilm cells | [148] | |
| thymol | carvacrol | ||||||||
 cinnamaldehyde | |||||||||
 citral |  menthol | ||||||||
 eugenol | |||||||||
| 2017 | Eudesmane sesquiterpene Source Tritomaria quinquedentata |  ent-isoalantolactone (ent-iLL) | C. albicans DSY654. Genotype: Dcdr1::hisG/Dcdr1::hisG/Dcdr2::hisG-URA3-hisG/ Dcdr2::hisG | Ent-iLL inhibited the yeast-to-hyphal switch at 4 or 8 µg/mL in agar plate tests or liquid medium, respectively | Ent-iLL reduced ergosterol content by inhibiting Erg11 and Erg6 | [151] | |||
| 2017 | β-diketone diphenol Source Curcuma longa (Zingiberaceae) |  curcumin (Cur) | C. albicans SC5314 | Cur at 50 µg/mL reduced the capacity of C. albicans to attach to polymethyl methacrylate (PMMA) denture base material | The MBIC80 for Cur was ≥200 μg/mL for sessile cells | Cur at 50 μg/mL down-regulated the adhesin ALS3, with minimal impact on ALS1. The clustered aggregative and flocculation genes AAF1, EAP1, and ALS5 transcripts were up-regulated | [152] | ||
| 2018 | Phenols with a variable length in the lateral chain (6 or 8 carbons) bearing a keto substituent and a β-OH (gingerols) or a Δ-5 double bond (6- shogaol) Source: Zingiber officinale |  6-gingerol (6-G)  8-gingerol (8-G)  6-shogaol (6-S) | Fluconazole-resistant C. albicans DAY185 | 6-S at 10 µg/mL was more effective in suppressing hyphal formation than 6 g at 50 µg/mL | 6-S at 10, 50, and 100 µg/mL inhibited 85, 94, and 94% biofilm formation, respectively. 6 g and 8 g at 50 µg/mL inhibited by 88 and 80%, respectively the biofilm formation | 6 g and 6-S significantly altered the expressions of some hypha-specific (HWP1 and ECE1), biofilm-related (HWP1 and RTA3) and multidrug transporter (CDR1 and CDR2) related genes. 80% of C. elegans infected with C. albicans survived in the presence of both compounds at 50 μg/mL | [153] | ||
| 2019 | Monoterpenes Source Origanum vulgare Cinamomum verum Cymbopogon citratus Mentha piperita and Thymus vulgaris |  thymol |  carvacrol | C. neoformans NCIM 3541 (equivalent to ATCC 32045) | The three compounds inhibit biofilm formation and eradicate mature biofilms by the following mechanisms: (i) ergosterol biosynthesis inhibition and selectively interaction via ergosterol binding, (ii) disruption of the biofilm cell surface with reduction in cell height, alterations in the fatty acid profile which attenuate the cell membrane fluidity with enhanced permeability, resulting in pore formation and efflux of the K+/intracellular content, (v) mitochondrial depolarization caused higher levels of ROS. Then, the oxidative stress caused a significant decline in the amount of EPM and capsule sugars (mannose, xylose, and glucuronic acid), leading to a reduced capsule size and an overall negative charge on the cell surface | [150] | |||
 citral | |||||||||
| 2019 | 1,4-naphtoquinone derivative Source (Lithospermum erythrorhizon) |  shikonin (SK) | C. albicans SC5314 and 10 clinical isolates from Changhai Hospital of Shanghai, China. | The filamentation in Lee’s media was completely inhibited by 0.5 µg/mL of SK | SK at 4 µg/mL inhibited biofilm formation by 65.4%, while the biofilm growth was almost totally inhibited when exposed to 32 µg/mL of SK | SK at 32 µg/mL destroyed mature biofilms by 92.8% | The expression of genes involved in hyphae formation and adhesion, ECE1, HWP1, EFG1, CPH1,RAS1, ALS1, ALS3 and CSH1 were downregulated while TUP1, NRG1, and BCR1 were upregulated | [154] | |
