Azithromycin through the Lens of the COVID-19 Treatment
Abstract
:1. Introduction
2. Methods
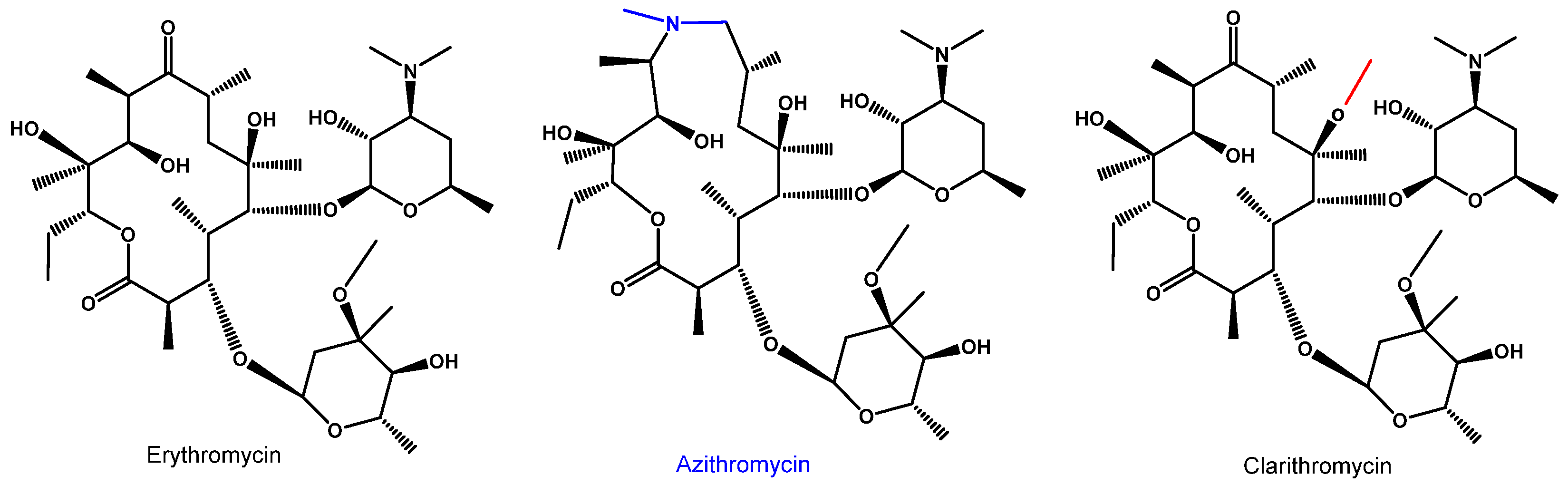
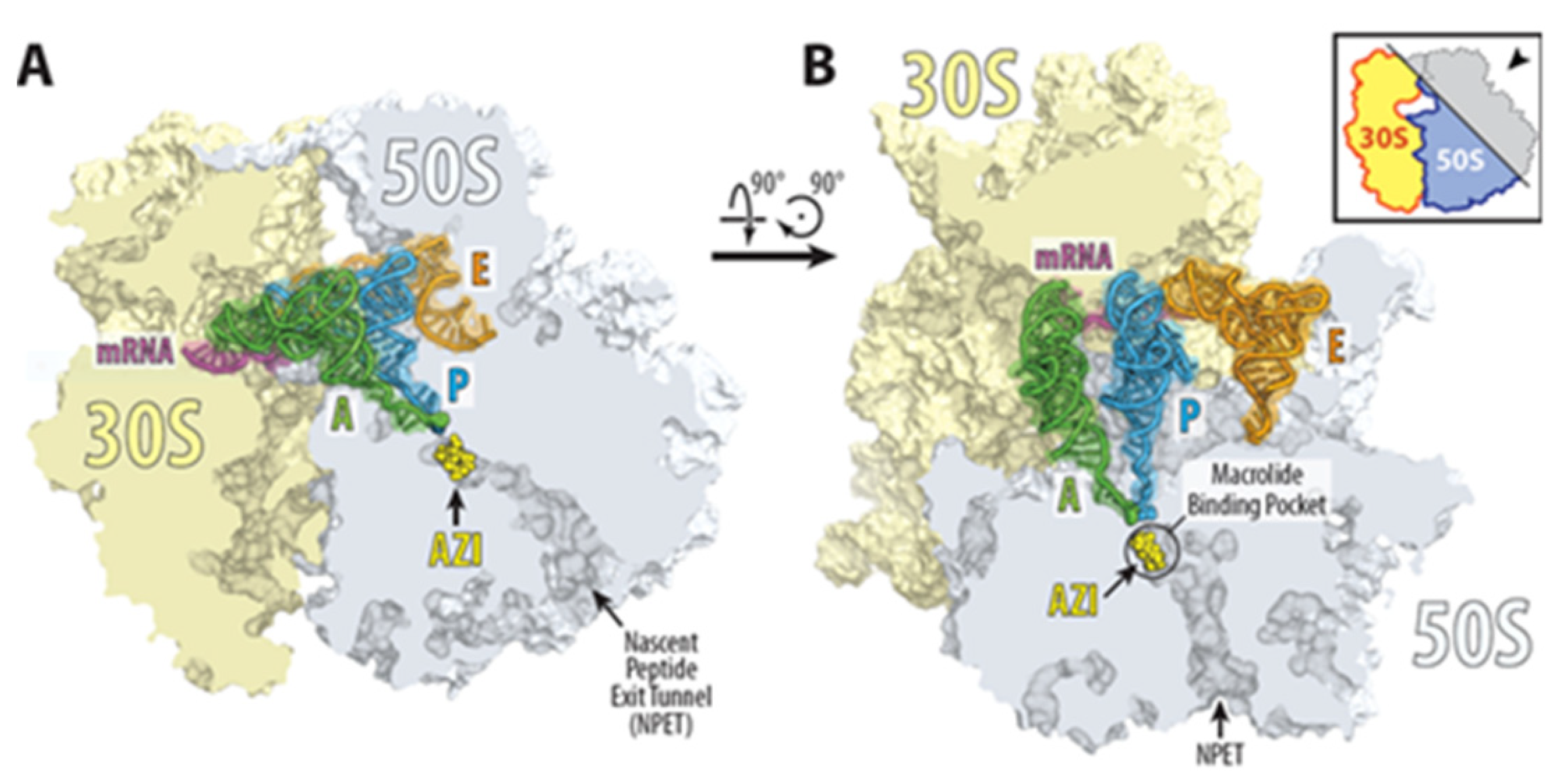
3. Azithromycin as an Antimicrobial Agent
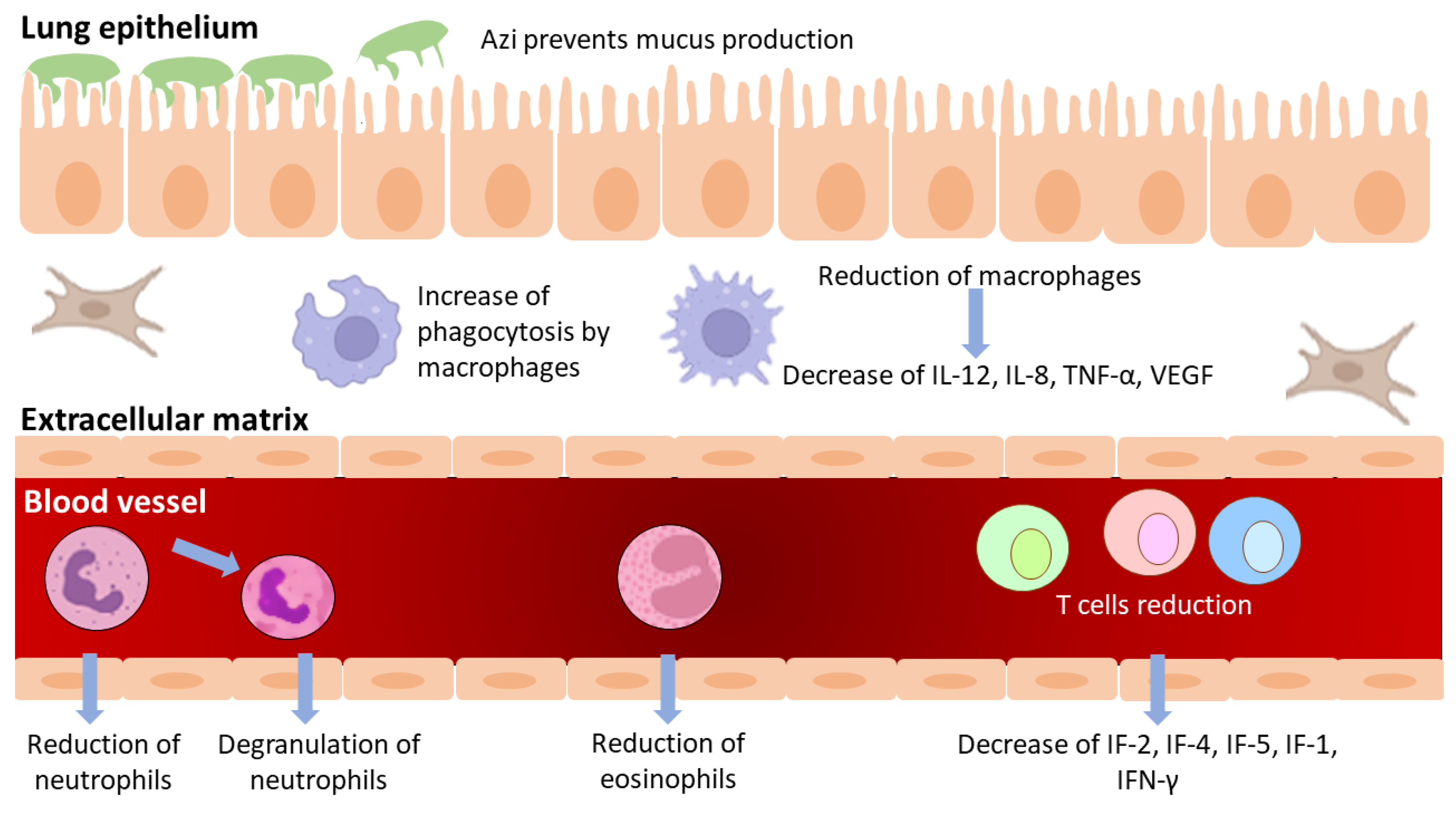
4. Azithromycin as an Anti-Inflammatory Agent
5. Azithromycin as an Antivirus Agent
6. Azithromycin and Betacoronovirus
7. Closing Remarks and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Dinos, G.P. The Macrolide Antibiotic Renaissance. Br. J. Pharmacol. 2017, 174, 2967–2983. [Google Scholar] [CrossRef] [PubMed]
- Barry, A.L.; Jones, R.N.; Thornsberry, C. In Vitro Activities of Azithromycin (CP 62,993), Clarithromycin (A-56268; TE-031), Erythromycin, Roxithromycin, and Clindamycin. Antimicrob. Agents Chemother. 1988, 32, 752–754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barry, A.L.; Fuchs, P.C.; Brown, S.D. Relative Potency of Telithromycin, Azithromycin and Erythromycin against Recent Clinical Isolates of Gram-Positive Cocci. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2001, 20, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, P.B.; Hardy, D.J. Comparative in Vitro Potencies of Nine New Macrolides. Drugs Exp. Clin. Res. 1988, 14, 445–451. [Google Scholar] [PubMed]
- Wise, R. The Development of Macrolides and Related Compounds. J. Antimicrob. Chemother. 1989, 23, 299–300. [Google Scholar] [CrossRef] [Green Version]
- Foulds, G.; Shepard, R.M.; Johnson, R.B. The Pharmacokinetics of Azithromycin in Human Serum and Tissues. J. Antimicrob. Chemother. 1990, 25 (Suppl. A), 73–82. [Google Scholar] [CrossRef]
- Retsema, J.A.; Girard, A.E.; Girard, D.; Milisen, W.B. Relationship of High Tissue Concentrations of Azithromycin to Bactericidal Activity and Efficacy in Vivo. J. Antimicrob. Chemother. 1990, 25 (Suppl. A), 83–89. [Google Scholar] [CrossRef]
- Hardy, D.J.; Guay, D.R.P.; Jones, R.N. Clarithromycin, a Unique Macrolide. A Pharmacokinetic, Microbiological, and Clinical Overview. Diagn. Microbiol. Infect. Dis. 1992, 15, 39–53. [Google Scholar] [CrossRef]
