Healthcare System Distrust and Non-Prescription Antibiotic Use: A Cross-Sectional Survey of Adult Antibiotic Users
Abstract
:1. Introduction
2. Results
2.1. Primary Analysis
2.1.1. Descriptive Statistics
2.1.2. Unadjusted Model
2.1.3. Fully Adjusted Model
2.1.4. Partially Adjusted Model
2.2. Sensitivity Analyses
2.2.1. Sensitivity Analysis I
2.2.2. Sensitivity Analysis II + III
3. Discussion
4. Materials and Methods
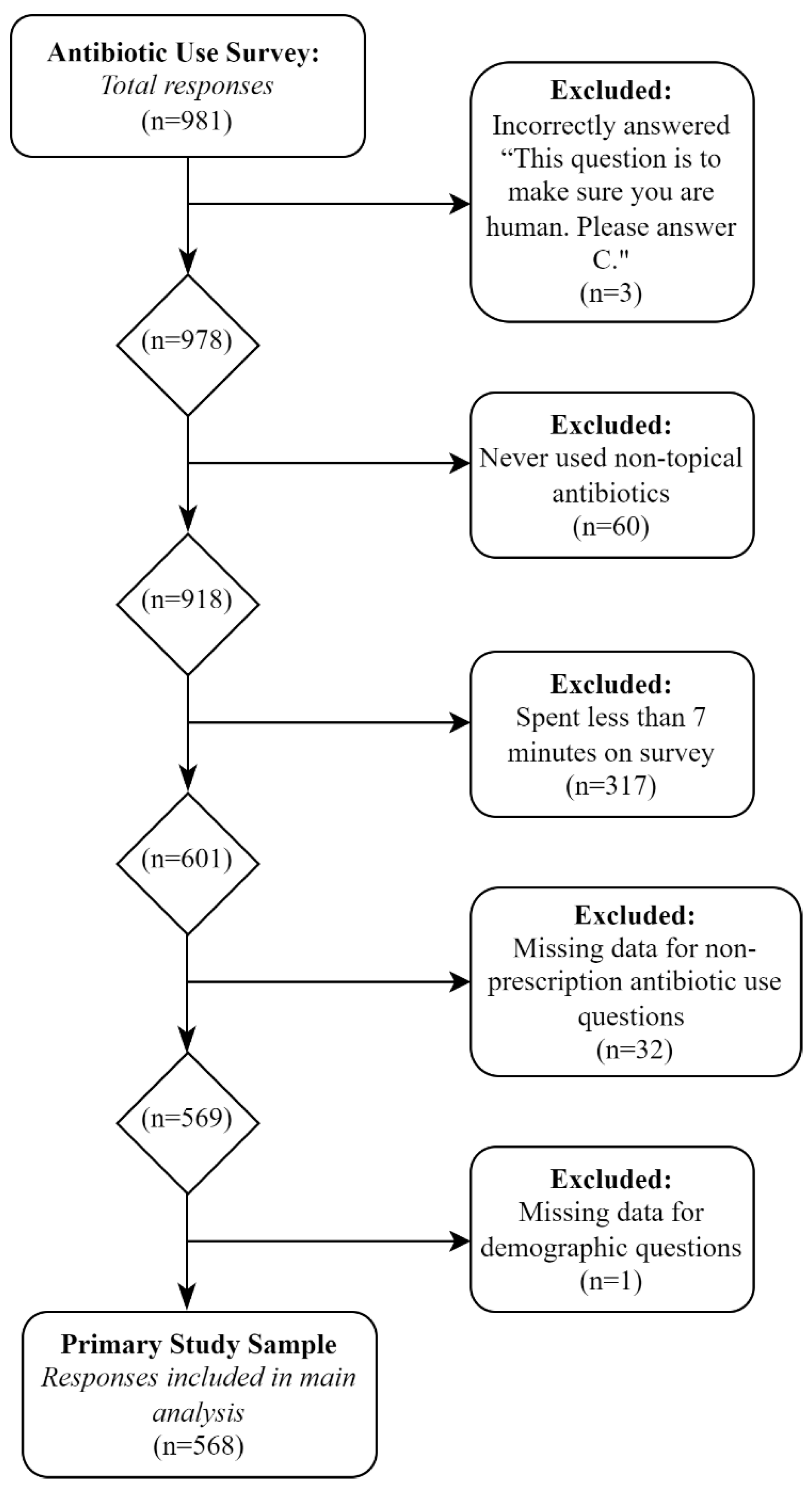
4.1. Study Design and Recruitment
4.2. Study Sample
4.3. Variables of Interest
4.4. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alós, J.-I. Antibiotic resistance: A global crisis. Enferm. Infect. Microbiol. Clin. 2015, 33, 692–699. [Google Scholar] [CrossRef]
- Martinez, J.L. General Principles of Antibiotic Resistance in Bacteria. Drug. Discov. Today Technol. 2014, 11, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Munita, J.M.; Arias, C.A. Mechanisms of Antibiotic Resistance. Microbiol. Spectr. 2016, 4, 1–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morehead, M.S.; Scarbrough, C. Emergence of Global Antibiotic Resistance. Prim. Care 2018, 45, 467–484. [Google Scholar] [CrossRef]
- Watkins, R.R.; Bonomo, R.A. Overview: Global and Local Impact of Antibiotic Resistance. Infect. Dis. Clin. N. Am. 2016, 30, 313–322. [Google Scholar] [CrossRef]
- Rehman, M.; Ahmed, S.; Ahmed, U.; Tamanna, K.; Sabir, M.S.; Niaz, Z. An Overview of Self-Medication: A Major Cause of Antibiotic Resistance and a Threat to Global Public Health. J. Pak. Med. Assoc. 2021, 71, 943–949. [Google Scholar] [CrossRef]
