Occurrence of blaNDM-1-Positive Providencia spp. in a Pig Farm of China
Abstract
:1. Introduction
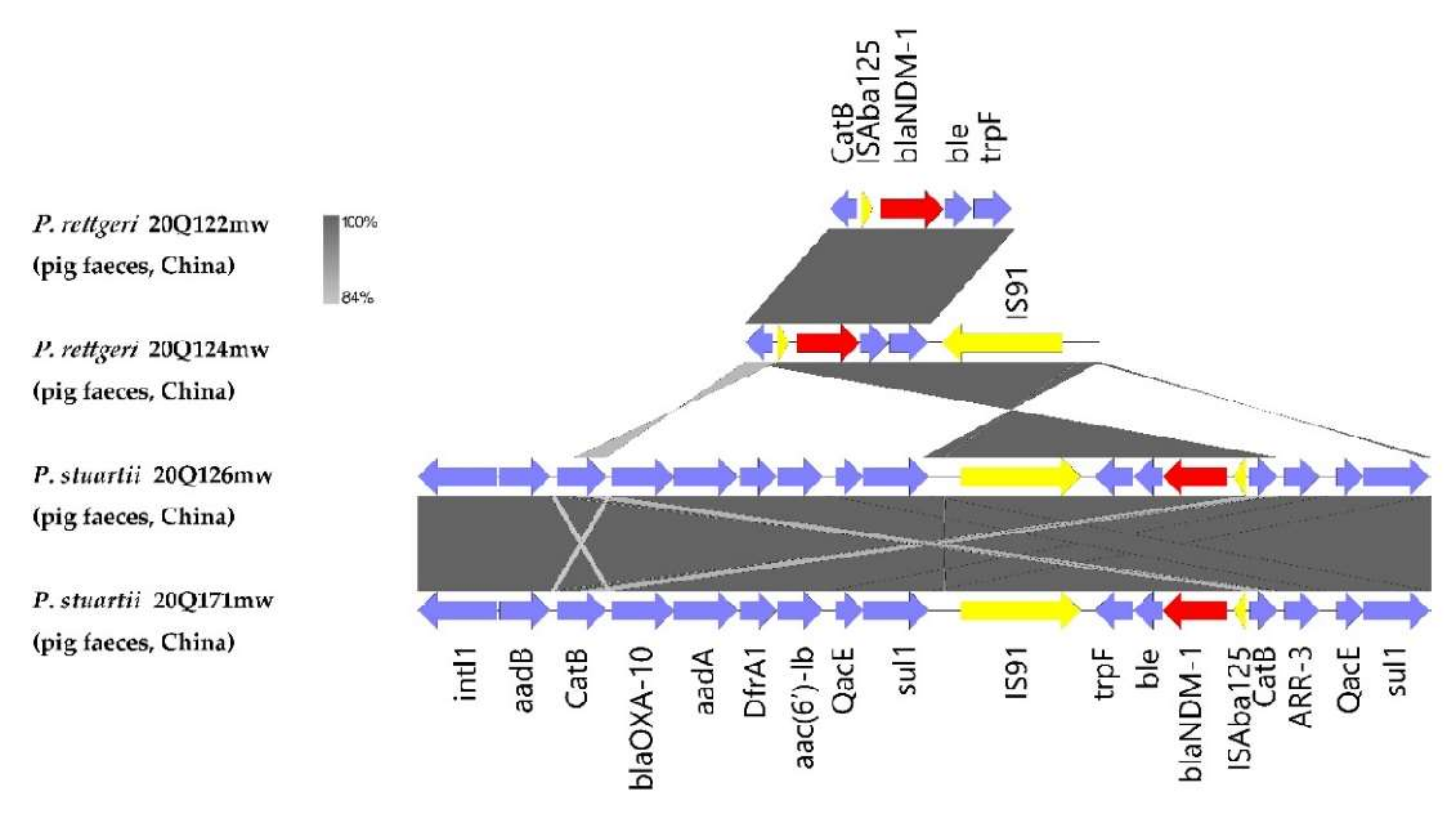
2. Results
2.1. Identification of blaNDM-1-Positive Isolates
2.2. Antimicrobial Susceptibility Profiles and conjugation experiments
2.3. WGS Analysis
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brinkac, L.; Voorhies, A.; Gomez, A.; Nelson, K.E. The Threat of Antimicrobial Resistance on the Human Microbiome. Microb. Ecol. 2017, 74, 1001–1008. [Google Scholar] [CrossRef] [PubMed]
- Sartelli, M.; Weber, D.G.; Ruppé, E.; Bassetti, M.; Wright, B.J.; Ansaloni, L.; Catena, F.; Coccolini, F.; Abu-Zidan, F.M.; Coimbra, R.; et al. Antimicrobials: A global alliance for optimizing their rational use in intra-abdominal infections (AGORA). World J. Emerg. Surg. 2016, 11, 1–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, C.; Rokana, N.; Chandra, M.; Singh, B.P.; Gulhane, R.D.; Gill, J.P.S.; Ray, P.; Puniya, A.K.; Panwar, H. Antimicrobial Resistance: Its Surveillance, Impact, and Alternative Management Strategies in Dairy Animals. Front. Vet. Sci. 2018, 4, 237. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, R.; Li, J.; Wu, Z.; Yin, W.; Schwarz, S.; Tyrrell, J.M.; Zheng, Y.; Wang, S.; Shen, Z.; et al. Comprehensive resistome analysis reveals the prevalence of NDM and MCR-1 in Chinese poultry production. Nat. Microbiol. 2017, 2, 16260. [Google Scholar] [CrossRef]
- Logan, L.K.; Weinstein, R.A. The Epidemiology of Carbapenem-Resistant Enterobacteriaceae: The Impact and Evolution of a Global Menace. J. Infect. Dis. 2017, 215, S28–S36. [Google Scholar] [CrossRef] [Green Version]
- Wu, W.F.Y.; Tang, G.; Qiao, F.; McNally, A.; Zong, Z. Ndm metallo-β-lactamases and their bacterial producers in health care settings. Clin. Microbiol. Rev. 2019, 32, e00115–e00118. [Google Scholar] [CrossRef] [Green Version]
- Yong, D.; Toleman, M.A.; Giske, C.G.; Cho, H.S.; Sundman, K.; Lee, K.; Walsh, T.R. Characterization of a new metallo-beta-lactamase gene, bla(ndm-1), and a novel erythromycin esterase gene carried on a unique genetic structure in klebsiella pneumoniae sequence type 14 from india. Antimicrob. Agents Chemother. 2009, 53, 5046–5054. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Lan, R.; Xiong, Y.; Ye, C.; Yuan, M.; Liu, X.; Chen, X.; Yu, D.; Liu, B.; Lin, W.; et al. Sequential Isolation in a Patient of Raoultella planticola and Escherichia coli Bearing a Novel ISCR1 Element Carrying blaNDM-1. PLoS ONE 2014, 9, e89893. [Google Scholar] [CrossRef]