- Wildfeuer, A.; Laufen, H.; Zimmermann, T. Distribution of Orally Administered Azithromycin in Various Blood Compartments. Int. J. Clin. Pharmacol. Ther. 1994, 32, 356–360. [Google Scholar]
- Ayerbe, L.; Risco-Risco, C.; Forgnone, I.; Pérez-Piñar, M.; Ayis, S. Azithromycin in Patients with COVID-19: A Systematic Review and Meta-Analysis. J. Antimicrob. Chemother. 2022, 77, 303–309. [Google Scholar] [CrossRef]
- Oldenburg, C.E.; Pinsky, B.A.; Brogdon, J.; Chen, C.; Ruder, K.; Zhong, L.; Nyatigo, F.; Cook, C.A.; Hinterwirth, A.; Lebas, E.; et al. Effect of Oral Azithromycin vs Placebo on COVID-19 Symptoms in Outpatients With SARS-CoV-2 Infection: A Randomized Clinical Trial. JAMA 2021, 326, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Schlünzen, F.; Zarivach, R.; Harms, J.; Bashan, A.; Tocilj, A.; Albrecht, R.; Yonath, A.; Franceschi, F. Structural Basis for the Interaction of Antibiotics with the Peptidyl Transferase Centre in Eubacteria. Nature 2001, 413, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Bulkley, D.; Innis, C.A.; Blaha, G.; Steitz, T.A. Revisiting the Structures of Several Antibiotics Bound to the Bacterial Ribosome. Proc. Natl. Acad. Sci. USA 2010, 107, 17158–17163. [Google Scholar] [CrossRef] [Green Version]
- Dunkle, J.A.; Xiong, L.; Mankin, A.S.; Cate, J.H.D. Structures of the Escherichia Coli Ribosome with Antibiotics Bound near the Peptidyl Transferase Center Explain Spectra of Drug Action. Proc. Natl. Acad. Sci. USA 2010, 107, 17152–17157. [Google Scholar] [CrossRef] [Green Version]
- Svetlov, M.S.; Plessa, E.; Chen, C.W.; Bougas, A.; Krokidis, M.G.; Dinos, G.P.; Polikanov, Y.S. High-Resolution Crystal Structures of Ribosome-Bound Chloramphenicol and Erythromycin Provide the Ultimate Basis for Their Competition. RNA 2019, 25, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Kannan, K.; Kanabar, P.; Schryer, D.; Florin, T.; Oh, E.; Bahroos, N.; Tenson, T.; Weissman, J.S.; Mankin, A.S. The General Mode of Translation Inhibition by Macrolide Antibiotics. Proc. Natl. Acad. Sci. USA 2014, 111, 15958–15963. [Google Scholar] [CrossRef] [Green Version]