- de Kraker, M.E.A.; Stewardson, A.J.; Harbarth, S. Will 10 Million People Die a Year Due to Antimicrobial Resistance by 2050? PLoS Med. 2016, 13, e1002184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC. The Biggest Antibiotic-Resistant Threats in the U.S. Available online: https://www.cdc.gov/drugresistance/biggest-threats.html (accessed on 24 March 2022).
- Garza-González, E.; Franco-Cendejas, R.; Morfín-Otero, R.; Echaniz-Aviles, G.; Rojas-Larios, F.; Bocanegra-Ibarias, P.; Flores-Treviño, S.; Ponce-de-León, A.; Rodríguez-Noriega, E.; Alavez-Ramírez, N.; et al. The Evolution of Antimicrobial Resistance in Mexico During the Last Decade: Results from the INVIFAR Group. Microb. Drug Resist. 2020, 26, 1372–1382. [Google Scholar] [CrossRef]
- Amabile-Cuevas, C.F. Antibiotic Usage and Resistance in Mexico: An Update after a Decade of Change. J. Infect. Dev. Ctries. 2021, 15, 442–449. [Google Scholar] [CrossRef]
- Pickens, C.I.; Wunderink, R.G. Principles and Practice of Antibiotic Stewardship in the ICU. Chest 2019, 156, 163–171. [Google Scholar] [CrossRef]
- CDC. Be Antibiotics Aware Toolkit. Available online: https://www.cdc.gov/antibiotic-use/week/toolkit/graphics.html (accessed on 20 March 2022).
- Thom, K.; Tamma, P.D.; Harris, A.D.; Morgan, D.; Dzintars, K.; Srinivasan, A.; Avdic, E.; Li, D.X.; Pineles, L.; Cosgrove, S.E. Prevent Antibiotic OverUSE (PAUSE): Impact of a Provider Driven Antibiotic-Time out on Antibiotic Use and Prescribing. Open Forum. Infect. Dis. 2017, 4, S20. [Google Scholar] [CrossRef] [Green Version]
- Dreser, A.; Vázquez-Vélez, E.; Treviño, S.; Wirtz, V.J. Regulation of Antibiotic Sales in Mexico: An Analysis of Printed Media Coverage and Stakeholder Participation. BMC Public Health 2012, 12, 1051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antibiotic Use|CDC. Available online: https://www.cdc.gov/antibiotic-use/index.html (accessed on 12 December 2022).
