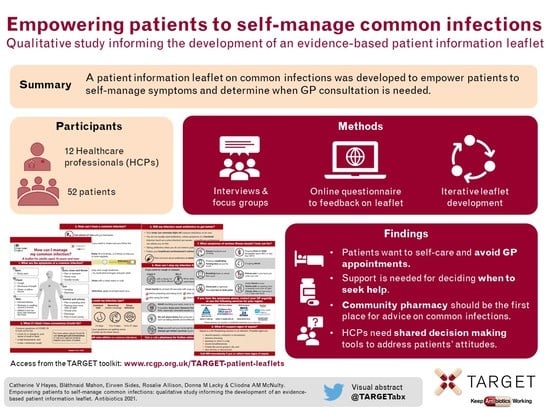
Empowering Patients to Self-Manage Common Infections: Qualitative Study Informing the Development of an Evidence-Based Patient Information Leaflet
Abstract
:1. Introduction
2. Results
2.1. Participant Characteristics
2.2. Emerging Themes on Management of Common Infections
2.2.1. Patients
2.2.2. Healthcare Professionals
2.3. Development of the Managing Common Infections leaflet
‘Great way to get a lot of information to the patient. Will lead to less calls.’(nurse, questionnaire)
‘I think it’s a very good leaflet, if the idea of this is to actually reduce the use of antibiotics when other simpler remedies could be used then I think it’s a good idea.’(Male patient, Focus Group 5)
‘Many BAME [Black and Minority Ethnic] patients have other underlying issues, which may present the same symptoms as described in the leaflet, maybe expressing if there is some difference to the normal symptom they present?’(patient, questionnaire)
‘I think if it could be quite basic if it has links to things on the internet…and then if you need to know more, this is where you go and look… and that set you on the path to helping yourself by finding out other things online.’(Female patient, Interview 1)
- What are the symptoms of a common infection?
- What if I think I have coronavirus (COVID-19)?
- How can I treat a common infection?
- How long could my infection last?
- Will my infection need antibiotics to get better?
- How can I stop my infection from spreading?
- What symptoms of serious illness should I look out for?
- What if I suspect signs of sepsis?
‘[For the title] I want to say, how you can manage your common infection, question mark… I think it will put the emphasis on empowering the person. Them at the centre of this, because that’s what I think it should be about.’(Pharmacist, focus group 1)
‘Depending on where they receive the leaflet. It could be attached to their prescriptions when they collect it from the pharmacy, or handed out at the GP surgery.’(pharmacy staff, questionnaire)
‘Unless it is translated, this would be a lot of text for an average non-English speaker. Visuals are great on this but I think there would be more required to help them better understand.’(patient, questionnaire)
3. Discussion
3.1. Summary
3.2. Strengths and Limitations
3.3. Comparison with Existing Literature
3.4. Implications for Research and Practice
4. Materials and Methods
4.1. Study Design
4.2. Intervention Development
4.2.1. Audience and Purpose of the Leaflet
4.2.2. Leaflet Development
4.3. Setting and Participant Recruitment
4.4. Data Collection
4.5. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. World Health Organisation: Antimicrobial Resistance Global Report on Surveillance; WHO: Geneva, Switzerland, 2014; Available online: https://apps.who.int/iris/bitstream/handle/10665/112642/9789241564748_eng.pdf;jsessionid=27B57B8DEF0B3D930FA9D25FC8BD1691?sequence=1 (accessed on 15 September 2019).
- Public Health England (PHE). English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR); Report 2019–2020; PHE: London, UK, 2020. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/936199/ESPAUR_Report_2019-20.pdf (accessed on 20 May 2021).