- Vázquez-Laslop, N.; Mankin, A.S. How Macrolide Antibiotics Work. Trends Biochem. Sci. 2018, 43, 668–684. [Google Scholar] [CrossRef]
- Beckert, B.; Leroy, E.C.; Sothiselvam, S.; Bock, L.V.; Svetlov, M.S.; Graf, M.; Arenz, S.; Abdelshahid, M.; Seip, B.; Grubmüller, H.; et al. Structural and Mechanistic Basis for Translation Inhibition by Macrolide and Ketolide Antibiotics. Nat. Commun. 2021, 12, 4466. [Google Scholar] [CrossRef]
- Ishimoto, H.; Mukae, H.; Sakamoto, N.; Amenomori, M.; Kitazaki, T.; Imamura, Y.; Fujita, H.; Ishii, H.; Nakayama, S.; Yanagihara, K.; et al. Different Effects of Telithromycin on MUC5AC Production Induced by Human Neutrophil Peptide-1 or Lipopolysaccharide in NCI-H292 Cells Compared with Azithromycin and Clarithromycin. J. Antimicrob. Chemother. 2009, 63, 109–114. [Google Scholar] [CrossRef] [Green Version]
- Nakayama, I. Macrolides in clinical practice. In Macrolide Antibiotics: Chemistry, Biology and Practice, 1st ed.; Omura, S., Ed.; Academic Press: Orlando, FL, USA, 2022. [Google Scholar]
- Firth, A.; Prathapan, P. Azithromycin: The First Broad-Spectrum Therapeutic. Eur. J. Med. Chem. 2020, 207, 112739. [Google Scholar] [CrossRef]
- Taylor, W.R.; Richie, T.L.; Fryauff, D.J.; Ohrt, C.; Picarima, H.; Tang, D.; Murphy, G.S.; Widjaja, H.; Braitman, D.; Tjitra, E.; et al. Tolerability of Azithromycin as Malaria Prophylaxis in Adults in Northeast Papua, Indonesia. Antimicrob. Agents Chemother. 2003, 47, 2199–2203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parnham, M.J.; Erakovic Haber, V.; Giamarellos-Bourboulis, E.J.; Perletti, G.; Verleden, G.M.; Vos, R. Azithromycin: Mechanisms of Action and Their Relevance for Clinical Applications. Pharmacol. Ther. 2014, 143, 225–245. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Model List of Essential Medicines - 22nd List. 2021. Available online: https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2021.02. (accessed on 15 February 2022).