| 2020 | Phenolic aldehyde Source Many plants including Melia azedarach |  vanillin (Van) | C. albicans SC5314, MRC10 (Δicl1) and MRC11. Consult the genotypes in the original reference | With Van at 62.5 µg/mL, C. albicans were unable to express filaments and presented a normal morphology with few or no adherence to buccal epithelial cells. | Adherence to polystyrene surface and biofilm formation were reduced by 49% | Mature biofilm eradication (52%) was observed | C. albicans biofilms were absent or negligible in C. elegans worms treated with 125 µg/mL of Van | [155] | |
| 2020 | Sesquiterpene alcohol Source Dimorphic fungus C. albicans |  farnesol (FS) | Fusarium keratinoplaticum ATCC 36031 | FS prevented the adhesion of conidia and filamentation for biofilm formation | FS reduced the number of viable cells and the total biofilm biomass. The metabolic activity was only reduced at 500 μM. At 700 μM, FS completely prevented the biofilm formation | FS was able to modulate preformed biofilms, decreasing significantly the number of viable cells, in particular at >600 μM | [156] | ||
| 2020 | Labdane diterpenoid Source liverwort Heteroscyphus coalitus |  heteroscyphin D (HSc-D) | CDR1 and CDR2 efflux pumps deficient strain C. albicans DSY654 and the wild type C. albicans S5314 | HSc-D restricted the formation of hyphae at 4 μg/ml, but showed no activity against SC5314. HSc-D decreased the adherent C. albicans cells on A549 cancer cell monolayers from 1 µg/mL | HSc-D completely prevented biofilm formation at ≥8μg/mL | HSc-D decreased the transcriptional levels of the genes ALS3, HWP1, and ECE1 encoding adhesins and affected the Ras1-cAMP-Efg1 pathway, NRG1 and UME6 to retard the yeast-to-hyphal transition. | [157] | ||
| 2020 | Artemisinin sesquiterpene lactone Scopoletin: coumarin derivative Sources Ar: Artemisiaannua Sc: from several plants including A. annua |  artemisinin (Ar)  scopoletin (Sc) | C. albicans 1372; C. dubliniensis 1470, C. tropicalis 1368, C. krusei 779, C. glabrata 1374 and C. guilliermondii 808 | FS and Sc reduced biofilm biomass and metabolic activity and led to non-viable cells | Ar was more effective in disrupting the preformed EPM- structure and in killing the sessile cells as compared to Sc at their respective MBEC10. In C. albicans, C. dubliniensis and C. glabrata | Ar and Sc promoted the accumulation of intracellular ROS by increasing oxidative stress at their respective MBEC10 | [158] | ||
| 2020 | Scopoletin: coumarin derivative Source Mitracarpus frigidus. |  scopoletin (Sc) | Fluconazole, itraconazol and amphothericin--resistant C. tropicalis ATCC 28707 | At 4× MIC (200 µg/mL), Sc produced a great reduction of the area occupied by biofilms on the surface of coverslips | At its MIC (50 µg/mL), Sc reduced preformed Candida biofilms | [159] | |||
| 2020 | Drimane sesquiterpene dialdehydes Source Warburgia ugandensis |  (+)-warburganal R=OH (-)-polygodial R=H | C. albicans SC5314; C. glabrata ATCC 2001 and C. glabrata BG2 | Warburganal: MBIC50 = 4.5 and ~50 µg/ml against C. albicans and C. glabrata, respectively. Polygodial: MBIC50 = ~10 and and ~50 µg/mL, respectively | Warburganal and polygodial: MBEC50 = ~ 16 µg/ml against C. albicans but did not eradicate the C. glabrata biofilm | [160] | |||