- Slaughter, L.M. Text—H.R.1587—115th Congress (2017–2018): Preservation of Antibiotics for Medical Treatment Act of 2017. Available online: https://www.congress.gov/bill/115th-congress/house-bill/1587/text (accessed on 26 March 2022).
- Gordon, S.M.; Mosure, D.J.; Lewis, J.; Brown, S.; McNagny, S.E.; Schmid, G.P. Prevalence of Self-Medication with Antibiotics among Patients Attending a Clinic for Treatment of Sexually Transmitted Diseases. Clin. Infect. Dis. 1993, 17, 462–465. [Google Scholar] [CrossRef] [PubMed]
- Mainous, A.G.; Diaz, V.A.; Carnemolla, M. Factors Affecting Latino Adults’ Use of Antibiotics for Self-Medication. J. Am. Board Fam. Med. 2008, 21, 128–134. [Google Scholar] [CrossRef] [Green Version]
- Mainous, A.G.; Cheng, A.Y.; Garr, R.C.; Tilley, B.C.; Everett, C.J.; McKee, M.D. Nonprescribed Antimicrobial Drugs in Latino Community, South Carolina. Emerg. Infect. Dis. 2005, 11, 883–888. [Google Scholar] [CrossRef]
- Morgan, D.J.; Okeke, I.N.; Laxminarayan, R.; Perencevich, E.N.; Weisenberg, S. Non-Prescription Antimicrobial Use Worldwide: A Systematic Review. Lancet Infect. Dis. 2011, 11, 692–701. [Google Scholar] [CrossRef] [Green Version]
- Zoorob, R.; Grigoryan, L.; Nash, S.; Trautner, B.W. Nonprescription Antimicrobial Use in a Primary Care Population in the United States. Antimicrob. Agents Chemother. 2016, 60, 5527–5532. [Google Scholar] [CrossRef] [Green Version]
- Jaiswal, J.; Halkitis, P.N. Towards a More Inclusive and Dynamic Understanding of Medical Mistrust Informed by Science. Behav. Med. 2019, 45, 79–85. [Google Scholar] [CrossRef]
- Kimball, D.; Rivera, D.; Gonzales, M.; Blashill, A.J. Medical Mistrust and the PrEP Cascade Among Latino Sexual Minority Men. AIDS Behav. 2020, 24, 3456–3461. [Google Scholar] [CrossRef]
- Ash, M.J.; Berkley-Patton, J.; Christensen, K.; Haardörfer, R.; Livingston, M.D.; Miller, T.; Woods-Jaeger, B. Predictors of Medical Mistrust among Urban Youth of Color during the COVID-19 Pandemic. Transl. Behav. Med. 2021, 11, 1626–1634. [Google Scholar] [CrossRef]
- LaVeist, T.A.; Isaac, L.A.; Williams, K.P. Mistrust of Health Care Organizations Is Associated with Underutilization of Health Services. Health Serv. Res. 2009, 44, 2093–2105. [Google Scholar] [CrossRef] [PubMed]
- Arnett, M.J.; Thorpe, R.J.; Gaskin, D.J.; Bowie, J.V.; LaVeist, T.A. Race, Medical Mistrust, and Segregation in Primary Care as Usual Source of Care: Findings from the Exploring Health Disparities in Integrated Communities Study. J. Urban Health 2016, 93, 456–467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolar, S.K.; Wheldon, C.; Hernandez, N.D.; Young, L.; Romero-Daza, N.; Daley, E.M. Human Papillomavirus Vaccine Knowledge and Attitudes, Preventative Health Behaviors, and Medical Mistrust Among a Racially and Ethnically Diverse Sample of College Women. J. Racial. Ethn. Health Disparities 2015, 2, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Pellowski, J.A.; Price, D.M.; Allen, A.M.; Eaton, L.A.; Kalichman, S.C. The Differences between Medical Trust and Mistrust and Their Respective Influences on Medication Beliefs and ART Adherence among African Americans Living with HIV. Psychol. Health 2017, 32, 1127–1139. [Google Scholar] [CrossRef]
- Scharff, D.P.; Mathews, K.J.; Jackson, P.; Hoffsuemmer, J.; Martin, E.; Edwards, D. More than Tuskegee: Understanding Mistrust about Research Participation. J. Health Care Poor Underserved 2010, 21, 879–897. [Google Scholar] [CrossRef] [Green Version]
- George, S.; Duran, N.; Norris, K. A Systematic Review of Barriers and Facilitators to Minority Research Participation Among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am. J. Public Health 2014, 104, e16–e31. [Google Scholar] [CrossRef]