- Gibson, P.G.; Yang, I.A.; Upham, J.W.; Reynolds, P.N.; Hodge, S.; James, A.L.; Jenkins, C.; Peters, M.J.; Marks, G.B.; Baraket, M.; et al. Effect of Azithromycin on Asthma Exacerbations and Quality of Life in Adults with Persistent Uncontrolled Asthma (AMAZES): A Randomised, Double-Blind, Placebo-Controlled Trial. Lancet (Lond. Engl.) 2017, 390, 659–668. [Google Scholar] [CrossRef] [Green Version]
- Hansen, M.P.; Scott, A.M.; McCullough, A.; Thorning, S.; Aronson, J.K.; Beller, E.M.; Glasziou, P.P.; Hoffmann, T.C.; Clark, J.; Del Mar, C.B. Adverse Events in People Taking Macrolide Antibiotics versus Placebo for Any Indication. Cochrane Database Syst. Rev. 2019, 18, CD011825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zimmermann, P.; Ziesenitz, V.C.; Curtis, N.; Ritz, N. The Immunomodulatory Effects of Macrolides-A Systematic Review of the Underlying Mechanisms. Front. Immunol. 2018, 9, 302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kudoh, S.; Azuma, A.; Yamamoto, M.; Izumi, T.; Ando, M. Improvement of Survival in Patients with Diffuse Panbronchiolitis Treated with Low-Dose Erythromycin. Am. J. Respir. Crit. Care Med. 1998, 157, 1829–1832. [Google Scholar] [CrossRef]
- Zarogoulidis, P.; Papanas, N.; Kioumis, I.; Chatzaki, E.; Maltezos, E.; Zarogoulidis, K. Macrolides: From in Vitro Anti-Inflammatory and Immunomodulatory Properties to Clinical Practice in Respiratory Diseases. Eur. J. Clin. Pharmacol. 2012, 68, 479–503. [Google Scholar] [CrossRef] [PubMed]
- Weng, D.; Wu, Q.; Chen, X.-Q.; Du, Y.-K.; Chen, T.; Li, H.; Tang, D.-L.; Li, Q.-H.; Zhang, Y.; Lu, L.-Q.; et al. Azithromycin Treats Diffuse Panbronchiolitis by Targeting T Cells via Inhibition of MTOR Pathway. Biomed. Pharmacother. 2019, 110, 440–448. [Google Scholar] [CrossRef]
- Wilms, E.B.; Touw, D.J.; Heijerman, H.G.M. Pharmacokinetics of Azithromycin in Plasma, Blood, Polymorphonuclear Neutrophils and Sputum during Long-Term Therapy in Patients with Cystic Fibrosis. Ther. Drug Monit. 2006, 28, 219–225. [Google Scholar] [CrossRef]
- Oliver, M.E.; Hinks, T.S.C. Azithromycin in Viral Infections. Rev. Med. Virol. 2021, 31, e2163. [Google Scholar] [CrossRef]
- Reijnders, T.D.Y.; Saris, A.; Schultz, M.J.; van der Poll, T. Immunomodulation by Macrolides: Therapeutic Potential for Critical Care. Lancet. Respir. Med. 2020, 8, 619–630. [Google Scholar] [CrossRef]
- Araki, N.; Yanagihara, K.; Morinaga, Y.; Yamada, K.; Nakamura, S.; Yamada, Y.; Kohno, S.; Kamihira, S. Azithromycin Inhibits Nontypeable Haemophilus Influenzae-Induced MUC5AC Expression and Secretion via Inhibition of Activator Protein-1 in Human Airway Epithelial Cells. Eur. J. Pharmacol. 2010, 644, 209–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hodge, S.; Hodge, G.; Jersmann, H.; Matthews, G.; Ahern, J.; Holmes, M.; Reynolds, P.N. Azithromycin Improves Macrophage Phagocytic Function and Expression of Mannose Receptor in Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2008, 178, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Persson, H.L.; Vainikka, L.K.; Sege, M.; Wennerström, U.; Dam-Larsen, S.; Persson, J. Leaky Lysosomes in Lung Transplant Macrophages: Azithromycin Prevents Oxidative Damage. Respir. Res. 2012, 13, 83. [Google Scholar] [CrossRef] [Green Version]
- Murphy, B.S.; Sundareshan, V.; Cory, T.J.; Hayes, D.J.; Anstead, M.I.; Feola, D.J. Azithromycin Alters Macrophage Phenotype. J. Antimicrob. Chemother. 2008, 61, 554–560. [Google Scholar] [CrossRef] [Green Version]
- Legssyer, R.; Huaux, F.; Lebacq, J.; Delos, M.; Marbaix, E.; Lebecque, P.; Lison, D.; Scholte, B.J.; Wallemacq, P.; Leal, T. Azithromycin Reduces Spontaneous and Induced Inflammation in DeltaF508 Cystic Fibrosis Mice. Respir. Res. 2006, 7, 134. [Google Scholar] [CrossRef] [Green Version]
- Yamauchi, K.; Shibata, Y.; Kimura, T.; Abe, S.; Inoue, S.; Osaka, D.; Sato, M.; Igarashi, A.; Kubota, I. Azithromycin Suppresses Interleukin-12p40 Expression in Lipopolysaccharide and Interferon-Gamma Stimulated Macrophages. Int. J. Biol. Sci. 2009, 5, 667–678. [Google Scholar] [CrossRef] [Green Version]
- Hodge, S.; Hodge, G.; Brozyna, S.; Jersmann, H.; Holmes, M.; Reynolds, P.N. Azithromycin Increases Phagocytosis of Apoptotic Bronchial Epithelial Cells by Alveolar Macrophages. Eur. Respir. J. 2006, 28, 486–495. [Google Scholar] [CrossRef]
- Yamaryo, T.; Oishi, K.; Yoshimine, H.; Tsuchihashi, Y.; Matsushima, K.; Nagatake, T. Fourteen-Member Macrolides Promote the Phosphatidylserine Receptor-Dependent Phagocytosis of Apoptotic Neutrophils by Alveolar Macrophages. Antimicrob. Agents Chemother. 2003, 47, 48–53. [Google Scholar] [CrossRef] [Green Version]