- Dolk, F.C.K.; Pouwels, K.B.; Smith, D.R.M.; Robotham, J.V.; Smieszek, T. Antibiotics in primary care in England: Which antibiotics are prescribed and for which conditions? J. Antimicrob. Chemother. 2018, 73 (Suppl. 2), ii2–ii10. [Google Scholar] [CrossRef] [PubMed]
- Pouwels, K.B.; Dolk, F.C.K.; Smith, D.R.M.; Robotham, J.V.; Smieszek, T. Actual versus ‘ideal’ antibiotic prescribing for common conditions in English primary care. J. Antimicrob. Chemother. 2018, 73 (Suppl. 2), 19–26. [Google Scholar] [CrossRef] [PubMed]
- Pouwels, K.B.; Dolk, F.C.K.; Smith, D.R.M.; Robotham, J.V.; Smieszek, T. Explaining variation in antibiotic prescribing between general practices in the UK. J. Antimicrob. Chemother. 2018, 73 (Suppl. 2), ii27–ii35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- HM Government. UK 5-Year Action Plan for Antimicrobial Resistance 2019 to 2024; Department of Health and Social Care: London, UK, 2019. [Google Scholar]
- National Institute for Health Care and Excellence (NICE). Summary of Antimicrobial Prescribing Guidance—Managing Common Infections; NICE: London, UK, 2021; Available online: https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/antimicrobial-prescribing-guidelines (accessed on 20 May 2021).
- National Institute for Health Care and Excellence (NICE). Antimicrobial Stewardship: Changing Risk-Related Behaviours in the General Population; NICE Guideline [NG63]; NICE: London, UK, 2017; Available online: https://www.nice.org.uk/guidance/ng63 (accessed on 20 May 2021).
- Jones, L.F.; Verlander, N.Q.; Lecky, D.M.; Altaf, S.; Pilat, D.; McNulty, C.A.M. Self-Reported Antimicrobial Stewardship Practices in Primary Care Using the TARGET Antibiotics Self-Assessment Tool. Antibiotics 2020, 9, 253. [Google Scholar] [CrossRef]
- Coxeter, P.; Del Mar, C.B.; McGregor, L.; Beller, E.M.; Hoffmann, T.C. Interventions to facilitate shared decision making to address antibiotic use for acute respiratory infections in primary care. Cochrane Database Syst. Rev. 2015, 2015, CD010907. [Google Scholar] [CrossRef] [Green Version]
- Smith, C.M.; Shallcross, L.J.; Dutey-Magni, P.; Conolly, A.; Fuller, C.; Hill, S.; Jhass, A.; Marcheselli, F.; Michie, S.; Mindell, J.S.; et al. Incidence, healthcare-seeking behaviours, antibiotic use and natural history of common infection syndromes in England: Results from the Bug Watch community cohort study. BMC Infect. Dis. 2021, 21, 105. [Google Scholar] [CrossRef]
- Murphy, M.; Scott, L.J.; Salisbury, C.; Turner, A.; Scott, A.; Denholm, R.; Lewis, R.; Iyer, G.; Macleod, J.; Horwood, J. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: A mixed-methods longitudinal study. Br. J. Gen. Pract. 2021, 71, e166–e177. [Google Scholar] [CrossRef]
- NHS Digital. Appointments in General Practice. Official Statistics, Experimental Statistics; NHS Digital: Leeds, UK, 2020; Available online: https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice (accessed on 15 July 2021).
- McNulty, C.; Hawking, M.; Lecky, D.; Jones, L.; Owens, R.; Charlett, A.; Butler, C.; Moore, P.; Francis, N. Effects of primary care antimicrobial stewardship outreach on antibiotic use by general practice staff: Pragmatic randomized controlled trial of the TARGET antibiotics workshop. J. Antimicrob. Chemother. 2018, 73, 1423–1432. [Google Scholar] [CrossRef]
- Jones, L.F.; Cooper, E.; Joseph, A.; Allison, R.; Gold, N.; Donald, I.; McNulty, C. Development of an information leaflet and diagnostic flow chart to improve the management of urinary tract infections in older adults: A qualitative study using the Theoretical Domains Framework. BJGP Open 2020, 4, bjgpopen20X101044. [Google Scholar] [CrossRef]
- Lecky, D.M.; Howdle, J.; Butler, C.C.; McNulty, C.A. Optimising management of UTIs in primary care: A qualitative study of patient and GP perspectives to inform the development of an evidence-based, shared decision-making resource. Br. J. Gen. Pract. 2020, 70, e330–e338. [Google Scholar] [CrossRef]
- Yardley, L.; Morrison, L.; Bradbury, K.; Muller, I. The Person-Based Approach to Intervention Development: Application to Digital Health-Related Behavior Change Interventions. JMIR 2015, 17, e30. [Google Scholar] [CrossRef]
- Royal College of General Practitioners. TARGET Antibiotics Toolkit. 2021. Available online: https://www.rcgp.org.uk/clinical-and-research/resources/toolkits/amr/target-antibiotics-toolkit.aspx (accessed on 16 June 2021).
