Qualitative Study on Antimicrobial Usage and Resistance in the Dairy Chain: A Situation Analysis and Solutions by Stakeholders from Punjab, India
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Approval
2.2. Study Participants
2.3. Data Analysis
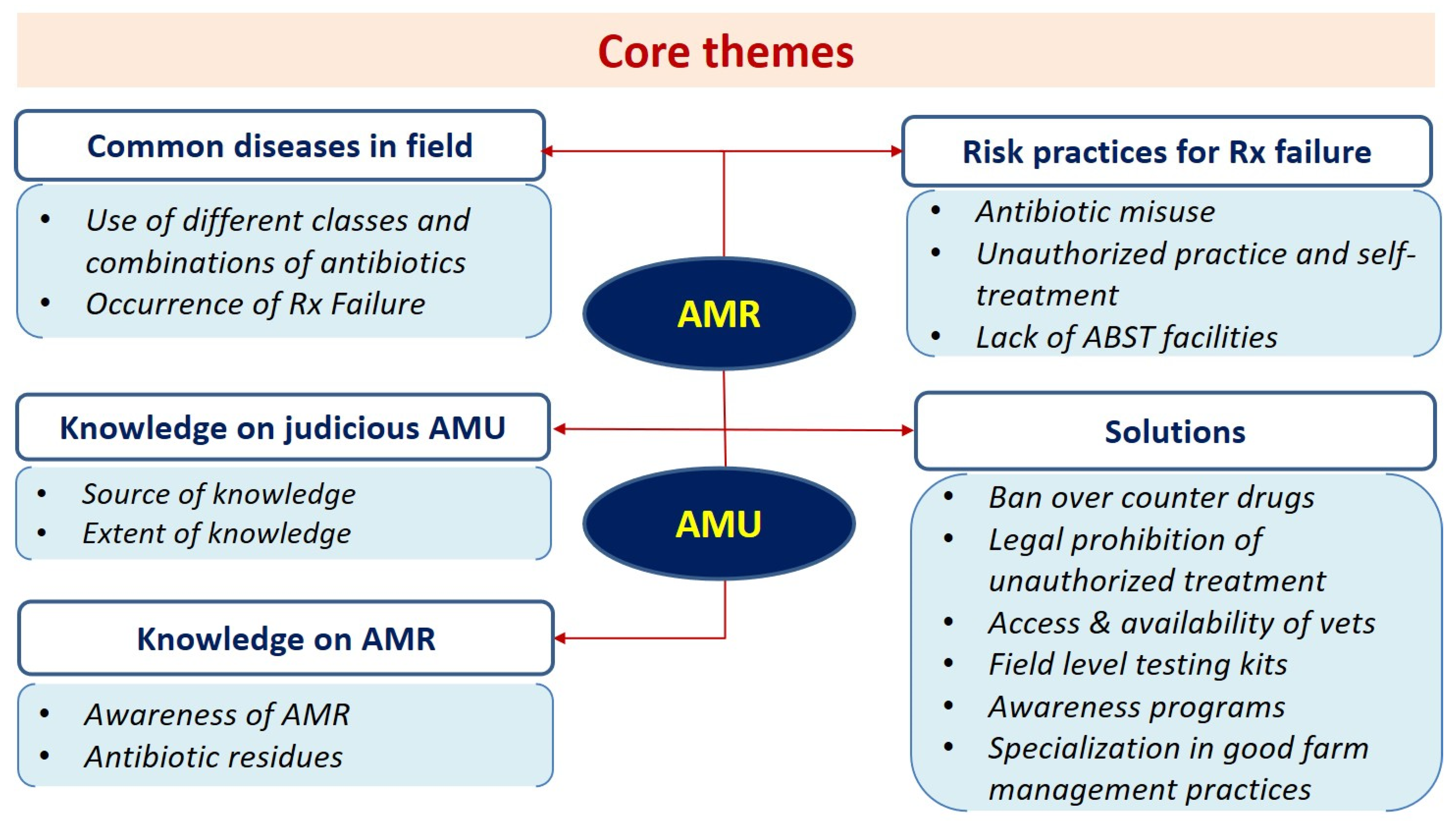
3. Results
- Theme 1: Common Disease Conditions in the Field and their Therapy
- Subtheme 1.1: Use of Different Classes of Antibiotics and Antibiotic Combinations
- Subtheme 1.2. Frequent Treatment Failure in the Field
- Theme 2: Risk Practices for Treatment Failure in the Field
- Subtheme 2.1. Antibiotic Misuse in the Field
- Subtheme 2.1.1: Incomplete Treatment Duration
- Subtheme 2.1.2. Availability of Antibiotics without Prescription
- Subtheme 2.2: Unauthorized Practitioners (i.e., Quackery) and Self-Treatment by Farmers
- Subtheme 2.2.1. Lack of Availability of Veterinarians
- Subtheme 2.2.2. Influence of Pharmaceutical Companies
- Subtheme 2.3: Lack of Antibiotic Susceptibility Testing
- Subtheme 2.3.1. Lack of Available Facilities
- Subtheme 2.3.2. Extra Burden on Farmers
- Subtheme 2.3.3. Need for Rapid and Accessible Testing Facilities
- Theme 3: Knowledge of Judicious Antibiotic Usage
- Subtheme 3.1. Source of Knowledge on Antibiotic Usage
- Subtheme 3.1.1. Influence of Social Media
- Subtheme 3.2. Extent of Knowledge on Antibiotic Usage
- Theme 4. Knowledge on Antimicrobial Resistance (AMR)
- Subtheme 4.1. Awareness of AMR
- Subtheme 4.2. Antibiotic Residues
- Subtheme 4.2.1. Withdrawal Period
- Subtheme 4.2.2. Antibiotic Residue Testing Scenario
- Theme 5: Solutions for Curbing the Problem
- Subtheme 5.1. Stopping over the Counter Availability of Drugs
- Subtheme 5.2. Legal Prohibition of Unauthorized Treatment or Quackery
- Subtheme 5.3. Access and Availability of Veterinarians
- Subtheme 5.4. Need for Field-Level Testing Kits
- Subtheme 5.4.1. Provision of Compensation to Farmers who Adhere to the Withdrawal Period
- Subtheme 5.5. Need for Widespread Awareness Programs
- Subtheme 5.5.1. Need for Continuing Veterinary Education Programs
- Subtheme 5.6. Specialization in Good Farm Management Practices
4. Discussion
5. Limitations of the Study
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chaudhry, D.; Tomar, P. Antimicrobial resistance: The next BIG pandemic. Int. J. Community Med. Public Health 2017, 4, 2632–2636. [Google Scholar] [CrossRef]