- Huang, S.-W.; Chen, Y.-J.; Wang, S.-T.; Ho, L.-W.; Kao, J.-K.; Narita, M.; Takahashi, M.; Wu, C.-Y.; Cheng, H.-Y.; Shieh, J.-J. Azithromycin Impairs TLR7 Signaling in Dendritic Cells and Improves the Severity of Imiquimod-Induced Psoriasis-like Skin Inflammation in Mice. J. Dermatol. Sci. 2016, 84, 59–70. [Google Scholar] [CrossRef]
- Culić, O.; Eraković, V.; Cepelak, I.; Barisić, K.; Brajsa, K.; Ferencić, Z.; Galović, R.; Glojnarić, I.; Manojlović, Z.; Munić, V.; et al. Azithromycin Modulates Neutrophil Function and Circulating Inflammatory Mediators in Healthy Human Subjects. Eur. J. Pharmacol. 2002, 450, 277–289. [Google Scholar] [CrossRef]
- Criqui, G.I.; Solomon, C.; Welch, B.S.; Ferrando, R.E.; Boushey, H.A.; Balmes, J.R. Effects of Azithromycin on Ozone-Induced Airway Neutrophilia and Cytokine Release. Eur. Respir. J. 2000, 15, 856–862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aubert, J.D.; Juillerat-Jeanneret, L.; Fioroni, P.; Dayer, P.; Plan, P.A.; Leuenberger, P. Function of Human Alveolar Macrophages after a 3-Day Course of Azithromycin in Healthy Volunteers. Pulm. Pharmacol. Ther. 1998, 11, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Southern, K.W.; Barker, P.M.; Solis-Moya, A.; Patel, L. Macrolide Antibiotics for Cystic Fibrosis. Cochrane database Syst. Rev. 2012, 11, CD002203. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.; Schechter, M.S.; Sly, P.D.; Winfield, K.; Smith, J.; Brennan, S.; Shinkai, M.; Henke, M.O.; Rubin, B.K. Clarithromycin Therapy for Patients with Cystic Fibrosis: A Randomized Controlled Trial. Pediatr. Pulmonol. 2012, 47, 551–557. [Google Scholar] [CrossRef]
- Gualdoni, G.A.; Lingscheid, T.; Schmetterer, K.G.; Hennig, A.; Steinberger, P.; Zlabinger, G.J. Azithromycin Inhibits IL-1 Secretion and Non-Canonical Inflammasome Activation. Sci. Rep. 2015, 5, 12016. [Google Scholar] [CrossRef] [Green Version]
- Böttger, E.C.; Springer, B.; Prammananan, T.; Kidan, Y.; Sander, P. Structural Basis for Selectivity and Toxicity of Ribosomal Antibiotics. EMBO Rep. 2001, 2, 318–323. [Google Scholar] [CrossRef] [Green Version]
- Brusselle, G.G.; Vanderstichele, C.; Jordens, P.; Deman, R.; Slabbynck, H.; Ringoet, V.; Verleden, G.; Demedts, I.K.; Verhamme, K.; Delporte, A.; et al. Azithromycin for Prevention of Exacerbations in Severe Asthma (AZISAST): A Multicentre Randomised Double-Blind Placebo-Controlled Trial. Thorax 2013, 68, 322–329. [Google Scholar] [CrossRef] [Green Version]
- Gielen, V.; Johnston, S.L.; Edwards, M.R. Azithromycin Induces Anti-Viral Responses in Bronchial Epithelial Cells. Eur. Respir. J. 2010, 36, 646–654. [Google Scholar] [CrossRef] [Green Version]
- Sajjan, U.S.; Jia, Y.; Newcomb, D.C.; Bentley, J.K.; Lukacs, N.W.; LiPuma, J.J.; Hershenson, M.B.H. Influenzae Potentiates Airway Epithelial Cell Responses to Rhinovirus by Increasing ICAM-1 and TLR3 Expression. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2006, 20, 2121–2123. [Google Scholar] [CrossRef] [Green Version]
- Taylor, S.L.; Leong, L.E.X.; Mobegi, F.M.; Choo, J.M.; Wesselingh, S.; Yang, I.A.; Upham, J.W.; Reynolds, P.N.; Hodge, S.; James, A.L.; et al. Long-Term Azithromycin Reduces Haemophilus Influenzae and Increases Antibiotic Resistance in Severe Asthma. Am. J. Respir. Crit. Care Med. 2019, 200, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.L.; Ivey, K.L.; Gibson, P.G.; Simpson, J.L.; Rogers, G.B. Airway Abundance of Haemophilus Influenzae Predicts Response to Azithromycin in Adults with Persistent Uncontrolled Asthma. Eur. Respir. J. 2020, 56, 2000194. [Google Scholar] [CrossRef] [PubMed]
- Schögler, A.; Kopf, B.S.; Edwards, M.R.; Johnston, S.L.; Casaulta, C.; Kieninger, E.; Jung, A.; Moeller, A.; Geiser, T.; Regamey, N.; et al. Novel Antiviral Properties of Azithromycin in Cystic Fibrosis Airway Epithelial Cells. Eur. Respir. J. 2015, 45, 428–439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tran, D.H.; Sugamata, R.; Hirose, T.; Suzuki, S.; Noguchi, Y.; Sugawara, A.; Ito, F.; Yamamoto, T.; Kawachi, S.; Akagawa, K.S.; et al. Azithromycin, a 15-Membered Macrolide Antibiotic, Inhibits Influenza A(H1N1)Pdm09 Virus Infection by Interfering with Virus Internalization Process. J. Antibiot. (Tokyo). 2019, 72, 759–768. [Google Scholar] [CrossRef] [PubMed]
- Retallack, H.; Di Lullo, E.; Arias, C.; Knopp, K.A.; Laurie, M.T.; Sandoval-Espinosa, C.; Mancia Leon, W.R.; Krencik, R.; Ullian, E.M.; Spatazza, J.; et al. Zika Virus Cell Tropism in the Developing Human Brain and Inhibition by Azithromycin. Proc. Natl. Acad. Sci. USA 2016, 113, 14408–14413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madrid, P.B.; Panchal, R.G.; Warren, T.K.; Shurtleff, A.C.; Endsley, A.N.; Green, C.E.; Kolokoltsov, A.; Davey, R.; Manger, I.D.; Gilfillan, L.; et al. Evaluation of Ebola Virus Inhibitors for Drug Repurposing. ACS Infect. Dis. 2015, 1, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Damle, B.; Vourvahis, M.; Wang, E.; Leaney, J.; Corrigan, B. Clinical Pharmacology Perspectives on the Antiviral Activity of Azithromycin and Use in COVID-19. Clin. Pharmacol. Ther. 2020, 108, 201–211. [Google Scholar] [CrossRef]