- Dortet, L.; Poirel, L.; Nordmann, P. Worldwide Dissemination of the NDM-Type Carbapenemases in Gram-Negative Bacteria. BioMed Res. Int. 2014, 2014, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Phan, H.T.T.; Stoesser, N.; Maciuca, I.; Toma, F.; Szekely, E.; Flonta, M.; Hubbard, A.T.M.; Pankhurst, L.; Do, T.; Peto, T.; et al. Illumina short-read and MinION long-read WGS to characterize the molecular epidemiology of an NDM-1 Serratia marcescens outbreak in Romania. J. Antimicrob. Chemother. 2017, 73, 672–679. [Google Scholar] [CrossRef] [Green Version]
- Oliveira, H.; Pinto, G.; Hendrix, H.; Noben, J.P.; Gawor, J.; Kropinski, A.M.; Łobocka, M.; Lavigne, R.; Azeredo, J. A lytic providencia rettgeri virus of potential ther-apeutic value is a deep-branching member of the t5virus genus. Appl. Environ. Microbiol. 2017, 83, e01567-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di, H.; Liang, S.; Li, Q.; Shi, L.; Shima, A.; Meng, H.; Yan, H.; Yamasaki, S. Providencia in retail meats from Guangzhou, China and Osaka, Japan: Prevalence, antimicrobial resistance and characterization of classes 1, 2 and 3 integrons. J. Vet. Med. Sci. 2018, 80, 829–835. [Google Scholar] [CrossRef] [Green Version]
- Andolfo, G.; Schuster, C.; Gharsa, H.B.; Ruocco, M.; Leclerque, A. Genomic analysis of the nomenclatural type strain of the nema-tode-associated entomopathogenic bacterium providencia vermicola. BMC Genomics. 2021, 22, 708. [Google Scholar] [CrossRef] [PubMed]
- Galac, M.R.; Lazzaro, B.P. Comparative genomics of bacteria in the genus providencia isolated from wild drosophila melanogaster. BMC Genom. 2012, 13, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Interaminense, J.A.; Nascimento, D.C.O.; Ventura, R.F.; Batista, J.E.C.; Souza, M.M.C.; Hazin, F.H.V.; Pontes-Filho, N.T.; Lima-Filho, J. Recovery and screening for antibiotic susceptibility of potential bacterial pathogens from the oral cavity of shark species involved in attacks on humans in Recife, Brazil. J. Med. Microbiol. 2010, 59, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Mnif, B.; Ktari, S.; Chaari, A.; Medhioub, F.; Rhimi, F.; Bouaziz, M.; Hammami, A. Nosocomial dissemination of providencia stuartii isolates carrying bla oxa-48, bla per-1, bla cmy-4 and qnra6 in a tunisian hospital. J. Antimicrob. Chemother. 2013, 68, 329–332. [Google Scholar] [CrossRef] [Green Version]
- Yuan, C.; Wei, Y.; Zhang, S.; Cheng, J.; Cheng, X.; Qian, C.; Wang, Y.; Zhang, Y.; Yin, Z.; Chen, H. Comparative Genomic Analysis Reveals Genetic Mechanisms of the Variety of Pathogenicity, Antibiotic Resistance, and Environmental Adaptation of Providencia Genus. Front. Microbiol. 2020, 11, 572642. [Google Scholar] [CrossRef]