- Bertoldi, A.D.; Camargo, A.L.; Silveira, M.P.T.; Menezes, A.M.B.; Assunção, M.C.F.; Gonçalves, H.; Hallal, P.C. Self-Medication Among Adolescents Aged 18 Years: The 1993 Pelotas (Brazil) Birth Cohort Study. J. Adolesc. Health 2014, 55, 175–181. [Google Scholar] [CrossRef] [Green Version]
- Banda, O.; Vlahakis, P.A.; Daka, V.; Matafwali, S.K. Self-Medication among Medical Students at the Copperbelt University, Zambia: A Cross-Sectional Study. Saudi. Pharm. J. 2021, 29, 1233–1237. [Google Scholar] [CrossRef]
- Dean, L.T.; Moss, S.L.; McCarthy, A.M.; Armstrong, K. Healthcare System Distrust, Physician Trust, and Patient Discordance with Adjuvant Breast Cancer Treatment Recommendations. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1745–1752. [Google Scholar] [CrossRef] [Green Version]
- Schröder, W.; Sommer, H.; Gladstone, B.P.; Foschi, F.; Hellman, J.; Evengard, B.; Tacconelli, E. Gender Differences in Antibiotic Prescribing in the Community: A Systematic Review and Meta-Analysis. J. Antimicrob. Chemother. 2016, 71, 1800–1806. [Google Scholar] [CrossRef]
- Wallin Lundell, I.; Eulau, L.; Bjarneby, F.; Westerbotn, M. Women’s Experiences with Healthcare Professionals after Suffering from Gender-Based Violence: An Interview Study. J. Clin. Nurs. 2018, 27, 949–957. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Multicenter Study on Self-Medication and Self-Prescription in Six Latin American Countries. Drug Utilization Research Group, Latin America. Clin. Pharm. 1997, 61, 488–493. [CrossRef]
- Matuz, M.; Benko, R.; Doro, P.; Hajdu, E.; Soos, G. Non-Prescription Antibiotic Use in Hungary. Pharm. World Sci. 2007, 29, 695–698. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Tang, X.; Yan, R.; Shao, Z.; Zhou, Y.; Deng, X.; Luo, S.; He, H. Non-Prescription Antibiotic Use for Cough among Chinese Children under 5 Years of Age: A Community-Based Cross-Sectional Study. BMJ Open 2021, 11, e051372. [Google Scholar] [CrossRef]
- Ayana, H.; Sileshi, T.; Bule, M.H.; Chaka, E.E. Non-Prescription Antibiotics Use and Associated Factors Among Drug Retail Outlets in Ambo, Ethiopia: A Cross-Sectional Study. Patient Prefer. Adherence 2021, 15, 2739–2747. [Google Scholar] [CrossRef]
- Luo, Y.; Tang, X.; Ding, L.; Shao, Z.; Yu, J.; Chen, Y.; Zhou, Y.; He, H.; Chen, Z. Non-Prescriptionxx Antibiotic Use for People Aged 15 Years or Older for Cough in China: A Community-Based Survey. Antimicrob. Resist. Infect. Control 2021, 10, 129. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.; Lv, B.; Zhu, S.; Yu, J.; Zhang, Y.; Ye, D.; Aziz, M.M.; Yang, C.; Fang, Y. Non-Prescription Use of Antibiotics among Children in Urban China: A Cross-Sectional Survey of Knowledge, Attitudes, and Practices. Expert Rev. Anti. Infect. 2018, 16, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Xuan, Z.; Storella, T.H.; Zhou, X. Determinants of Non-Prescription Antibiotic Dispensing in Chinese Community Pharmacies from Socio-Ecological and Health System Perspectives. Soc. Sci. Med. 2020, 256, 113035. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Cuevas, R.; Doubova, S.V.; Wirtz, V.J.; Servan-Mori, E.; Dreser, A.; Hernández-Ávila, M. Effects of the Expansion of Doctors’ Offices Adjacent to Private Pharmacies in Mexico: Secondary Data Analysis of a National Survey. BMJ Open 2014, 4, e004669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- What Is Amazon Mechanical Turk. Available online: https://aws.amazon.com/premiumsupport/knowledge-center/mechanical-turk-use-cases/ (accessed on 7 December 2021).