- Menzel, M.; Akbarshahi, H.; Bjermer, L.; Uller, L. Azithromycin Induces Anti-Viral Effects in Cultured Bronchial Epithelial Cells from COPD Patients. Sci. Rep. 2016, 6, 28698. [Google Scholar] [CrossRef] [Green Version]
- Zeng, S.; Meng, X.; Huang, Q.; Lei, N.; Zeng, L.; Jiang, X.; Guo, X. Spiramycin and Azithromycin, Safe for Administration to Children, Exert Antiviral Activity against Enterovirus A71 in Vitro and in Vivo. Int. J. Antimicrob. Agents 2019, 53, 362–369. [Google Scholar] [CrossRef]
- de Wit, E.; van Doremalen, N.; Falzarano, D.; Munster, V.J. SARS and MERS: Recent Insights into Emerging Coronaviruses. Nat. Rev. Microbiol. 2016, 14, 523–534. [Google Scholar] [CrossRef]
- Ou, X.; Liu, Y.; Lei, X.; Li, P.; Mi, D.; Ren, L.; Guo, L.; Guo, R.; Chen, T.; Hu, J.; et al. Characterization of Spike Glycoprotein of SARS-CoV-2 on Virus Entry and Its Immune Cross-Reactivity with SARS-CoV. Nat. Commun. 2020, 11, 1620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E. Remdesivir for the Treatment of COVID-19 - Preliminary Report. Reply. N. Engl. J. Med. 2020, 383, 994. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, D.; Du, G.; Du, R.; Zhao, J.; Jin, Y.; Fu, S.; Gao, L.; Cheng, Z.; Lu, Q.; et al. Remdesivir in Adults with Severe COVID-19: A Randomised, Double-Blind, Placebo-Controlled, Multicentre Trial. Lancet (Lond. Engl. ) 2020, 395, 1569–1578. [Google Scholar] [CrossRef]
- Williamson, B.N.; Feldmann, F.; Schwarz, B.; Meade-White, K.; Porter, D.P.; Schulz, J.; van Doremalen, N.; Leighton, I.; Yinda, C.K.; Pérez-Pérez, L.; et al. Clinical Benefit of Remdesivir in Rhesus Macaques Infected with SARS-CoV-2. Nature 2020, 585, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Andreani, J.; Le Bideau, M.; Duflot, I.; Jardot, P.; Rolland, C.; Boxberger, M.; Wurtz, N.; Rolain, J.-M.; Colson, P.; La Scola, B.; et al. In Vitro Testing of Combined Hydroxychloroquine and Azithromycin on SARS-CoV-2 Shows Synergistic Effect. Microb. Pathog. 2020, 145, 104228. [Google Scholar] [CrossRef]
- Touret, F.; Gilles, M.; Barral, K.; Nougairède, A.; van Helden, J.; Decroly, E.; de Lamballerie, X.; Coutard, B. In Vitro Screening of a FDA Approved Chemical Library Reveals Potential Inhibitors of SARS-CoV-2 Replication. Sci. Rep. 2020, 10, 13093. [Google Scholar] [CrossRef]
- Gautret, P.; Lagier, J.-C.; Parola, P.; Hoang, V.T.; Meddeb, L.; Mailhe, M.; Doudier, B.; Courjon, J.; Giordanengo, V.; Vieira, V.E.; et al. Hydroxychloroquine and Azithromycin as a Treatment of COVID-19: Results of an Open-Label Non-Randomized Clinical Trial. Int. J. Antimicrob. Agents 2020, 56, 105949. [Google Scholar] [CrossRef]
- Gyselinck, I.; Janssens, W.; Verhamme, P.; Vos, R. Rationale for Azithromycin in COVID-19: An Overview of Existing Evidence. BMJ open Respir. Res. 2021, 8. [Google Scholar] [CrossRef]
- Maisonnasse, P.; Guedj, J.; Contreras, V.; Behillil, S.; Solas, C.; Marlin, R.; Naninck, T.; Pizzorno, A.; Lemaitre, J.; Gonçalves, A.; et al. Hydroxychloroquine Use against SARS-CoV-2 Infection in Non-Human Primates. Nature 2020, 585, 584–587. [Google Scholar] [CrossRef]
- Albani, F.; Fusina, F.; Giovannini, A.; Ferretti, P.; Granato, A.; Prezioso, C.; Divizia, D.; Sabaini, A.; Marri, M.; Malpetti, E.; et al. Impact of Azithromycin and/or Hydroxychloroquine on Hospital Mortality in COVID-19. J. Clin. Med. 2020, 9, 280. [Google Scholar] [CrossRef]
- Arshad, S.; Kilgore, P.; Chaudhry, Z.S.; Jacobsen, G.; Wang, D.D.; Huitsing, K.; Brar, I.; Alangaden, G.J.; Ramesh, M.S.; McKinnon, J.E.; et al. Treatment with Hydroxychloroquine, Azithromycin, and Combination in Patients Hospitalized with COVID-19. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2020, 97, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Sekhavati, E.; Jafari, F.; SeyedAlinaghi, S.; Jamalimoghadamsiahkali, S.; Sadr, S.; Tabarestani, M.; Pirhayati, M.; Zendehdel, A.; Manafi, N.; Hajiabdolbaghi, M.; et al. Safety and Effectiveness of Azithromycin in Patients with COVID-19: An Open-Label Randomised Trial. Int. J. Antimicrob. Agents 2020, 56, 106143. [Google Scholar] [CrossRef] [PubMed]
- Lauriola, M.; Pani, A.; Ippoliti, G.; Mortara, A.; Milighetti, S.; Mazen, M.; Perseghin, G.; Pastori, D.; Grosso, P.; Scaglione, F. Effect of Combination Therapy of Hydroxychloroquine and Azithromycin on Mortality in Patients With COVID-19. Clin. Transl. Sci. 2020, 13, 1071–1076. [Google Scholar] [CrossRef] [PubMed]