- Van Boeckel, T.P.; Brower, C.; Gilbert, M.; Grenfell, B.T.; Levin, S.A.; Robinson, T.P.; Teillant, A.; Laxminarayan, R. Global trends in antimicrobial use in food animals. Proc. Natl. Acad. Sci. USA 2015, 112, 5649–5654. [Google Scholar] [CrossRef]
- Scott, A.M.; Beller, E.; Glasziou, P.; Clark, J.; Ranakusuma, R.W.; Byambasuren, O.; Bakhit, M.; Page, S.W.; Trott, D.; Del Mar, C. Is antimicrobial administration to food animals a direct threat to human health? A rapid systematic review. Int. J. Antimicrob. Agents 2018, 52, 316–323. [Google Scholar] [CrossRef]
- Ma, F.; Xu, S.; Tang, Z.; Li, Z.; Zhang, L. Use of antimicrobials in food animals and impact of transmission of antimicrobial resistance on humans. Biosaf. Health 2021, 3, 32–38. [Google Scholar] [CrossRef]
- Hinchliffe, S.; Butcher, A.; Rahman, M.M. The AMR problem: Demanding economies, biological margins, and co-producing alternative strategies. Palgrave Commun. 2018, 4, 1–2. [Google Scholar] [CrossRef]
- Tiseo, K.; Huber, L.; Gilbert, M.; Robinson, T.P.; Van Boeckel, T.P. Global trends in antimicrobial use in food animals from 2017 to 2030. Antibiotics 2020, 9, 918. [Google Scholar] [CrossRef] [PubMed]
- Ayukekbong, J.A.; Ntemgwa, M.; Atabe, A.N. The threat of antimicrobial resistance in developing countries: Causes and control strategies. Antimicrob. Resist. Infect. Control 2017, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.; Singh, B.B.; Tiwari, H.K.; Josan, H.S.; Jaswal, N.; Kaur, M.; Kostoulas, P.; Khatkar, M.S.; Aulakh, R.S.; Gill, J.P.; et al. Using Dairy Value Chains to Identify Production Constraints and Biosecurity Risks. Animals 2020, 10, 2332. [Google Scholar] [CrossRef]
- Walia, K.; Sharma, M.; Vijay, S.; Shome, B.R. Understanding policy dilemmas around antibiotic use in food animals & offering potential solutions. Indian J. Med. Res. 2019, 149, 107. [Google Scholar] [PubMed]
- Nyumba, T.O.; Wilson, K.; Derrick, C.J.; Mukherjee, N. The use of focus group discussion methodology: Insights from two decades of application in conservation. Methods Ecol. Evol. 2018, 9, 20–32. [Google Scholar] [CrossRef] [Green Version]
- Cornwall, A.; Jewkes, R. What is participatory research? Soc. Sci. Med. 1995, 41, 1667–1676. [Google Scholar] [CrossRef]
- Sutton, J.; Austin, Z. Qualitative research: Data collection, analysis, and management. Can. J. Hosp. Pharm. 2015, 68, 226. [Google Scholar] [CrossRef] [PubMed]
- Stalmeijer, R.E.; McNaughton, N.; Van Mook, W.N. Using focus groups in medical education research: AMEE Guide No. 91. Med. Teach. 2014, 36, 923–939. [Google Scholar] [CrossRef]