- Rose, A.; Peters, N.; Shea, J.A.; Armstrong, K. Development and Testing of the Health Care System Distrust Scale. J. Gen. Intern. Med. 2004, 19, 57–63. [Google Scholar] [CrossRef]
- Céspedes, A.; Larson, E. Knowledge, Attitudes, and Practices Regarding Antibiotic Use among Latinos in the United States: Review and Recommendations. Am. J. Infect. Control 2006, 34, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Jamhour, A.; El-Kheir, A.; Salameh, P.; Hanna, P.A.; Mansour, H. Antibiotic Knowledge and Self-Medication Practices in a Developing Country: A Cross-Sectional Study. Am. J. Infect. Control 2017, 45, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Kosiyaporn, H.; Chanvatik, S.; Issaramalai, T.; Kaewkhankhaeng, W.; Kulthanmanusorn, A.; Saengruang, N.; Witthayapipopsakul, W.; Viriyathorn, S.; Kirivan, S.; Kunpeuk, W.; et al. Surveys of Knowledge and Awareness of Antibiotic Use and Antimicrobial Resistance in General Population: A Systematic Review. PLoS ONE 2020, 15, e0227973. [Google Scholar] [CrossRef] [PubMed]
- SAS. OnDemand for Academics. Available online: https://welcome.oda.sas.com/home (accessed on 7 December 2021).

| Characteristic | Total (n = 568) | Non-Prescription Antibiotic Use (n = 276) | Prescription Antibiotic Use (n = 292) | p-Value |
|---|---|---|---|---|
| n (% a) | n (% b) | n (% b) | χ2-test | |
| Gender | 0.57 | |||
| Male | 310 (54.6) | 154 (49.7) | 156 (50.3) | |
| Female | 258 (45.4) | 122 (47.3) | 136 (52.7) | |
| Age | <0.01 | |||
| 18–24 | 28 (4.9) | 15 (53.8) | 13 (46.4) | |
| 25–34 | 229 (40.3) | 132 (57.6) | 97 (42.4) | |
| 35–44 | 189 (33.3) | 87 (46.0) | 102 (54.0) | |
| 45–54 | 66 (11.6) | 24 (36.4) | 42 (63.6) | |
| 55+ | 56 (9.9) | 18 (32.1) | 38 (67.9) | |
| Education level | <0.01 | |||
| High school diploma or less | 120 (21.1) | 44 (36.6) | 76 (63.3) | |
| High school diploma or more | 448 (78.9) | 232 (51.8) | 216 (48.2) | 0.02 |
| Income c | ||||
| Low | 51 (9.0) | 26 (51.0) | 25 (49.0) | |
| Middle | 301 (53.0) | 161 (53.5) | 140 (46.5) | |
| High | 216 (38.0) | 89 (41.2) | 127 (58.8) | |
| Political views | <0.01 | |||
| Very left wing/liberal | 55 (9.7) | 15 (27.3) | 40 (72.7) | |
| Left wing/liberal | 107 (18.8) | 51 (47.7) | 56 (52.3) | |
| Center left/slightly liberal | 52 (9.2) | 23 (44.2) | 29 (55.8) | |
| Middle of the road | 113 (19.9) | 40 (35.4) | 73 (64.6) | |
| Center right/slightly conservative | 63 (11.1) | 29 (46.0) | 34 (54.0) | |
| Right wing/conservative | 135 (23.8) | 89 (65.9) | 46 (34.1) | |
| Very right wing/conservative | 43 (7.6) | 29 (67.4) | 14 (32.6) | |
| Ethnicity | 0.15 | |||
| Hispanic/Latinx | 185 (32.6) | 98 (53.0) | 87 (47.0) | |
| Non-Hispanic/Latinx | 383 (67.4) | 178 (46.5) | 205 (53.5) | |
| Race | <0.01 | |||