- Tanriverdİ, E.; Çörtük, M.; Yildirim, B.Z.; Uğur Chousein, E.G.; Turan, D.; Çinarka, H.; Özgül, M.A.; Çetinkaya, E. Hydroxychloroquine plus Azithromycin and Early Hospital Admission Are Beneficial in COVID-19 Patients: Turkish Experience with Real-Life Data. Turkish J. Med. Sci. 2021, 51, 10–15. [Google Scholar] [CrossRef]
- Guérin, V.; Lévy, P.; Thomas, J.-L.; Lardenois, T.; Lacrosse, P.; Sarrazin, E.; de Andreis, N.R.; Wonner, M. Azithromycin and Hydroxychloroquine Accelerate Recovery of Outpatients with Mild/Moderate COVID-19. Asian J. Med. Heal. 2020, 18, 15–55. [Google Scholar] [CrossRef]
- Kuderer, N.M.; Choueiri, T.K.; Shah, D.P.; Shyr, Y.; Rubinstein, S.M.; Rivera, D.R.; Shete, S.; Hsu, C.-Y.; Desai, A.; de Lima Lopes, G.J.; et al. Clinical Impact of COVID-19 on Patients with Cancer (CCC19): A Cohort Study. Lancet (Lond. Engl.) 2020, 395, 1907–1918. [Google Scholar] [CrossRef]
- Rosenberg, E.S.; Dufort, E.M.; Udo, T.; Wilberschied, L.A.; Kumar, J.; Tesoriero, J.; Weinberg, P.; Kirkwood, J.; Muse, A.; DeHovitz, J.; et al. Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State. JAMA 2020, 323, 2493–2502. [Google Scholar] [CrossRef]
- Cavalcanti, A.B.; Zampieri, F.G.; Rosa, R.G.; Azevedo, L.C.P.; Veiga, V.C.; Avezum, A.; Damiani, L.P.; Marcadenti, A.; Kawano-Dourado, L.; Lisboa, T.; et al. Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate COVID-19. N. Engl. J. Med. 2020, 383, 2041–2052. [Google Scholar] [CrossRef]
- Ayerbe, L.; Risco-Risco, C.; Ayis, S. The Association of Treatment with Hydroxychloroquine and Hospital Mortality in COVID-19 Patients. Intern. Emerg. Med. 2020, 15, 1501–1506. [Google Scholar] [CrossRef]
- Lammers, A.J.J.; Brohet, R.M.; Theunissen, R.E.P.; Koster, C.; Rood, R.; Verhagen, D.W.M.; Brinkman, K.; Hassing, R.J.; Dofferhoff, A.; El Moussaoui, R.; et al. Response to Correspondence Concerning: “Early Hydroxychloroquine but Not Chloroquine Use Reduces ICU Admission in COVID-19 Patients”. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2021, 103, 478–479. [Google Scholar] [CrossRef]
- Kamel, A.M.; Monem, M.S.A.; Sharaf, N.A.; Magdy, N.; Farid, S.F. Efficacy and Safety of Azithromycin in COVID-19 Patients: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Rev. Med. Virol. 2022, 32, e2258. [Google Scholar] [CrossRef] [PubMed]
- Echeverría-Esnal, D.; Martin-Ontiyuelo, C.; Navarrete-Rouco, M.E.; De-Antonio Cuscó, M.; Ferrández, O.; Horcajada, J.P.; Grau, S. Azithromycin in the Treatment of COVID-19: A Review. Expert Rev. Anti. Infect. Ther. 2021, 19, 147–163. [Google Scholar] [CrossRef] [PubMed]
- Szente Fonseca, S.N.; de Queiroz Sousa, A.; Wolkoff, A.G.; Moreira, M.S.; Pinto, B.C.; Valente Takeda, C.F.; Rebouças, E.; Vasconcellos Abdon, A.P.; Nascimento, A.L.A.; Risch, H.A. Risk of Hospitalization for COVID-19 Outpatients Treated with Various Drug Regimens in Brazil: Comparative Analysis. Travel Med. Infect. Dis. 2020, 38, 101906. [Google Scholar] [CrossRef]
- Geleris, J.; Sun, Y.; Platt, J.; Zucker, J.; Baldwin, M.; Hripcsak, G.; Labella, A.; Manson, D.K.; Kubin, C.; Barr, R.G.; et al. Observational Study of Hydroxychloroquine in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2020, 382, 2411–2418. [Google Scholar] [CrossRef] [PubMed]
- Furtado, R.H.M.; Berwanger, O.; Fonseca, H.A.; Corrêa, T.D.; Ferraz, L.R.; Lapa, M.G.; Zampieri, F.G.; Veiga, V.C.; Azevedo, L.C.P.; Rosa, R.G.; et al. Azithromycin in Addition to Standard of Care versus Standard of Care Alone in the Treatment of Patients Admitted to the Hospital with Severe COVID-19 in Brazil (COALITION II): A Randomised Clinical Trial. Lancet (Lond. Engl.) 2020, 396, 959–967. [Google Scholar] [CrossRef]
- Azithromycin for Community Treatment of Suspected COVID-19 in People at Increased Risk of an Adverse Clinical Course in the UK (PRINCIPLE): A Randomised, Controlled, Open-Label, Adaptive Platform Trial. Lancet (Lond. Engl.) 2021, 397, 1063–1074. [CrossRef]
- Hinks, T.S.C.; Barber, V.S.; Black, J.; Dutton, S.J.; Jabeen, M.; Melhorn, J.; Rahman, N.M.; Richards, D.; Lasserson, D.; Pavord, I.D.; et al. A Multi-Centre Open-Label Two-Arm Randomised Superiority Clinical Trial of Azithromycin versus Usual Care in Ambulatory COVID-19: Study Protocol for the ATOMIC2 Trial. Trials 2020, 21, 718. [Google Scholar] [CrossRef]
- Tocilizumab in Patients Admitted to Hospital with COVID-19 (RECOVERY): A Randomised, Controlled, Open-Label, Platform Trial. Lancet (Lond. Engl.) 2021, 397, 1637–1645. [CrossRef]
- Bogdanić, N.; Močibob, L.; Vidović, T.; Soldo, A.; Begovać, J. Azithromycin Consumption during the COVID-19 Pandemic in Croatia, 2020. PLoS One 2022, 17, e0263437. [Google Scholar] [CrossRef]