- Thomas, L.; MacMillan, J.; McColl, E.; Hale, C.; Bond, S. Comparison of focus group and individual interview methodology in examining patient satisfaction with nursing care. Soc. Sci. Health 1995, 1, 206–220. [Google Scholar]
- Ivanoff, S.D.; Hultberg, J. Understanding the multiple realities of everyday life: Basic assumptions in focus-group methodology. Scand. J. Occup. Ther. 2006, 13, 125–132. [Google Scholar] [CrossRef]
- Bradbury-Jones, C.; Sambrook, S.; Irvine, F. The phenomenological focus group: An oxymoron? J. Adv. Nurs. 2009, 65, 663–671. [Google Scholar] [CrossRef]
- Vijay, D. Study on Antimicrobial Usage, Resistance and Residues in Dairy Herds of Punjab Using a ‘One-Health’ Approach. Ph.D. Thesis, Guru Angad Dev Veterinary and Animal Sciences University, Ludhiana, India, 2022. [Google Scholar]
- Vijay, D.; Bedi, J.S.; Dhaka, P.; Singh, R.; Singh, J.; Arora, A.K.; Gill, J.P. Knowledge, Attitude, and Practices (KAP) Survey among Veterinarians, and Risk Factors Relating to Antimicrobial Use and Treatment Failure in Dairy Herds of India. Antibiotics 2021, 10, 216. [Google Scholar] [CrossRef]
- Gautham, M.; Spicer, N.; Chatterjee, S.; Goodman, C. What are the challenges for antibiotic stewardship at the community level? An analysis of the drivers of antibiotic provision by informal healthcare providers in rural India. Soc. Sci. Med. 2021, 275, 113813. [Google Scholar] [CrossRef] [PubMed]
- Mutua, F.; Sharma, G.; Grace, D.; Bandyopadhyay, S.; Shome, B.; Lindahl, J. A review of animal health and drug use practices in India, and their possible link to antimicrobial resistance. Antimicrob. Resist. Infect. Control 2020, 9, 1–3. [Google Scholar] [CrossRef]
- Garcia, S.N.; Osburn, B.I.; Cullor, J.S. A one health perspective on dairy production and dairy food safety. One Health 2019, 7, 100086. [Google Scholar] [CrossRef]
- U.N. Interagency Coordination Group on Antimicrobial Resistance. No Time to Wait: Securing the Future from Drug-Resistant Infections; Report to the Secretary-General of the United Nations; World Health Organization: Geneva, Switzerland, 2019; pp. 1–36. [Google Scholar]
- Mangesho, P.E.; Caudell, M.A.; Mwakapeje, E.R.; Ole-Neselle, M.; Kabali, E.; Obonyo, M.; Dorado-Garcia, A.; Valcarce, A.; Kimani, T.; Price, C.; et al. “We are doctors”: Drivers of animal health practices among Maasai pastoralists and implications for antimicrobial use and antimicrobial resistance. Prev. Vet. Med. 2021, 188, 105266. [Google Scholar] [CrossRef] [PubMed]