- O’Hara CM, B.F.; Miller, J.M. Classification, identification, and clinical significance of proteus, providencia, and morganella. Clin. Microbiol. Rev. 2000, 13, 534–546. [Google Scholar] [CrossRef]
- Lezameta, L.; Cuicapuza, D.; Dávila-Barclay, A.; Torres, S.; Salvatierra, G.; Tsukayama, P.; Tamariz, J. Draft genome sequence of a new delhi metallo-β-lactamase (ndm-1)-producing providencia stuartii strain isolated in Lima, Peru. Microbiol. Resour. Announc. 2020, 9, e00788-20. [Google Scholar] [CrossRef]
- Shen, S.; Huang, X.; Shi, Q.; Guo, Y.; Yang, Y.; Yin, D.; Zhou, X.; Ding, L.; Han, R.; Yu, H.; et al. Occurrence of NDM-1, VIM-1, and OXA-10 Co-Producing Providencia rettgeri Clinical Isolate in China. Front. Cell. Infect. Microbiol. 2022, 11. [Google Scholar] [CrossRef]
- Wailan, A.M.; Paterson, D.L.; Kennedy, K.; Ingram, P.R.; Bursle, E.; Sidjabat, H.E. Genomic characteristics of ndm-producing entero-bacteriaceae isolates in australia and their blandm genetic contexts. Antimicrob Agents Chemother. 2016, 60, 136–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xia, S.; Xiao, S.; Zhang, Q.; Zhao, Q.; Lin, B.; Huang, Z.; Zhuo, C.; Chen, R. Emergence of carbopenem resistant providencia rettgeri and its resistance mechanisms. J. Third Mil. Med. Univ. 2013, 35, 2508–2512. [Google Scholar]
- Köck, R.; Daniels-Haardt, I.; Becker, K.; Mellmann, A.; Friedrich, A.W.; Mevius, D.; Schwarz, S.; Jurke, A. Carbapenem-resistant Enterobacteriaceae in wildlife, food-producing, and companion animals: A systematic review. Clin. Microbiol. Infect. 2018, 24, 1241–1250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rui, P.; Tian, T.; Liu, X.; Zhang, D.; Yang, C.; Liu, X.; Song, T.; Meng, Y.; Ma, Z. Isolation and identification of providencia rettgeri which caused diarrhea in piglets. Chin. J. Vet. Sci. 2017, 37, 1910. [Google Scholar]
- European Food Safety, A.; European Centre for Disease Control. The european union summary report on antimicrobial re-sistance in zoonotic and indicator bacteria from humans, animals and food in 2017. EFSA J. 2019, 17, e05598. [Google Scholar]
- Zhao, Q.; Berglund, B.; Zou, H.; Zhou, Z.; Xia, H.; Zhao, L.; Nilsson, L.E.; Li, X. Dissemination of blandm-5 via incx3 plasmids in car-bapenem-resistant enterobacteriaceae among humans and in the environment in an intensive vegetable cultivation area in eastern china. Environ. Pollut. 2021, 273, 116370. [Google Scholar] [CrossRef]
- Hayakawa, K.; Marchaim, D.; Divine, G.W.; Pogue, J.M.; Kumar, S.; Lephart, P.; Risko, K.; Sobel, J.D.; Kaye, K.S. Growing prevalence of Providencia stuartii associated with the increased usage of colistin at a tertiary health care center. Int. J. Infect. Dis. 2012, 16, e646–e648. [Google Scholar] [CrossRef] [Green Version]