| White | 399 (70.3) | 180 (45.1) | 219 (54.9) | |
| American Indian or Alaskan Native | 11 (1.9) | 6 (54.6) | 5 (45.5) | |
| Asian | 24 (4.2) | 9 (37.5) | 15 (62.5) | |
| Black or African American | 79 (13.9) | 58 (73.4) | 21 (26.6) | |
| Native Hawaiian or Pacific Islander | 6 (1.1) | 6 (100.0) | 0 (0.0) | |
| Mixed race | 20 (3.5) | 6 (30.0) | 14 (70.0) | |
| Other | 29 (5.1) | 11 (37.9) | 18 (62.1) | |
| Country of primary residence | 0.62 | |||
| United States | 475 (83.6) | 233 (49.0) | 242 (51.0) | |
| Mexico | 93 (16.4) | 43 (46.2) | 50 (53.8) | |
| Proximity to the US-Mex border | 0.82 | |||
| Zip code ≤ 100 km | 58 (10.2) | 29 (50.0) | 29 (50.0) | |
| Zip code >100 km | 510 (89.8) | 247 (48.4) | 263 (51.6) | |
| Healthcare system distrust | <0.01 | |||
| Quartile 1 (lowest scores) | 143 (25.2) | 39 (27.3) | 104 (72.7) | |
| Quartile 2 | 144 (25.4) | 55 (38.2) | 89 (61.8) | |
| Quartile 3 | 167 (29.4) | 102 (61.1) | 65 (38.9) | |
| Quartile 4 (highest scores) | 114 (20.1) | 80 (70.2) | 34 (29.8) | |
| mean (±SD) | mean (±SD) | mean (±SD) | t-test | |
| Healthcare system distrust d | 28.3 (±6.7) | 30.6 (±6.1) | 26.1 (±6.8) | <0.01 |
| Antibiotic knowledge e | 5.11 (±3.0) | 3.6 (±2.5) | 6.5 (±2.8) | <0.01 |
| Unadjusted OR (95% CI) | Fully Adjusted a OR (95% CI) | Partially Adjusted b OR (95% CI) | |
|---|---|---|---|
| Healthcare system distrust score c | |||
| Quartile 1 (lowest) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Quartile 2 | 1.65 (1.0, 2.7) | 1.33 (0.8, 2.3) | 1.34 (0.8, 2.4) |
| Quartile 3 | 4.19 (2.6, 6.8) | 2.10 (1.2, 386) | 2.36 (1.4, 4.0) |
| Quartile 4 (highest) | 6.23 (3.6, 10.8) | 3.20 (1.8, 6.1) | 3.51 (1.9, 6.5) |
| Gender | |||
| Male | - | 1.00 (ref) | - |
| Female | - | 1.09 (0.7, 1.6) | - |
| Age | |||
| 18–34 | - | 1.00 (ref) | - |
| 35+ | - | 0.72 (0.5, 1.1) | - |
| Education level | |||
| High school diploma or more | - | 1.00 (ref) | - |
| High school diploma or less | - | 0.83 (0.5, 1.4) | - |
| Income d | |||
| High | - | 1.00 (ref) | - |
| Low/middle | - | 1.45 (0.9, 2.2) | - |
| Political views | |||
| Liberal/middle of the road | - | 1.00 (ref) | 1.00 (ref) |
| Conservative | - | 1.56 (1.0, 2.4) | 1.39 (0.9, 2.1) |
| Ethnicity | |||
| Not Hispanic/Latinx or of Spanish origin | - | 1.00 (ref) | - |
| Hispanic/Latinx or of Spanish origin | - | 1.16 (0.7, 2.0) | - |
| Race | |||
| Non-black/African American | - | 1.00 (ref) | 1.00 (ref) |
| Black/African American | - | 2.34 (1.3, 4.3) | 2.48 (1.4, 4.5) |
| Country of primary residence | |||
| United States | - | 1.00 (ref) | - |
| Mexico | - | 1.40 (0.7, 2.9) | - |
| Proximity to the US-Mex border | |||
| Zip code > 100 km | - | 1.00 (ref) | - |
| Zip code ≤ 100 km | - | 1.27 (0.6, 2.6) | - |