- Bahta, M.; Debesai, M.; Bahta, I.; Kessete, A.; Afendi, A.; Fitsum, Y.; Nambozi, J.; NKidane, S.; HTesfamariam, E. Knowledge, attitude and practice of antibiotics and their determinants in Eritrea. BMJ Open 2021, 11, e046432. [Google Scholar]
- Sakeena, M.H.; Bennett, A.A.; McLachlan, A.J. Enhancing pharmacists’ role in developing countries to overcome the challenge of antimicrobial resistance: A narrative review. Antimicrob. Resist. Infect. Control 2018, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm. Policy Ment. Health Ment. Health Serv. Res. 2015, 42, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 1, 77–101. [Google Scholar] [CrossRef]
- Charmaz, K. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis; SAGE Publication: New York, NY, USA, 2006. [Google Scholar]
- World Health Organization. Global Action Plan on Antimicrobial Resistance [Internet]; World Health Organization: Geneva, Switzerland, 2015; Available online: https://www.who.int/antimicrobial-resistance/global-action-plan/en/ (accessed on 12 October 2021).
- Verma, H.; Rawat, S.; Sharma, N.; Jaiswal, V.; Singh, R.; Harshit, V. Prevalence, bacterial etiology and antibiotic susceptibility pattern of bovine mastitis in Meerut. J. Entomol. Zool. Stud. 2018, 6, 706–709. [Google Scholar]
- Dutta, T.K.; Kumar, V.S.; Kotwal, S.K. Prevalence and antibiotic resistance pattern of bacteria from clinical and subclinical cases of bovine mastitis in Jammu region. Indian J. Anim. Sci. 2007, 77, 427–429. [Google Scholar]
- Kumar, R.; Yadav, B.R.; Singh, R.S. Antibiotic resistance and pathogenicity factors in Staphylococcus aureus isolated from mastitic Sahiwal cattle. J. Biosci. 2011, 36, 175–188. [Google Scholar] [CrossRef]
- Kumar, V.; Das, S.C.; Guin, S.; Malik, S.V. Virulence, enterotoxigenicity and antibiotic profile of Staphylococcus aureus from buffalo clinical mastitis. Indian J. Anim. Sci. 2012, 82, 48–51. [Google Scholar]
- Kumar, V.; Meena, H.R.; Kadian, K.S.; Sankhala, G.; Mohanty, T.K.; Lathwal, S.S.; Kar, P. Comparative Analysis of Minor-veterinary Services Rendered by Paraveterinariansin Four Different States of India: Stakeholders’ Perspective. J. Community Mobilization Sustain. Dev. 2021, 16, 319–329. [Google Scholar]
- World Health Organization. WHO List of Critically Important Antimicrobials. 2019. Available online: https://www.who.int/foodsafety/areas_work/antimicrobial-resistance/cia/en (accessed on 20 April 2021).