- Qin, S.; Qi, H.; Zhang, Q.; Zhao, D.; Liu, Z.-Z.; Tian, H.; Xu, L.; Xu, H.; Zhou, M.; Feng, X.; et al. Emergence of Extensively Drug-Resistant Proteus mirabilis Harboring a Conjugative NDM-1 Plasmid and a Novel Salmonella Genomic Island 1 Variant, SGI1-Z. Antimicrob. Agents Chemother. 2015, 59, 6601–6604. [Google Scholar] [CrossRef] [Green Version]
- Zhu, X.; Zhang, Y.; Shen, Z.; Xia, L.; Wang, J.; Zhao, L.; Wang, K.; Wang, W.; Hao, Z.; Liu, Z. Characterization of NDM-1-Producing Carbapenemase in Proteus mirabilis among Broilers in China. Microorganisms 2021, 9, 2443. [Google Scholar] [CrossRef]
- Xiang, T.; Chen, C.; Wen, J.; Liu, Y.; Zhang, Q.; Cheng, N.; Wu, X.; Zhang, W. Resistance of Klebsiella pneumoniae Strains Carrying blaNDM–1 Gene and the Genetic Environment of blaNDM–1. Front. Microbiol. 2020, 11, 700. [Google Scholar] [CrossRef]
- Tang, B.; Chang, J.; Cao, L.; Luo, Q.; Xu, H.; Lyu, W.; Qian, M.; Ji, X.; Zhang, Q.; Xia, X.; et al. Characterization of an NDM-5 carbapenemase-producing Escherichia coli ST156 isolate from a poultry farm in Zhejiang, China. BMC Microbiol. 2019, 19, 82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olasz, F.; Kiss, J.; Arini, A.; Arber, W. Terminal inverted repeats of insertion sequence is30 serve as targets for transposition. J. Bacteriol 1997, 179, 7551–7558. [Google Scholar] [CrossRef] [Green Version]
- Weber, R.E.; Pietsch, M.; Fruhauf, A.; Pfeifer, Y.; Martin, M.; Luft, D.; Gatermann, S.; Pfennigwerth, N.; Kaase, M.; Werner, G.; et al. Is26-mediated transfer of bla ndm-1 as the main route of resistance transmission during a polyclonal, multispecies outbreak in a german hospital. Front. Microbiol. 2019, 10, 2817. [Google Scholar] [CrossRef] [PubMed]
- Poirel, L.; Walsh, T.R.; Cuvillier, V.; Nordmann, P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn. Microbiol. Infect. Dis. 2011, 70, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.J.; Petty, N.K.; Beatson, S.A. Easyfig: A genome comparison visualizer. Bioinformatics 2011, 27, 1009–1010. [Google Scholar] [CrossRef]
- Alikhan, N.-F.; Petty, N.K.; Ben Zakour, N.L.; Beatson, S.A. BLAST Ring Image Generator (BRIG): Simple prokaryote genome comparisons. BMC Genom. 2011, 12, 402. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Strains | Sites | Species | Source | MIC (µg/mL) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MEM | AMK | FFC | CL | TGC | GEN | CIP | CTX | CEF | TCY | PTZ | ||||