- HM Government. Coronavirus (COVID-19). 2021. Available online: https://www.gov.uk/coronavirus (accessed on 23 July 2021).
- UK Sepsis Trust. The UK Sepsis Trust. 2021. Available online: https://sepsistrust.org/ (accessed on 23 July 2021).
- Atkins, L.; Francis, J.; Islam, R.; O’Connor, D.; Patey, A.; Ivers, N.; Foy, R.; Duncan, E.M.; Colquhoun, H.; Grimshaw, J.M.; et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement. Sci. 2017, 12, 77. [Google Scholar] [CrossRef]
- Jones, L.F.; Owens, R.; Sallis, A.; Ashiru-Oredope, D.; Thornley, T.; Francis, N.A.; Butler, C.; McNulty, C.A.M. Qualitative study using interviews and focus groups to explore the current and potential for antimicrobial stewardship in community pharmacy informed by the Theoretical Domains Framework. BMJ Open 2018, 8, e025101. [Google Scholar] [CrossRef] [Green Version]
- Brookes-Howell, L.; Elwyn, G.; Hood, K.; Wood, F.; Cooper, L.; Goossens, H.; Ieven, M.; Butler, C.C. ‘The body gets used to them’: Patients’ interpretations of antibiotic resistance and the implications for containment strategies. J. Gen. Intern. Med. 2012, 27, 766–772. [Google Scholar] [CrossRef] [Green Version]
- Brooks, L.; Shaw, A.; Sharp, D.; Hay, A. Towards a better understanding of patients’ perspectives of antibiotic resistance and MRSA: A qualitative study. Fam. Pract. 2008, 25, 341–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, M.E.; Liu, T.L.; Taylor, Y.; Davidson, L.; Schmid, M.; Yates, T.; Scotton, J.; Spencer, M. Exploring Patient Awareness and Perceptions of the Appropriate Use of Antibiotics: A Mixed-Methods Study. Antibiotics 2017, 6, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawkings, N.J.; Butler, C.C.; Wood, F. Antibiotics in the community: A typology of user behaviours. Patient Educ. Couns. 2008, 73, 146–152. [Google Scholar] [CrossRef]
- Hawkings, N.J.; Wood, F.; Butler, C.C. Public attitudes towards bacterial resistance: A qualitative study. J. Antimicrob. Chemother. 2007, 59, 1155–1160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- George, S.; Duran, N.; Norris, K. A Systematic Review of Barriers and Facilitators to Minority Research Participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am. J. Public Health 2014, 104, e16–e31. [Google Scholar] [CrossRef] [PubMed]
- Butler, C.C.; Hawking, M.K.D.; Quigley, A.; McNulty, C.A.M. Incidence, severity, help seeking, and management of uncomplicated urinary tract infection: A population-based survey. Br. J. Gen. Pract. 2015, 65, e702–e707. [Google Scholar] [CrossRef] [Green Version]
- Leydon, G.M.; Turner, S.; Smith, H.; Little, P. The journey from self-care to GP care: A qualitative interview study of women presenting with symptoms of urinary tract infection. Br. J. Gen. Pract. 2009, 59, e219–e225. [Google Scholar] [CrossRef] [Green Version]
- McDermott, L.; Leydon, G.M.; Halls, A.; Kelly, J.; Nagle, A.; White, J.; Little, P. Qualitative interview study of antibiotics and self-management strategies for respiratory infections in primary care. BMJ Open 2017, 7, e016903. [Google Scholar]