- CDDEP. Antibiotic Use and Resistance in Food Animals. Current Policy and Recommendations; Center for Disease Dynamics Economics and Policy: Washington, DC, USA, 2016. [Google Scholar]
- Yusuf, H.; Rukkwamsuk, T.; Idris, S.; Paul, M. Antimicrobial usage surveillance of cattle in Indonesia to address antimicrobial resistance. In Proceedings of the Advances in Social Science, Education and Humanities Research (ASSEHR); Atlantis Press: Amsterdam, The Netherlands, 2017; Volume 98, pp. 355–359. [Google Scholar]
- Wangmo, K.; Dorji, T.; Pokhrel, N.; Dorji, T.; Dorji, J.; Tenzin, T. Knowledge, attitude, and practice on antibiotic use and antibiotic resistance among the veterinarians and para-veterinarians in Bhutan. PLoS ONE 2021, 16, e0251327. [Google Scholar] [CrossRef]
- Cobo Angel, C.; LeBlanc, S.J.; Roche, S.M.; Ritter, C. A focus group study of Canadian dairy farmers’ attitudes and social referents on antimicrobial use and antimicrobial resistance. Front. Vet. Sci. 2021, 8, 639. [Google Scholar] [CrossRef] [PubMed]
- Roderick, S.; Stevenson, P.; Mwendia, C.; Okech, G. The use of trypanocides and antibiotics by Maasai pastoralists. Trop. Anim. Health Prod. 2000, 32, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Caudell, M.A.; Quinlan, M.B.; Subbiah, M.; Call, D.R.; Roulette, C.J.; Roulette, J.W.; Roth, A.; Matthews, L.; Quinlan, R.J. Antimicrobial use and veterinary care among agro-pastoralists in Northern Tanzania. PLoS ONE 2017, 26, e0170328. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Mutua, F.; Deka, R.P.; Shome, R.; Bandyopadhyay, S.; Shome, B.R.; Goyal Kumar, N.; Grace, D.; Dey, T.K.; Venugopal, N.; et al. A qualitative study on antibiotic use and animal health management in smallholder dairy farms of four regions of India. Infect. Ecol. Epidemiol. 2020, 10, 1792033. [Google Scholar] [CrossRef]
- Patnaik, N.M.; Gupta, J.; Acharya, P.; Kar, P. Use of Antimicrobials for Treatment of Dairy Animals by Veterinarian and Paravet in Punjab: A Study on Prescription Pattern. Indian J. Ext. Educ. 2019, 55, 86–91. [Google Scholar]
- Dinki, N.; Balcha, E. Detection of antibiotic residues and determination of microbial quality of raw milk from milk collection centres. Adv. Anim. Vet. Sci. 2013, 1, 80–83. [Google Scholar]
- Chauhan, A.S.; George, M.S.; Chatterjee, P.; Lindahl, J.; Grace, D.; Kakkar, M. The social biography of antibiotic use in smallholder dairy farms in India. Antimicrob. Resist. Infect. Control 2018, 7, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Report of the Working Group on Animal Husbandry & Dairying 12th Five Year Plan (2012–2017); Submitted to Planning Commission; Government of India: New Delhi, India. Available online: https://niti.gov.in/planningcommission.gov.in/docs/aboutus/committee/wrkgrp12/agri/AHD_REPORT_Final_rev.pdf (accessed on 12 October 2021).
- Caudell, M.A.; Dorado-Garcia, A.; Eckford, S.; Creese, C.; Byarugaba, D.K.; Afakye, K.; Chansa-Kabali, T.; Fasina, F.O.; Kabali, E.; Kiambi, S.; et al. Towards a bottom-up understanding of antimicrobial use and resistance on the farm: A knowledge, attitudes, and practices survey across livestock systems in five African countries. PLoS ONE 2020, 24, e0220274. [Google Scholar] [CrossRef]
- Kimera, Z.I.; Frumence, G.; Mboera, L.E.; Rweyemamu, M.; Mshana, S.E.; Matee, M.I. Assessment of drivers of antimicrobial use and resistance in poultry and domestic pig farming in the Msimbazi river basin in Tanzania. Antibiotics 2020, 9, 838. [Google Scholar] [CrossRef]
- Singh, B. Who is responsible for emergence and spread of AMR? How to handle it? In Proceedings of the 17th convocation of National Academy of Veterinary Sciences (India) and Scientific Seminar on Livestock Sector towards One Health, Food Security and Safety, Bhubaneswar, India, 19–20 December 2018; Available online: https://www.researchgate.net/publication/329828053_Who_is_responsible_for_Emergence_and_spread_of_AMR_How_to_handle_it (accessed on 24 June 2020).