| 2020 | Dammarane-type glycosides (gypenosides) Source Gynostemma pentaphyllum | No description of the compounds tested dammarane skeleton | Flu-resistant C. albicans CA10 and CA16 | Gypenosides showed MBIC80 > 128 µg/mL | [161] | ||||
| 2021 | Polyciclic compound with a lipophilic side chain Source Sea squirt microbiome constituent Micromonospora sp. |  turbinmicin (TBM) | C. albicans SN250, C. tropicalis 98-234, C. glabrata 4720, C. auris B11220 and A. fumigatus 293 | At 2 and 4 µg/mL, TBM reduced the biofilms by 50% | TBM inhibited the biofilm extracelular vesicle (EV) production and, thus, eliminated the EPM assembly | Ten μg/mL of TBM eliminated C. albicans C. tropicalis, C. glabrata, C. auris and A. fumigatus, biofilms from catheters | [162] | ||
| 2021 | Organosulfur compound. Diallyl thiosulfinate Source (Allium sativum) |  allicin | C. albicans ATCC 14053 | Allicin eradicated 50% C. albicans biofilms at sub-MIC = 4 µg/mL | [164] | ||||
| 2021 | Terpenphenol __________ Source Cannabis sativa |  cannabidiol (CBD) | C. albicans SC5314 C. albicans SC5314 carrying the green fluorescent protein (GFP) reporter gene (C. albicans–GFP) | CBD at 25 µg/mL caused a pronounced inhibitory biofilm formation effect. MBIC90 = 100 µg/mL | At 1.56 and 3.12 µg/mL, mature biofilm decreased 28% and 44%, respectively. | CBD showed a multitarget mode of action with up- regulation of yeast-associated genes and downregulation of hyphae-specific genes. C. albicans virulence genes decreased. CBD increases ROS production, reduces the intracellular ATP levels, modifies the cell wall, and increases the plasma membrane permeability | [165] | ||
| 2021 | Monoterpenes Sources EO from many species of genera such as Cinnamomum, Eucalyptus, Artemisia, Salvia and Thuja |  camphor  eucalyptol | C. albicans 475/15, C. albicans 503/15, C. albicans ATCC 1023,; C. krusei H1/16; C. tropicalis ATCC 750 and C. parapsilosis ATCC 22019 | Camphor at 0.125 mg/mL and eucalyptol at 23 mg/mL induced a notable reduction in the number of hyphal cells in C. albicans 475/15 | Camphor and eucalyptol inhibited C. albicans, C. tropicalis, C. parapsilosis and C. krusei biofilm biomass | Camphor at 0.125 mg/mL reduced ROS by 52% while eucalyptol was inactive | [166] | ||
| Nanosystems formed with essential oils (EOs) | ||||||||
| Year | EOs Included in Nanosystems | Type of Nano System | Fungal Strains | Inhibition of Cell Adhesión or Hyphal Formation | Biofilm Formation | Eradication of Mature Biofilms | Mechanisms of Action or Genes Expression | Reference |
| 2017 | Eucalyptus globulus EO | Nanoemulsions (NE) __________ Composition Oil phase: 5% EO and 2% sorbitan monooleate Aqueous phase: 2% Tween 80 and 25 mL of water | C. albicans ATCC 14053; C. tropicalis ATCC 66029; C. glabrata ATCC 66032 | (EO-NE) at 22.5 mg/mL reduced C. albicans, C. tropicalis and C. glabrata biofilm formation | [169] | |||
| 2017 | Melaleuca alternifolia EO (tea tree oil, TTO) | Nanoparticles (NP) __________ Composition Proprietary method from Inventiva® (Porto Alegre, Brazil)), based on high pressure homogenization. 7.5% (w/v) of TTO, cetyl palmitate as the solid lipid and Tween 80 as the surfactant | C. albicans ATCC 14053; C. glabrata ATCC 66032; C. parapsilopsis ATCC 220190; C. tropicalis ATCC 66029; C. membranaefaciens ATCC 2013770 | TTO-NP at 15.6% decreased the biofilm formation of all strains tested. The antibiofilm activity was higher in C. glabrata | TTO-NP decreased EPM and protein content in biofilms, and TTO-NPs inhibited the enzyme succinate dehydrogenase | [171] | ||