- Allison, R.; Chapman, S.; Howard, P.; Thornley, T.; Ashiru-Oredope, D.; Walker, S.; Jones, L.F.; McNulty, C.A.M. Feasibility of a community pharmacy antimicrobial stewardship intervention (PAMSI): An innovative approach to improve patients’ understanding of their antibiotics. JAC Antimicrob. Resist. 2020, 2, dlaa089. [Google Scholar] [CrossRef]
- Cabral, C.; Lucas, P.J.; Ingram, J.; Hay, A.D.; Horwood, J. “It’s safer to …” parent consulting and clinician antibiotic prescribing decisions for children with respiratory tract infections: An analysis across four qualitative studies. Soc. Sci. Med. 2015, 136–137, 156–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halls, A.; Van’t Hoff, C.; Little, P.; Verheij, T.; Leydon, G.M. Qualitative interview study of parents’ perspectives, concerns and experiences of the management of lower respiratory tract infections in children in primary care. BMJ Open 2017, 7, e015701. [Google Scholar] [CrossRef] [Green Version]
- Ingram, J.; Cabral, C.; Hay, A.D.; Lucas, P.J.; Horwood, J. Parents’ information needs, self-efficacy and influences on consulting for childhood respiratory tract infections: A qualitative study. BMC Fam. Pract. 2013, 14, 106. [Google Scholar] [CrossRef] [Green Version]
- Neill, S.J. Containing acute childhood illness within family life: A substantive grounded theory. J. Child Health Care 2010, 14, 327–344. [Google Scholar] [CrossRef] [Green Version]
- Tonkin-Crine, S.; Yardley, L.; Coenen, S.; Fernandez-Vandellos, P.; Krawczyk, J.; Touboul, P.; Verheij, T.; Little, P. GPs’ views in five European countries of interventions to promote prudent antibiotic use. Br. J. Gen. Pract. 2011, 61, e252–e261. [Google Scholar] [CrossRef] [PubMed]
- McNulty, C.A.; Boyle, P.; Nichols, T.; Clappison, P.; Davey, P. Don’t wear me out—The public’s knowledge of and attitudes to antibiotic use. J. Antimicrob. Chemother. 2007, 59, 727–738. [Google Scholar] [CrossRef] [Green Version]
- McNulty, C.A.M.; Collin, S.M.; Cooper, E.; Lecky, D.M.; Butler, C.C. Public understanding and use of antibiotics in England: Findings from a household survey in 2017. BMJ Open 2019, 9, e030845. [Google Scholar] [CrossRef] [Green Version]
- Norris, P.; Chamberlain, K.; Dew, K.; Gabe, J.; Hodgetts, D.; Madden, H. Public Beliefs about Antibiotics, Infection and Resistance: A Qualitative Study. Antibiotics 2013, 2, 465–476. [Google Scholar] [CrossRef] [PubMed]
- NHS England. CCG Outcomes Tools: Quality Premium. 2021. Available online: https://www.england.nhs.uk/ccg-out-tool/qual-prem/ (accessed on 16 June 2021).
- Bloomfield, S.F.; Stanwell-Smith, R.; Crevel, R.W.R.; Pickup, J. Too clean, or not too clean: The hygiene hypothesis and home hygiene. Clin. Exp. Allergy 2006, 36, 402–425. [Google Scholar] [CrossRef]
- Royal Society of Public Health. Too Clean or Not Too Clean? The Case for Targeted Hygiene in Home and Everyday Life. 2019. Available online: https://www.rsph.org.uk/our-work/policy/infection-control/too-clean-or-not-too-clean.html (accessed on 20 September 2019).