- Ranjalkar, J.; Chandy, S.J. India’s National Action Plan for antimicrobial resistance—An overview of the context, status, and way ahead. J. Fam. Med. Prim. Care 2019, 8, 1828. [Google Scholar] [CrossRef] [PubMed]
- Green, J.; Nicki, T. Qualitative Methods for Health Research, 4th ed.; SAGE Publications Ltd.: London, UK, 2018. [Google Scholar]
| Variable | Categories | Veterinarians (n = 56) | Para-Veterinarians (n = 28) | Chemists (n = 18) | Dairy Quality Managers (n = 12) | Total (%) (N = 114) |
|---|---|---|---|---|---|---|
| Sex | Male | 39 | 28 | 16 | 12 | 95 (83.3) |
| Female | 17 | 0 | 02 | 0 | 19 (16.7) | |
| Age | 20–30 | 12 | 8 | 7 | 0 | 27 (23.7) |
| 31–40 | 29 | 7 | 3 | 5 | 44 (38.6) | |
| 41–60 | 15 | 13 | 8 | 7 | 43 (37.7) | |
| >60 | 0 | 0 | 0 | 0 | 0 | |
| Area | Rural | 48 | 16 | 12 | 10 | 86 (75.4) |
| Urban | 3 | 0 | 6 | 2 | 11 (9.6) | |
| Both | 5 | 12 | 0 | 0 | 17 (14.9) | |
| Education | 10th | 0 | 0 | 0 | 0 | 0 |
| 11–12th | 0 | 0 | 4 | 0 | 4 (3.5) | |
| Diploma | 0 | 28 | 14 | 0 | 42 (36.8) | |
| Bachelor’s degree | 35 | 0 | 0 | 12 | 47 (41.2) | |
| Master’s degree | 21 | 0 | 0 | 0 | 21 (18.4) | |
| PhD degree | 0 | 0 | 0 | 0 | 0 | |
| Main occupation | Government | 56 | 28 | 0 | 12 | 96 (84.2) |
| Private | 0 | 0 | 18 | 0 | 18 (15.8) | |
| Experience | 2–10 | 12 | 9 | 6 | 7 | 34 (29.8) |
| 11–20 | 31 | 16 | 10 | 5 | 62 (54.4) | |
| 21–30 | 11 | 2 | 2 | 0 | 15 (13.2) | |
| >30 | 2 | 1 | 0 | 0 | 3 (2.6) |
| Themes | Subthemes | |||
|---|---|---|---|---|
| Veterinarians | Para-Veterinarians | Chemists | Dairy Quality Managers | |
| Common disease conditions and their therapy |
|
|
| |
| Risk factors for treatment failure in the field |
|
|
|
|
| Knowledge of judicious antibiotic usage |
|
|
| |
| Knowledge on antimicrobial resistance |
|
|
|
|
| Solutions for curbing the problem |
|
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vijay, D.; Bedi, J.S.; Dhaka, P.; Singh, R.; Singh, J.; Arora, A.K.; Gill, J.P.S. Qualitative Study on Antimicrobial Usage and Resistance in the Dairy Chain: A Situation Analysis and Solutions by Stakeholders from Punjab, India. Antibiotics 2022, 11, 1229. https://doi.org/10.3390/antibiotics11091229
Vijay D, Bedi JS, Dhaka P, Singh R, Singh J, Arora AK, Gill JPS. Qualitative Study on Antimicrobial Usage and Resistance in the Dairy Chain: A Situation Analysis and Solutions by Stakeholders from Punjab, India. Antibiotics. 2022; 11(9):1229. https://doi.org/10.3390/antibiotics11091229
Chicago/Turabian StyleVijay, Deepthi, Jasbir Singh Bedi, Pankaj Dhaka, Randhir Singh, Jaswinder Singh, Anil Kumar Arora, and Jatinder Paul Singh Gill. 2022. "Qualitative Study on Antimicrobial Usage and Resistance in the Dairy Chain: A Situation Analysis and Solutions by Stakeholders from Punjab, India" Antibiotics 11, no. 9: 1229. https://doi.org/10.3390/antibiotics11091229
APA StyleVijay, D., Bedi, J. S., Dhaka, P., Singh, R., Singh, J., Arora, A. K., & Gill, J. P. S. (2022). Qualitative Study on Antimicrobial Usage and Resistance in the Dairy Chain: A Situation Analysis and Solutions by Stakeholders from Punjab, India. Antibiotics, 11(9), 1229. https://doi.org/10.3390/antibiotics11091229