- Gouin, K.A.; Creasy, S.; Beckerson, M.; Wdowicki, M.; Hicks, L.A.; Lind, J.N.; Geller, A.I.; Budnitz, D.S.; Kabbani, S. Trends in Prescribing of Antibiotics and Drugs Investigated for Coronavirus Disease 2019 (COVID-19) Treatment in US Nursing Home Residents During the COVID-19 Pandemic. Clin. Infect. Dis. an Off. Publ. Infect. Dis. Soc. Am. 2022, 74, 74–82. [Google Scholar] [CrossRef]
- Stoichitoiu, L.E.; Pinte, L.; Ceasovschih, A.; Cernat, R.C.; Vlad, N.D.; Padureanu, V.; Sorodoc, L.; Hristea, A.; Purcarea, A.; Badea, C.; et al. In-Hospital Antibiotic Use for COVID-19: Facts and Rationales Assessed through a Mixed-Methods Study. J. Clin. Med. 2022, 11, 3194. [Google Scholar] [CrossRef] [PubMed]
- Prestinaci, F.; Pezzotti, P.; Pantosti, A. Antimicrobial Resistance: A Global Multifaceted Phenomenon. Pathog. Glob. Health 2015, 109, 309–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomes, C.; Ruiz-Roldán, L.; Mateu, J.; Ochoa, T.J.; Ruiz, J. Azithromycin Resistance Levels and Mechanisms in Escherichia Coli. Sci. Rep. 2019, 9, 6089. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bommer, U.; Burkhardt, N.; Junemann, R.; Spahn, C.M.T.; Triana- Alonso, F.J.; Nierhaus, K.H. Ribosomes and Polysomes. In Subcellular Fractionation. A Practical Approach; Graham, J.D., Rickwoods, E., Eds.; IRL Press at Oxford University Press: Oxford, UK, 1996; pp. 271–301. [Google Scholar]
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global Burden of Bacterial Antimicrobial Resistance in 2019: A Systematic Analysis. Lancet (Lond. Engl.) 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Lansbury, L.; Lim, B.; Baskaran, V.; Lim, W.S. Co-Infections in People with COVID-19: A Systematic Review and Meta-Analysis. J. Infect. 2020, 81, 266–275. [Google Scholar] [CrossRef]
- Chertow, D.S.; Memoli, M.J. Bacterial Coinfection in Influenza: A Grand Rounds Review. JAMA 2013, 309, 275–282. [Google Scholar] [CrossRef]
- Ishaqui, A.A.; Khan, A.H.; Sulaiman, S.A.S.; Alsultan, M.T.; Khan, I.; Naqvi, A.A. Assessment of Efficacy of Oseltamivir-Azithromycin Combination Therapy in Prevention of Influenza-A (H1N1)Pdm09 Infection Complications and Rapidity of Symptoms Relief. Expert Rev. Respir. Med. 2020, 14, 533–541. [Google Scholar] [CrossRef] [Green Version]
- Lee, N.; Wong, C.-K.; Chan, M.C.W.; Yeung, E.S.L.; Tam, W.W.S.; Tsang, O.T.Y.; Choi, K.-W.; Chan, P.K.S.; Kwok, A.; Lui, G.C.Y.; et al. Anti-Inflammatory Effects of Adjunctive Macrolide Treatment in Adults Hospitalized with Influenza: A Randomized Controlled Trial. Antiviral Res. 2017, 144, 48–56. [Google Scholar] [CrossRef]
- Segala, F.V.; Bavaro, D.F.; Di Gennaro, F.; Salvati, F.; Marotta, C.; Saracino, A.; Murri, R.; Fantoni, M. Impact of SARS-CoV-2 Epidemic on Antimicrobial Resistance: A Literature Review. Viruses 2021, 13, 2110. [Google Scholar] [CrossRef]
- Pinte, L.; Ceasovschih, A.; Niculae, C.-M.; Stoichitoiu, L.E.; Ionescu, R.A.; Balea, M.I.; Cernat, R.C.; Vlad, N.; Padureanu, V.; Purcarea, A.; et al. Antibiotic Prescription and In-Hospital Mortality in COVID-19: A Prospective Multicentre Cohort Study. J. Pers. Med. 2022, 12, 0877. [Google Scholar] [CrossRef]
| Name of Clinical Trial | Year | Participants | Clinical Outcome | Type of Study |
|---|---|---|---|---|
| Furtado et al., 2020 (COALITION II)[87] | 2020 | 447 | No justification for the use of azithromycin for better clinical outcomes. | Open label |
| Butler et al., 2021 (PRINCIPLE)[88] | 2021 | 292 | No justification for the use of azithromycin for reducing time to recovery or risk of hospitalization. | Open label |
| Hinks et al., 2021 (ATOMIC 2)[89] | 2021 | 263 | No justification for the use of azithromycin for reducing the risk of hospitalization or death. | Open label |
| Horby et al., 2021 (RECOVERY) [90] | 2021 | 2265 | No justification for the use of azithromycin on inpatients for increase in survival. | Open label |
| Oldenburg et al., 2021 [11] | 2021 | 7763 | No justification for the use of azithromycin versus placebo for elimination of symptoms at day 14. | Blind |
| Gyselinck et al., 2022 (DAWn-AZITHRO) [70] | 2022 | 160 | Early trial termination, failed to demonstrate a benefit of azithromycin. | Open label |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kournoutou, G.G.; Dinos, G. Azithromycin through the Lens of the COVID-19 Treatment. Antibiotics 2022, 11, 1063. https://doi.org/10.3390/antibiotics11081063
Kournoutou GG, Dinos G. Azithromycin through the Lens of the COVID-19 Treatment. Antibiotics. 2022; 11(8):1063. https://doi.org/10.3390/antibiotics11081063
Chicago/Turabian StyleKournoutou, Georgia G., and George Dinos. 2022. "Azithromycin through the Lens of the COVID-19 Treatment" Antibiotics 11, no. 8: 1063. https://doi.org/10.3390/antibiotics11081063
APA StyleKournoutou, G. G., & Dinos, G. (2022). Azithromycin through the Lens of the COVID-19 Treatment. Antibiotics, 11(8), 1063. https://doi.org/10.3390/antibiotics11081063