- Bloomfield, S.F. The case for Targeted Hygiene. Perspect. Public Health 2019, 139, 219–221. [Google Scholar]
- Coronado-Vázquez, V.; Canet-Fajas, C.; Delgado-Marroquín, M.T.; Magallón-Botaya, R.; Romero-Martín, M.; Gómez-Salgado, J. Interventions to facilitate shared decision-making using decision aids with patients in Primary Health Care: A systematic review. Medicine 2020, 99, e21389. [Google Scholar] [CrossRef]
- Peiffer-Smadja, N.; Allison, R.; Jones, L.F.; Holmes, A.H.; Patel, P.; Lecky, D.L.; Ahmad, R.; McNulty, C.A.M. Preventing and Managing Urinary Tract Infections: Enhancing the Role of Community Pharmacists-A Mixed Methods Study. Antibiotics 2020, 9, 583. [Google Scholar] [CrossRef]
- Ashiru-Oredope, D.; Doble, A.; Thornley, T.; Saei, A.; Gold, N.; Sallis, A.; McNulty, C.A.M.; Lecky, D.; Umoh, E.; Klinger, C. Improving Management of Respiratory Tract Infections in Community Pharmacies and Promoting Antimicrobial Stewardship: A Cluster Randomised Control Trial with a Self-Report Behavioural Questionnaire and Process Evaluation. Pharmacy 2020, 8, 44. [Google Scholar] [CrossRef] [Green Version]
- Little, P.; Stuart, B.; Andreou, P.; McDermott, L.; Joseph, J.; Mullee, M.; Moore, M.; Broomfield, S.; Thomas, T.; Yardley, L. Primary care randomised controlled trial of a tailored interactive website for the self-management of respiratory infections (Internet Doctor). BMJ Open 2016, 6, e009769. [Google Scholar] [CrossRef] [Green Version]
- McNulty, C.A.M.; Read, B.; Quigley, A.; Verlander, N.Q.; Lecky, D.M. What the public know about antibiotic use and resistance in 2020—A face-to-face questionnaire survey. BMJ Open 2021. manuscript submitted. [Google Scholar]
- Han, S.M.; Greenfield, G.; Majeed, A.; Hayhoe, B. Impact of Remote Consultations on Antibiotic Prescribing in Primary Health Care: Systematic Review. J. Med. Internet Res. 2020, 22, e23482. [Google Scholar] [CrossRef]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough?:An Experiment with Data Saturation and Variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Guest, G.; Namey, E.; McKenna, K. How Many Focus Groups Are Enough? Building an Evidence Base for Nonprobability Sample Sizes. Field Methods 2016, 29, 3–22. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]

| Patients n = 52 | Healthcare Professionals n = 12 | ||||
|---|---|---|---|---|---|
| INT and FGs (n = 27) | Questionnaire (n = 25) | INT and FGs (n = 7) | Questionnaire (n = 5) | ||
| Age | Profession | ||||
| 16–24 | 1 | 3 | Community | 3 | - |
| 25–34 | 3 | 12 | pharmacist | ||
| 35–49 | 8 | 1 | General | 2 | - |
| 50–64 | 8 | 2 | Practitioner | ||
| 65+ | 7 | 5 | Prescribing advisor | 1 | 1 |
| Unknown | - | 2 | Nurse practitioner | 1 | 4 |
| Gender | Gender | ||||
| Female | 18 | 13 | Female | 3 | - |
| Male | 9 | 11 | Male | 3 | - |
| Unknown | - | 1 | Unknown | 1 | 5 |
| Ethnicity | |||||
| Bangladeshi | 1 | 5 | |||
| Black African | - | 2 | |||
| Black Caribbean | 1 | 2 | |||
| Chinese | - | 5 | |||
| Indian | - | 6 | |||
| Pakistani | 1 | 2 | |||
| Sri Lankan | 2 | 1 | |||
| White British | 20 | - | |||
| White European | 2 | 2 | |||
| Theme | Sub Themes | TDF Domain(s) | Quotes | Implications for Leaflet |
|---|---|---|---|---|
| Preventing infections |
| Knowledge; Belief about consequences; Social influences; Reinforcement | ‘I’ve suffered from urinary tract infections so drinking plenty of water is really important for me and having a lot of vegetables and fruit.’ (Female, FG5) ‘A lot of cleaning, a lot more cleaning. I used to clean a lot anyway but since this COVID-19, I find that it’s just in my head all the time.’ (Female, FG4) |
|
| Self-caring for infections |
| Skills; Belief about consequences; Belief about capabilities; Environmental context | ‘Not being a child, you come across things that you’ve had in the past and you either using the tried and tested that you’ve done before… And if it is something that persists or goes on for longer, I go to the pharmacist.’ (Male, FG4) |
|
| Health-seeking behaviours |