| 20Q122mw | Piglet room | P. rettgeri | Pig feces | 4 | 4 | >128 | >128 | 1 | 0.25 | 4 | 16 | 16 | 2 | 32 |
| 20Q124mw | Piglet room | P. rettgeri | Pig feces | 4 | 4 | >128 | >128 | 1 | 0.25 | 4 | 16 | 16 | 2 | 32 |
| 20Q126mw | Piglet room | P. stuartii | Pig feces | 4 | 4 | >128 | >128 | 2 | 16 | 4 | 16 | 32 | 4 | 32 |
| 20Q171mw | Fattening room | P. stuartii | Pig feces | 4 | 4 | >128 | >128 | 2 | 16 | 4 | 16 | 32 | 4 | 32 |
| Strains | Source | Species | Sequencing Platforms | Size | GC Content | Antibiotic Resistance Genes |
|---|---|---|---|---|---|---|
| 20Q122mw | Pig feces | P. rettgeri | Illumina Hiseq | 4,612,974 bp | 40.3% | blaNDM-1, blaTEM-116, msr(E), aph(3′)-Ia, aadA1, aac(6′)-Ib-cr, aadA2, dfrA1, dfrA12, sul1, tet(D), mph(E), qnrA1, ARR-3, qacE, floR, catB3 |
| 20Q124mw | Pig feces | P. rettgeri | Illumina Hiseq | 4,607,625 bp | 40.3% | blaNDM-1, msr(E), aac(6′)-Ib-cr, aph(3′)-Ia, aadA2, aadA1, tet(D), qnrA1, sul1, dfrA12, dfrA1, ARR-3, mph(E), qacE, catB3, floR |
| 20Q126mw | Pig feces | P. stuartii | Nanopore minION | 4,712,152 bp | 40.7% | blaNDM-1, blaOXA-10, dfrA1, sul1, sul2, aph(6)-Id, aac(6′)-Ib3, aac(6′)-Ib-cr, aadA1, ant(2″)-Ia, aph(3′)-Ia, aph(3″)-Ib, ARR-3, mph(E), msr(E), qnrD1, tet(B), qacE, catB8, floR, catB3, lnu(G) |
| 20Q171mw | Pig feces | P. stuartii | Illumina Hiseq | 4,665,324 bp | 40.6% | blaNDM-1, blaOXA-10, blaTEM-116, ant(2″)-Ia, aadA1, aph(3′)-Ia, aac(6′)-Ib-cr, aph(3″)-Ib, aph(6)-Id, aac(6’)-Ib3, dfrA1, sul1, sul2, ARR-3, mph(E), msr(E), qnrD1, tet(B), qacE, catB8, catB3, floR, lnu(G) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, W.; Liu, Z.; Lin, H.; Yang, J.; Liu, T.; Zheng, J.; Long, X.; Sun, Z.; Li, J.; Chen, X. Occurrence of blaNDM-1-Positive Providencia spp. in a Pig Farm of China. Antibiotics 2022, 11, 713. https://doi.org/10.3390/antibiotics11060713
Chen W, Liu Z, Lin H, Yang J, Liu T, Zheng J, Long X, Sun Z, Li J, Chen X. Occurrence of blaNDM-1-Positive Providencia spp. in a Pig Farm of China. Antibiotics. 2022; 11(6):713. https://doi.org/10.3390/antibiotics11060713
Chicago/Turabian StyleChen, Wenxin, Zhihong Liu, Hongguang Lin, Jie Yang, Ting Liu, Jiaomei Zheng, Xueming Long, Zhiliang Sun, Jiyun Li, and Xiaojun Chen. 2022. "Occurrence of blaNDM-1-Positive Providencia spp. in a Pig Farm of China" Antibiotics 11, no. 6: 713. https://doi.org/10.3390/antibiotics11060713
APA StyleChen, W., Liu, Z., Lin, H., Yang, J., Liu, T., Zheng, J., Long, X., Sun, Z., Li, J., & Chen, X. (2022). Occurrence of blaNDM-1-Positive Providencia spp. in a Pig Farm of China. Antibiotics, 11(6), 713. https://doi.org/10.3390/antibiotics11060713