| Nanosystems formed with natural compounds | ||||||||
| Year | Type of Compound Name and Structure Natural Source | Nanosystem | Fungal Biofilms spp. | Inhibition of Cell Adhesion or Hyphal Formation | Biofilm Formation | Eradication of Mature Biofilms | Studies of Mechanisms of Action | Reference |
| 2020 | β-Diketone diphenol curcumin (Cur) Source Curcuma longa | Positively charged chitosan nanoparticles (CSNP) Cur was loaded on CSNP, forming CSNP-Cur | C. albicans DAY185 | CSNP-Cur at 200 μg/mL inhibited almost completely the C. albicans biofilm formation | CSNP-Cur at 400 μg/mL eradicated the preformed C. albicans biofilms | [172] | ||
| 2020 | 1,4-Naphtoquinone derivative juglone (JU) Source Juglans regia | Nanoemulsions JU was loaded on poly (D,L-lactic-co-glycolic acid) (PLGA) forming PLGA-JU | C. albicans, non-specified voucher | PLGA-JU reduced the cell adhesion at 1.25 and 0.625 mg/mL | PLGA-JU at 1.25 and 0.625 mg/mL inhibited by 100% the C. albicans biofilm formation, being more effective than free JU and Fluconazole | PLGA-JU at doses equivalent to 1.25 and 0.625 mg/mL of JU completely inhibited pre-established C. albicans biofilms | PLGA-JU caused membrane depolarization of biofilm cells | [173] |
| 2021 | β-Diketone diphenol compound curcumin (Cur) curcumin (Cur)Source Curcuma longa | Cur-SL Nanocomplex formed with the surfactant sophorolipid (SL) Cur was loaded to the nanoparticle prepared with SL forming Cur-SL | C. albicans DAY185 | CU-SL at sub-inhibitory concentrations of 9.37 μg/mL significantly suppressed fungal adhesion | CU-SL at 9.37 μg/mL inhibited biofilm development and maturation | Four major transcriptional genes that promote biofilm formation, ROB1, EFG 1, TEC1, BRG 1 and NDT80 were down-regulated, as well as the adhesin genes ALS1, SAP8 and EAP1, the hyphal regulatory genes SAP4, HWP1 RAS1 and HYR1 and ERG11 | [174] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Butassi, E.; Svetaz, L.; Carpinella, M.C.; Efferth, T.; Zacchino, S. Fungal Biofilms as a Valuable Target for the Discovery of Natural Products That Cope with the Resistance of Medically Important Fungi—Latest Findings. Antibiotics 2021, 10, 1053. https://doi.org/10.3390/antibiotics10091053
Butassi E, Svetaz L, Carpinella MC, Efferth T, Zacchino S. Fungal Biofilms as a Valuable Target for the Discovery of Natural Products That Cope with the Resistance of Medically Important Fungi—Latest Findings. Antibiotics. 2021; 10(9):1053. https://doi.org/10.3390/antibiotics10091053
Chicago/Turabian StyleButassi, Estefanía, Laura Svetaz, María Cecilia Carpinella, Thomas Efferth, and Susana Zacchino. 2021. "Fungal Biofilms as a Valuable Target for the Discovery of Natural Products That Cope with the Resistance of Medically Important Fungi—Latest Findings" Antibiotics 10, no. 9: 1053. https://doi.org/10.3390/antibiotics10091053
APA StyleButassi, E., Svetaz, L., Carpinella, M. C., Efferth, T., & Zacchino, S. (2021). Fungal Biofilms as a Valuable Target for the Discovery of Natural Products That Cope with the Resistance of Medically Important Fungi—Latest Findings. Antibiotics, 10(9), 1053. https://doi.org/10.3390/antibiotics10091053