| Memory attention and decision-making; Belief about consequences; Environmental context; Emotions | ‘Anything where I’m feeling this is not just an easy cold to manage. This could have quite an impact on other people, because I’m self-employed as well. So it’s a really hard judgement call…’ (Female, FG2) ‘I think after COVID I start to get a bit more anxious now thinking is it something more serious and I think if I had more of a cold now, I’d probably seek more medical attention…’ (Female, FG5) |
|
| Healthcare expectations |
| Reinforcement; Goals; Knowledge; Belief about consequences; Intentions | ‘Hopefully a way to end this illness. I don’t want to come out thinking I’m none the wiser than what I was before. I’d like to know that there’s an end in sight.’ (Male, FG3) ‘That belief that if you take antibiotics too frequently then they don’t actually work as well. That’s always been drummed into me, don’t take antibiotics for everything.’ (Female, FG3) |
|
| Theme | Sub Themes | TDF Domain(s) | Quotes | Implications for Leaflet |
|---|---|---|---|---|
| Roles and responsibilities |
| Belief about capabilities; Optimism; Knowledge; Skills; Social and professional role | ‘I’m optimistic in terms of what I can do to educate the patients, whether than then translates into a reduction in resistance is another matter. But I’m certainly confident in what I do.’ (INT 4, GP, Male) |
|
| Approaches to managing common infections |
| Belief about consequences; Belief about capabilities; Goals Social influences; Environmental context | ‘I personally place a huge emphasis on self-care because in this day and age of consent, shared decision-making, empowering the patient as well, culturally we’ve moved away from being told by healthcare professionals what to do and how to do it exactly. It is very much a collaborative process.’ (FG1, pharmacist, female) ‘[about remote consultations] …can’t physically assess their illnesses and [GPs] will probably prescribe more than if they were able to have that face-to-face physical assessment just to err on the side of caution unfortunately.’ (FG1, pharmacist, female) ‘I worked in a practice which had six partners plus extra doctors and the variation in the threshold for prescribing was enormous… I think if you’ve got that variation at a clinician level it’s very difficult to expect staff to have consistent messaging.’ (FG1, GP, Male) |
|
| Patient attitudes and context |
| Belief about consequences; Belief about capabilities; Environmental context; Social influences | ‘It can be quite clear the patients might have a pathway in their mind about what the treatment should be like, for instance, rather than taking the information on board. I think that’s probably the biggest barrier, patient expectation.’ (INT 1, pharmacist, Male) ‘I have prescribed paracetamol in families that I know would have struggled… but you have to bear in mind that if they really are struggling financially, all the self-care advice that you give is going to be difficult if they can’t afford it.’ (INT 2, nurse practitioner, Female) |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hayes, C.V.; Mahon, B.; Sides, E.; Allison, R.; Lecky, D.M.; McNulty, C.A.M. Empowering Patients to Self-Manage Common Infections: Qualitative Study Informing the Development of an Evidence-Based Patient Information Leaflet. Antibiotics 2021, 10, 1113. https://doi.org/10.3390/antibiotics10091113
Hayes CV, Mahon B, Sides E, Allison R, Lecky DM, McNulty CAM. Empowering Patients to Self-Manage Common Infections: Qualitative Study Informing the Development of an Evidence-Based Patient Information Leaflet. Antibiotics. 2021; 10(9):1113. https://doi.org/10.3390/antibiotics10091113
Chicago/Turabian StyleHayes, Catherine V., Bláthnaid Mahon, Eirwen Sides, Rosie Allison, Donna M. Lecky, and Cliodna A. M. McNulty. 2021. "Empowering Patients to Self-Manage Common Infections: Qualitative Study Informing the Development of an Evidence-Based Patient Information Leaflet" Antibiotics 10, no. 9: 1113. https://doi.org/10.3390/antibiotics10091113
APA StyleHayes, C. V., Mahon, B., Sides, E., Allison, R., Lecky, D. M., & McNulty, C. A. M. (2021). Empowering Patients to Self-Manage Common Infections: Qualitative Study Informing the Development of an Evidence-Based Patient Information Leaflet. Antibiotics, 10(9), 1113. https://doi.org/10.3390/antibiotics10091113