| Antibiotic knowledge e | - | 0.75 (0.7, 0.8) | 0.75 (0.7, 0.8) |
| Primary Analysis (n = 568) Adjusted OR a (95% CI) | Sensitivity Analysis (n = 387) Adjusted OR a (95% CI) | |
|---|---|---|
| Healthcare system distrust score b | ||
| Quartile 1 (lowest) | 1.00 (ref) | 1.00 (ref) |
| Quartile 2 | 1.34 (0.8, 2.4) | 1.91 (1.0, 3.8) |
| Quartile 3 | 2.36 (1.4, 4.0) | 2.53 (1.3, 4.9) |
| Quartile 4 (highest) | 3.51 (1.9, 2.1) | 3.29 (1.5, 7.0) |
| Political views | ||
| Liberal/middle of the road | 1.00 (ref) | 1.00 (ref) |
| Conservative | 1.39 (0.9, 2.1) | 1.36 (0.8, 2.3) |
| Race | ||
| Non-black/African American | 1.00 (ref) | 1.00 (ref) |
| Black/African American | 2.48 (1.4, 4.5) | 1.66 (0.9, 3.2) |
| Antibiotic knowledge c | 0.75 (0.7, 0.8) | 0.75 (0.7, 0.8) |
| Bought Non-Prescription Antibiotics a (n = 568) Adjusted OR c (95% CI) | Borrowed Non-Prescription Antibiotics b (n = 568) Adjusted OR c (95% CI) | |
|---|---|---|
| Healthcare system distrust score d | ||
| Quartile 1 (lowest) | 1.00 (ref) | 1.00 (ref) |
| Quartile 2 | 1.23 (0.7, 2.2) | 2.56 (1.2, 5.3) |
| Quartile 3 | 1.65 (0.9, 2.9) | 3.33 (1.7, 6.7) |
| Quartile 4 (highest) | 1.97 (1.1, 3.6) | 5.95 (2.8, 12.5) |
| Political views | ||
| Liberal/middle of the road | 1.00 (ref) | 1.00 (ref) |
| Conservative | 0.92 (0.6, 1.4) | 2.20 (1.4, 3.4) |
| Race | ||
| Non-black/African American | 1.00 (ref) | 1.00 (ref) |
| Black/African American | 2.79 (1.7, 4.7) | 1.72 (1.0, 3.0) |
| Antibiotic knowledgee | 0.78 (0.7, 0.8) | 0.75 (0.7, 0.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hawkes, B.A.; Khan, S.M.; Bell, M.L.; Guernsey de Zapien, J.; Ernst, K.C.; Ellingson, K.D. Healthcare System Distrust and Non-Prescription Antibiotic Use: A Cross-Sectional Survey of Adult Antibiotic Users. Antibiotics 2023, 12, 79. https://doi.org/10.3390/antibiotics12010079
Hawkes BA, Khan SM, Bell ML, Guernsey de Zapien J, Ernst KC, Ellingson KD. Healthcare System Distrust and Non-Prescription Antibiotic Use: A Cross-Sectional Survey of Adult Antibiotic Users. Antibiotics. 2023; 12(1):79. https://doi.org/10.3390/antibiotics12010079
Chicago/Turabian StyleHawkes, Brooke A., Sana M. Khan, Melanie L. Bell, Jill Guernsey de Zapien, Kacey C. Ernst, and Katherine D. Ellingson. 2023. "Healthcare System Distrust and Non-Prescription Antibiotic Use: A Cross-Sectional Survey of Adult Antibiotic Users" Antibiotics 12, no. 1: 79. https://doi.org/10.3390/antibiotics12010079
APA StyleHawkes, B. A., Khan, S. M., Bell, M. L., Guernsey de Zapien, J., Ernst, K. C., & Ellingson, K. D. (2023). Healthcare System Distrust and Non-Prescription Antibiotic Use: A Cross-Sectional Survey of Adult Antibiotic Users. Antibiotics, 12(1), 79. https://doi.org/10.3390/antibiotics12010079







